Abstract
Background
Exercise is recognized to evoke multisystemic adaptations that, particularly in obese subjects, reduce body weight, improve glucometabolic control, counteract sarcopenia, and lower the risk of cardiometabolic diseases. Understanding the molecular and cellular mechanisms of exercise-induced benefits is of great interest due to the therapeutic implications against obesity.
Objectives and methods
The aim of the present study was to evaluate time-related changes in size distribution and cell origin of extracellular vesicles (EVs) in obese and normal-weight subjects who underwent a moderate-intensity exercise on a treadmill (at 60% of their VO2max). Blood samples were drawn before, immediately at the end of the exercise and during the postexercise recovery period (3 and 24 h). Circulating EVs were analyzed by a nanoparticle tracking analysis and flow cytometry after labeling with the following cell-specific markers: CD14 (monocyte/macrophage), CD61 (platelet), CD62E (activated endothelium), CD105 (total endothelium), SCGA (skeletal muscle), and FABP (adipose tissue).
Results
In all subjects, acute exercise reduced the release of total (i.e., 30–700 nm) EVs in circulation, predominantly EVs in the microvesicle size range (i.e., 130–700 nm EVs). The postexercise release of microvesicles was higher in normal-weight than obese subjects; after exercise, circulating levels of exosomes (i.e., 30–130 nm EVs) and microvesicles were, respectively, lower and higher in females than males. In all experimental subgroups (males vs. females and obese vs. normal-weight subjects), acute exercise reduced and increased, respectively, CD61 + and SCGA + EVs, being the effect on CD61 + EVs prolonged up to 24 h after the end of the test with subjects in resting conditions. Total EVs, exosomes, and CD61 + EVs were associated with HOMA-IR.
Conclusions
Though preliminary, the results of the present study show that a single bout of acute exercise modulates the release of EVs in circulation, which are tissue-, sex-, and BMI specific, suggesting that the exercise-related benefits might depend upon a complex interaction of tissue, endocrine, and metabolic factors.
Similar content being viewed by others
Introduction
Exercise is reported to induce multisystemic benefits in humans, including decreasing cardiovascular risk [1, 2], improvement of glucometabolic homeostasis [3, 4], promotion of weight loss [5], counteracting sarcopenia [6, 7], and stimulation of anabolic hormones [8,9,10] in obese and/or type 2 diabetic patients. In particular, to understand the “obesity paradox” that higher body mass index (BMI) is associated with lower morbility/mortality, mainly in the geriatric population, it is important to take muscle mass into account rather than adiposity. In fact, there is evidence that sarcopenia with obesity (i.e., sarcopenic obesity) may be associated with higher levels of metabolic disorders and an increased risk of mortality than obesity or sarcopenia alone [11]. Therefore, our rehabilitative efforts to promote exercise in obese subjects should focus on both preventing obesity and maintaining or increasing muscle mass [12].
Anyway, uncertain are the molecular mechanisms governing the interaction between exercising skeletal muscle and the other organs, such as adipose tissue, endothelium, and immune system, from which the exercise-induced cardiometabolic benefits derive.
There is robust evidence that exercise induces physiological and biochemical adaptations through the action of exerkines on target organs [13, 14], which can be distant from the site of production/release, mimicking the typical organization of the endocrine system [15].
Most biomolecules are extremely labile, easily inactivable by proteases and RNAases present in the plasma. In order to counteract this inhospitable environment, a very sophisticate system of extracellular trafficking and cell-to-cell targeting has been organized, i.e., the extracellular vesicles (EVs), including in particular exosomes and microvesicles. These are vacuolar structures, membrane-covered, containing proteins, nucleic acids (also of mitochondrial origin), and metabolites, which are implied in a wide range of physiological and pathological processes [16].
In particular, muscle-derived EVs have been shown to transfer exerkines of different chemical structure among cells and tissues [17, 18]. Furthermore, circulating levels of EVs change after exercise, having been produced and released by different tissues (not exclusively skeletal muscle) [19]. Type, intensity, and duration of exercise can modify size distribution and cell origin of EVs [20, 21]. There is the intriguing hypothesis that exercise-induced benefits, including improvement of glucometabolic homeostasis, decrease in cardiovascular risk and conversion/distribution of adipose tissue, are mediated by exosomes and/or microvesicles, which may act in an autocrine, paracrine, and endocrine manner, transferring exerkines from cell to cell [15].
One might hypothesize that EVs, native or pharmacologically modified, enriched with specific exerkines and endowed with antidiabetogenic, antisarcopenic, and antiobesogenic properties will represent, in future, a new therapeutic option for obesity-related comorbidities [14, 19]. In this context, the recent demonstration of a vesiculogenic hyper-responsiveness in obese subjects to environmental exposure (particularly, particulate matter, PM) with a (presumptive) increase in thrombotic and, in general, cardiovascular risk [22], suggests the existence of a “bad” vesiculogenic profiling, potentially changeable with adequate therapeutic intervention, including constant execution of moderate exercise [23].
