Abstract
Background
Obesity is an established risk factor for renal disease and for disease progression. Therefore, an accurate determination of renal function is necessary in this population. Renal function is currently evaluated by estimated glomerular filtration rate (GFR) by formulas, a procedure with a proven high variability. Moreover, the adjustment of GFR by body surface area (BSA) confounds the evaluation of renal function. However, the error of using estimated GFR adjusted by BSA has not been properly evaluated in overweight and obese subjects.
Methods
We evaluated the error of 56 creatinine- and/or cystatin-C-based equations and the adjustment of GFR by BSA in 944 subjects with overweight or obesity with or without chronic kidney disease (CKD). The error between estimated (eGFR) and measured GFR (mGFR) was evaluated with statistics of agreement: the total deviation index (TDI), the concordance correlation coefficient (CCC) and the coverage probability (cp).
Results
The error of eGFR by any equation was common and wide: TDI averaged 55%, meaning that 90% of estimations ranged from −55 to 55% of mGFR. CCC and cp averaged 0.8 and 26, respectively. This error was comparable between creatinine and cystatin-C-based formulas both in obese or overweight subjects. The error of eGFR was larger in formulas that included weight or height. The adjustment of mGFR or eGFR led to a relevant underestimation of renal function, reaching at least 10 mL/min in 25% of the cases.
Conclusions
In overweight and obese patients, formulas failed in reflecting real renal function. In addition, the adjustment for BSA led to a relevant underestimation of GFR. Both errors may have important clinical consequences. Thus, whenever possible, the use of a gold standard method to measure renal function is recommended. Moreover, the sense of indexing for BSA should be re-considered and probably abandoned.
Similar content being viewed by others
Introduction
Worldwide, obesity has nearly tripled since 1975. In 2016, more than 1.25 billion adults (33% of the world's adult population) were overweight and 650 million were obese [1]. This pandemic of overweight and obesity may have severe consequences in Nephrology. In the context of metabolic syndrome i.e., the combination of obesity, hypertension, dyslipidemia and prediabetes among other alterations, obesity is a risk factor for renal disease [2,3,4,5]. In patients with established chronic kidney disease (CKD), obesity is also a risk factor for disease progression [6, 7]. Therefore, in obese and overweight patients, an accurate determination of renal function is necessary to evaluate the risk for renal disease as well as to monitor CKD progression.
More than 70 equations, based on creatinine and/or cystatin-C, have been developed in the last 60 years to estimate glomerular filtration rate (GFR). These equations have been extensively used in day-to-day clinical practise and research. However, the reliability of estimated GFR (eGFR) is still a matter of debate. Several studies criticise the use of formulas in diverse clinical conditions, such as CKD [8, 9], diabetes [10, 11], renal transplantation [12, 13], polycystic kidney disease [14], cancer [15], heart failure [16] and cirrhosis [17], among others. However, few studies specifically evaluated the error of eGFR in the obese population [18,19,20,21,22,23,24]. In addition, eGFR values are frequently reported as adjusted by body surface area (BSA). This adjustment is considered as the standard procedure in the evaluation of renal function, but in general reduces GFR in obesity. However, the difference between adjusted and unadjusted GFR in this population has been rarely evaluated [25,26,27,28,29,30,31]
The present study aimed to evaluate the error of creatinine and cystatin-C-based formulas as well as the impact of the adjustment of GFR by BSA in a group of 944 overweight and obese patients with and without CKD.
Material and methods
Patients
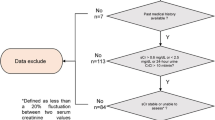
We performed a cross-sectional study of 944 consecutive obese (body mass index—BMI ≥ 30 kg/m2) or overweight (BMI 25–29.9 kg/m2) adult subjects with or without CKD attending the outpatient clinic of the Nephrology department at the Hospital Universitario de Canarias who underwent mGFR between July 2013 and December 2018. All patients signed an informed consent, and the study was approved by the Ethics and Clinical Research Committee.
Measured GFR
GFR was measured by the plasma clearance of iohexol as previously shown [32, 33]. In brief, 5 mL of iohexol (Omnipaque 300, GE-Healthcare) was injected intravenously during 2 min. Afterwards, venous samples or capillary blood by finger prick were obtained at 120, 180, 240, 300, 360, 420 and 480 min for patients with eGFR ≤ 40 mL/min; or at 120, 150, 180, 210 and 240 min for those with eGFR > 40 mL/min. For the dried blood spot (DBS) analysis, a fixed volume of capillary blood (10 µL) was drawed by a capillary pipette and deposited on filter paper (volumetric DBS method). Then, a circle of filter paper containing the whole drop of blood was punched out for analysis. The concentrations of iohexol were determined in plasma or DBS testing [32, 33].
Plasma clearance of iohexol was calculated according to a one-compartment model (CL1) by the formula: CL1 = Dose/AUC, where AUC is the area under the plasma concentration–time curve. Plasma clearances were then corrected using the formula proposed by Bröchner-Mortensen [34]: CL = (0.990778 × CL1)−(0.001218 × CL12).
