Abstract
Background/objectives
Obesity is strongly associated with leptin resistance. It is unclear whether leptin resistance results from the (over)consumption of energy-dense diets or if reduced leptin sensitivity is also a pre-existing factor in rodent models of diet-induced obesity (DIO). We here tested whether leptin sensitivity on a chow diet predicts subsequent weight gain and leptin sensitivity on a free choice high-fat high-sucrose (fcHFHS) diet.
Methods
Based upon individual leptin sensitivity on chow diet, rats were grouped in leptin sensitive (LS, n = 22) and leptin resistant (LR, n = 19) rats (P = 0.000), and the development of DIO on a fcHFHS diet was compared. The time-course of leptin sensitivity was measured over weeks in individual rats.
Results
Both on a chow and a fcHFHS diet, high variability in leptin sensitivity was observed between rats, but not over time per individual rat. Exposure to the fcHFHS diet revealed that LR rats were more prone to develop DIO (P = 0.013), which was independent of caloric intake (p ≥ 0.320) and the development of diet-induced leptin resistance (P = 0.769). Reduced leptin sensitivity in LR compared with LS rats before fcHFHS diet exposure, was associated with reduced leptin-induced phosphorylated signal transducer and activator of transcription 3 (pSTAT3) levels in the dorsomedial and ventromedial hypothalamus (P ≤ 0.049), but not the arcuate nucleus (P = 0.558).
Conclusions
A pre-existing reduction in leptin sensitivity determines the susceptibility to develop excessive DIO after fcHFHS diet exposure. Rats with a pre-existing reduction in leptin sensitivity develop excessive DIO without eating more calories or altering their leptin sensitivity.
Similar content being viewed by others
Introduction
The prevalence of obesity has increased dramatically over the last few decades [1]. The majority of human obesity is thought to result from a combination of genetic susceptibility and environmental influences, such as the availability of a variety of energy-dense diets, high in saturated fat and sugar [1, 2]. To model the human situation, rodent models have been developed in which obesity is induced by dietary manipulation, i.e., diet-induced obesity (DIO). Both in humans and rodents, the development and/or maintenance of obesity has been assumed to result from diet-induced leptin resistance [3,4,5,6,7,8,9,10,11,12,13,14].
In normal weight individuals, the brain responds to increased plasma leptin levels by reducing food intake and increasing energy expenditure [15,16,17,18]. Leptin exerts its effects by acting on leptin receptors, which are highly expressed in the arcuate nucleus (ARC) of the hypothalamus, but also in other (extra)hypothalamic brain regions, including the dorsomedial hypothalamus (DMH) [19,20,21]. Most obese individuals show high circulating leptin levels [8,9,10, 13, 14, 17, 22]. After exogenous administration of leptin, obese individuals do not respond with a decrease in food intake that is normally observed in lean individuals, and are hence considered leptin-resistant [5, 7,8,9, 11,12,13, 22,23,24]. At the cellular level, the development of leptin resistance is often demonstrated by an attenuation in the incremental increase or maximal level of leptin-induced phosphorylation of signal transducer and activator of transcript 3 (pSTAT3), a critical transcription factor for leptin’s action [25, 26], in the ARC of rodents [12, 17, 18, 22].
In DIO models, the resistance to leptin is often relative, i.e., a reduced but not complete absent sensitivity to the food intake suppressing effects of exogenous leptin, usually observed at one or a few time-points following leptin injection [7, 12, 15, 16, 23, 24]. However, it is difficult to demonstrate the development of (absolute) leptin resistance, as there is no consensus with respect to the timing of leptin’s food intake suppressing effects. Our systematic review of leptin sensitivity in control diet fed rats indicates that the anorectic effects of leptin range between 2 and 38 h after leptin injection, and the effect sizes vary between 7 and 30% (Table S1). Even studies performed by the same research group showed variable results [7, 11, 12, 15, 23, 27]. So, the well established food intake suppressing effect of leptin is not that straightforward. Interestingly, Ruffin et al. previously reported high variability in leptin sensitivity between rats, and the response to leptin at 2 h food intake on a control diet was related to subsequent weight gain on a high-energy diet (HED) [28]. In addition, Levin et al. showed reduced central leptin sensitivity before HED exposure in rats that were retrospectively identified as DIO prone [29]. So, there is some evidence that reduced leptin sensitivity does not necessarily result from HED feeding, but may already be present before HED exposure and predispose rats to exacerbated DIO. However, in previous studies it remains unclear whether leptin sensitivity is a stable parameter in a rat and therefore to what extent a pre-existing reduction in leptin sensitivity is a predictor for DIO. Furthermore, as leptin sensitivity was only tested before HED exposure, it is currently unknown whether exposure to a HED further reduces the pre-existing reduction in leptin sensitivity in DIO prone rats and thereby aggravates DIO.
Since the response to leptin is quite variable, we here aimed to carefully study leptin sensitivity of individual rats at 1–24 h after leptin injection, and to make a trajectory of leptin sensitivity over weeks in rats that were offered a chow or a free-choice high-fat high-sucrose (fcHFHS) diet. Further, we also tested whether leptin sensitivity on a chow diet predicts subsequent body weight gain on a fcHFHS diet, and how this is related to the development of diet-induced leptin resistance. Leptin sensitivity was assessed by examining both the feeding response to leptin and the associated leptin receptor signal transduction, by using pSTAT3 activation as a marker for cellular leptin sensitivity.
Materials and methods
Systematic review of leptin sensitivity
We searched PubMed for original articles concerning the acute food intake suppressing effects of leptin in rats fed a control diet until February 12, 2017. The full search strategy for PubMed was composed of four elements: leptin injection, diet, rats, and food intake/obesity (for complete search strategy see Table S2). No language restrictions were used. Studies were included in the systematic review if they fulfilled all of the following criteria: (1) the test subject was rat, (2) leptin was administered peripherally, (3) food intake after leptin injection was assessed, (4) a control diet group was included, and (5) the study was an original full text paper (Figure S1). Studies were excluded if: (1) leptin was administered centrally or locally, (2) leptin was administered repeatedly, (3) the result or protocol was unclear, (4) no leptin sensitivity test was performed Study selection was based on title and abstract. In case of doubt, the full text article was evaluated. After selection of all studies that assessed the acute food intake suppressing effect of leptin in rats fed a control diet in a relevant and clear way, a selection of the most common way to test leptin sensitivity was made. Intraperitoneal leptin injection after light phase food restriction was the most common way to test leptin sensitivity, and the timing of leptin’s food intake suppressing effect was only compared between studies that used this protocol. If data were only presented graphically, effect sizes were estimated from the graphs. Only the effects of the control diet group were studied, and all different types of control diet were included.