Therefore, based on the previous considerations, evaluation of vesiculogenesis in obese (vs. normal-weight) female/male subjects undergoing an acute bout of exercise might be of great interest. So, taking into account the tissues on which exercise exerts beneficial effects (such as endothelium, muscle, adipose tissue, and the immune system) cytofluorimetric characterization of cell-specific EVs could be useful. In particular, this approach could help to set the protocols of metabolic rehabilitation adopted in the multidisciplinary integrated programs of body weight reduction. Furthermore, these knowledges could help in understanding the pathophysiological mechanisms underlying the “altered” vesiculogenic responsiveness in obese subjects to cardiometabolic factors [24] and environmental stimuli [22].
Material and methods
Subjects and protocol
Obese subjects (BMI > 40 kg/m2), hospitalized at the Istituto Auxologico Italiano, Piancavallo (VB), Italy, to take part of a multidisciplinary integrated program of body weight reduction were recruited for the current study. Normal-weight healthy subjects, age-matched, selected among friends and relatives of the medical and nursing staff, were recruited as control group. Both obese and normal-weight subjects were moderately active (60 min of physical activity, two-times/week). All females were eumenorrheic; the study was carried out in the follicular phase of their menstrual cycle.
After having verified exclusion criteria, particularly the existence of any disease, including blood hypertension and type 2 diabetes mellitus, apart from morbid obesity, or assumption of any drug, clinical, biochemical, and anthropometric data were collected from each participant, including evaluation of body composition by bioimpedance analysis (Human-IM Scan, DS-Medigroup, Milan, Italy). The test (described below) was administered after at least 5 days of accommodation/admission at Piancavallo, where there are very low levels of air pollution, in order to avoid the confounding factor of the environmental exposures on vesiculogenesis, such as PM [22].
Each subject underwent, in two different days (08:30–09:30 AM), the following exercise protocols:
Pilot test At the beginning of the study, each participant performed an incremental exercise on a treadmill (Technogym, Gambettola, Italy) until voluntary exhaustion; in particular, after 3 min of resting, the subject performed 2 min of walking at 4 km/h and 0% of slope, followed by speed increments of 0.5 km/h for each min up to 6 km/h; subsequent slope increments were of 1% for each min up to 15%. Exhaustion was defined when one of the following criteria was reached: (1) maximal levels (higher than 10) of self-perceived exertion, using the Borg’s modified CR10 scale [25] or (2) heart rate (HR) values higher than 90% of the age-predicted maximum. Data collected during the incremental test, including VO2max (Table 1) by indirect calorimetry (CPX Express, Medical Graphics Corp, MN), were utilized to set the intensity of the submaximal test.
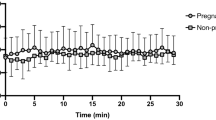
Submaximal test An exercise at a moderate constant workload, corresponding to 60% of the aerobic threshold (VO2max), established during the pilot test (see above), was maintained for 30 min or until voluntary exhaustion. Obese subjects reached a HR peak of 170.5 ± 9.9 beats per minute (bpm), while normal-weight subjects a HR peak of 166.7 ± 13.9 bpm, without any significant difference.
Four blood samples, referred to the submaximal test, were drawn from an antecubital vein of the arm by venipuncture: 1 h before exercise (basal), immediately at the end of the exercise (T0), 3 h after (T3) and in the next day at the same time when the test was performed (T24). While EV characterization (for size and cell origin) was performed in all time points, biochemical parameters were measured only in the basal sample (see Supplementary Material for details). Participants were permitted to consume comparable daily meals (i.e., lunch and dinner of the experimental day), which were strictly supervisioned by a nutritionist for food composition (about 21% proteins, 53% carbohydrates, and 26% lipids) and energy intake (adherence); the submaximal test (at the experimental day) and the last blood sampling (in the next day) were performed after 12 h fasting.
Characterization of size distribution and cell origin of EVs
Blood was collected into tubes containing EDTA and centrifuged at 1200 × g for 15 min at room temperature to obtain platelet-free plasma, which was transferred in temperature-controlled conditions (+4 C) to the EPIGET Lab (University of Milan) from Istituto Auxologico Italiano within 3–27 h after blood sampling. A detailed description of the method of EVs isolation and purification from plasma is reported in Supplementary Material.
Count and size of EVs were assessed by NTA (nanoparticle tracking analysis), a technique that measures the Brownian motion of vesicles suspended in fluid, which are displayed in real time through a high sensitivity CCD camera. Using a NanoSight LM10-HS system (Amesbury, UK), EVs were detected by laser light scattering. Five 30-s recordings were made for each sample. Collected data were analyzed with NTA software, which provides high-resolution particle-size distribution profiles and concentration measurements of the EVs (count/ml in plasma).
