Abstract
Background
Decreasing selection and consumption of sodium and added sugars in the school cafeteria setting is important to provide optimal nutrition to children.
Objective
The ofjective of this study is to determine whether Louisiana (LA) Health, a school-based obesity prevention intervention, could successfully reduce children’s selection and consumption of sodium and added sugars during school lunches vs. the control group.
Design
Food selection, consumption, and plate waste from student lunches (3 consecutive days) in 33 public schools in rural Louisiana were collected and analyzed using the digital photography of foods method at baseline and after a 28-month obesity prevention intervention (LA Health) beginning in 4th–6th grade (87% of children received free or reduced cost lunch). Selection and consumption of energy, added sugar, and sodium was objectively measured using digital photography of foods. Mixed models, including Race and BMI, were used to determine whether change in selection and consumption differed by group.
Results
Sodium decreased for selection (− 233.1 ± 89.4 mg/lunch, p = 0.04) and consumption (− 206.3 ± 65.9, mg/lunch) in the intervention (vs. control) by month 18, and in consumption by month 28 (− 153.5 ± 66.9 mg/lunch, p = 0.03). Change in added sugar consumption decreased in the intervention (vs. control) at month 18 (− 3.7 ± 1.6, p = 0.05) and at month 28 (− 3.5 ± 1.6 tsp/lunch, p = 0.05).
Conclusions
LA Health decreased the amount of added sugar and sodium selected and consumed, but not plate waste, by month 28. Results highlight the importance of long-term interventions and policies targeting provision and selection to improve dietary patterns in children, with less focus on plate waste.
Similar content being viewed by others
Introduction
Dietary guidelines influence millions of people’s eating patterns through the food served and mandated by federal programs in the United States. The Healthy, Hunger-Free Kids Act of 2010 highlights the central role school nutrition has in health among children and provides updated nutrition standards for the National School Lunch Program (NSLP) in response to growing obesity trends in US children and adolescents [1]. Changes include increasing selection of fruit, vegetable, whole grain, and low-fat and fat-free milk, while lowering total fat, saturated fat, and sodium. The goal is to meet the dietary needs of children within their required calorie ranges. Upper limits are set for energy, saturated fat, total fat, and sodium consumption, whereas no specific guidelines were created for added sugar.
The 2010 Dietary Guidelines for Americans recommend that individuals consume ≤ 2300 mg/day of sodium and 1500 mg/day for special populations such as black individuals and children with cardiovascular disease (CVD), metabolic syndrome, and chronic kidney disease [2]. The reduction of dietary sodium has long been a focus of the USDA when setting school meal guidelines, although very little progress has been made in meeting the guidelines. Currently, over 90% of children in the United States consume too much sodium. Excess consumption of sodium can be associated with high blood pressure leading to heart disease and stroke, which occur more commonly in adulthood, with origins in childhood [3]. In addition, some studies report that sodium may be implicated in weight gain, possibly due to increased thirst levels and sugar-sweetened beverage consumption patterns [4, 5]. Finding ways to decrease sodium and added sugar in school cafeterias is crucial to providing optimal nutrition for the 31 + million children that receive most of their meals in the school setting through the NSLP [6, 7].
Based on scientific evidence, new recommendations from the American Heart Association (AHA) are that Americans ( ≥ 2 years) should not be consuming more than six teaspoons of added sugar per day, which accounts for no more than ~100 kcal/day from added sugar alone [8]. In addition, the 2015–2020 Dietary Guidelines for Americans recently revised their recommendations for added sugar to be ≤ 10% daily kcal from added sugars, but currently there are no standards for school meals [9]. Excess sugar intake is associated with dental caries, obesity, metabolic syndrome, and heart disease [8, 10, 11]. In addition, it provides extra calories with little to no nutritional benefit that children cannot afford, as more than one-third (37.4%) of US children and adolescents are overweight (OW) or obese (OB) [12, 13].