Animals and dietary intervention
Male Wistar rats (7 weeks old; Charles River, Sulzfeld, Germany) were individually housed in Plexiglas cages in a temperature controlled (21–23 °C) and light controlled (lights on between 0700 and 1900 h) room. Upon arrival, all rats had ad libitum access to pelleted rat chow (3.31 kcal/g; Special Diet Service, UK) and tap water. When the rats had reached a body weight of >300 g, they were implanted with intra-arterial silicone catheters through the right jugular vein, according to the method of Steffens [30]. Four weeks later, rats were equally divided into two diet groups based upon their average body weight, body weight gain, daily caloric intake, and leptin sensitivity in the week before the division. Sample sizes were calculated based on expected effect sizes and variance. One group of control rats remained on chow and tap water over the entire experimental period (n = 21), whereas the other group was subjected to a fcHFHS diet for 8 weeks (n = 20). The fcHFHS diet consisted of a choice between lard (9.1 Kcal/g Ossewit/Blanc de Boeuf, Belgium) and 30% sucrose solution (1.0 M sucrose mixed from commercial grade sugar and tap water), in addition to regular chow and tap water. Subsequently, the chow and fcHFHS diet group were both divided into subgroups of LS and LR rats based upon their leptin sensitivity on chow diet, as described below. Body weight and 24-hour food intake were measured 5 days per week. All experiments were performed in accordance with Dutch laws (Wet op de Dierproeven, 1996) and European regulations (Guideline 86/609/EEC), and were approved by the Animal Ethics Committee of Utrecht University.
Leptin sensitivity
Leptin sensitivity was tested before fcHFHS diet exposure, and after 2, 4, and 8 weeks of fcHFHS diet exposure. To measure leptin sensitivity, animals were food restricted overnight (10 gr chow at 1600 h). The next morning at 0900 h, leptin (250 µg/250 µl; recombinant murine leptin, NHPP, USA) or vehicle (250 µl, phosphate buffered saline, PBS) was injected via the jugular vein catheter, and 45 min later food was given back. A latin-square design was used, as such that half of the rats in each dietary group first received leptin, and 3–4 days later rats were tested a second time with treatments reversed. Food intake was measured 1–24 h after food return by using data collected by Scales (Department Biomedical Engineering, UMC Utrecht, The Netherlands). This program records the weight of food hoppers in the home cage automatically every 12 s, as well as the amount of licks from water or sucrose bottles.
To divide the chow control group into two types of responders, leptin sensitivity of each individual rat was determined at four different time-points (before fcHFHS diet exposure, and at 2, 4, and 8 weeks of fcHFHS diet exposure), and subsequently the average response of all four tests was taken. Leptin sensitivity was measured by normalizing cumulative food intake after leptin injection to cumulative food intake after vehicle injection. Rats were divided into two subgroups based upon their feeding response at 1 h after leptin injection, as the variability was the largest at this time-point. Rats showing a reduction in food intake (percentage suppression < 100) were designated as LS (n = 11), whereas rats showing no reduction or even an increase in food intake were designated as LR (percentage suppression ≥ 100, n = 10). Rats offered the fcHFHS diet were selected as LS (n = 11) or LR (n = 7) based upon their leptin sensitivity test before fcHFHS diet exposure.
Immunohistochemistry
Rats were injected with leptin (250 µg/250 µl) or vehicle via the jugular vein catheter, and subsequently all chow, lard, and the 30% sucrose solution were removed. Two hours later, rats were anesthetized with sodium pentobarbital (Nembutal, 100 mg/kg/ml) and perfused with ice cold 0.9% NaCl, followed by 4% paraformaldehyde (PFA). Brains were removed, incubated overnight in 4% PFA, and subsequently immersed in 30% sucrose solution in PBS. Brains were cut in 40 µm coronal free-floating slices, collected in six series, and pSTAT3 immunohistochemistry was performed as described previously [31]. In brief, one of the six series of free-floating slices was blocked in horse serum and then incubated overnight with rabbit anti-pSTAT3 (1:1000, rabbit monoclonal, Cell Signaling, # 9145S). Slices were washed and incubated with biotinylated anti-rabbit antibody (1:250), followed by avidin-biotin-complex labeling. Pictures were taken using a bright-field microscope with a digital camera (Axiocam, Zeiss, Germany). Slices were matched to the stereotaxic brain atlas from Paxinos and Watson (1998; fourth edition), using the fornix, mammillothalamic tract, and optic tract as landmarks. For each animal, the number of pSTAT3 positive cells was counted blindly in both sides of the ARC and DMH, and the intensity of the bright field signal was quantified in the ventromedial hypothalamus (VMH) with background intensity subtracted, at one slice at Bregma −3.30.
Body composition
At the end of the experiment, rats were anesthetized and prior to perfusion, individual epididymal and subcutaneous (inguinal) white adipose tissues were dissected from the left side, cleaned and weighed.
Plasma leptin levels
Blood samples were taken shortly prior to leptin or vehicle injection during each leptin sensitivity test session and immediately chilled on ice. Blood was centrifuged (4 °C; 10.000 rpm; 20 min) and plasma was stored at −20 °C until further analysis. Plasma leptin levels were measured in duplicate using a radioimmunoassay kit (Multi-Species Leptin RIA, XL-85K, Merck Millipore, USA). The amounts of sample, standards, label, antibody and precipitating reagent were divided by four.