Estimated GFR by formulas
Simultaneously to the plasma clearance of iohexol, serum and urinary creatinine and serum cystatin-C were determined to calculate eGFR. All the studied formulas are shown in www.ecihucan.es/lfr/apps/documents/egfr_formulas_v2019feb.pdf.
Adjustment for BSA
The agreement between eGFR and mGFR was evaluated with the formulas adjusted and unadjusted for BSA. When eGFR was already adjusted, we reversed the adjustment of the result by applying the following formula (GFR adjusted = GFR unadjusted/BSA × 1.73) [22, 25]. On the other hand, when eGFR was unadjusted, we adjusted the result by applying the formula (GFR unadjusted = GFR adjusted × BSA/1.73). BSA was calculated by DuBois and DuBois formula (BSA = 0.007184 × Weight0.425 × Height0.725) [35].
Biochemistry
Creatinine (mg/dL) was measured by enzymatic assay (IDMS-traceable creatinine) using the cobas c711 module (Roche Diagnostics). Cystatin-C (mg/L) was measured by immunonephelometry (BN II System-Siemens Healthcare Diagnostics), calibrated with ERM-DA471/IFCC.
Statistical analysis
Agreement between eGFR and mGFR
The agreement between eGFR and mGFR was assessed by specific statistics of agreement for continuous data, including: the concordance correlation coefficient (CCC), total deviation index (TDI) and coverage probability (CP) [36,37,38]. The CCC varies from 0 to 1 and combines meaningful components of accuracy and precision. A CCC > 0.90, reflects optimal concordance between measurements. TDI captures a large proportion of data within a boundary for allowed differences between two measurements. Empirical TDI was calculated for a theoretical TDI of 10% and a CP of 90%. We defined a priori that acceptable bias between eGFR and mGFR should be at least 10% and that 90% of the estimations should be included within these limits. This is based on the total variation of the method, which is 5–7% [39]. CP varies from 0 to 1, and estimates whether a given TDI is less than a pre-specified fixed percentage. Bland–Altman plots show the relationship between target and observed measurements and the mean of both [40]. The smaller the limits of agreements are, the higher is the degree of agreement between measurements.
The influence of indexing for BSA on renal function
The difference between adjusted and unadjusted mGFR or eGFR was calculated as the difference between unadjusted and adjusted GFR values.
Accuracy of estimated GFR with measured GFR
Finally, for the seek of comparability with other studies, we assessed the accuracy of each formula as the proportion of eGFR results within 10% (P10) and 30% (P30) of mGFR.
For agreement analyses, we designed and implemented a software solution (AGP Agreement Programme v1.0 IGEKO, SP) available at: www.ecihucan.es/lfr/apps/?dir=agreement_installer.
Also we used SPSS Statistics for Windows, version 17.0 (SPSS Inc., Chicago, IL, USA), and MedCalc Statistical Software version 13.0.2 (MedCalc Software bvba, Ostend, Belgium)
Results
Patients
We evaluated 944 patients, 491 overweight and 453 obese (298 class I, BMI = 30–34.9 kg/m2; 104 class II, BMI = 35–39.9; and 51 class III, BMI ≥ 40). About 70% of the patients were male and age averaged 59 ± 14 years (Table 1). Unadjusted and adjusted mGFR averaged 62.3 ± 34.6 mL/min (9.8–189.2 mL/min) and 54.8 ± 29.9 (9.4–160.5 mL/min), respectively (Table 1). Based on unadjusted mGFR, 212 subjects (22.5%) were classified in CKD 1; 252 (26.7%) in CKD-2; 262 (27.8%) in CKD 3; 198 (21.0%) in CKD-4; and 20 (2.1%) in CKD-5 (Table 1). A total of 630 (66.7%) had CKD and 314 (33.3%) had no evidence of renal disease (Table 1).
Agreement between measured and estimated GFR
Creatinine-based formulas
Thirty-three creatinine-based formulas were evaluated in all patients. For the equations unadjusted for BSA, TDI values were highly variable, ranging from 46.3% for the Lund–Malmö(Rv) to 144.7% for the Lund-2(LBM) equations (Supplementary Table S1). Frequently used formulas showed a TDI of ~55% indicating that 90% of estimations ranged from −55 to 55% of mGFR (Table 2). TDI values were comparable between subjects with overweight and obesity (Table 2) and including those with BMI > 35 kg/m2 (Supplementary Table S1). Only formulas that included weight, height or BSA had TDI values that increased from overweight to obesity (Table 3). In example, the TDI of the Cockcroft–Gault formula was 53.2% in subjects with overweight, 82.2% in obesity, and reached 100.6% in those with BMI > 35 kg/m2 (Table 3). The Salazar–Corcoran formula, which was specifically devised for obese subjects, showed a TDI comparable with other non-specific equations (Table 2). CCC averaged 0.84 for all formulas, reflecting moderate precision and accuracy in obese and overweight (Supplementary Table S1). CP averaged 22 for all formulas in overweight and obese population, indicating that more than 78% had an error greater than ±10% (Supplementary Table S1). The agreement between eGFR and mGFR using values adjusted for BSA was comparable with the results of unadjusted equations (Supplementary Table S2). Bland and Altman plots showed wide limits of agreement between mGFR and eGFR unadjusted for BSA, averaging from +30 to −40 mL/min, which indicates very poor agreement between eGFR and mGFR (Supplementary Fig. S1). Bland and Altman plots using mGFR and eGFR adjusted for BSA were comparable with the results of unadjusted values (Supplementary Fig. S1).
