Abstract
Background
Overweight is shown to track (= to maintain a relative position in a distribution) from childhood to adulthood, but is mostly studied in preobesogenic cohorts and in single ethnic groups. Little is known about tracking of thinness by ethnicity.
Objectives
to determine (differences in) tracking of BMI (class) from 3 through 15 years and the prediction of BMI class at 13–15 years of age in contemporary Dutch, Turkish, Moroccan and South Asian children living in the Netherlands.
Methods
Historical cohort of 7625 children, born 1994–1997, with 24,376 measurements of BMI. BMI z-score and BMI class was analysed using universal criteria. South Asian children were also assessed using ethnic specific BMI criteria. Diagnostic odds ratios (OR) and test properties were calculated to estimate the ability of BMI class at 3–4 years to predict BMI class at 13–15 years.
Results
Tracking of thinness between 3 and 15 years was stronger than that of overweight, as indicated by a generally higher diagnostic OR. BMI trajectories between 3 and 15 years of age of thin, normal weight and overweight adolescents were, although significantly different, quite similarly shaped in children of Dutch, Turkish and Moroccan descent. The South Asian BMI trajectory deviated considerably from the other ethnic groups, but the differences disappeared when South Asian specific BMI criteria were applied. A substantial proportion of overweight developed between 5–10 years, after which less children shifted to other BMI classes. A total of 55–78% of children with overweight at 3–4 years retained their overweight at 13–15 years, and 10–20% of 3–4 year olds with thinness remained thin.
Conclusions
In all ethnic groups, overweight and especially thinness highly tracked into adolescence. South Asian children differed from the other ethnic groups when universal BMI criteria were applied, but with South Asian specific BMI criteria tracking patterns became more concordant.
Similar content being viewed by others
Introduction
In the past decades childhood obesity has grown into a true pandemic that poses a major public health threat in affected populations [1, 2] because of the associated cardiometabolic health risks [3]. Although there are several prevention programmes for overweight and obesity, the significant changes in body mass index (BMI, weight/height [2]) or other measures of nutritional status after a life style intervention are generally small and improvements are often not sustained in the long term [4, 5]. Nevertheless, in several developed countries the prevalence of overweight has been shown to stabilise [6, 7]. In the Netherlands in most ethnic groups the rates of overweight and obesity seem to be levelling off. There has even been a decrease found in Dutch children (of European descent) in the prevalence of overweight and obesity since 1999 [8]. The exact causes of the stabilising and declining trends in overweight or obesity rates in Dutch children are unclear, but may perhaps be attributed to the increased public awareness as well as to the many prevention programmes and interventions that have been implemented throughout the Netherlands in the past decade [9].
However, as BMI and overweight have been shown to track (=1 to maintain a relative position in the (BMI) distribution over time, or 2 the ability to predict future values from a previous measurement or classification) [10] from childhood into adulthood [11,12,13] the obesity epidemic may not be over.
Most of the studies investigating ‘tracking of overweight’ involved populations born in a preobesogenic era, when obesity rates were much smaller. Therefore, in contemporary populations, exposed to an obesogenic environment from birth, the tracking pattern may be different [14], i.e. they might gain more fat from an earlier age, and consequently show a steeper increase in BMI than previous generations. For prevention strategies and interventions to be most effective, it is important to determine which groups are at greatest risk for developing obesity and related diseases. When the natural history of the development of overweight and associated health risks is known, interventions can be targeted particularly at those high-risk groups.
Many cohort studies already showed that birth weight is related to cardiometabolic disease later in life. Most of these studies found an inverse linear relation: the lower a baby’s birth weight, the higher the risk of cardiometabolic disease [15, 16]. Some other studies reported a U-shaped relation between birth weight and cardiometabolic disease, indicating for both the lower and the higher end of the birth weight range an increased risk of cardiometabolic disease in adult life, compared with those that were born average or in the ‘normal’ range [17, 18].