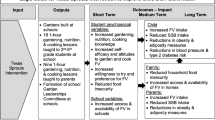
Previous studies testing school-based interventions that modify school cafeteria environments have shown improvements in nutrition measures, including increased selection and consumption of healthy foods [14,15,16,17]. As previously reported, the LA Health intervention was a long-term school-based obesity prevention intervention resulting in decreased body fat. In addition, secondary outcomes of the intervention revealed improved healthy eating among children after modification of the school cafeteria environment when compared with the control group. Results showed a significant decrease in energy, fat, and saturated fat consumption, as well as improved diet quality calculated using the Healthy Eating Index (HEI) [14, 18, 19]. The aim of the current analysis is to determine whether a 28-month school-based obesity prevention intervention (vs. control) reduced children’s selection and consumption of added sugars and sodium during school lunches. It was hypothesized that the children in the Louisiana (LA) Health intervention (vs. control) would decrease the amount of added sugar and sodium selected and consumed at lunch. The LA Health intervention provides a unique opportunity, to examine nutritional changes in components of children’s lunch consumption using objectively measured food intake data from the school cafeteria setting. These results could help provide further direction for federal regulation of sodium and added sugars in school meals, as well as guidance for schools to reduce sodium and added sugar in meals provided.
Methods
Participants and procedures
The LA Health study was a randomized (by school cluster) controlled trial that compared two active treatment arms with a control group [19]. The intervention arms of relevance to this paper included a 28-month school-based obesity prevention program that focused on modification of the school environment to promote healthy eating and physical activity. This paper focuses on the modification of the cafeteria environment and extends the findings reported in two earlier papers [14, 18]. This school environmental program was delivered from 2006 to 2009, to children in 33 elementary schools in rural LA with a high prevalence of low socioeconomic status (n = 1626). The goal of the project was to investigate the efficacy of a multi-component intervention focused on modifying environmental and behavioral factors to help prevent inappropriate weight gain in children beginning in 4th –6th grade with follow-up in 6th–8th grade. The two school-based prevention programs of the LA Health study were described as primary (environmental) and a combination of primary and secondary (internet/classroom) prevention strategies. Primary prevention strategies expose all individuals to the prevention program and, in this case, focused on changes to the school environment compatible with conventional nutrition recommendations (e.g., five fruits and vegetables per day, < 30% of dietary energy from total fat, < 10% of dietary energy from saturated fat, and 20–30 g of fiber/day), increasing physical activity by the promotion of 60 min of moderate to vigorous activity per day. In addition, the intervention targets the food service environment by promoting the Child Nutrition Program to meet USDA guidelines for the NSLP [20], the WIC Reauthorization Act of 2004 [21], and Act 331 of the LA Legislature related to advertisement of fast foods and the content of vending machines and concessions in schools [22]. Secondary prevention strategies target affected individuals and, in this study, relied upon the social learning theory, and were designed to target individual behaviors based on the child’s weight status through computer-generated learning modules directed at the child’s individual weight status. Secondary prevention approaches place greater emphasis on behavior modification approaches designed to change personal factors such as increased healthy eating habits, increased physical activity, and decreased sedentary behavior. No differences in primary (weight change) or secondary outcomes (nutrition measures) were shown between the primary and primary + secondary arms of the intervention; thus, data for analysis of these treatment arms were combined to define an intervention arm and control arm. Dietary measures were quantified at lunch over at least 3 days for each participant at baseline, 18 months, and 28 months follow-up. For further details, refer to Williamson et al. [19]. All children participating in the study signed an assent form to be in the study, and all children and their parents signed consent to participate before data collection.