Cell origin of EVs was characterized by flow cytometry (MACSQuant, Miltenyi Biotec) according to a standardized protocol [22]. Shortly, fluoresbrite® Carboxylate Size Range Kit I (0.2, 0.5, 0.75, and 1 μm) was used to set the calibration gate on the analyzer. To analyze EV integrity, 60 μl aliquots were stained with 0.02 μM 5(6)-carboxyfluorescein diacetate N-succinimidyl ester (CFSE) at 37 °C for 20 min in the dark. Each aliquot of CFSE-stained sample was incubated with a specific antibody: CD14-APC (clone TÜK4) for monocyte/macrophage-derived EVs, CD105-APC (clone 43A4E1) for total endothelium-derived EVs, CD62E (clone REA280) for activated endothelium-derived EVs, CD61-APC (clone Y2/51) for platelet-derived EVs (Miltenyi Biotec, Bergisch Gladbach, Germany), A-FABP (clone B-4) for adipocyte-derived EVs, and α-sarcoglycan SCGA (clone F-7) for skeletal muscle-derived EVs (Santa Cruz Biotechnology, Dallas, Texas, USA). Before use, each antibody was centrifuged at 17,000 × g for 30 min at 4 °C to eliminate aggregates. The stained PBS control sample was used to detect the autofluorescence of the antibody. Quantitative multiparameter analysis of flow cytometry data was carried out by using FlowJo Software (Tree Star, Inc.).
Statistical analysis
Standard descriptive statistics were performed on all variables. Continuous data are expressed as mean ± standard deviation, while categorical data are presented as frequencies and percentages. Boxplots were used to represent counts of EVs and cell-specific EVs.
The Wilcoxon rank-sum test was used to compare, at baseline, demographics, clinical, and biochemical characteristics between obese and normal-weight subjects.
Since the aim of the study was to evaluate time-related changes in size distribution (analyzed as the following size ranges: 30–130 nm or exosomes, 130–700 nm or microvesicles and 30–700 nm or total EVs) and cell origin of EVs (i.e., CD14+, CD61+, CD62E+, CD105+, SCG+, and FABP+) in obese and normal-weight subjects, having outcome variables expressed as concentration (count/ml), a Poisson regression model for count data was applied to determine the associations between exercise (basal, T0, T3, and T24) and EVs or cell origins. The absence of over-dispersion was tested by the likelihood ratio test. All potential confounders were included in the multivariate model after having verified the presence of an association in a univariate model. Best model selection was based on the minimization of the Akaike information criterion and maximization of the explained variance of the model. The final models were adjusted for sex (F/M), BMI (obese/normal-weight) and HOMA-IR. Other variables, including smoking, duration of exercise, systolic and diastolic blood pressures, HR, waist to hip ratio (WHR), hCRP, HbA1C, LDL-C, HDL-C, T-C, and TG, were additionally considered, and then excluded in the final model as their contribution to explain variance was not relevant.
We further analyzed the effect of exercise in terms of distribution of vesicle mean concentrations for each EV size. For each EV size: (1) we estimated EV mean concentration and 95% confidence interval (CI) at each time with unadjusted Poisson linear regression models; (2) we compared the EV mean differences at each postexercise time with respect to basal; (3) we calculated q-FDR values using the multiple comparison methods based on Benjamini–Hochberg false discovery rate (FDR), which takes into account the high number of comparisons. As we observed different sex- and BMI patterns, the study population was stratified in four groups according to BMI (obese/normal-weight) and sex (M/F). Results were reported as a series graph for EV mean concentrations of each size and vertical bar charts to represent the three p- and q- (i.e., FDR p-) values obtained comparing T0, T3, or T24 vs. basal. For all the graphs, X axis was the size of EVs.
A p-value < 0.05 was considered statistically significant.
All analyses were run using SAS Software (version 9.4, Cary, NC: SAS Institute. Inc.).
Results
Study population included fifteen obese (F/M = 8/7) and eight normal-weight healthy subjects (F/M = 4/4). Main characteristics of the subjects, subdivided into normal-weight/obese and female/male groups, are reported in Table 1.
Boxplots describing time-dependent release of exosomes (i.e., 30–130 nm EVs), microvesicles (i.e., 130–700 nm EVs), and total EVs (i.e., 30–700 nm EVs) are reported in Fig. 1. Comparisons of the adjusted means of these EVs among the time points of the protocol (i.e., basal, T0, T3, and T24) are summarized in Table 2.