Also, BMI at a young age was shown to be independently (from birth weight) related to cardiovascular disease in adulthood [15]. In the Netherlands, a cohort study of young adults born in 1977–1986 showed that the BMI increase in the age period 2–6 years was the strongest predictor of adult overweight [19], as well as of cardiovascular and metabolic risks in adulthood [20]. Other studies showed that children with rapid growth in weight or BMI during infancy or children that were obese during infancy had a higher risk of developing obesity at subsequent ages [21]. For contemporary generations it is currently unknown in the Netherlands how strong BMI tracks during childhood and to what degree overweight during earlier ages is predictive of overweight at an older age. Considering the large differences in prevalence of obesity among ethnic groups in the Netherlands [8], tracking patterns are likely to be different between ethnic groups, as was previously demonstrated in the USA [22]. Further reports comparing tracking of overweight in various ethnic groups are scarce. Also, little is known about tracking of thinness in general, and in different ethnic groups living in developed countries in particular.
In the Netherlands, children of South Asian descent have received increased attention from youth health care nurses and physicians, and other public health workers such as health promotion professionals. This is not only because South Asian children have a generally higher risk of cardiometabolic disease compared with populations of European descent [23, 24], but also because the BMI distribution and the relation between BMI and fat mass was shown to be different from other ethnic groups [25, 26].
The aim of this study is to investigate ethnic differences in tracking of BMI and BMI class between children of Dutch, Turkish, Moroccan and South Asian descent from 3 through 15 years of age.
Methods
Data collection
In the Netherlands, all children are invited periodically for a general health assessment by a Youth Health Care nurse or physician, as part of the national child health surveillance programme. Children between 3 and 15 years of age are invited four times for a voluntary health assessment. Participation rates are generally high (80–90%) [27]. Incompleteness of health records can generally be attributed to non-participance and the moving of families into and out of the city during the follow-up period.
The Youth Health Care organisation of the city of The Hague (the Netherlands) has kept a digital record system since 1998 in which details of the preventive health assessments of all children are registered. For this study, growth data on height and weight, and background data such as sex, date of birth, the child’s surname and parental country of birth were extracted from the digital records of a cohort of children born 1994–1997. Height and weight data of all standard health assessments at the ages of 3–4, 5–6, 7–10 and 13–15 years of age were subsequently selected. Data from younger ages were not available. Measurements were taken between January 1998 and November 2013. All children with a measurement at 13–15 years of age and at least one measurement at a younger age were included in the study.
As this study involved the analysis of routinely collected data, under Dutch law ethical consent was not needed [28], provided that regulations regarding privacy are met. Therefore, after determining ethnicity and age, identifying personal information was removed from the research database.
Ethnic groups
In the Netherlands, the largest ethnic minority groups, i.e. people of Turkish, Moroccan and South Asian descent have lived in the Netherlands for up to three generations. Therefore, country of birth is insufficient to determine the ethnic origin in descendants of the second and third generation. To be able to appropriately assign the correct ethnic origin to the members of the cohort, ethnicity was first based on country of birth of both parents. If the mother and father were both born outside the Netherlands but in different countries, the country of birth of the mother prevailed. If one of the parents was born in the Netherlands and the other outside the Netherlands, the country of birth of the non-Dutch parent determined the ethnicity of the child. In cases where both parents were born in the Netherlands the child’s surname was matched with lists of typically Dutch, Turkish and Moroccan surnames to distinguish native Dutch parents from Dutch second generation Turkish and Moroccan parents (of whom parents were born in the Netherlands but grandparents in Turkey or Morocco). As most South Asians in the Netherlands originate from the former Dutch colony Suriname, South Asian ethnicity was determined both by parental country of birth (Suriname) and the presence of a typically (Surinamese) South Asian surname of the child.
Anthropometric measurements and cut-off values
Height and weight of children were measured by trained youth health care physicians, nurses and physician’s assistants; height with a stadiometer (Seca 202; Hamburg, Germany) or height measuring tape (Seca 206 or equivalent), rounded to the nearest 0.1 cm and weight with a calibrated mechanical step scale (Seca 761 or equivalent), rounded to the nearest 0.5 kg. Up till the age of 7 years, children were measured in underclothes and from that age in light clothes without shoes.