Measures and procedures
The digital photography of foods method, which has been found to accurately quantify food consumption in cafeteria settings [19, 23,24,25,26,27], was used to objectively measure food selection, food consumption, and plate waste of children’s cafeteria lunches over 3 days. Briefly, foods selected before eating were photographed with digital video cameras. Plate waste was photographed with a second camera after children ate and returned their trays. Children were aware that their food selection and waste was being captured and the participants in the research project were identified by an identification card on their tray. Food consumption was calculated using existing and validated procedures that produce reliable and accurate food intake measurements among adults [26, 27] and children [25, 28]. For this analysis, the data on selection, consumption, and plate waste for added sugar and sodium in the intervention and control groups were evaluated to assess change from baseline to follow-up. Intraclass correlation coefficients (ICCs) were calculated on 30% of the data that were evaluated by two estimates as a measure of inter-rater agreement to assess the reliability of the digital photography method. The ICCs for estimates of food selection, consumption, and plate waste for energy (kcal), sodium, and sugar ranged from 0.97 to 0.99.
Statistical analysis
All data were collected at the individual child level. All analyses were performed using intention-to-treat principle. Children who had data at baseline and at least 18 months or 28 months were included in the model. Change in added sugar (tsp/meal) and sodium (mg/meal) from baseline were the primary outcomes. Change in energy (kcals/lunch) was included in this analysis for comparison of changes in sodium and added sugar relative to changes in energy, although these results were previously published elsewhere using a different statistical model [14]. Analyses were completed using SAS/STAT® software, Version 9.4 of the SAS System for Windows (Cary, NC, USA). Separate linear mixed models for repeated measures were used to model observed differentials for energy, added sugar, and sodium from baseline (BL/Week 0) to follow-up measurements (months 18 and 28). Terms for intervention group, timeID [(1) change from BL to 18 months and (2) change from BL to 28 months], race, and body mass index (BMI) percentile group (underweight/normal weight, OW, and OB) were used in constructing the model along with all interactions among these terms. Covariates were also included to account for sex, age at enrollment, and baseline values of energy, sodium, or added sugar. Random effects were incorporated to address participant-level serial correlations and variability due to independent school clusters. The subject-level correlations were characterized with a compound symmetric structure. Linear contrasts of least squares means were constructed to compare within- and between-intervention group changes from baseline to 28 months, both overall and by race and BMI percentile groups. A step down Sidak adjustment was applied to control type I error rate among the multiple pairwise post hoc comparisons and significance was set at p ≤ 0.05.
Results
Characteristics of the sample
The study sample included 1626 children (intervention: n = 1195, control: n = 431) with approximately 95.6 children per school and can be found in Table 1. The mean (SD) age of the sample was 10.5 (1.2) years; the sample was 58.6% female and 69.8% Black (Table 1). Children who brought their own lunches were not included in the analysis, but as 87% of children received free or reduced cost lunch we were able to catch a large majority of the students. BMI percentile was highly skewed so the data are reported as median (min, max) and was 78.9 (0.0, 99.9) at baseline. Baseline added sugar selection (control: 17.9 ± 9.5 tsp/lunch, intervention: 18.0 ± 8.7 tsp/lunch) and consumption (control: 12.2 ± 8.4 tsp/lunch, intervention: 12.5 ± 7.6 tsp/lunch), as well as sodium selection (control: 1295.7 ± 326.3 mg/lunch, intervention: 1316.6 ± 340.8 mg/lunch) and consumption (control: 876.5 ± 305.5 mg/lunch, intervention: 972.7 ± 335.9 mg/lunch) can be found in Table 1. At baseline, there were significant differences in sodium consumption between the control and intervention arms. Furthermore, the study cohort had a higher prevalence of black (69.8%) children in comparison with white (30.2%) children and this difference was observed in both treatment arms. Differences between white and black children are discussed briefly below.
Change in energy
Change in energy selection, consumption, and plate waste (kcals/lunch) between the intervention and control groups at month 18 and 28 can be found in Fig. 1. There was a significant main effect of treatment × timeID for selection (p = 0.002) and consumption (p ≤ 0.001). At month 18, no differences were shown for change in energy selection, consumption, or plate waste. At month 28, there was a significant change in energy consumption (p = 0.02); the intervention consumed 75.6 ± 27.4 kcals/lunch less compared with the control. No other between-group differences were found.