Cystatin-C-based formulas
Cystatin-C measurement was available in 731 patients (77.4%). TDI averaged 60% for the 19 cystatin-C-based equations, ranging from 44% for the Stevens-2 to 110% for the Perkins equations (Table 2). Frequently used equations showed a TDI of about 60% indicating that 90% of estimations ranged from −60 to 60% (Table 2). For example, the MCQ formula had a TDI of 54.6%, indicating that 90% of the estimations ranged from −54.6 to 54.6% of mGFR (Table 2). CCC averaged 0.90 for all the formulas, reflecting moderate precision and accuracy in obese and overweight patients (Table 2). Finally, CP averaged 26 for all the formulas, and so, 74% of the estimations had an error greater that ±10% in overweight and obese patients (Table 2). The agreement between eGFR and mGFR using values adjusted for BSA was comparable with the results of unadjusted equations (Supplementary Table S2). Bland and Altman plots showed wide limits of agreement between mGFR and eGFR unadjusted for BSA, averaging from +25 to −30 mL/min, which indicates poor agreement between eGFR and mGFR (Supplementary Fig. S1). Bland and Altman plots using mGFR and eGFR adjusted for BSA were comparable with the results of unadjusted values (Supplementary Fig. S1).
Creatinine and cystatin-C-based formulas
TDI averaged 48% for all the creatinine-cystatin-C-based formulas, ranging from 37.8% for the Stevens equation in overweight subjects to 71.2% for the FAS formula in obese subjects (Supplementary Table S1). For example, CKD-EPI formula in overweight patients had a TDI of 38.8%, and so, 90% of the estimations ranged from −38.8 to 38.8% (Table 2). CCC averaged 0.92 for all formulas, reflecting a good level of precision and accuracy, ranging from 0.85 to 0.95, for the FAS equation in overweight patients and the Stevens equation in obese patients, respectively (Supplementary Table S1). However, CP averaged 30 for all the formulas, indicating that more than 70% of the estimations had an error greater than ±10% (Supplementary Table S1). The agreement between eGFR and mGFR using values adjusted for BSA was comparable with the results of unadjusted equations (Supplementary Table S2). Bland and Altman plots showed wide limits of agreement between mGFR and eGFR unadjusted for BSA, averaging from +20 to −30 mL/min, which indicates poor agreement between eGFR and mGFR (Supplementary Fig. S1). Bland and Altman plots using mGFR and eGFR adjusted for BSA were comparable with the results of unadjusted values (Supplementary Fig. S1).
Creatinine Clearance
Creatinine clearance was available in 545 patients (57.7%). The agreement between creatinine clearance and mGFR reflected a TDI of 80%, so 90% of the estimations ranged from −80 to 80%. CCC averaged 0.84, reflecting moderate level of precision and accuracy. CP averaged 20, indicating that more than 80% of the estimations had an error greater than ±10% (Supplementary Table S3).
Accuracy between estimated and measured GFR
The proportion of eGFR results within ±10% (P10) of mGFR values (mL/min) were 26, 29 and 35% for creatinine, cystatin-C and creatinine and cystatin-C-based formulas, respectively. The proportion of eGFR results within ±30% of mGFR values (P30) were 65, 71 and 79% for the same group of equations (Supplementary Table S4). Similar results were observed for mGFR values adjusted for BSA (mL/min/1.73 m2) (Supplementary Table S5).
Examples of the error of eGFR
Table 4 illustrates the variability of eGFR through a wide range of values of unadjusted mGFR, from 12 to 120 mL/min. The cases were selected in groups of four including two overweight and two obese patients with similar mGFR values.
For cases 1–4 (mGFR of 12 mL/min), all formulas overestimated GFR in cases 1 and 3 (from 22 to 30 mL/min) and either over or underestimated in case 4 (from 7 to 20 mL/min). Moreover, the same equation could either overestimate or underestimate the same value of mGFR. In example, for cases 1 and 4, the CKD-EPI-cy estimated either 21 or 7 mL/min (Table 4). Similar errors were observed in all the examples. In some cases, the over or underestimation was as large as ±30–50%: cases 5–8 (mGFR of 30 mL/min), GFR was either overestimated (51 mL/min—case 8, Cockcroft–Gault) or underestimated (20 mL/min—case 7, CKD-EPI-cy) (Table 4). This variability led to misclassification in CKD stages: i.e., case 11 (mGFR = 45 mL/min, CKD 3) was incorrectly classified as CKD 1 by the Cockcroft–Gault formula (eGFR of 94 mL/min), whereas case 10 with a similar mGFR was misclassified in stage 2 by the same equation (eGFR of 71 mL/min) (Table 4). Also, hyperfiltration was misdiagnosed: i.e., cases 17 and 20 were not hyperfiltering based on mGFR (90 mL/min) while according to some equations had GFR > 120 mL/min; on the other hand, patients with real hyperfiltration (cases 22 and 23) were not classified as such by several equations (Table 4). Similar results were observed between eGFR and mGFR using data adjusted for BSA (Supplementary Table S6).