Boxplot of postexercise releases of plasma exosomes (30–130 nm EVs), microvesicles (130–700 nm EVs), and total EVs (30–700 nm EVs) (for all data). The vertical line inside the box is the median (50th percentile); the two vertical lines that constitute the top and bottom of the box are the 25th and 75th percentiles, respectively; the whiskers are calculated as ±1.5 × IQR; finally, the outliers are drawn as a small symbol. Mean EVs concentrations on Y axis are expressed as 108 count/ml. Asterisks indicate significant comparisons between adjusted mean EVs at each postexercise time point vs. basal value. *p < 0.05; **p < 0.01. Note that p-values were calculated from multivariable linear models adjusted for sex, BMI (obese/normal-weight), HOMA-IR, and time
In particular, after adjusting the models for sex, BMI, HOMA-IR, and time, the total EVs after exercise significantly decreased (p = 0.045), being the adjusted means of these EVs significantly reduced immediately at the end of the exercise and after 3 and 24 h (p = 0.013, p = 0.001, and p = 0.013 vs. basal, respectively) (Table 2). A similar significant decrease in microvesicles occurred after exercise (p = 0.008), being the adjusted means of these EVs significantly reduced after 3 and 24 h (p < 0.001 vs. basal for both time pints) (Table 2). The effect of exercise on exosomes was not significant (p = 0.265); anyway, exosomes immediately after the end of the exercise were significantly lower than those at the basal (p = 0.042) (Table 3). There was a significantly higher postexercise release of microvesicles in normal-weight than obese subjects (p = 0.036). Furthermore, a significant association of microvesicles with sex was found, being the postexercise release of these EVs higher in females than males (p = 0.033). When considering the association of exosomes with sex, there was a significantly lower release of these EVs in females than males (p < 0.042). No significant association of exosomes with BMI was found.
Figure 2 shows, in a whole view, without any pooling for size ranges, the effect of exercise in terms of distribution of vesicle mean concentrations for each EV (single) size. As different sex- and BMI-related patterns were present, the study population was stratified in four groups: i) normal-weight females (NW-F, panel A); ii) normal-weight males (NW-M, panel B); iii) obese females (OB-F, panel C); iv) obese males (OB-M, panel D). In particular, as shown by the upper part of each panel of Fig. 2, corresponding to one of these patients’ groups, exercise produced evident changes in the mean concentrations calculated for each EV size, ranging from 30 to 700 nm. The comparisons among the EV sizes are shown in the lower part of each panel of Fig. 2, where the three p- and q- (i.e., FDR p-) values obtained comparing T0, T3, or T24 vs basal are reported.
The top of each panel reports size profiling of plasma EVs at the nanoparticle tracking analysis (NTA) for each time of blood sampling (b T0, T3, and T24) after a single bout of acute exercise. The study population was stratified in four groups: a normal-weight females (NW-F); b normal-weight males (NW-M); c obese females (OB-F); d obese males (OB-M). The bottom of each panel reports the p- (dark dots) and q- (shaded dots) values of comparisons of EVs for the entire 30–700 nm size range at one postexercise time point (i.e., T0, T3, or T24) vs. basal b
Comparisons of the adjusted means of cell-specific EVs (i.e., CD14+, CD61+, CD62E+, CD105+, SCG+, and FABP + EVs) among the four time points of the protocol (basal, T0, T3, and T24) are summarized in Table 3. Figure 3 reports boxplots describing time-dependent releases of CD61+ and SCG + EVs.
Boxplot of postexercise releases of plasma CD61 + EVs (i.e., platelet-derived EVs) (left panel) and SCGA + EVs (i.e., muscle-derived EVs) (right panel). The vertical line inside the box is the median (50th percentile); the two vertical lines that constitute the top and bottom of the box are the 25th and 75th percentiles, respectively; the whiskers are calculated as ±1.5 × IQR; finally, the outliers are drawn as a small symbol. Asterisks indicate significant comparisons between adjusted mean EVs at each postexercise time point vs. basal value. *p < 0.05; **p < 0.01. Note that p-values were calculated from multivariable linear models adjusted for sex, BMI (obese/normal-weight), HOMA-IR, and time
In particular, after exercise, CD61 + EVs (i.e., platelet-derived EVs) significantly decreased (p = 0.025), being the adjusted mean of these EVs significantly reduced after 24 h (p < 0.001 vs. basal), with the counts at the other time points not significantly different vs. basal (Table 3). No significant association of CD61 + EVs with BMI was found; on the contrary, there was a significant higher postexercise release of these EVs in females than males (p = 0.037).
The effect of exercise on SCGA + EVs (i.e., skeletal muscle-derived EVs) was not significant (p = 0.121); nevertheless, there was a significant postexercise increase in the adjusted mean of these EVs immediately after the end of the exercise (p = 0.016 vs. basal), with the counts at the other time points not significantly different vs. basal (Table 3). No significant associations of SCGA + EVs with sex or BMI were found.
There were no significant associations of CD14+, CD62E+, CD105+, and FABP + EVs (i.e., monocyte/macrophage-, activated endothelium-, total endothelium-, and adipose tissue-derived EVs, respectively) with exercise, sex, and BMI.
Total EVs, exosomes and CD61 + EVs were significantly associated with HOMA-IR (β = 0.123 ± 0.044, p = 0.005; β = 0.183 ± 0.054, p = 0.001; β = −0.123 ± 0.044, p = 0.005; β = 0.238 ± 0.097, p = 0.014, respectively).