Change in energy a selection, b consumption, and c plate waste for control and intervention from baseline (BL) to 18 and 28 months. No significant between group changes were shown by month 18 for selection (p = 0.51), consumption (p = 0.42), and plate waste (p = 0.99). By month 28, change in consumption (p = 0.02) was significantly difference between groups, but not for selection (p = 0.08) or plate waste (p = 0.99). *Significant between-group change (p < 0.05)
Change in sodium
Change in sodium selection, consumption, and plate waste (mg/lunch) between the intervention and control groups can be found in Fig. 2. There was a significant main effect of treatment for change in sodium selection (p = 0.04) and consumption (p = 0.01). At month 18, change in sodium selection (233.10 ± 89.4 mg/lunch, p = 0.04) and consumption (206.3 ± 81.6 mg/lunch, p = 0.01) increased in the control compared with the intervention. By month 28, change in sodium consumption increased in the control compared with the intervention (153.5 ± 66.9 mg/lunch, p = 0.03). No other between-group differences were found.
Change in sodium a selection, b consumption, and c plate waste for control and intervention from baseline (BL) to 18 and 28 months. At month 18, change in sodium was significantly lower for the intervention (vs. control) for selection (p = 0.04) and consumption (p = 0.01), but not plate waste (p = 0.77). By month 28, change in sodium consumption (p = 0.03) was significantly lower for the intervention (vs. control), whereas no differences were shown for selection (p = 0.07) or plate waste (p = 0.77). *Significant between group change (p < 0.05)
Change in added sugar
Change in added sugar selection, consumption, and plate waste (tsp/lunch) between the intervention and control groups can be found in Fig. 3. There was a significant effect of treatment for consumption (p = 0.03). At month 18, change for added sugar consumption (p = 0.02) increased by 2.4 ± 1.9 tsp/lunch in the control, whereas no change was shown in the intervention. By month 28, change in added sugar consumption (p = 0.05) significantly decreased by − 3.5 ± 1.6 tsp/lunch in the intervention compared with the control. No other between-group difference was found.
Change in added sugar a selection, b consumption, and c plate waste for control and intervention from baseline (BL) to 18 and 28 months. By month 18, change in added sugar consumption (p = 0.02) was significantly lower for the intervention (vs. control), but no differences were shown for selection (p = 0.08) or plate waste (p = 0.74). By month 28, change in added sugar consumption (p = 0.05) was significantly lower in the intervention (vs. control), whereas no differences were shown for change in consumption (p = 0.08) or plate waste (p = 0.74). *Significant between-group change (p < 0.05)
Discussion
To our knowledge, we are the first to examine if a 28-month school-based obesity prevention intervention can reduce children’s selection and consumption of sodium and added sugars during school lunches. The results demonstrate that the LA Health obesity prevention intervention, when compared with the control, is effective at reducing children’s overall sodium and added sugar consumption in a 28-month intervention to school cafeterias. These results further demonstrate the effectiveness of the LA Health intervention to increase measures of healthy eating and dietary quality in children. No meaningful changes were shown in plate waste measures for energy, added sugar or sodium; therefore, similar to previously reported results [14], reductions reflect changes to the food provided to, and selected by, the students. This highlights the role that environment can have in overall health of children and support adherence to recent updates to school nutrition guidelines [1]; by modifying the school cafeteria environment, improvements can be seen in healthy eating and quality of dietary intake in children, especially over time.
Non-communicable diseases (NCD), such as hypertension (HTN), CVD, metabolic syndrome, and obesity are the leading cause of death world-wide and they are most common in lower and middle-income populations [29]. Although NCDs and associated complications are commonly found in adulthood, several studies suggest that preventative actions should be taken in childhood [30,31,32,33,34]. Recently, the USDA revised the school nutrition guidelines and created upper limits for the amount of energy, fat, saturated fat, and sodium, and lower limits on fruits, vegetables, meats, grains, and milk to increase the nutritional density of school cafeteria lunches within their energy ranges. The goal of the LA Health intervention was to decrease excessive weight gain among children by delivering an environmental obesity prevention program. To accomplish this aim, the types of foods and food preparation methods in the intervention schools were altered to promote a healthier diet (e.g., a lower total fat and saturated fat diet, lower sodium foods, decreased added sugar, increased consumption of fruits and vegetables, etc.). This provides an ideal sample to examine nutritional indicators as well as strategies to improve dietary outcomes.