Differences between measured or estimated GFR adjusted and unadjusted for BSA
The median underestimation of mGFR by the adjustment for BSA was −6 mL/min (IQR −11.3 to −2.3 mL/min) in the whole population, –4 mL/min (IQR −9.1 to −1.3) in overweight and −7 mL/min (IQR −14.5 to 3.3) in obese subjects (Fig. 1a). The lower IQR means that in one patient out of four, the difference between adjusted and unadjusted mGFR ranged from −10 to −15 mL/min. This difference was even larger in extreme obese subjects (BMI > 40 kg/m2), where the median difference was −12.5 mL/min (IQR −23.2 to −4.7) (Fig. 1). Similar differences were observed for eGFR (Fig. 1). The overestimation by the adjustment of BSA was unusual.
Effect of the adjustment for body surface area (BSA) on measured and estimated glomerular filtration rate (mGFR/eGFR): The subjects were divided in overweight and obesity classes. The effect of the adjustment was evaluated by substracting the median value of unadjusted GFR to the median value of adjusted GFR. The result of this substraction implies an underestimation of both mGFR and eGFR that, in addition, increases as body mass index (BMI) becomes larger
Finally, patients with the same values of unadjusted GFR and BMI could have different adjusted GFR values (Fig. 2). In example, two patients with unadjusted mGFR of 100 mL/min and a BMI of 29 kg/m2 had adjusted mGFR values of 94 and 79 mL/min (Fig. 2). The variability of the results after adjustment was explained by the different BSA (Fig. 2). Finally, the higher the BSA the larger the difference between adjusted and unadjusted GFR values (Fig. 2). Similar differences were observed for eGFR (Fig. 2).
Effect of body surface area (BSA) and body mass index (BMI) in adjusted an unadjusted mGFR and eGFR values. a Patients with measured glomerular filtration rate (mGFR) of 100 mL/min (unadjusted): effect of the adjustment for body surface area in subjects with comparable BMI and different BSA. b Patients with estimated glomerular filtration rate of 100 mL/min by Chronic Kidney Disease Epidemiology Collaboration formulas based on creatinine (CKD-EPI-cr) of 100 mL/min (unadjusted): effect of the adjustment for body surface area (BSA) in subjects with comparable BMI and different BSA
Unnoticed hyperfiltration due to adjustment for BSA
The indexations of mGFR for BSA led to unnoticed hyperfiltering patients in 65% of the cases (Supplementary Table S7). Most common formulas misdiagnosed 25% of the patients with GFR > 120mL/min (Supplementary Table S8).
Discussion
We evaluated the error of eGFR in a group of obese and overweight subjects with BMI ranging from 25 to 64 kg/m2, with and without renal disease, including all CKD stages. Renal function was estimated with 56 formulas based on creatinine and/or cystatin-C, including old and recent equations, creatinine clearance and mGFR with a gold standard procedure, the plasma clearance of iohexol.
Our major finding was that the error of eGFR by any equation was wide and frequent. This error was comparable between subjects with overweight or obesity, either using adjusted or unadjusted eGFR. Formulas that included weight, height or BSA had an error that increased with BMI. The adjustment of mGFR or eGFR for BSA led to a relevant underestimation of renal function: ≥10 mL/min in 25% of the patients.
The error of formulas was extremely wide: 90% of the estimations had an error within ±55% of real GFR. This means that in subjects with a value of mGFR of 50 mL/min, renal function could be estimated from ~75 mL/min (+50%) to ~25 mL/min (−50%). Moreover, in the remaining 10% of the cases, this variability could be even larger. The error was comparable between creatinine-, cystatin- or creatinine + cystatin-based equations. Thus, cystatin-C seems not to improve the reliability of eGFR, a fact that questions the usefulness of this new marker, at least in overweight and obese patients. The agreement between eGFR and mGFR was comparable between modern or old formulas, meaning that more recent equations do not outperform the previous ones. Also, formulas specifically designed in obese subjects like the Salazar–Corcoran's had a similar TDI (51%) to other formulas (Table 2). Remarkably, the errors of eGFR were observed at random, since the same formula could over or underestimate a similar mGFR value, as observed in Table 4. For instance, the CKD-EPI-cr formula estimated 103 mL/min (+72%) or 48 mL/min (−20%) in two different patients with mGFR of 60 mL/min (cases 13 and 16, Table 4).