Statistical analysis
Two rats could not be tested for their leptin sensitivity at week 4, three rats could not be tested at week 8, and two rats could not be tested during the entire experiment because of a blockade of their catheter. Blood collection was not successful at one or more time-points in 16 rats. These rats were excluded from the concerning analyses. Fat mass was only tested in a subgroup of 16 rats, and pSTAT3 levels were tested in a subgroup of 30 rats. Food intake data were computed automatically. Since the leptin sensitivity data of each rat was used to group them, and as rats were offered either a chow or fcHFHS diet, experimenters were not explicitly blinded for experimental treatments or group allocation.
For differences in body weight (gain), caloric intake, and plasma leptin levels, two-way repeated measures ANOVA’s were performed with week as within-subject variable and diet (chow vs. fcHFHS and/or responder) as between-subject variable. For fat mass analysis, a one-way ANOVA was performed with diet/responder as between-subject variable. Feeding responses to leptin were assessed using a three-way repeated measures ANOVA with time and treatment as within-subject variables and diet/responder as between subject-variable. Count data of leptin sensitivity was analyzed with a two-way repeated measures ANOVA with diet (before/after fcHFHS) as within subjects-variable and responder as between subject-variable. Analysis of pSTAT3 levels was performed with a MANOVA with treatment, diet, and group as between subject-variable.
Mauchly’s test of sphericity was used to test whether variances of the differences between treatment levels were equal. If the assumption of sphericity was violated, degrees of freedom were corrected using Greenhouse–Geisser (GG) estimates of sphericity or Huynh-Feldt estimates of sphericity when the GG estimate was >0.75. When appropriate, post hoc analyses were conducted using Student’s t-tests or pairwise Bonferroni comparisons. Each parameter was tested for normality with the Kolmogorov-Smirnov test. When data were not normally distributed, data were log transformed prior to statistical analyses.
The unbiased clustering analysis of leptin sensitivity on chow diet was carried out by means of a TwoStep cluster analysis. Individual leptin sensitivity at 1 h after injection, as measured by cumulative food intake after leptin injection normalized to baseline vehicle, was introduced as input variable in the cluster analysis. The log-likelihood method was used to determine inter-subject distance. The number of clusters was determined automatically based on Schwarz’s Bayesian criteria and log-likelihood method.
Statistical analyses were conducted using SPSS 20.3 for Windows. The threshold for statistical significance was set at p < 0.05; all tests were two-sided. Data are presented as mean ± SEM.
Results
Exposure to the fcHFHS diet results in hyperphagia and obesity
As reported previously [16, 32], rats offered a fcHFHS diet (n = 20) showed increased body weight, caloric intake, and adiposity compared with control rats on a chow diet (n = 21) (Fig. 1a, b, d). In addition, plasma leptin levels were higher from 4 weeks of fcHFHS diet exposure onwards compared with control rats (Fig. 1c).
Obesity-related parameters in rats offered a chow or fcHFHS diet. a Body weight, (b) caloric intake, and (c) plasma leptin levels during the whole experimental period (n = 20–21 per group). Fweek*diet ≥ 6.402, p ≤ 0.007. d Epididymal and subcutaneous (inguinal) white adipose tissues at week 9 (n = 8 per group), t = −6.042, p = 0.000. Data is shown as mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001 compared with chow controls
Both chow and fcHFHS fed rats show high variability in individual leptin sensitivity
We next determined whether fcHFHS diet fed rats developed leptin resistance. Leptin sensitivity was tested before fcHFHS diet feeding, and after 2, 4, and 8 weeks of fcHFHS diet exposure. As leptin’s food intake suppressing effects were previously reported at variable time-points after exogenous leptin injection (Table S1) [28, 33], we here show leptin sensitivity at the four most common time-points reported by previous studies (Fig. 2). Leptin sensitivity was tested via two common methods, i.e., by comparing absolute cumulative caloric intake after leptin or vehicle injection (Fig. 2a–c) and by calculating the percentage suppression from baseline vehicle (Fig. 2d–f). Before fcHFHS diet exposure, rats significantly reduced their food intake at 14–24 h after leptin injection, and leptin sensitivity did not differ between prospective chow and fcHFHS diet fed rats (Fig. 2a, d). At week 2, no differences in leptin sensitivity were observed between the chow and fcHFHS group (data not shown). However, from week 4 onwards leptin sensitivity was impaired in fcHFHS fed rats compared with chow controls (Fig. 2b, c, e, f). The chow group was still leptin sensitive at both week 4 and week 8, whereas the fcHFHS group did no longer show a reduction in food intake after leptin injection. So, by testing leptin sensitivity at the group level, the fcHFHS group developed leptin resistance from week 4 onwards. However, individual data points show high variability in leptin sensitivity between rats in both the chow and fcHFHS group, especially at the first hours after injection (Fig. 2d–f).
Feeding response to leptin in rats offered a chow or fcHFHS diet. a–c Leptin sensitivity, as measured by absolute cumulative caloric intake after vehicle or leptin injection, is shown (a) before, (b) after 4 weeks, and (c) after 8 weeks of fcHFHS diet exposure. d–f Leptin sensitivity, as measured by cumulative food intake after leptin injection normalized to vehicle cumulative food intake, was measured (d) before, (e) after 4 weeks, and (f) after 8 weeks of fcHFHS diet exposure. Before fcHFHS, Fdiet*treatment ≥ 0.001, p ≥ 0.951, Ftreatment ≥ 9.670, p ≤ 0.004; week 4 and 8, Fdiet*treatment ≥ 4.397, p ≤ 0.044; chow week 4 and 8, Ftreatment ≥ 6.529, p ≤ 0.019; fcHFHS week 4 and 8, Ftreatment ≥ 0.118, p ≥ 0.223. Data is shown as mean ± SEM; n = 17–21 per group. *P < 0.05, **P < 0.01,***P < 0.001 compared with vehicle
Based upon variability in individual leptin sensitivity on chow diet, rats were divided into two types of responders
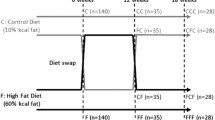
Since the chow group was kept on chow diet for 8 weeks and tested for leptin sensitivity every 2 weeks, we were able to determine whether leptin sensitivity is a stable parameter in a rat (Fig. 3a). Leptin sensitivity was tested by normalizing 1–24 h cumulative caloric intake after leptin injection to baseline vehicle. Individual rats showed a stable response pattern over weeks (Figure S2). Closer inspection of individual leptin sensitivity on chow diet revealed two types of responders. Rats were divided in those showing a reduction in food intake at the first hour after leptin injection (leptin sensitive, LS, n = 11), and those that reduced their food intake at later time-points after leptin injection, showing no reduction or even an increase in food intake at the first hours after injection (relatively leptin resistant, LR, n = 10) (Fig. 3b, c). The selection of LS and LR rats was based on the average leptin sensitivity of four independent leptin sensitivity tests (Fig. 3a, c and Figure S2). The response to leptin at 1 h food intake ranged from −26.5 to −6.3% (−21.7 ± 2.4) in LS rats and from +0.2 to +98.4% (+22.4 ± 10.0) in LR rats. Statistical analyses confirmed that the selected LS and LR rats also responded differently to leptin at other time-points after injection, especially at 2–4 h after injection (Fig. 3). Only LS rats differed significantly from baseline vehicle at the first four hours after leptin injection. At 13–24 h after leptin injection, LS and LR rats showed a similar reduction in food intake. In accordance with the general response patterns, LS rats showed their strongest reduction in food intake at an earlier time-point after leptin injection compared with LR rats (4.8 ± 0.7 h vs. 7.6 ± 0.6 h) (Fig. 3d).