As previously reported, ~45% of children in this study were OW or OB at baseline [35]. This is consistent with other studies examining a student population with a high prevalence of low socioeconomic status and suggests that many children are consuming energy in excess of their appropriate estimated energy requirements for their age [15, 16, 36,37,38]. Energy consumption decreased in the intervention group only by month 28 and, as previously reported [14], improved measures of healthy eating (via HEI) were shown for children in the LA Health intervention. The current mixed model-based analysis was modified from previously reported analyses of these data to allow investigation of intervention effects, while controlling for race and BMI status. Previously reported data on the Wise Mind Intervention [14, 28], which had similar intervention approaches, revealed significant decreases in energy consumption in the intervention group during an 18-month intervention. However, it should be noted that subject population of the Wise Mind Study was almost entirely White children (95% White) and, as previously mentioned, ~70% of the children in The LA Health intervention were black and of lower socioeconomic status than Wise Mind.
Most people in the United States are consuming sodium in excess of daily guidelines ( ≤ 2300 mg/day) and no meaningful progress has been made in reducing consumption. Similar to adults, children with high sodium diets often have higher blood pressure and reducing sodium consumption during childhood has been shown to lower blood pressure. Thus, decreasing sodium consumption during childhood and early adulthood can help attenuate age-related increases in blood pressure and possibly help prevent, or delay the onset, of clinical HTN. The current guidelines for sodium in school lunches ( ≤ 1230 mg/lunch for K-5th grade, ≤ 1360 mg/lunch for 6th–8th grade, and ≤ 1420 mg/lunch for 9th–12th grade) were included due to evidence of a relationship between sodium consumption and blood pressure, as well as between CVD and blood pressure [39]. Healthy People 2020 emphasizes the need to further decrease sodium in school lunches with the goal of ≤ 640 mg/lunch for k-5th grade, ≤ 710 mg/lunch for 6th–8th grade, and ≤ 740 mg/lunch for 9th–12th grade by school year 2022–2023 [40]. At baseline, children in the LA Health intervention were selecting ~1300 mg and consuming ~925 mg during lunch alone. Sodium selection and consumption was moderated in children in the LA Health intervention, whereas the control group increased the amount of sodium consumed by ~257 mg for selection and ~244 mg for consumption. The increase in sodium seen in the control group reflected natural changes to the school food environment, which were mitigated by the intervention, further demonstrating the need for interventions of the school cafeteria environment focusing on all aspects of a school nutrition guidelines.
Children consume ~19 teaspoons of added sugar daily in the United States, which equates to ~300 kcal. Children in this study had a baseline added sugar selection of 18 tsp and consumption was ~12 tsp during lunch alone. Sugary foods often take precedence over more healthy foods and therefore children are overfed energy while being undernourished [8]. Current guidelines advise decreasing added sugar in the overall diet, but no specific guidelines have been established for added sugar. The 2015–2020 Dietary Guidelines for Americans include guidelines to be set at ≤ 10% daily kcals from added sugars (also required on all food labels by July 2018 [41]) and the AHA followed that with recommendations of no more than six teaspoons per day of added sugar. A recent meta-analysis concluded that sugar consumption is a determinant of body weight in free-living individuals resulting primarily from an alteration in energy balance, as shown in studies where sugar consumption is deliberately increased. A small reduction in body weight was shown when reducing sugars in the diet, although the effects of long-term reduction of sugar in the diet is lacking [42]. Children in the LA Health intervention decreased their total added sugar intake by ~6 tsp per lunch when compared with the control group, which equates to ~100 kcal less a day coming from empty calories. These improvements only account for reductions in lunches served in schools and if projected over the rest of the day would reflect meaningful daily reductions.