Discussion
The results of the present study, carried out in obese and normal-weight females and males undergoing a single bout of acute exercise, show that: (1) acute exercise is capable of decreasing the release of (total, i.e., 30–700 nm) EVs in circulation, acting predominantly on the microvesicle-enriched fraction (i.e., 130–700 nm EVs); (2) the postexercise release of microvesicles (i.e., 130–700 nm EVs) is higher in normal-weight than obese subjects; (3) the postexercise releases of exosomes (i.e., 30–130 EVs) and microvesicles (i.e., 130–700 nm EVs) are, respectively, lower and higher in females than males; (4) in all experimental subgroups (males vs. females and obese vs. normal-weight subjects), acute exercise reduces and increases, respectively, CD61 + EVs (i.e., those deriving from platelets) and SCGA + EVs (i.e., those deriving from skeletal muscle), being the effect on CD61 + EVs prolonged up to 24 h after the end of the test with subjects in resting conditions; (5) total (i.e., 30–700 nm) EVs, exosomes (i.e., 30–130 nm EVs), and CD61+ (i.e., platelet-derived EVs) are associated with HOMA-IR.
The major limitation of our study (present in most of the studies similar to ours) was the tissue characterization of EVs by using only a restricted panel of cell-specific antibodies. Furthermore, one tissue can release many EVs, phenotypically and functionally different, presumably characterizable with a variety of antibodies [26, 27]. For example, platelet-derived EVs can be CD61+, but not all platelet-derived EVs are likely to be CD61+ [28].
Based on the previous considerations, our finding that acute exercise provokes marked changes in sizes and counts of plasma EVs irrespectively from the characterization of cell origin suggests that an enormous variety of EVs, deriving from different tissues or from the same tissue with a different phenotype, is affected by exercise [21]. Further studies are needed to characterize these EVs mainly in terms of cell origin, an obligatory step before identifying the cargo of biomolecules inside each type of EVs and understanding their function [14].
In the present study, while there was no postexercise effect on exosomes (i.e., 30–130 nm EVs) apart from the significant post hoc comparison immediately after the end of the exercise (vs. basal). the release of plasma total (i.e., 30–700 nm) EVs and microvesicles (i.e., 130–700 nm EVs) decreased at 3 and 24 h after exercise. Total EVs also decreased immediately after the end of the exercise. Analyzing the counts of EVs for size and cell origin, these results cannot be numerically explained by the decrease of platelet-derived EVs (i.e., those CD61+), which, though prevalently microvesicles, represent only a minimal fraction. We can also rule out the contributions of the other EVs, characterized by flow cytometry with the antibodies used in the present study, being their plasma counts unchanged after exercise (particularly, endothelium-, adipocyte, and monocyte/macrophage-derived EVs). Because some cell-specific EVs could increase after exercise (see below for SGCA + EVs), this search becomes more difficult.
Sex-related differences in postexercise release of EVs were observed in the present study: in particular, after exercise, exosomes (i.e., 30–130 nm EVs) were lower in females than males, while microvesicles (i.e., 130–700 nm) were higher in females than males. Although postexercise release of EVs in females and males has been investigated in only a few studies [28, 29], sex hormones are likely to be responsible of this sex-related difference as suggest by the effects of menstrual cycle on (resting) vesiculogenesis [30].
Unfortunately, we were unable to characterize the cell origin of the EVs differently present in females vs. males, being negligible the higher postexercise contribution of CD61 + EVs (i.e., platelet-derived EVs) in females than males of our study. In this context, some other studies have demonstrated a sex dismorphism in the postexercise release of (CD31+/CD42b−) platelet- and (CD62E+) endothelium-derived EVs, an effect which also depends on exercise intensity [28, 29].
Although conflicting results have been reported, obese subjects generally exhibit increased plasma levels of EVs in resting conditions (approximately tenfold when compared with a normal-weight group), being the size profiling of the EVs formed by exosomes (20%) and microvesicles (80%) [31]. In contrast, in the present study, a BMI-related difference in postexercise vesiculogenesis was found, being the release of microvesicles (130–700 nm EVs) higher in normal-weight than obese subjects undergoing the same exercise test. As there were no BMI-related differences in postexercise decrease in total (i.e., 30–700 nm) EVs and CD61 + EVs and increase in SCGA + EVs, based on the results of the present study, EVs deriving from other tissues should be detected in future studies to determine the predominant tissue source of the different vesiculogenesis in obese vs. normal-weight subjects at rest and after an acute stimulus such as exercise.
Though acute exercise did not change the release of FABP + EVs (i.e., adipocyte-derived EVs), we hypothesize that the postexercise vesiculogenic responsiveness of obese subjects, when compared with the normal-weight counterpart, is due to “metabolic” factors to be identified. In this context, it is noteworthy that HOMA-IR was associated with postexercise releases of total (i.e., 30–700 nm) EVs, exosomes, and CD61 + EVs. The link between glucometabolic homeostasis and vesiculogenesis may be of great interest to understand the molecular and cellular mechanisms underlying the well-known antidiabetogenic effect of exercise in obese subjects [3, 4]. Given that obese patients are frequently insulin-resistant (a condition not occurring in the present study), an (intriguing) hypothesis is that it may not be obesity per se, but rather insulin resistance that produces a different postexercise response in EVs between obese vs. normal-weight groups. So, one might argue that a metabolically controlled obese subject obtains better cardiometabolic benefits from exercise. Indeed, the effectiveness of some multidisciplinary integrated programs of body weight reduction, in which exercise is combined with other interventions such as diet and pharmacotherapy, might derive from the relationship between vesiculogenesis and insulin resistance/sensitivity. Further studies are mandatory to confirm this hypothesis.