Body mass index was calculated with the formula [weight in kg]/[height in metres] [2]. BMI z-scores and BMI categories were calculated with the latest international BMI references and cut-offs for children [29]. BMI categories were determined with the z-scores that correspond to the adult BMI cut-offs of < 17 kg/m2 for thinness, ≥ 17 but < 25 kg/m2 for normal weight, and ≥ 25 kg/m2 for overweight (including obesity). A recently developed South Asian specific BMI reference for South Asian children in the Netherlands, including a new BMI classification [30], was also used but only for South Asian children. This reference was based on the BMI distribution of a population of South Asian children in the Netherlands born in a preobesogenic era with BMI cut-offs for thinness corresponding to a BMI of <15 kg/m2 at 18 years of age, and cut-offs for overweight to a BMI of ≥23 kg/m2 at 18 years of age [30].
Statistical analyses
The term tracking is firstly used to describe a variable’s longitudinal development and the maintenance of a relative position or ranking of the variable within the variable’s distribution. Second, tracking involves the ability to predict subsequent measures from previous measures [10]. For this article these two concepts of tracking were studied using BMI z-scores and the BMI classification (thinness, normal weight and overweight).
All variables were tested for normality. The longitudinal development of the mean BMI z-score (=dependent) over time was analysed by ethnic group and age group with a linear mixed-effects model (repeated measures). Sex was added to the model as a potential confounder. Estimated Marginal Mean BMI z-scores were calculated by ethnic group and age group from the fitted model while adjusting for the other variables in the model.
The longitudinal development of the mean BMI z-score was determined for each BMI class at 13–15 years and tested with a linear mixed-effects model (repeated measures) analysis, with the BMI z-score of each BMI class as dependent factor, and age, sex and ethnic group as covariates. Trends in the prevalence of overweight (vs no overweight) or thinness (vs no thinness) by age were tested with a generalised estimating equations logistic model, as this model takes the correlation between repeated measures into account. Additionally, when overweight or thinness status at a younger age considered a test for overweight or thinness respectively at 13–15 years of age, the test properties (sensitivity, specificity, positive predictive value) were calculated for ages 3–4, 5–6 and 7–10 years by ethnic group. The 95% confidence interval (CI) was determined by calculating the Wilson score interval with continuity correction [31, 32].
As test of discriminatory performance the diagnostic odds ratio (diagnostic OR with 95% Confidence interval) was calculated for every age group by ethnicity. This single indicator combines sensitivity and specificity (which are not easily interpreted when comparing tests) and is independent of the prevalence [33]. The resulting odds ratio represents the ratio of the odds of the test being positive if the child has the condition (overweight/thinness), divided by the odds of the test being positive if the child does not have the condition. When tracking is strong this will result in a higher diagnostic OR than when tracking is less strong.
The statistical significance level was set at P < 0.05 (two-sided). IBM SPPS Statistics v22 software was used for all statistical tests.
Results
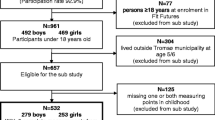
In this study, 7625 children were included, with a total of 25,604 registered measurements. Figure 1 shows the numbers of performed health checks at each age of the cohort. Though the study population involved a dynamic cohort participating in a routine health surveillance programme 51% of all included children had all four, and 33% had three follow-up check-ups registered. The population characteristics were similar between the ethnic groups (Table 1).
Prevalence of overweight and thinness
The highest prevalence of overweight was found in children of South Asian descent (ethnic specific reference) followed by children of Turkish, Moroccan and Dutch descent (Table 2). Overweight rates significantly increased with age in all ethnic groups (P < 0.001), with the largest increase between 5–6 and 7–10 years of age. The prevalence of thinness was generally very low in all ethnic groups, except in children of South Asian descent (universal BMI cut-offs) (Table 3). When South Asian specific BMI cut-offs were applied thinness prevalences were concordant with those found in the other ethnic groups.