Individual 1–24 h leptin sensitivity in rats offered a chow diet. Based upon leptin sensitivity on chow diet, rats were divided in those showing a reduction in food intake at the first hour after leptin injection (LS) and those that did not change or increased their food intake with leptin at 1 h food intake (LR). a Experimental design. Leptin sensitivity was measured by cumulative food intake after leptin injection normalized to vehicle food intake. Average leptin sensitivity of four tests is shown. Leptin sensitivity (b) at group level and (c) individual level; a heat plot of the relative level of sensitivity is shown at 1–24 h food intake for each individual rat (i.e., each row). The heat plot indicates the relative degree of leptin sensitivity at a particular time point in comparison with the other time-points in the row. 1–24 h: Fhour*treatment*group = 8.239, p = 0.000, post hoc p < 0.05 at 1–4 h. 1–4 h: LS, Ftreatment = 48.561, p = 0.000; LR, Ftreatment = 0.931, p = 0.360. d The average time-point of the strongest food intake suppressing effect of leptin is shown for each individual rat (average of four tests is shown); t = −3.164, p = 0.005. Data is shown as mean ± SEM; n = 9–11 per group. **P < 0.01 for LS vs. LR
We confirmed our manual selection of LS and LR rats by carrying out an unbiased TwoStep clustering analysis based upon individual leptin sensitivity on chow diet. The number of clusters was determined automatically and yielded two clusters, in which rats were classified in exactly the same subgroups as in our manual classification (n = 11, 52.4%; n = 10, 47.6%). The cluster analysis resulted in an average Silhouette measure of cluster cohesion and separation of 0.70, indicating a good cluster quality.
A pre-existing reduction in leptin sensitivity on chow diet predicts the susceptibility to develop excessive DIO
Like the chow diet group, the fcHFHS diet group was also divided into LS (n = 12) and LR (n = 9) rats based upon leptin sensitivity before fcHFHS diet exposure (Fig. 4a). Obesity-related parameters were studied in both chow and fcHFHS diet fed LS and LR rats. Chow diet fed LS and LR rats did not differ in body weight gain, caloric intake, plasma leptin levels, and adiposity (Fig. 4). However, LR rats offered a fcHFHS diet gained 10.6% more body weight compared with chow diet fed controls (Fig. 4b). Body weight gain in fcHFHS diet fed LS rats did not differ from chow controls. Although both LS and LR rats fed a fcHFHS diet increased their plasma leptin levels and adiposity over the course of diet exposure, plasma leptin levels, and adiposity were higher in LR rats compared with LS rats after 8 weeks of fcHFHS diet exposure (Fig. 4c, d). Increased body weight gain on the fcHFHS diet in LR vs. LS rats could not be explained by differences in average caloric intake or the average consumption of the different components of the fcHFHS diet (Fig. 4e, f). So, these data show that leptin sensitivity on a chow diet predicts the susceptibility to develop excessive DIO, as LR rats were more prone to develop obesity on a fcHFHS diet compared with LS rats.
Obesity-related parameters in LS and LR rats offered either a chow or fcHFHS diet. a Experimental design. Rats were first divided into a chow and fcHFHS group, and subsequently divided into LS and LR rats. The selection of LS and LR rats was based on the average leptin sensitivity of four independent leptin sensitivity tests in the chow diet group, and leptin sensitivity before fcHFHS diet exposure in the fcHFHS diet group. b Body weight gain, (c) Epididymal and subcutaneous (inguinal) white adipose tissues at week 9, and (d) Plasma leptin levels during the whole experimental period. Fweek*diet/subgroup ≥ 3.390, p ≤ 0.013. e Caloric intake (week average of kcal per day), (f) consumption of the different components of the fcHFHS diet (week average of kcal per day). Fweek*diet/subgroup = 8.340, p = 0.000; chow, Fsubgroup = 0.008, p = 0.931; fcHFHS, Fsubgroup ≥ 0.057, p ≥ 0.320. g Leptin resistance as measured by cumulative food intake after leptin injection normalized to vehicle food intake, followed by a count of the number of time-points with a value of ≥100. Data show the response to leptin before fcHFHS diet exposure (chow) and for the average of week 4 and 8 of the fcHFHS diet. Fdiet*subgroup = 7.316, p = 0.016. Data is shown as mean ± SEM; n = 4–12 per group. Different lowercase letters represent significant differences (P < 0.05) between bars. #P < 0.07; *P < 0.05; **P < 0.01 in comparison with the LS and/or LR rats on chow diet
Exposure to the fcHFHS diet does not further reduce leptin sensitivity in rats with a pre-existing reduction in leptin sensitivity
As diet-induced leptin resistance has been proposed to initiate and/or maintain DIO [5, 7,8,9, 11,12,13, 22,23,24], the development of leptin resistance on the fcHFHS diet was compared between LS and LR rats. Leptin sensitivity was tested by normalizing 1–24 h cumulative caloric intake after leptin injection to baseline vehicle (Figure S3), and by counting the number of time-points out of 24 h time-points at which the rats did not reduce their food intake after leptin injection compared with vehicle (i.e., number of time-points with a percentage suppression of ≥100) (Fig. 4g). The feeding response to leptin before fcHFHS diet exposure was compared with the average response at week 4 and 8 of the fcHFHS diet, as rats developed leptin resistance at the group level from 4 weeks of fcHFHS diet feeding onwards (Fig. 2). Before fcHFHS diet exposure, LS rats were more leptin sensitive compared with LR rats (Fig. 4g and Figure S3). LS rats became less leptin sensitive during fcHFHS diet exposure, whereas the fcHFHS diet did not further reduce leptin sensitivity in LR rats. As a result, leptin sensitivity did no longer differ between the subgroups after fcHFHS diet feeding. Thus, LR rats, which were more prone to develop DIO than LS rats (Fig. 4), did not develop diet-induced leptin resistance. Conversely, LS rats, which were less prone to develop DIO, did develop leptin resistance after fcHFHS diet exposure (Fig. 4). These findings indicate that a pre-existing reduction in leptin sensitivity rather than diet-induced leptin resistance is critical for the development of excessive DIO.