It is suggested healthy eating behaviors should be directed to children since an unhealthy diet early in life can lead to serious health consequences later in life. The inclusion of children ≥ 2 years of age for sodium and added sugar guidelines is based partly on concerns with development of taste preferences for salt and sugar dense foods [43,44,45,46]. Reducing sodium and sugar in school meals has been a challenge, because these foods are appealing to students and school administrators since these typically sell more, providing additional funds for schools [47, 48]. The LA Health intervention provides crucial environmental and behavioral strategies for improving healthy eating in children, especially in decreasing sodium and added sugar consumption. Interventions focused on increasing fruit and vegetable intake, such as community gardens are suggested, as they have shown to increase consumption of important nutrients and should be used in future studies to target children at an early age [49, 50].
Small changes can be made in nutrition measures with sustained acceptance from children, especially over time, to offer children more nutrient dense, but not calorically dense, meals [28, 38, 51]. The LA Health intervention was successful at reducing selection and consumption of sodium and added sugar during school lunches by month 28. Further, the results stress the importance of long-term interventions to see effective results in children as no significant changes were shown at month 18 in this population. Together, these data suggest that policy regarding sodium and added sugar consumption in children is likely an effective strategy to reduce the risk of OW and OB in children, and that rigorous efforts need to be taken to change behaviors and the environment to improve diet quality for children. Future studies should focus on further reduction of sodium and added sugar in the schools, specifically during breakfast and snacks, as well as outside the school setting, with a special focus on underserved children. Finally, we need to work at various levels to rely less on the sugar and sodium industry and agree on proper public health guidelines to limit sodium and added sugar consumption in children.
References
Food and Nutrition Service, United States Department of Agriculture. Nutrition standards in the National School Lunch and School Breakfast Programs; proposed rule. Fed Regist. 2012;77:4088–167.
McGuire S. US Department of Agriculture and US Department of Health and Human Services, Dietary Guidelines for Americans, 2010. Washington, DC: US Government Printing Office, January 2011. Adv Nutr. 2011;2:293–4.
Center for Disease Control and Prevention. Vital signs: food categories contributing the most to sodium consumption-United States, 2007-2008. MMWR Morb Mortal Wkly Rep. 2012;61:92–8.
Grimes CA, Wright JD, Liu K, Nowson CA, Loria CM. Dietary sodium intake is associated with total fluid and sugar-sweetened beverage consumption in US children and adolescents aged 2–18 y: NHANES 2005–2008. Am J Clin Nutr. 2013;98:189–96.
Grimes CA, Bolhuis DP, He FJ, Nowson CA. Dietary sodium intake and overweight and obesity in children and adults: a protocol for a systematic review and meta-analysis. Syst Rev. 2016;5:1.
Byker CJ, Pinard CA, Yaroch AL, Serrano EL. New NSLP guidelines: challenges and opportunities for nutrition education practitioners and researchers. J Nutr Educ Behav. 2013;45:683–9.
Henry JE, Taylor CL. Strategies to reduce sodium intake in the United States. National Academies Press; 2010.
Vos MB, Kaar JL, Welsh JA, Van Horn LV, Feig DL, Anderson CAM, et al. Added sugars and cardiovascular disease risk in children. Circulation 2017;135:e1017–34.
Health UDo, Services H. 2015–2020 Dietary Guidelines for Americans. Washington, DC: US Government Printing Office. 2015.
Wilson C. Obesity: sugar-sweetened beverages--fueling the epidemic of childhood obesity? Nat Rev Endocrinol. 2012;8:696.
Wang J. Consumption of added sugars and development of metabolic syndrome components among a sample of youth at risk of obesity. Appl Physiol, Nutr, Metab. 2014;39:512–512.
Johnson RK. Reducing intakes of sugar sweetened beverages is vital to improving our nation’s health. Circulation 2016;133:347–9.