SCGA (i.e., sarcoglycan α) is a component of the dystrophin-glycoprotein complex, which, being implicated in type 2D autosomal recessive limb-girdle muscular dystrophy, has been supposed to play a fundamental role in the stability of muscle fiber membranes and in the connection of cytoskeleton to the extracellular matrix [32]. The gene scga is strictly expressed in striated skeletal muscle [33]. Postexercise release of SCGA + EVs has been already reported in humans together with the identification of a specific mRNA cargo [34].
To our best knowledge, the present study is the first to show that there is a postexercise of SCGA + EVs in obese subjects, too, a response that was similar to that in normal-weight subjects, with no differences in females and males for both BMI subgroups.
We are not aware whether there is an alteration in muscle vesiculogenesis in sarcopenic obesity, as our obese subjects were young with no clinical signs of sarcopenia. So far, this topic has been never investigated. Anyway, if SCGA + EVs are supposed to transfer a cargo of biomolecules endowed with “myoregulatory” function, such as myomiRs [34], any effort should be made to maximally stimulate the release of SCGA + EVs, which, in autocrine and paracrine manner, could contrast (or prevent) sarcopenia in obesity [15]. Therefore, the choice of an exercise in terms of type, intensity, and duration is fundamental when setting rehabilitative programs for sarcopenic obese subjects [19]. Further studies in exercising sarcopenic and nonsarcopenic obese subjects are mandatory to confirm our hypothesis regarding the physiological and also therapeutic role of SCGA + EVs.
Differently from the results of other studies, in which no difference or an increase in postexercise platelet-derived EVs (particularly, CD41a+, or CD42b + EVs) was found [19, 35, 36], a decrease in CD61 + EVs occurred in our study population after acute exercise. Interestingly, this effect was more evident at 24 h after the end of the test.
The physiological or pathophysiological role of CD61 + EVs, simply platelet-derived EVs, is only partially known [37]. There is some evidence that these EVs, including their cargo of biomolecules, are implicated in thrombotic, atherogenic and inflammatory processes [38]. So, one might argue that the exercise-induced beneficial effects on the cardiovascular system are mediated, at least in part, by an inhibition of platelet vesiculogenesis. As the protective effect of exercise on the cardiovascular system has been also demonstrated in healthy normal-weight subjects [39], our finding that both normal-weight and obese subjects exhibited a similar postexercise decrease in the release of CD61 + EVs supports the notion that a common molecular and cellular mechanism underlies the beneficial effects of exercise in all individuals with or without cardiometabolic diseases. Nevertheless, when exercise is strenuously executed at high intensity and for long times, the cardiovascular risk seems to increase, mainly due to a hypercoagulative state [40], which has been associated to a postexercise increase of plasma platelet-derived EVs in normal-weight subjects [41].
In the present study, use of antibodies for other cell-specific markers, for example CD14, CD62b, CD105, and FABP, evidenced no changes in the postexercise releases of monocyte/macrophage-, activated/resting endothelium-, and adipocyte-derived EVs, respectively. As conflicting results have been reported in the literature [19], we should identify the reasons of this discrepancy. Methodological differences, including the specificity of the antibodies, characteristics of the exercise test administered to the recruited subjects (type, intensity, and duration), times of blood sampling, and statistical pitfalls, such as sample size might be the most relevant reasons to be taken into account. As postexercise vesiculogenesis is crucial in understand molecular and cellular mechanisms underlying exercise-induced beneficial effects in special populations, particularly obese subjects [15], further studies, including those carried out in in vitro models consisting of specific cell lines, are needed to solve this issue.
In conclusion, the results of the present study show that a single bout of acute exercise induces changes in the release of EVs in circulation, which are tissue-, sex-, and BMI specific, suggesting that the exercise-related benefits might depend upon a complex interaction of tissue, endocrine, and metabolic factors [14, 19, 42].
Data availability
The datasets used and/or analyzed in the present study are available from the corresponding author on reasonable request.
References
Lin X, Zhang X, Guo J, Roberts CK, McKenzie S, Wu WC, et al. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2015;4:e002014.
Kasargod Prabhakar CR, Stewart R. Physical activity and mortality in patients with stable coronary heart disease. Curr Opin Cardiol. 2018;33:653–9.
Boniol M, Dragomir M, Autier P, Boyle P. Physical activity and change in fasting glucose and HbA1c: a quantitative meta-analysis of randomized trials. Acta Diabetol. 2017;54:983–91.
Pan B, Ge L, Xun YQ, Chen YJ, Gao CY, Han X, et al. Exercise training modalities in patients with type 2 diabetes mellitus: a systematic review and network meta-analysis. Int J Behav Nutr Phys Act. 2018;15:72.