A pre-existing reduction in cellular leptin signaling in the DMH and VMH but not the ARC, predicts the susceptibility to develop excessive DIO
Finally, we studied whether the pre-existing reduction in leptin sensitivity in LR compared with LS rats could be explained by differences in cellular leptin sensitivity in the hypothalamus. The number of pSTAT3 positive neurons was counted in the ARC, VMH, and DMH (Fig. 5). Basal pSTAT3 levels did not differ between chow diet fed LS and LR rats. In the ARC, a leptin-induced increase in pSTAT3 levels was shown, but pSTAT3 levels did not differ between LS and LR rats (Fig. 5a, b). In contrast, in the VMH and DMH, the leptin-induced pSTAT3 activation was lower in LR rats compared with LS rats (Fig. 5a, c). So, the obesity-prone LR rats show a pre-existing reduction in cellular leptin sensitivity in the VMH and DMH but not the ARC.
Hypothalamic leptin sensitivity in LS and LR rats. a Representative images of pSTAT3 immunoreactivity in the hypothalamic arcuate nucleus (ARC), ventromedial hypothalamus (VMH), and dorsomedial hypothalamus (DMH) of LS and LR rats fed a chow or fcHFHS diet. b–d Number of pSTAT3 immunoreactive cells in the ARC (b), VMH (c), and DMH (d). ARC, Fdiet*treatment = 4.348, p = 0.049; Fsubgroup = 0.354, p = 0.558. VMH, Fdiet*treatment = 4.490, p = 0.046, Fdiet*subgroup = 8.530, p = 0.008, Ftreatment = 40.151, p = 0.000. DMH, Fdiet*treatment*subgroup = 4.338, p = 0.049. Data is shown as mean ± SEM; n = 3–5 per group. Different lowercase letters represent significant differences (P < 0.05) between bars
We also studied the development of diet-induced leptin resistance at the cellular level. In the ARC, basal pSTAT3 levels were elevated in fcHFHS diet fed rats compared with chow controls (Fig. 5a, b). Leptin injection did not further increase pSTAT3 levels in fcHFHS diet fed rats. Thus, fcHFHS diet fed rats showed increased endogenous leptin signaling in the ARC and could not further increase their signaling after leptin injection. fcHFHS diet fed LS and LR rats did not differ in either basal or leptin-induced pSTAT3 levels in the ARC. In the DMH, however, fcHFHS diet fed LS rats showed lower leptin-induced pSTAT3 levels compared with LR rats (Fig. 5a, c). In comparison with chow diet fed rats, leptin-induced pSTAT3 levels in the DMH and VMH were dramatically reduced (~70%) in fcHFHS diet fed LS rats, but not affected in fcHFHS diet fed LR rats. These findings show that exposure to the fcHFHS diet does not further reduce the pre-existing reduction in pSTAT3 activation in the VMH and DMH in the obesity-prone LR rats. Thus, a pre-existing, but not diet-induced, reduction in leptin signaling in the VMH and DMH is associated with the susceptibility to develop DIO.
Discussion
Across species, there is a high and unexplained variability in the development of obesity upon exposure to energy-dense diets high in saturated fat and sugar. We here demonstrate that individual leptin sensitivity on a chow diet, prior to exposure to a diet high in saturated fat and sugar, predicts the susceptibility to develop DIO (Fig. 6). We showed that leptin sensitivity is highly variable between chow-diet fed rats, but stable over time per individual rat, and is therefore a reliable predictor for DIO. Leptin resistant (LR) rats, which showed a pre-existing reduction in leptin sensitivity compared with leptin sensitive (LS) rats, gained more body weight and adiposity after 8 weeks of fcHFHS diet exposure, without eating more calories or altering leptin sensitivity. The pre-existing reduction in the anorectic response to leptin in LR compared with LS rats was associated with reduced leptin-induced pSTAT3 levels in the DMH and VMH but not the ARC, a brain area known to be a critical regulator of food intake [34,35,36,37]. These results challenge the generally accepted concept of diet-induced leptin resistance in the ARC as a causal factor for the initiation and/or maintenance of DIO.
We first systematically reviewed literature to show that both the time-points and effect sizes of the anorectic response to leptin are very variable (Table S1) [28]. In addition, leptin sensitivity was often studied at the group level instead of comparing the treatment effects within individual rats (Table S1). We next showed the importance of studying leptin sensitivity at the individual level and at multiple time-points after injection. At the group level, the fcHFHS diet group developed leptin resistance after 4 weeks of fcHFHS diet feeding, whereas the chow group was still leptin sensitive. However, both the chow and fcHFHS diet group showed high variability in individual leptin sensitivity. Closer inspection of individual leptin sensitivity on chow diet revealed two different types of leptin responders, LS and LR rats, which were hidden in the group average data. LS and LR rats especially differed in their leptin sensitivity at 1–4 h after leptin injection, but did not differ at 13–24 h food intake. Only since we monitored food intake continuously over 24 h following leptin injection, we were able to discover the two types of leptin responders on a chow diet. This turned out to be crucial to predict which rats increase body weight after fcHFHS diet exposure.