Tracking: the maintenance of a relative position of BMI
The trajectory of the estimated marginal mean (EMM = the mean value, adjusted for repeated measures and the other variables in the model) BMI z-score by age group (Fig. 2) differed between the ethnic groups (P < 0.001). Within each ethnic group there were no significant differences in BMI z-score between males and females. Children of Turkish descent had the highest BMI z-score at every age, ranging from a z-score of 0.4 at 3–4 years of age up till a z-score of 1.0 at 13–15 years. For children of Dutch, Moroccan and Turkish descent the overall BMI z-score followed a similar pattern between 3 and 15 years of age: between 3 and 6 years the mean BMI z-score remained fairly stable, increased between 5–6 and 7–10 years, and reached a plateau from that age.
The BMI trajectory of children of South Asian descent deviated considerably when based on the universal BMI reference. The BMI z-scores in this group were very low until 5–6 years of age (−0.7 to −0.3), increased sharply between 5–6 and 7–10 years by 0.7 SD, and from then on remained fairly stable. However, when applying the South Asian specific reference the BMI z-score trajectory was more concordant with the other ethnic groups, following a BMI trajectory between that of children of Turkish and Moroccan descent.
The BMI z-score trajectory of thin, normal weight and overweight 13–15-year-old adolescents shows how on average the final BMI z-score was reached from the age of 3–4 years (Fig. 3). No differences were found between the sexes within each ethnic group by BMI class. The BMI z-score trajectories of overweight adolescents of Dutch, Moroccan and Turkish descent, although statistically significantly different (P < 0.001), followed similar patterns. For thin and normal weight adolescents of these ethnic groups, the BMI trajectory showed more variation (P < 0.001), but also here the trend of the pattern was quite similar. In general, thin children at age 13–15 years had been already relatively thin (<−0.9 SD) in earlier years, whereas normal weight adolescents had a mean BMI z-score that started at 3–4 years around a value of 0 and remained largely stable. Overweight adolescents on average had already considerably higher mean BMI z-scores at younger ages (around + 1 SD), that increased by 0.8–0.9 SD between 3–4 years and 13–15 years of age.
The BMI trajectory of thin, normal weight and overweight children of South Asian descent, when based on the universal BMI reference, deviated considerably with a sharp increase in BMI z-scores from 3–4 up to 7–10 years of age, both in normal weight and overweight 13–15 year olds. When applying the South Asian specific reference the BMI tracking pattern in this group was again largely consistent with the pattern found in the other ethnic groups.
Prediction of BMI class by testing BMI class at a younger age
When the presence of overweight (vs. no overweight) or thinness (vs no thinness) at a younger age is considered a positive test for overweight or thinness at 13–15 years, respectively, test properties such as sensitivity, specificity, positive predictive value and diagnostic odds ratio (Tables 2 and 3) are informative of the predictive ability of the BMI class (overweight yes/no; thinness yes/no) at a younger age to predict overweight or thinness at 13–15 years, respectively. Low values (<90%) of one of the test properties sensitivity or specificity indicate that children with thinness or overweight at a younger age shifted to another BMI class at 13–15 years of age. A high-positive predictive value means that a high percentage of children with overweight (thinness) at a younger age remain overweight (thin) at 13–15 years. The diagnostic OR shows the degree of tracking with higher values signifying a stronger tracking compared to lower diagnostic OR.