In general, the error of eGFR was comparable between obese and overweight subjects with the exception of those formulas that include height, weight or BSA in the equation (Table 3). For this group of formulas, the error of eGFR increased with BMI. This is not unexpected since these variables are factors of the equation and usually multiplied by other numerical constants in the numerator, a fact that artificially increase the relationship between weight and GFR in these patients (see www.ecihucan.es/lfr/apps/documents/egfr_formulas_v2019feb.pdf). In example, for two different cases (17 and 20, Table 4) with comparable mGFR of ~90 mL/min but different BMI: 26 and 36 kg/m2, the estimation of GFR by Cockcroft–Gault formula were 65 and 143 mL/min, respectively. Thus, these formulas should not be used in the overweight and obese population.
The utility of eGFR is a matter of debate [41]. The error of formulas in estimating GFR is common and averages ± 30% of real renal function [41]. Detailed information of the error of eGFR is available in refference [41]. In obesity, several studies have evaluated the reliability of formulas based on creatinine and/or cystatin-C in reflecting real renal function [18,19,20,21,22,23,24]. Our findings are in line with other studies. Verhave et al. evaluated the reliability of Cockcroft–Gault and MDRD formulas in 295 overweight and 190 obese patients. They concluded that Cockcroft–Gault and MDRD equations are not reliable in estimating GFR when obesity is present [21]. Also, the authors observed that increasing BMI was associated with GFR overestimation using Cockcroft–Gault equation (probably due to the inclusion of weight in the equation), whereas the estimations by MDRD formula were unaffected in the obese group [21]. On the other hand, some studies reported good correlation between eGFR and mGFR [18, 23]. However, they also showed wide limits of agreement between estimated and mGFR [18, 23].
The error of eGFR was comparable between formulas adjusted or unadjusted for BSA. This is not surprising: from a mathematical point of view, the adjustment for BSA is the same procedure applied to all formulas. So, adjusting or unadjusting the same value would not change the difference between the estimation and the measurement of renal function. On the other hand, the adjustment of GFR, either estimated or measured, led to a relevant underestimation of renal function in most of the cases. In fact, in one patient out of four, the difference between adjusted and unadjusted was about 10 mL/min or more in obese or overweight (Fig. 1). This underestimation of true GFR increased with the level of BSA (Fig. 1). Moreover, the overestimation of GFR increased with BMI. Also, BSA plays a role in the overestimation of GFR in obesity. Subjects with the same values of unadjusted mGFR and BMI may have different results of adjusted mGFR, reflecting the influence of the adjustment by BSA in the evaluation of renal function (Fig. 2a). Indexing GFR for BSA was based on the hypothesis, established in the 19th century, that metabolic rate was proportional to BSA [42]. This assumption is currently inexact [43,44,45]. Nevertheless, it was accepted in 1928 when McIntosh et al. noted the influence of BSA on urea clearance [46]. Needless to say, urea clearance is not a reliable procedure to estimate GFR. Metabolic rate is linked to nutritional and maintenance fluid requirements rather that weight or BSA [43]. Actually, Turner et al. showed that GFR did not increase as a linear function of BSA [45]. Moreover, BSA is not correlated with mGFR [47] or the number of glomeruli [29]. Chagnac et al. defended that the number of nephrons does not increase with body fat, and that obesity must result in an increase in the single-nephron GFR [48]. Also, the calculation of BSA is based on a questionable method initiated by the DuBois brothers in 1915 [49]. They devised a ‘height–weight formula’, using the ‘mould method' in nine patients as the gold standard, to estimate the surface of subjects if only their height or weight was known [35, 49]. Nevertheless, this equation has been questioned for its inaccuracy and wrong assumptions regarding the calculation of the surface area [43, 44]. Thus, the use of indexation of GFR by BSA is found on a deceitful premise and a rudimentary and inexact method to estimate BSA. Despite these limitations, indexing GFR by the Dubois–Dubois formula is widely used. Few groups have described the error of the adjustment for BSA. Delanaye and colleagues have elegantly criticised the error induced by indexing GFR for BSA [26,27,28]. Lemoine et al. concluded that indexing GFR by BSA would always lead to errors in GFR estimation [18]. Indeed, when drug dosing is considered, the Kidney Disease Improving Global Outcomes, Food and Drug Administration and European Medicines Agency recommend using a value for eGFR, which is not adjusted to the BSA [50,51,52]. Redal-Baigorri et al. [25] also noted that removing the adjustment by BSA improved the accuracy and precision of the CKD-EPI equation. Adjustment for BSA in obese or overweight patients should be re-considered and avoided.
The clinical consequences of the error of eGFR and underestimation due to adjustment for BSA are several and relevant, including: (1) incorrect evaluation of patients with CKD; (2) limitations in the risk assessment of renal disease progression since formulas may estimate either a faster or a slower decline of renal function compared with real GFR decline; (3) misclassification in higher or lower stages of CKD to stablish the magnitude of the disease; (4) no detection of hyperfiltration (GFR > 120 mL/min) considered as the first clinical sign of obesity-related glomerulopathy and diabetic nephropathy. Also, our findings must be taken into account in the design of studies aimed at evaluating the impact of weight reduction in the treatment and prevention of CKD. In these studies GFR must not be adjusted by BSA.