Petridou A, Siopi A, Mougios V. Exercise in the management of obesity. Metabolism. 2019;92:163–9.
Lee DC, Shook RP, Drenowatz C, Blair SN. Physical activity and sarcopenic obesity: definition, assessment, prevalence and mechanism. Future Sci OA. 2016;2:FSO127.
Polyzos SA, Margioris AN. Sarcopenic obesity. Hormones. 2018;17:321–31.
Sartorio A, Lafortuna CL, Maffiuletti NA, Agosti F, Marazzi N, Rastelli F, et al. GH responses to two consecutive bouts of whole body vibration, maximal voluntary contractions or vibration alternated with maximal voluntary contractions administered at 2 h intervals in healthy adults. Growth Horm IGF Res. 2010;20:416–21.
Giunta M, Rigamonti AE, Agosti F, Patrizi A, Compri E, Cardinale M, et al. Combination of external load and whole body vibration potentiates the GH-releasing effect of squatting in healthy females. Horm Metab Res. 2013;45:611–6.
Rigamonti AE, Haenelt M, Bidlingmaier M, De Col A, Tamini S, Tringali G, et al. Obese adolescents exhibit a constant ratio of GH isoforms after whole body vibration and maximal voluntary contractions. BMC Endocr Disord. 2018;18:96.
Wannamethee SG, Atkins JL. Muscle loss and obesity: the health implications of sarcopenia and sarcopenic obesity. Proc Nutr Soc. 2015;74:405–12.
Rigamonti AE, De Col A, Tamini S, Cicolini S, Caroli D, De Micheli R, et al. Multidisciplinary integrated metabolic rehabilitation in elderly obese patients: effects on cardiovascular risk factors, fatigue and muscle performance. Nutrients. 2019;11:E1240.
Piccirillo R. Exercise-induced myokines with therapeutic potential for muscle wasting. Front Physiol. 2019;10:287.
Safdar A, Tarnopolsky MA. Exosomes as mediators of the systemic adaptations to endurance exercise. Cold Spring Harb Perspect Med. 2018;8:a029827.
Safdar A, Saleem A, Tarnopolsky MA. The potential of endurance exercise-derived exosomes to treat metabolic diseases. Nat Rev Endocrinol. 2016;12:504–17.
van Niel G, D’Angelo G, Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat Rev Mol Cell Biol. 2018;19:213–28.
Demonbreun AR, McNally EM. Muscle cell communication in development and repair. Curr Opin Pharmacol. 2017;34:7–14.
Whitham M, Parker BL, Friedrichsen M, Hingst JR, Hjorth M, Hughes WE, et al. Extracellular vesicles provide a means for tissue crosstalk during exercise. Cell Metab. 2018;27:237–51.
Eichner NZM, Erdbrügger U, Malin SK. Extracellular vesicles: a novel target for exercise-mediated reductions in type 2 diabetes and cardiovascular disease risk. J Diabetes Res. 2018;2018:7807245.
Wilhelm EN, González-Alonso J, Parris C, Rakobowchuk M. Exercise intensity modulates the appearance of circulating microvesicles with proangiogenic potential upon endothelial cells. Am J Physiol Heart Circ Physiol. 2016;311:H1297–310.
Wilhelm EN, Mourot L, Rakobowchuk M. Exercise-derived microvesicles: a review of the literature. Sports Med. 2018;48:2025–39.
Pergoli L, Cantone L, Favero C, Angelici L, Iodice S, Pinatel E, et al. Extracellular vesicle-packaged miRNA release after short-term exposure to particulate matter is associated with increased coagulation. Part Fibre Toxicol. 2017;14:32.
Davidson SM, Takov K, Yellon DM. Exosomes and cardiovascular protection. Cardiovasc Drugs Ther. 2017;31:77–86.
Csongrádi É, Nagy B Jr, Fulop T, Varga Z, Karányi Z, Magyar MT, et al. Increased levels of platelet activation markers are positively associated with carotid wall thickness and other atherosclerotic risk factors in obese patients. Thromb Haemost. 2011;106:683–92.
Borg GA. Perceived exertion: a note on “history” and methods. Med Sci Sports. 1973;5:90–3.
Xu R, Greening DW, Zhu HJ, Takahashi N, Simpson RJ. Extracellular vesicle isolation and characterization: toward clinical application. J Clin Investig. 2016;126:1152–62.
Milioli M, Ibáñez-Vea M, Sidoli S, Palmisano G, Careri M, Larsen MR. Quantitative proteomics analysis of platelet-derived microparticles reveals distinct protein signatures when stimulated by different physiological agonists. J Proteomics. 2015;121:56–66.
Durrer C, Robinson E, Wan Z, Martinez N, Hummel ML, Jenkins NT, et al. Differential impact of acute high-intensity exercise on circulating endothelial microparticles and insulin resistance between overweight/obese males and females. PLoS ONE. 2015;10:e0115860.