When taking South Asian children (ethnic specific criteria) as an example and overweight at the age of 3–4 years as a test for overweight at 13–15 years, we see that the sensitivity is 47%, which means that 47% of the South Asian children classified as having overweight as 13–15-year-old did also have overweight at the age of 3–4 years. The found specificity of 87% at this age means that 87% of South Asian children classified as having no overweight at 13–15 years did also not have overweight at 3–4 years. In the other ethnic groups the sensitivity was even lower, which signifies that most children with overweight at 13–15 years developed overweight at an older age. But as expected, the sensitivity increases by age, indicating a larger proportion maintaining their overweight. The high specificities of overweight at ages 3–4, 5–6 and 7–10 years in South Asian children (and in the other ethnic groups) means that most children without overweight as 13–15-year-old did not have overweight at a younger age. On the other hand, the high positive predictive value of 71–77% at ages 3–10 in South Asian children (ethnic specific criteria) indicates that, once overweight is present at a younger age, in 71–77% of cases their overweight is maintained up till 13–15 years of age.
In addition, a statistically significant diagnostic OR > 1 means that there is tracking. The higher the diagnostic OR the better the test (overweight or thinness at a younger age) predicts overweight or thinness at 13–15 years of age. The highest diagnostic OR’s for overweight were found for overweight at 7–10 years in all ethnic groups, ranging between 23 and 31. For thinness the OR’s were considerably higher, even up to a value of 319 in Turkish 7–10 year olds, indicating a strong ability of thinness at the age of 7–10 years to predict thinness at 13–15 years of age.
Discussion
Main findings
In this study two concepts of tracking were studied. First, the longitudinal development of BMI over time, and second the predictive ability of the BMI class at a younger age for thinness and overweight as 13–15 year olds. Children of Dutch, Turkish and Moroccan descent showed, although significantly different, quite similar tracking patterns of BMI z-score and BMI classes from 3 through 15 years of age. The longitudinal development of BMI in children of South Asian descent, when based on universal BMI criteria, showed large discrepancies compared with other ethnic groups, which disappeared to a great extent when South Asian specific BMI criteria were applied. In all ethnic groups the presence of overweight and especially thinness at 3–4 years of age highly tracked into adolescence, although a considerable proportion of thinness and overweight at 13–15 years developed after that age.
Strengths of this study are the large sample size, the longitudinal and population-based design, the inclusion of children from different ethnic groups, and measurements performed by trained professionals. Another strength is the high follow-up rate. Although this study was designed as a descriptive study of tracking of BMI in different ethnic groups, the addition of parental educational level (socioeconomic status) or parental BMI to the model could have had added value to explain potential ethnic differences. Unfortunately, as routine registration data were used for the study, such covariates were not available.
Meaning of findings and practical implications
This study found considerable ethnic differences in thinness and overweight rates by age. Previous Dutch cross-sectional growth studies already showed that children of Turkish and Moroccan descent had a considerably higher prevalence of overweight and obesity than children of Dutch descent [34, 35]. The current rates of overweight in Turkish and Moroccan adolescents of our cohort are comparable to those found in the latest study [34]. South Asian children had the highest thinness prevalence of 16% at 3–4 years of age and also the lowest overweight rate at that age (8%) when based on the universal BMI criteria. However, when applying South Asian specific BMI cut-offs (based on the BMI of an affluent cohort of South Asian children born before the obesity epidemic), the thinness rates were concordant with those found in other ethnic groups, but simultaneously the overweight prevalence increased to the highest level of all ethnic groups, 27% at 3–4 years up to 45% at 7–10 years. This indicates that in this ethnic group universal BMI cut-offs highly overestimate thinness and underestimate overweight rates [25]. Although previously, an expert panel from the UK did not yet recommend separate BMI definitions for South Asian children and adolescents [36], our findings support the use of South Asian specific BMI criteria.
Based on diagnostic odds ratios, thinness tracked generally stronger than overweight. Other studies also found a strong tracking of thinness from childhood to adolescence [37, 38]. An explanation is that these thin children represent the lower end of the normal BMI distribution. As BMI during infancy and childhood was shown to be highly correlated with lean body mass in adolescence and adulthood, and not with fat mass [39, 40], thin children of our study are likely to have a predisposition for a smaller lean body mass.