We implemented the plasma clearance of iohexol in 2012 [53]. This method is an excellent choice to measure GFR, since it is simple, reproducible, reliable, with reduced cost and safe. Then, we further simplified the method by blood collection using dried blood spots (DBS) [33]. The method is simple because it only requires a single intravenous injection of a small volume of the marker (5 mL), followed by repeated extractions of blood (10 μL each time). Also, neither extra-renal clearance nor renal metabolism of iohexol have been reported, which makes urine collection unnecessary [54]. In addition, the technique is reliable and reproducible because it is measured by a standard chromatographic technique, ultra violet high performance liquid chromatography which enables accurate quantification of low plasma concentrations. Of note, the inter-laboratory reproducibility is about 5% Equalis AB (Uppsala, Sweden). Finally, the safety profile of iohexol is excellent, with only minor side effects reported [39, 55, 56].
This study has strengths and limitations. To the best of our knowledge, this is the first study that evaluated all the available creatinine and/or cystatin-C-based formulas in overweight and obese. Also, we used modern and potent statistical tools such as the agreement method proposed by Lin et al. [36,37,38], to evaluate the reliability of these equations. Our population was entirely Caucasian and therefore, we cannot extrapolate the results to other populations like African Americans or Asian populations. Finally, our analysis is cross-sectional and the our results cannot be extrapolated to the analysis of GFR decline.
To conclude, formulas failed in reflecting properly renal function in overweight and obese patients. Formulas that include height, weight or BSA should not be used in this population. Caution is needed with the use of these formulas in clinical practise. The indexation of GFR by BSA results in a significant underestimation of GFR, especially in overweight and obese patients. The sense of indexing for BSA should be re-considered and probably abandoned. Whenever possible, measured renal function is recommended.
References
World Health Organization: obesity and overweight fact sheet. http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accesed 13 Nov 2018.
Pinto-Sietsma SJ, Navis G, Janssen WM, de Zeeuw D, Gans RO, de Jong PE, et al. A central body fat distribution is related to renal function impairment, even in lean subjects. Am J Kidney Dis. 2003;41:733–74.
Foster MC, Hwang SJ, Larson MG, Lichtman JH, Parikh NI, Vasan RS. Overweight, obesity, and the development of stage 3 CKD: the framingham heart study. Am J Kidney Dis. 2008;52:39–48.
Kramer H, Luke A, Bidani A, Cao G, Cooper R, McGee D. Obesity and prevalent and incident CKD: the hypertension detection and follow-up program. Am J Kidney Dis. 2005;46:587–94.
Vivante A, Golan E, Tzur D, Leiba A, Tirosh A, Skorecki K, et al. Body mass index in 1.2 million adolescents and risk for end-stage renal disease. Arch Intern Med. 2012;172:1644–50.
Bonnet F, Deprele C, Sassolas A, Moulin P, Alamartine E, Berthezène F, et al. Excessive body weight as a new independent risk factor for clinical an pathological progression in primary IgA nephritis. Am. J. Kidney Dis. 2001;37:720–7.
Berthoux F, Mariat C, Maillard N. Overweight/obesity revisited as a predictive risk factor in primary IgA nephropathy. Nephrol Dial Transplant. 2013;28 Suppl. 4:iv 160–6.
Padala S, Tighiouart H, Inker LA, Contreras G, Beck GJ, Lewis J, et al. Accuracy of a GFR estimating equation over time in people with a wide range of kidney function. Am J Kidney Dis. 2012;60:217–24.
Inker LA, Tighiouart H, Coresh J, Foster MC, Anderson AH, Beck GJ. GFR estimation using β-trace protein and β2-microglobulin in CKD. Am J Kidney Dis. 2016;67:40–8.
Iliadis F, Didangelos T, Ntemka A, Makedou A, Moralidis E, Gotzamani-Psarakou A, et al. Glomerular filtration rate estimation in patients with type 2 diabetes: creatinine- or cystatin-C-based equations? Diabetologia. 2011;54:2987–94.
Gaspari F, Ruggenenti P, Porrini E, Motterlini N, Cannata A, Carrara F, et al. The GFR and GFR decline cannot be accurately estimated in type 2 diabetics. Kidney Int. 2013;84:164–73.
Bosma RJ, Doorenbos CR, Stegeman CA, Van der Heide JJ, Navis G. Predictive performance of renal function equations in renal transplant recipients: an analysis of patient factors in bias. Am J Transplant. 2005;5:2193–203.
Luis-Lima S, Marrero-Miranda D, González-Rinne A, Torres A, González-Posada JM, Rodríguez A, et al. Estimated glomerular filtration rate in renal transplantation: the nephrologist in the mist. Transplantation. 2015;99:2625–33.
Ruggenenti P, Gaspari F, Cannata A, Carrara F, Cella C, Ferrari S, et al. Measuring and estimating GFR and treatment effect in ADPKD patients: results and implications of a longitudinal cohort study. PLoS One. 2012;7:e32533.