Note that in contrast to earlier studies in which leptin was injected only once [28, 29], in our study, we found that individual chow diet fed rats show a stable response pattern to leptin over weeks, as was tested with four independent leptin sensitivity tests. Thus, we show that leptin sensitivity is a stable parameter in a rat and is therefore a reliable predictor for DIO. The finding that LS and LR rats especially differed in their leptin sensitivity at 1–4 h after leptin injection is in accordance with Ruffin et al. and Levin et al., who also reported the major differences in leptin sensitivity before HED exposure at 2 or 4 h, but not 24 h, food intake [28, 29]. The predominant variability in leptin sensitivity at the first four hours after leptin injection might be due to the food restriction instead of fasting prior to leptin sensitivity testing: rats might respond differently to food restriction instead of fasting and/or the drive to eat was probably stronger at the first hours after food return. Interestingly, a highly variable effect of leptin (range −94 to +129%) on food intake was specifically reported by Ruffin et al. [28], who also administered leptin intravenously in male Wistar rats, as opposed to the more common intraperitoneal leptin administration in mostly Sprague-Dawley rats (Table S1) [29]. Therefore, the high variability in leptin sensitivity we observed, including the (non-significant) tendency of LR to increase their food intake after leptin injection, could be a strain effect or result from the intravenous instead of intraperitoneal route of administration.
Levin et al. reported that selectively bred DIO rats and DR rats, fed a chow diet, did not differ in leptin transport across the blood brain barrier [33]. However, DIO rats showed reduced Lepr-b expression [33, 38], leptin receptor binding [39], and leptin-induced pSTAT3 levels in the ARC, VMH, and DMH compared with DR rats [33, 40]. We here also studied whether the reduced anorectic response to leptin in chow diet fed LR compared with LS rats could be explained by differences in hypothalamic pSTAT3 activation, and found that LR rats showed lower leptin-induced pSTAT3 activation in the DMH and VMH but not the ARC. There is evidence that leptin’s regulation of food intake is also mediated via leptin signaling in the DMH [18, 41, but see 42]. So, lower leptin evoked pSTAT3 activation in the DMH could explain the reduced anorectic response to leptin in chow diet fed LR rats. The discrepancy with the above described results of Levin et al. [33] might result from their selective breeding of DR and DIO rats or differences in rat strain and/or supplier.
Despite that LS and LR rats were selected based on their acute feeding response to leptin, they displayed similar daily caloric intake on both a chow and fcHFHS diet. This is particularly fascinating as leptin is believed to be a physiological regulator of (long-term) energy intake [34, 35, 37]. Previous studies in rats with a pre-existing or experimentally-induced impairment in leptin sensitivity showed a considerable increase in daily caloric intake on high-energy or high-fat diet, and sometimes even on chow diet [24, 25, 28, 29]. In previous studies, obesity in (outbred or selectively bred) Wistar and Sprague-Dawley rats with a pre-existing reduction in leptin sensitivity largely resulted from hyperphagia. In contrast, we here show that daily caloric intake was similar in LS and LR rats. Thus, caloric intake cannot explain why LR rats gained more weight and adiposity on a fcHFHS diet compared with LS rats, which makes our model interesting to study food intake independent mechanisms by which a pre-existing reduction in leptin sensitivity predisposes rats to develop exacerbated DIO on a energy-dense diet. In the model of Levin et al., reduced cellular leptin sensitivity in the ARC may predispose DIO rats to hyperphagic obesity [33, 40], while in our model the development of obesity may result from differences in pSTAT3 activation in the VMH/DMH between LS and LR rats. Leptin action in the DMH and VMH has been shown to regulate energy balance by increasing thermogenesis and energy expenditure [18, 41,42,43,44]. Therefore, reduced thermogenesis and/or energy expenditure could explain the increased body weight gain and adiposity in fcHFHS diet fed LR rats. Alternatively, LR rats might have an increased capacity to absorb energy from the fcHFHS diet, as increased energy extraction has been associated with high-fat diet feeding, obesity, and reduced leptin sensitivity [45,46,47].
One major question we addressed in this study was whether DIO mostly results from diet-induced leptin resistance or if a pre-existing reduction in leptin sensitivity is more critical for the development of DIO. This issue was not resolved by previous studies, as leptin sensitivity was usually tested only before [28, 29, 33] or after [7, 11, 12, 15, 16, 23] high-energy or high-fat diet exposure. LR rats showed a pre-existing reduction in leptin sensitivity on chow diet compared with LS rats. Exposure to the fcHFHS diet impaired leptin sensitivity in LS rats, but did not further reduce leptin sensitivity in LR rats. Since LR rats showed exacerbated weight gain and adiposity compared with LS rats during fcHFHS diet feeding, our data indicate that the susceptibility to develop excessive DIO depends on a pre-existing reduction in leptin responsiveness rather than diet-induced leptin resistance. This conclusion is supported by the findings of leptin sensitivity at the cellular level, showing that LR rats showed a pre-existing reduction in leptin-induced pSTAT3 activation in the DMH and VMH compared with LS rats, which was not further reduced by fcHFHS diet exposure. Both LS and LR rats did not develop leptin resistance in the ARC after fcHFHS diet exposure. Leptin treatment did not induce pSTAT3 activation in the ARC, but this resulted from the elevated basal pSTAT3 levels upon exposure to the fcHFHS diet, indicating increased endogenous leptin signaling [9]. The finding of ongoing endogenous leptin signaling in the ARC of both LS and LR rats contradicts previous studies showing selective leptin resistance in the ARC after high-fat diet feeding [18, 22]. Thus, our results challenge the generally accepted concept of diet-induced leptin resistance in the ARC as a causal factor for the initiation and/or maintenance of DIO. We show that a predisposing reduction in leptin sensitivity, as measured by both the early anorectic response to leptin and cellular leptin sensitivity in the VMH/DMH, is more critical for the development of excessive DIO than diet-induced leptin resistance.