The very high prevalence of overweight at age 3 in children of Turkish, Moroccan and South Asian descent (17–27%) implies that factors before that age are also important determinants of overweight. A recent Dutch study showed that weight gain in the first 6 months of life and maternal pre-pregnancy BMI explained most of the differences in overweight rates between 2-year-old children of Turkish, Moroccan and Dutch descent [41]. In the current study, overweight prevalence remained fairly stable from 3 to 6 years in all ethnic groups, followed by a considerable increase, and a plateau in the overweight prevalence from the age of 7–10 years.
Previously, overweight at the age of 9–11 years was shown to track into adulthood [42]. However, many adults with overweight were not affected by overweight as a child. In the Netherlands, the prevalence of adult overweight is currently levelling off but the rates are considerably higher than in Dutch adolescents of our study. In 2015 almost 29% of 20–30-year-old Dutch adults were affected by overweight and 42% of 30–40 year olds [43]. It is likely that a large proportion of adolescents with overweight will maintain their overweight, but most overweight in this group is likely to develop during late adolescence and adulthood [44]. Those who ultimately will be affected by overweight as an adult is still difficult to exactly predict and likely depends on many life style factors and personal circumstances.
In all ethnic groups a considerable proportion of 3–4 year olds already had overweight, and most of these children maintained their overweight as an adolescent (positive predictive values of 55–78%), indicating that once children have become overweight it is difficult to gain a ‘normal weight’. It is likely that many of these children will become adults with overweight together with an increased risk of cardiometabolic disease compared with those that remain normal weight [20, 45, 46]. Especially children of South Asian descent are at increased risk of cardiometabolic disease [47]. Considering the extremely high overweight rates and the strong tracking of overweight in this group, this group should be specifically targeted for (preventive) interventions. In general, preventive interventions should preferably start at a young age, possibly already during the first year of life. And because of the increase in overweight prevalence between the age of 5–6 years and 7–10 years, also 3–10 year olds should be targets of preventive activities. Furthermore, for a proper assessment of BMI in children of South Asian descent, ethnic specific criteria are recommended.
Conclusion
In this study, the mean BMI z-score of both overweight and thin children of all studied ethnic groups followed a similar pattern between 3 and 15 years of age (provided that South Asian specific BMI criteria were applied). The different tracking pattern found in children of South Asian descent compared with the other ethnic groups raises doubts over the use of universal BMI criteria for all ethnic groups. Although at 3–4 years of age already a large proportion of children of Turkish, Moroccan and South Asian descent had overweight, between 5 and 10 years many children gained overweight, stabilising from the age of 10 years. Once a child is affected by overweight, in most cases this is maintained during adolescence. These findings may enable health care providers to early intervene in children at increased risk of developing or maintaining overweight or obesity, especially children of South Asian descent. Preventive interventions and strategies should preferably start during infancy and continue throughout childhood.
References
Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–82.
Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25.
Friedemann C, Heneghan C, Mahtani K, Thompson M, Perera R, Ward AM. Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ. 2012;345:e4759.
Flynn MA, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’ recommendations. Obes Rev. 2006;7(Suppl 1):7–66.
Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011: CD001871.
Olds T, Maher C, Zumin S, Peneau S, Lioret S, Castetbon K, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes. 2011;6:342–60.
Rokholm B, Baker JL, Sorensen TI. The levelling off of the obesity epidemic since the year 1999--a review of evidence and perspectives. Obes Rev. 2010;11:835–46.
de Wilde JA, Verkerk PH, Middelkoop BJ. Declining and stabilising trends in prevalence of overweight and obesity in Dutch, Turkish, Moroccan and South Asian children 3-16 years of age between 1999 and 2011 in the Netherlands. Arch Dis Child. 2014;99:46–51.
Schonbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, Hirasing RA, et al. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PLoS ONE. 2011;6:e27608.
Foulkes MA, Davis CE. An index for tracking of longitudinal data. Biometrics. 1981;37:439–46.