Lansford KA, Shill DD, Dicks AB, Marshburn MP, Southern WM, Jenkins NT. Effect of acute exercise on circulating angiogenic cell and microparticle populations. Exp Physiol. 2016;101:155–67.
Toth B, Nikolajek K, Rank A, Nieuwland R, Lohse P, Pihusch V, et al. Gender-specific and menstrual cycle dependent differences in circulating microparticles. Platelets. 2007;18:515–21.
Pardo F, Villalobos-Labra R, Sobrevia B, Toledo F, Sobrevia L. Extracellular vesicles in obesity and diabetes mellitus. Mol Aspects Med. 2018;60:81–91.
Tarakci H, Berger J. The sarcoglycan complex in skeletal muscle. Front Biosci. 2016;21:744–56.
Liu LA, Engvall E. Sarcoglycan isoforms in skeletal muscle. J Biol Chem. 1999;274:38171–6.
Guescini M, Canonico B, Lucertini F, Maggio S, Annibalini G, Barbieri E, et al. Muscle releases alpha-sarcoglycan positive extracellular vesicles carrying miRNAs in the bloodstream. PLoS ONE. 2015;10:e0125094.
Guiraud T, Gayda M, Juneau M, Bosquet L, Meyer P, Théberge-Julien G, et al. A single bout of high-intensity interval exercise does not increase endothelial or platelet microparticles in stable, physically fit men with coronary heart disease. Can J Cardiol. 2013;29:1285–91.
Chanda M, Nantakomol D, Suksom D, Palasuwan A. Cell-derived microparticles after exercise in individuals with G6PD Viangchan. Clin Hemorheol Microcirc. 2015;60:241–51.
Tao SC, Guo SC, Zhang CQ. Platelet-derived extracellular vesicles: an emerging therapeutic approach. Int J Biol Sci. 2017;13:828–34.
Wang ZT, Wang Z, Hu YW. Possible roles of platelet-derived microparticles in atherosclerosis. Atherosclerosis. 2016;248:10–6.
Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. 2018;5:135.
Ribeiro J, Almeida-Dias A, Ascensão A, Magalhães J, Oliveira AR, Carlson J, et al. Hemostatic response to acute physical exercise in healthy adolescents. J Sci Med Sport. 2007;10:164–9.
Maruyama K, Kadono T, Morishita E. Plasma levels of platelet-derived microparticles are increased after anaerobic exercise in healthy subjects. J Atheroscler Thromb. 2012;19:585–7.
Rigamonti AE, Resnik M, Compri E, Agosti F, De Col A, Monteleone P, et al. The cholestyramine-induced decrease of PYY postprandial response is negatively correlated with fat mass in obese women. Horm Metab Res. 2011;43:569–73.
Acknowledgements
The authors acknowledge the head-nurse Angela Seddone and the nursing staff at the Division of Auxology, Istituto Auxologico Italiano, Piancavallo, VB, Italy. Our special thanks go to the subjects and their families for their willingness to participate in this research. The authors thank Dr S. Zajac for the careful English revision.
Funding
The study was supported by Progetti di Ricerca Corrente, Istituto Auxologico Italiano, IRCCS, Milan, Italy.
Author information
Authors and Affiliations
Contributions
AER, together with VB and AS, designed the study. ADC, ST, and SC enrolled the subjects and performed the tests. RDM and GT performed the evaluation of body composition of all patients. ADC performed the biochemical determinations, while LP isolated and characterized plasma EVs. ST, ADC, and SC elaborated the database. SI and AER analyzed the data. AER, together with AS, wrote the manuscript. VB and SGC contributed to data interpretation and discussion writing. All authors contributed to the manuscript revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The patients and their parents (for the subjects younger than 18 years) and the healthy controls were fully informed of the procedures and possible risks associated with the experiments before giving their written consent to participate to the study. The protocol was approved by the local ethics committee (reference code: 01C825-2018; acronym: VESCIOBES). All procedures were in accordance with the Declaration of Helsinki (2000) of the World Medical Association.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rigamonti, A.E., Bollati, V., Pergoli, L. et al. Effects of an acute bout of exercise on circulating extracellular vesicles: tissue-, sex-, and BMI-related differences. Int J Obes 44, 1108–1118 (2020). https://doi.org/10.1038/s41366-019-0460-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0460-7
- Springer Nature Limited
This article is cited by
-
Enhancing circulatory myokines and extracellular vesicle uptake with targeted exercise in patients with prostate cancer (the MYEX trial): a single-group crossover study
BMC Cancer (2024)
-
Exploiting the therapeutic potential of contracting skeletal muscle-released extracellular vesicles in cancer: Current insights and future directions
Journal of Molecular Medicine (2024)
-
Effect of hypercholesterolemia on circulating and cardiomyocyte-derived extracellular vesicles
Scientific Reports (2024)
-
Extracellular vesicle distribution and localization in skeletal muscle at rest and following disuse atrophy
Skeletal Muscle (2023)
-
Sex differences in the transcriptome of extracellular vesicles secreted by fetal neural stem cells and effects of chronic alcohol exposure
Biology of Sex Differences (2023)