To conclude, the results described in this study indicate that individual leptin sensitivity on chow diet, during the first hour following leptin injection, predicts the susceptibility to DIO. Those rats with a pre-existing reduction in leptin sensitivity escalated their weight gain merely during exposure to a diet high in saturated fat and sugar. Therefore, the overabundance of readily available energy-dense food in today’s society might be especially a risk factor for individuals with a pre-existing susceptibility to develop obesity. It would be interesting to test whether the feeding response to leptin is suitable as a biomarker for humans with an increased susceptibility to develop excessive obesity, as such that those identified as susceptible know that they should be very cautious with their diet and lifestyle in order to prevent the development of obesity.
References
Nguyen DM, El-Serag HB. The epidemiology of obesity. Gastroenterol Clin North Am. 2010;39:1–7.
Pandit R, Mercer JG, Overduin J, la Fleur SE, Adan RA. Dietary factors affect food reward and motivation to eat. Obes Facts. 2012;5:221–42.
Schwartz MW, Peskind E, Raskind M, Boyko EJ, Porte D Jr Cerebrospinal fluid leptin levels: relationship to plasma levels and to adiposity in humans. Nat Med. 1996;2:589–93.
Considine RV, Stephens TW, Nyce M, Ohannesian JP, Marco CC, McKee LJ, et al. Serum immunoreactive-leptin concentrations in normal-weight and obese humans. New Engl J Med. 1996;334:292.
Heymsfield SB, Greenberg AS, Fujioka K, Dixon RM, Kushner R, Hunt T, et al. Recombinant leptin for weight loss in obese and lean adults: a randomized, controlled, dose-escalation trial. JAMA. 1999;282:1568–75.
Caro JF, Kolaczynski JW, Nyce MR, Ohannesian JP, Opentanova I, Goldman WH, et al. Decreased cerebrospinal-fluid/serum leptin ratio in obesity: a possible mechanism for leptin resistance. Lancet. 1996;348:159–61.
Apolzan JW, Harris RB. Rapid onset and reversal of peripheral and central leptin resistance in rats offered chow, sucrose solution, and lard. Appetite. 2013;60:65–73.
Myers MG Jr Leptin keeps working, even in obesity. Cell Metab. 2015;21:791–2.
Ottaway N, Mahbod P, Rivero B, Norman LA, Gertler A, D’Alessio DA, et al. Diet-induced obese mice retain endogenous leptin action. Cell Metab. 2015;21:877–82.
Lin L, Martin R, Schaffhauser AO, York DA. Acute changes in the response to peripheral leptin with alteration in the diet composition. Am J Physiol Regul Integr Comp Physiol. 2001;280:R504–9.
Shapiro A, Tumer N, Gao Y, Cheng KY, Scarpace PJ. Prevention and reversal of diet-induced leptin resistance with a sugar-free diet despite high fat content. Br J Nutr. 2011;106:390–7.
Haring SJ, Harris RB. The relation between dietary fructose, dietary fat and leptin responsiveness in rats. Physiol Behav. 2011;104:914–22.
Scarpace PJ, Matheny M, Tumer N, Cheng KY, Zhang Y. Leptin resistance exacerbates diet-induced obesity and is associated with diminished maximal leptin signalling capacity in rats. Diabetologia. 2005;48:1075–83.
Frederich RC, Hamann A, Anderson S, Lollmann B, Lowell BB, Flier JS. Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med. 1995;1:1311–4.
Harris RB, Apolzan JW. Changes in glucose tolerance and leptin responsiveness of rats offered a choice of lard, sucrose, and chow. Am J Physiol Regul Integr Comp Physiol. 2012;302:R1327–39.
van den Heuvel JK, Eggels L, van Rozen AJ, Luijendijk MC, Fliers E, Kalsbeek A, et al. Neuropeptide Y and leptin sensitivity is dependent on diet composition. J Neuroendocrinol. 2014;26:377–85.
Enriori PJ, Evans AE, Sinnayah P, Jobst EE, Tonelli-Lemos L, Billes SK, et al. Diet-induced obesity causes severe but reversible leptin resistance in arcuate melanocortin neurons. Cell Metab. 2007;5:181–94.
Enriori PJ, Sinnayah P, Simonds SE, Garcia Rudaz C, Cowley MA. Leptin action in the dorsomedial hypothalamus increases sympathetic tone to brown adipose tissue in spite of systemic leptin resistance. J Neurosci. 2011;31:12189–97.
Mercer JG, Hoggard N, Williams LM, Lawrence CB, Hannah LT, Trayhurn P. Localization of leptin receptor mRNA and the long form splice variant (Ob-Rb) in mouse hypothalamus and adjacent brain regions by in situ hybridization. FEBS Lett. 1996;387:113–6.
Elmquist JK, Bjorbaek C, Ahima RS, Flier JS, Saper CB. Distributions of leptin receptor mRNA isoforms in the rat brain. J Comp Neurol. 1998;395:535–47.
Hakansson ML, Brown H, Ghilardi N, Skoda RC, Meister B. Leptin receptor immunoreactivity in chemically defined target neurons of the hypothalamus. J Neurosci. 1998;18:559–72.
Munzberg H, Flier JS, Bjorbaek C. Region-specific leptin resistance within the hypothalamus of diet-induced obese mice. Endocrinology. 2004;145:4880–9.
Desai BN, Harris RB. An acute method to test leptin responsiveness in rats. Am J Physiol Regul Integr Comp Physiol. 2014;306:R852–60.
Scarpace PJ, Zhang Y. Leptin resistance: a prediposing factor for diet-induced obesity. Am J Physiol Regul Integr Comp Physiol. 2009;296:R493–500.
Bates SH, Stearns WH, Dundon TA, Schubert M, Tso AW, Wang Y, et al. STAT3 signalling is required for leptin regulation of energy balance but not reproduction. Nature. 2003;421:856.
Gao Q, Wolfgang MJ, Neschen S, Morino K, Horvath TL, Shulman GI, et al. Disruption of neural signal transducer and activator of transcription 3 causes obesity, diabetes, infertility, and thermal dysregulation. Proc Natl Acad Sci USA. 2004;101:4661–6.