Aarestrup J, Bjerregaard LG, Gamborg M, Angquist L, Tjonneland A, Overvad K, et al. Tracking of body mass index from 7 to 69 years of age. Int J Obes. 2016;40:1376–83.
Magarey AM, Daniels LA, Boulton TJ, Cockington RA. Predicting obesity in early adulthood from childhood and parental obesity. Int J Obes Relat Metab Disord. 2003;27:505–13.
Power C, Lake JK, Cole TJ. Body mass index and height from childhood to adulthood in the 1958 British born cohort. Am J Clin Nutr. 1997;66:1094–101.
Singh AS, Mulder C, Twisk JW, van MW, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–88.
Andersen LG, Angquist L, Eriksson JG, Forsen T, Gamborg M, Osmond C, et al. Birth weight, childhood body mass index and risk of coronary heart disease in adults: combined historical cohort studies. PLoS ONE. 2010;5:e14126.
Whincup PH, Kaye SJ, Owen CG, Huxley R, Cook DG, Anazawa S, et al. Birth weight and risk of type 2 diabetes: a systematic review. JAMA. 2008;300:2886–97.
Gunnarsdottir I, Birgisdottir BE, Thorsdottir I, Gudnason V, Benediktsson R. Size at birth and coronary artery disease in a population with high birth weight. Am J Clin Nutr. 2002;76:1290–4.
Harder T, Rodekamp E, Schellong K, Dudenhausen JW, Plagemann A. Birth weight and subsequent risk of type 2 diabetes: a meta-analysis. Am J Epidemiol. 2007;165:849–57.
de Kroon ML, Renders CM, van Wouwe JP, van Buuren S, Hirasing RA. The Terneuzen birth cohort: BMI changes between 2 and 6 years correlate strongest with adult overweight. PLoS ONE. 2010;5:e9155.
de Kroon ML, Renders CM, van Wouwe JP, van Buuren S, Hirasing RA. The Terneuzen Birth Cohort: BMI change between 2 and 6 years is most predictive of adult cardiometabolic risk. PLoS ONE. 2010;5:e13966.
Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;331:929.
Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Racial differences in the tracking of childhood BMI to adulthood. Obes Res. 2005;13:928–35.
Whincup PH, Gilg JA, Papacosta O, Seymour C, Miller GJ, Alberti KG, et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ. 2002;324:635.
Misra A, Khurana L. Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes. 2011;35:167–87.
de Wilde JA, Zandbergen-Harlaar S, van Buuren S, Middelkoop BJ. Trends in body mass index distribution and prevalence of thinness, overweight and obesity in two cohorts of Surinamese South Asian children in The Netherlands. Arch Dis Child. 2013;98:280–5.
Hudda MT, Nightingale CM, Donin AS, Fewtrell MS, Haroun D, Lum S, et al. Body mass index adjustments to increase the validity of body fatness assessment in UK Black African and South Asian children. Int J Obes. 2017;41:1048–55.
de Wilde JA, van Dommelen P, Middelkoop BJ, Verkerk PH. Trends in overweight and obesity prevalence in Dutch, Turkish, Moroccan and Surinamese South Asian children in the Netherlands. Arch Dis Child. 2009;94:795–800.
Netherlands. Medical Research Involving Human Subjects Act. Bull Med Ethics. 1999;152:13-8.
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284–94.
de Wilde JA, van Dommelen P, Middelkoop BJ. Appropriate body mass index cut-offs to determine thinness, overweight and obesity in South asian children in the Netherlands. PLoS ONE. 2013;8:e82822.
Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–72.
Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;22:209–12.
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PMM. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56:1129–35.
van Dommelen P, Schonbeck Y, HiraSing RA, van Buuren S. Call for early prevention: prevalence rates of overweight among Turkish and Moroccan children in The Netherlands. Eur J Public Health. 2015;25:828–33.
Fredriks AM, van Buuren S, Sing RA, Wit JM, Verloove-Vanhorick SP. Alarming prevalences of overweight and obesity for children of Turkish, Moroccan and Dutch origin in The Netherlands according to international standards. Acta Paediatr. 2005;94:496–8.