Ford MC, Gordon NP, Howell A, et al. Obesity severity, dietary behaviors, and lifestyle risks vary by race/ethnicity and age in a Northern California cohort of children with obesity. J Obes. 2016;2016::4287976.
Williamson DA, Han H, Johnson WD, Martin CK, Newton RL Jr. Modification of the school cafeteria environment can impact childhood nutrition. Results from the Wise Mind and LA Health studies. Appetite. 2013;61:77–84.
Peirson L, Fitzpatrick-Lewis D, Morrison K, et al. Prevention of overweight and obesity in children and youth: a systematic review and meta-analysis. CMAJ Open. 2015;3:E23–33.
Sharma M. Dietary education in school-based childhood obesity prevention programs. Adv Nutr. 2011;2:207S–216S.
Madsen KA. Effect of the healthy schools program on prevalence of overweight and obesity in California schools, 2006–2012. Prev Chronic Dis. 2015;12:E77.
Williamson DA, Champagne CM, Harsha DW, et al. Effect of an environmental school-based obesity prevention program on changes in body fat and body weight: a randomized trial. Obesity (Silver Spring). 2012;20:1653–61.
Williamson DA, Champagne CM, Harsha D, et al. Louisiana (LA) Health: design and methods for a childhood obesity prevention program in rural schools. Contemp Clin Trials. 2008;29:783–95.
Melancon KD, J. Popular diets for treatment of overweight and obesity. In: Wadden TS, AJ., editor. Handbook of obesity treatment. New York: Guilford; 2002. p. 249–82.
Child Nutrition and WIC Reauthorization Act of 2004. 2004.
Louisiana Laws. Foods and beverages other than school breakfast or lunch in public elementary and secondary schools; legislative findings; restrictions. Louisiana: Louisiana Laws; 2005.
Williamson DA, Allen HR, Martin PD, Alfonso AJ, Gerald B, Hunt A. Comparison of digital photography to weighed and visual estimation of portion sizes. J Am Diet Assoc. 2003;103:1139–45.
Williamson D, Allen H, Martin PD, Alfonso A, Gerald B, Hunt A. Digital photography: a new method for estimating food intake in cafeteria settings. Eat Weight Disord Stud Anorex, Bulim Obes. 2004;9:24–28.
Martin CK, Newton RL Jr., Anton SD, et al. Measurement of children’s food intake with digital photography and the effects of second servings upon food intake. Eat Behav. 2007;8:148–56.
Martin CK, Correa JB, Han H, et al. Validity of the remote food photography method (RFPM) for estimating energy and nutrient intake in near real‐time. Obesity. 2012;20:891–9.
Martin CK, Nicklas T, Gunturk B, Correa JB, Allen HR, Champagne C. Measuring food intake with digital photography. J Human Nutr Diet. 2014;27(Suppl 1):72–81.
Williamson DA, Copeland AL, Anton SD, et al. Wise Mind Project: a school-based environmental approach for preventing weight gain in children. Obesity. 2007;15:906–17.
Ding D, Lawson KD, Kolbe-Alexander TL, et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet. 2016;388:1311–24.
Johnson RK, Appel LJ, Brands M, et al. Dietary sugars intake and cardiovascular health a scientific statement from the American Heart Association. Circulation. 2009;120:1011–20.
Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98:1084–102.
Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009;123:e661–e667.
Fiorito LM, Marini M, Francis LA, Smiciklas-Wright H, Birch LL. Beverage intake of girls at age 5 y predicts adiposity and weight status in childhood and adolescence. Am J Clin Nutr. 2009;90:935–42.
Forshee RA, Anderson PA, Storey ML. Sugar-sweetened beverages and body mass index in children and adolescents: a meta-analysis. Am J Clin Nutr. 2008;87:1662–71.
Martin CK, Thomson JL, LeBlanc MM, et al. Children in school cafeterias select foods containing more saturated fat and energy than the Institute of Medicine recommendations. J Nutr. 2010;140:1653–60.