Craig AJ, Samol J, Heenan SD, Irin AG, Britten A. Overestimation of carboplatin doses is avoided by radionuclide GFR measurement. Br J Cancer. 2012;107:1310–6.
Smilde TD, van Veldhuisen DJ, Navis G, Voors AA, Hillege HL. Drawbacks and prognostic value of formulas estimating renal function in patients with chronic heart failure and systolic dysfunction. Circulation. 2006;114:1572–80.
Francoz C, Nadim MK, Baron A, Prié D, Antoine C, Belghiti J, et al. Glomerular filtration rate equations for liver-kidney transplantation in patients with cirrhosis: validation of current recommendations. Hepatology. 2014;59:1514–21.
Lemoine S, Panaye M, Pelletier C, Bon C, Juillard L, Dubourg L, et al. Cystatin-C-creatinine based glomerular filtration rate equation in obese chronic kidney disease patients: impact of deindexation and gender. Am J Nephrol. 2016;44:63–70.
Friedman AN, Strother M, Quinney SK, Hall S, Perkins SM, Brizendine EJ, et al. Measuring the glomerular filtration rate in obese individuals without overt kidney disease. Nephron Clin Pract. 2010;116:c224–c234.
Ozmen S, Kaplan MA, Kaya H, Akin D, Danis R, Kizilkan B, et al. Role of lean body mass for estimation of glomerular filtration rate in patients with chronic kidney disease with various body mass indices. Scand J Urol Nephrol. 2009;43:171–6.
Verhave JC, Fesler P, Ribstein J, du Cailar G, Mimran A. Estimation of renal function in subjects with normal serum creatinine levels: Influence of age and body mass index. Am J Kidney Dis. 2005;46:233–41.
Bouquegneau A, Vidal-Petiot E, Moranne O, Mariat C, Boffa JJ, Vrtovsnik F, et al. Creatinine-based equations for the adjustment of drug dosage in an obese population. Br J Clin Pharmacol. 2016;81:349–61.
Lemoine S, Guebre-Egziabher F, Sens F, Nguyen-Tu MS, Juillard L, Dubourg L, et al. Accuracy of GFR estimation in Obese Patients. Clin J Am Soc Nephrol. 2014;9:720–7.
Von Scholten BJ, Persson F, Svan MS, Hansen TW, Madsbad S, Rossing P. Effect of large weight reductions on measured and estimated kidney function. BMC Nephrol. 2017;18:52.
Redal-Baigorri B, Rasmussen K, Goya-Heaf J. The use of absolute values improves performance of estimation formulae: a retrospective cross sectional study. BMC Nephrol. 2013;14:271.
Delanaye P, Radermecker RP, Rovire M, Depas G, Krzesinki JM. Indexing glomerular filtration rate for body surface area in obese patients is misleading: concept and example. Nephrol Dial Transplant. 2005;20:2024–8.
Delanaye P, Mariat C, Cavalier E, Krzesinski JM. Errors induced by indexing glomerular filtration rate for body surface area: reductio ad absurdum. Nephrol Dial Transplant. 2009;24:3593–6.
Delanaye P, Krzesinski JM. Indexing of renal function parameters by body surface area: intelligence of folly? Nephron Clin Pract. 2011;119:c289–c292.
Nyengaard JR, Bendsten TF. Glomerular number and size in relation to age, kidney weight, and body surface in normal man. Anat Rec. 1992;232:194–201.
Hughson M, Farris AB 3rd, Douglas-Denton R, Hoy WE, Bertram JF. Glomerular number and size in autopsy kidneys: the relationship to birth weight. Kidney Int. 2003;63:2113–22.
D'Agati V, Chagnac A, de Vries AP, Levi M, Porrini E, Herman-Edelstein M, et al. Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol. 2016;12:453–71.
Luis-Lima S, Marrero-Miranda D, González-Rinne A, Torres A, González-Posada JM, Rodríguez A, et al. Estimated Glomerular Filtration Rate in Renal. Transplantation. 2015;99:2625–33.
Luis-Lima S, Gaspari F, Negrín-Mena N, Carrara F, Díaz-Martín L, Jímenez-Sosa A, et al. Iohexol plasma clearance simplified by dried blood spot testing. Nephrol Dial Transplant. 2017;2017. https://doi.org/10.1093/ndt/gfx323.
Bröchner-Mortensen J. A simple method for the determination of glomerular filtration rate. Scand J Clin Lab Investig. 1972;30:271–4.
Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition. 1989;5:303–11.
Lin L. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–68.
Lin L, Hedayat AS, Wu W. A comparative model for continuous and categorical data. In: Lin L, Hedayat AS, Wu W, editors. Statistical tools for measuring agreement. New York: Springer; 2012. p. 111–137.
Lin L, Hedayat AS, Sinha B, Yang M. Statistical methods in assessing agreement. J Am Stat Assoc. 2002;97:257.
Delanaye P, Ebert N, Melsom T, Gaspari F, Mariat C, et al. Iohexol plasma clearance for measuring glomerular filtration rate in clinical practice and research: a review. Part 1: how to measure glomerular filtration rate with iohexol? Clin Kidney J. 2016;9:682–99.