Viner RM, Cole TJ, Fry T, Gupta S, Kinra S, McCarthy D, et al. Insufficient evidence to support separate BMI definitions for obesity in children and adolescents from south Asian ethnic groups in the UK. Int J Obes. 2010;34:656–8.
Ge S, Kubota M, Nagai A, Mamemoto K, Kojima C. Retrospective individual tracking of body mass index in obese and thin adolescents back to childhood. Asia Pac J Clin Nutr. 2011;20:432–7.
Julia M,Van Weissenbruch MM,Prawirohartono EP,Surjono A,Delemarre-van de Waal HA, Tracking for underweight, overweight and obesity from childhood to adolescence: a 5-year follow-up study in urban Indonesian children. Horm Res. 2008;69:301–6.
Sachdev HS, Fall CH, Osmond C, Lakshmy R, Dey Biswas SK, Leary SD, et al. Anthropometric indicators of body composition in young adults: relation to size at birth and serial measurements of body mass index in childhood in the New Delhi birth cohort. Am J Clin Nutr. 2005;82:456–66.
Johnson W, Choh AC, Lee M, Towne B, Czerwinski SA, Demerath EW. Is infant body mass index associated with adulthood body composition trajectories? An exploratory analysis. Pediatr Obes. 2017;12:10–18.
de Hoog ML, van Eijsden M, Stronks K, Gemke RJ, Vrijkotte TG. Overweight at age two years in a multi-ethnic cohort (ABCD study): the role of prenatal factors, birth outcomes and postnatal factors. BMC Public Health. 2011;11:611.
Deshmukh-Taskar P, Nicklas TA, Morales M, Yang SJ, Zakeri I, Berenson GS. Tracking of overweight status from childhood to young adulthood: the Bogalusa Heart Study. Eur J Clin Nutr. 2006;60:48–57.
Statistics Netherlands. Length and weight of persons, underweight and overweight; from 1981. The Netherlands:The Hague/Heerlen; 2016.
Buscot MJ, Wotherspoon SS, Magnussen CG, Juonala M, Sabin MA, Burgner DP, et al. Bayesian hierarchical piecewise regression models: a tool to detect trajectory divergence between groups in long-term observational studies. BMC Med Res Methodol. 2017;17:86.
Allcock DM, Gardner MJ, Sowers JR. Relation between childhood obesity and adult cardiovascular risk. Int J Pediatr Endocrinol. 2009;2009:108187.
Umer A, Kelley GA, Cottrell LE, Giacobbi P Jr., Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health. 2017;17:683.
Nightingale CM, Krishnaveni GV, Rudnicka AR, Owen CG, Veena SR, Hill JC, et al. Cardiometabolic risk markers in Indian children: comparison with UK Indian and white European children. PLoS ONE. 2012;7:e36236.
Acknowledgements
We thank Ron Smit and Marion Groeneveld for their help in retrieving the required data from the youth health care database.
Authors contribution
JAdW, BJCM and PHV conceived the idea for the study. JAdW managed and analysed the data. All authors were involved in writing the paper, and approved of the submitted and published version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
de Wilde, J., Middelkoop, B. & Verkerk, P. Tracking of thinness and overweight in children of Dutch, Turkish, Moroccan and South Asian descent from 3 through 15 years of age: a historical cohort study. Int J Obes 42, 1230–1238 (2018). https://doi.org/10.1038/s41366-018-0135-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0135-9
- Springer Nature Limited
This article is cited by
-
Tracking between cardiovascular-related measures at 4 and 8 years of age in the INMA-Asturias cohort
European Journal of Pediatrics (2023)
-
Looking backwards and forwards: tracking and persistence of weight status between early childhood and adolescence
International Journal of Obesity (2021)
-
Prevalence of Dyslipidemia in Students from Han, Uygur, and Kazakh Ethnic Groups in a Medical University in Xinjiang, China
Scientific Reports (2019)