Williamson DA, Han H, Johnson WD, Stewart TM, Harsha DW. Longitudinal study of body weight changes in children: who is gaining and who is losing weight. Obesity (Silver Spring). 2011;19:667–70.
Briefel RR, Crepinsek MK, Cabili C, Wilson A, Gleason PM. School food environments and practices affect dietary behaviors of US public school children. J Am Diet Assoc. 2009;109:S91–S107.
Ribeiro R, Alves L. Comparison of two school-based programmes for health behaviour change: the Belo Horizonte Heart Study randomized trial. Public Health Nutr. 2013;26:1–10.
Frieden TR. Sodium reduction—saving lives by putting choice into consumers’ hands. JAMA. 2016;316:579–80.
U.S. Department of Health and Human Services. (2010). Healthy People 2020. Retrieved from www.healthypeople.gov.
Federal Register. Food labelling: revision of nutrition and supplent facts labels. Final rule. Federal Register. 2016;81:33741–999.
Te ML, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2013;346:e7492.
Ventura AK, Worobey J. Early influences on the development of food preferences. Curr Biol. 2013;23:R401–R408.
Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101(Supplement 2):539–49.
Drewnowski A, Mennella JA, Johnson SL, Bellisle F. Sweetness and food preference. J Nutr. 2012;142:1142S–1148S.
Drewnowski A. Taste preferences and food intake. Annu Rev Nutr. 1997;17:237–53.
Poti JM, Slining MM, Popkin BM. Solid fat and added sugar intake among US children: The role of stores, schools, and fast food, 1994–2010. Am J Prev Med. 2013;45:551–9.
Piernas C, Ng SW, Popkin B. Trends in purchases and intake of foods and beverages containing caloric and low-calorie sweeteners over the last decade in the United States. Pediatr Obes. 2013;8:294–306.
Alaimo K, Beavers AW, Crawford C, Snyder EH, Litt JS. Amplifying health through community gardens: a framework for advancing multicomponent, behaviorally based neighborhood interventions. Curr Environ Health Rep. 2016;3:302–12.
Burgess-Champoux, Teri L. PhD, RD, LD and Sullivan, Mandy, “Community gardens involving young children as a potential obesityprevention strategy: A systematic review to inform future research and practice” (2013). Sr. Seraphim Gibbons Undergraduate Symposium. 50. http://sophia.stkate.edu/undergraduate_research_symposium/2013/Sciences/50
Williamson DA, Han H, Johnson WD, Martin CK, Newton RL. Modification of the school cafeteria environment can impact childhood nutrition. Results from the Wise Mind and LA Health studies. Appetite. 2013;61:77–84.
Acknowledgements
The LA Health project was supported by the National Institutes of Health grant R01 HD048483 and the US Department of Agriculture grant 58-6435-4-90. This work was also partially supported by the NORC center grant #1P30 DK072476 entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by the NIDDK. KRH is supported by NIH grant T32 DK064584. JHB was funded in part 1 U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center.
Author’s contributions
DAW conceptualized and designed the study, conducted the research, reviewed and revised the manuscript, and approved the final manuscript as written. KRH analyzed the data, wrote the paper, and had primary responsibility for final content. JHB carried out all analysis, reviewed and revised the manuscript, and approved the final manuscript as written. CKM conducted the research, reviewed and revised the manuscript, had primary responsibility for final content, and approved the final manuscript as written. JWA and JLT reviewed and revised the manuscript, and approved the final manuscript as written.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hawkins, K.R., Burton, J.H., Apolzan, J.W. et al. Efficacy of a school-based obesity prevention intervention at reducing added sugar and sodium in children’s school lunches: the LA Health randomized controlled trial. Int J Obes 42, 1845–1852 (2018). https://doi.org/10.1038/s41366-018-0214-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0214-y
- Springer Nature Limited
This article is cited by
-
Obesity Management Solutions in Rural Communities
Current Cardiovascular Risk Reports (2023)
-
Review of the validity and feasibility of image-assisted methods for dietary assessment
International Journal of Obesity (2020)