Altman DG, editor. Practical statistics for medical research. London: Chapman and Hall; 1991.
Porrini E, Ruggenenti P, Luis-Lima S, Carrara F, Jiménez A, de Vries APJ, et al. Estimated GFR: time for critical appraisal. Nat Rev Nephrol. 2019;15:177–90.
Rubner M. Ueber den Einfluss der Körpergrösse auf Stoff- und Kraftwechsel. Zeitschrift für Biologie. 1883;19:535–62.
Slone TH. Body surface area misconceptions. Risk Anal. 1993;13:375–7.
Gibson S, Numa A. The importance of metabolic rate and the folly of body surface area calculations. Anaesthesia. 2003;58:50–5.
Turner ST, Reilly SL. Fallacy of indexing renal and systemic hemodynamic measurements for body surface area. Am J Physiol. 1995;268:R978–R988.
Mcintosh JF, Möller R, VanSlyke DD. Studies of urea excretions: the influence of body size on urea output. J Clin Investig. 1928;6:467–83.
Dooley MJ, Poole SG. Poor correlation between body surface area and glomerular filtration rate. Cancer Chemother Pharmacol. 2000;46:523–6.
Chagnac A, Weinstein T, Korzets A, Ramadan E, Hirsch J, Gafter U. Glomerular hemodynamics in severe obesity. Am J Physiol. 2000;278:F817–F822.
Dubois D, Dubois E. The measurement of the surface area of man. Arch Intern Med. 1915;16:868–81.
KDIGO. CKD Evaluation & Management. KDIGO. http://kdigo.org/home/guidelines/ckd-evaluation-management.
EMA. Guideline on the evaluation of the pharmacokinetics of 4 medicinal products in patients with decreased renal 5 function. EMA. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/02/WC500162133.pdf.
FDA. Pharmacokinetics in patients with impaired renal function-study design, data analysis, and impact on dosing and labeling. FDA. http://www.fda.gov/downloads/Drugs/Guidances/UCM204959.pdf.
Luis-Lima S, Gaspari F, Porrini E, García-González M, Batista N, Bosa-Ojeda F, et al. Measurement of glomerular filtration rate: internal and external validations of the iohexol plasma clearance technique by HPLC. Clin Chim Acta. 2014;430:84–5.
Soveri I, Berg UB, Björk J, Elinder CG, Grubb A, Mejare I, et al. SBU GFR review group. Measuring GFR: a systematic review. Am J Kidney Dis. 2014;64:411–24.
Gaspari F, Thakar S, Carrara F, Perna A, Trillini M, Aparicio MC, et al. Safety of iohexol administration to measure glomerular filtration rate in different patient populations: a 25-year experience. Nephron. 2018;140:1–8.
Delanaye P, Melsom T, Ebert N, Bäck SE, Mariat C, Cavalier E, et al. Iohexol plasma clearance for measuring glomerular filtration rate in clinical practice and research: a review. Part 2: why to measure glomerular filtration rate with iohexol? Clin Kidney J. 2016;9:700–4.
Acknowledgements
We thank the Instituto de Tecnologías Biomédicas (ITB), the DISA Foundation, the Spanish Society of Nephrology (SENEFRO) and the IMBRAIN project for support (FP7-RE6-POT-2012-CT2012-31637-IMBRAIN) funded under the 7th Frameworks Programme capacities.
Funding
SLL is a researcher of the Juan Rodés Contract (Grant number: JR18/00027) of the Instituto de Salud Carlos III (Spain). EP is a researcher of the Programme Ramón y Cajal (Grant number: RYC-2014-16573) of the Ministerio de Ciencia, Innovación y Universidades (Spain). This study was supported by grants from the Instituto de Salud Carlos III (Grant numbers: PI13/00342 and PI16/01814) and Red de Investigación Renal (REDinREN) (Grant number: RD16/0009/0031).
Author information
Authors and Affiliations
Contributions
MLM, SLL and EP had the idea of the study. EM, MND, TF, BE, SE, PDM, DMM, AGR, RMMR, MACC and AT helped in the performance of the study. LDM and NNM performed the plasma clearance of iohexol. SLL evaluated the GFR determination. FGR design the figures and AJS performed the statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
López-Martínez, M., Luis-Lima, S., Morales, E. et al. The estimation of GFR and the adjustment for BSA in overweight and obesity: a dreadful combination of two errors. Int J Obes 44, 1129–1140 (2020). https://doi.org/10.1038/s41366-019-0476-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0476-z
- Springer Nature Limited
This article is cited by
-
The error of estimated GFR in predialysis care
Scientific Reports (2024)
-
Suggested clarification for the description of formulas on adjusting GFR for BSA
International Journal of Obesity (2023)
-
Kidney Considerations in Pediatric Obesity
Current Obesity Reports (2023)
-
Obesity and glomerular filtration rate
International Urology and Nephrology (2023)
-
Glomerular hyperfiltration
Nature Reviews Nephrology (2022)