Shapiro A, Mu W, Roncal C, Cheng KY, Johnson RJ, Scarpace PJ. Fructose-induced leptin resistance exacerbates weight gain in response to subsequent high-fat feeding. Am J Physiol Regul Integr Comp Physiol. 2008;295:R1370–5.
Ruffin MP, Adage T, Kuipers F, Strubbe JH, Scheurink AJ, van Dijk G. Feeding and temperature responses to intravenous leptin infusion are differential predictors of obesity in rats. Am J Physiol Regul Integr Comp Physiol. 2004;286:R756–63.
Levin BE, Dunn-Meynell AA. Reduced central leptin sensitivity in rats with diet-induced obesity. Am J Physiol Regul Integr Comp Physiol. 2002;283:R941–8.
Steffens AB. A method of frequent sampling blood and continuous infusion of fluids in the rat without disturbing the animal. Physiol Behav. 1969;4:836.
Munzberg H, Huo L, Nillni EA, Hollenberg AN, Bjorbaek C. Role of signal transducer and activator of transcription 3 in regulation of hypothalamic proopiomelanocortin gene expression by leptin. Endocrinology. 2003;144:2121–31.
la Fleur SE, van Rozen AJ, Luijendijk MC, Groeneweg F, Adan RA. A free-choice high-fat high-sugar diet induces changes in arcuate neuropeptide expression that support hyperphagia. Int J Obes (Lond). 2010;34:537–46.
Levin BE, Dunn-Meynell AA, Banks WA. Obesity-prone rats have normal blood–brain barrier transport but defective central leptin signaling before obesity onset. Am J Physiol Regul Integr Comp Physiol. 2004;286:R143–50.
Wilson JL, Enriori PJ. A talk between fat tissue, gut, pancreas and brain to control body weight. Mol Cell Endocrinol. 2015;418:108–19.
Zhou Y, Rui L. Leptin signaling and leptin resistance. Front Med. 2013;7:207–22.
Satoh N, Ogawa Y, Katsuura G, Hayase M, Tsuji T, Imagawa K, et al. The arcuate nucleus as a primary site of satiety effect of leptin in rats. Neurosci Lett. 1997;224:149–52.
Morton GJ, Niswender KD, Rhodes CJ, Myers MG Jr, Blevins JE, Baskin DG, et al. Arcuate nucleus-specific leptin receptor gene therapy attenuates the obesity phenotype of Koletsky (fa(k)/fa(k)) rats. Endocrinology. 2003;144:2016–24.
Levin BE, Dunn-Meynell AA, Ricci M, Cummings DE. Abnormalities of leptin and ghrelin regulation in obesity-prone juvenile rats. Am J Physiol Endocrinol Metab. 2003;285:E949–E957.
Irani BG, Dunn-Meynell AA, Levin BE. Altered hypothalamic leptin, insulin and melanocortin binding associated with moderate fat diet and predisposition to obesity. Endocrinology. 2007;148:310–6.
Bouret SG, Gorski JN, Patterson CM, Chen S, Levin BE, Simerly RB. Hypothalamic neural projections are permanently disrupted in diet-induced obese rats. Cell Metab. 2008;7:179–85.
Dodd GT, Worth AA, Nunn N, Korpal AK, Bechtold DA, Allison MB, et al. The thermogenic effect of leptin is dependent on a distinct population of prolactin-releasing peptide neurons in the dorsomedial hypothalamus. Cell Metab. 2014;20:639–49.
Rezai-Zadeh K, Yu S, Jiang Y, Laque A, Schwartzenburg C, Morrison CD, et al. Leptin receptor neurons in the dorsomedial hypothalamus are key regulators of energy expenditure and body weight, but not food intake. Mol Metab. 2014;3:681–93.
Minokoshi Y, Haque MS, Shimazu T. Microinjection of leptin into the ventromedial hypothalamus increases glucose uptake in peripheral tissues in rats. Diabetes. 1999;48:287–91.
Pandit R, Beerens S, Adan RAH. Role of leptin in energy expenditure: the hypothalamic perspective. Am J Physiol Regul Integr Comp Physiol. 2017;312:R938–47.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–31.
Schele E, Grahnemo L, Anesten F, Hallen A, Backhed F, Jansson JO. The gut microbiota reduces leptin sensitivity and the expression of the obesity-suppressing neuropeptides proglucagon (Gcg) and brain-derived neurotrophic factor (Bdnf) in the central nervous system. Endocrinology. 2013;154:3643–51.
Park DY, Ahn YT, Park SH, Huh CS, Yoo SR, Yu R, et al. Supplementation of Lactobacillus curvatus HY7601 and Lactobacillus plantarum KY1032 in diet-induced obese mice is associated with gut microbial changes and reduction in obesity. PLOS One. 2013;8:e59470.
Acknowledgements
We thank Diana van Tuijl, Inge Wolterink-Donselaar, Jos Brits, Harrie van der Eerden, and Henk Spierenburg for their practical assistance.
Funding
This research was supported by the Dutch Technology Foundation STW (grant 12264), which is part of the Netherlands Organisation for Scientific Research (NWO), and which is partly funded by the Ministry of Economic Affairs, and by the NWO under project number 863.13.018 (NWO/ALW Veni grant).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
de Git, K.C.G., Peterse, C., Beerens, S. et al. Is leptin resistance the cause or the consequence of diet-induced obesity?. Int J Obes 42, 1445–1457 (2018). https://doi.org/10.1038/s41366-018-0111-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0111-4
- Springer Nature Limited
This article is cited by
-
Pharmacological targeting of glutamatergic neurons within the brainstem for weight reduction
Nature Metabolism (2022)
-
Obesity and COVID-19: A Fatal Alliance
Indian Journal of Clinical Biochemistry (2020)
-
Orexin A-induced inhibition of leptin expression and secretion in adipocytes reducing plasma leptin levels and hypothalamic leptin resistance
Pflügers Archiv - European Journal of Physiology (2019)
-
Palmitic acid is an intracellular signaling molecule involved in disease development
Cellular and Molecular Life Sciences (2019)