Abstract
Background/objectives
Study sex- and ethnic-specific childhood BMI growth trajectories of US children, and explore the potential causes of ethnic disparities in childhood BMI trajectories, including household socio-economic status (SES) and parenting practice using nationally representative longitudinal data.
Subjects/methods
BMI trajectory curves between 7 months to 16 years of age were fitted using mixed effect models with fractional polynomial functions using pooled 10-year (1998–2008) longitudinal data collected from 29,254 children from two US nationally representative cohorts-Early Childhood Longitudinal Study-Birth (ECLS-B, 2001) and Kindergarten (ECLS-K, 1998–99). A multivariable regression model was used to examine the effects of SES and parenting factors on ethnic disparities in childhood BMI trajectory.
Results
Hispanic boys (HB) and African-American girls (AAG) continuously had the highest prevalence of overweight and obesity (HB: 52.5%, AAG: 49.1% around age of 11) and mean BMI after adiposity rebound than their counterparts. They had the earliest adiposity rebound (age mean [SD]: HB- 57.9 [7.8]; AAG- 59.0 [7.2] months), steeper BMI growth velocity (HB- 5.7 [1.8]; AAG- 7.0 [1.5] 10-2 kg/m2/month), and highest area under curve (HB- 2724.5 [489.8]; AAG- 2681.2 [426.7] kg/m2*month) from adiposity rebound to 16 years of age. The racial/ethnic disparities in childhood BMI trajectories were associated with household SES and family rules for children’s regular bedtime (p < 0.05).
Conclusions
In the US, ethnic disparities in childhood BMI trajectories and obesity are apparent starting from adiposity rebound around age of five. Some minority groups have unfavorable BMI trajectories. These disparities are partially explained by household SES and parenting factors.
Similar content being viewed by others
Introduction
Childhood obesity has become a global epidemic. It is seriously affecting the young generation’s health and future, as well as social and economic developments in many countries worldwide [1,2,3]. Over the past two decades, the prevalence of childhood overweight and obesity has been rising in many countries [4, 5]. Worldwide 42% of adults and approximately one-fifth of children are overweight or obese [5]. The US leads other countries in youth overweight/obesity rates, with 34.5% of 12–19-year-olds are overweight or obese in 2011–2012; childhood obesity is more common among certain racial and ethnic groups such as Hispanic boys and Black girls [6].
Ethnic disparities in childhood body mass index (BMI) trajectory may have their origins in the earliest stages of life [7,8,9,10,11]. In previous research, household socio-economic status (SES), family rules for children’s behavior, physiological/ genetic differences and early exposure in utero have been studied as predictors of ethnic disparities in childhood obesity but mainly separately and using small study samples, or/and cross-sectional data. No studies could identify individual’s BMI milestones from infancy to adolescence and use nationally representative data [12,13,14,15,16] due to difficulties in modeling fluctuations in childhood BMI curve and limited data with repeated anthropometric measurements during childhood. No study has examined ethnic disparities in childhood obesity and related causes using recent, nationally representative data in the US.
This study aimed to (1) provide recent estimates of sex- and ethnic-specific childhood BMI trajectories and dynamic of obesity status with age in the US; and (2) study causes of ethnic disparities in childhood BMI trajectories and obesity rates.
Methods and materials
Study design and study sample
Longitudinal data from two US nationally representative cohorts, the Early Childhood Longitudinal Study-Birth Cohort (ECLS-B) and the ECLS Kindergarten Class of 1998–99 (ECLS-K) were used. The ECLS-B followed 10,700 children born in the US in 2001 through kindergarten entry (at 9 months, 2–4–5–6 year; 5 waves); ECLS-K 1998–99 followed 21,410 kindergarteners from kindergarten to middle school (at kindergarten fall and spring, 1–3–5–8th grade; 6 waves) in diverse socio-economic and ethnic backgrounds. The present study included children with available information on sex, ethnicity, and one or more times of height and weight measurements (The final sample size was 29,250; of them 9,350 [88% of total subjects] from ECLS-B and 19,900 [93% of total subjects] from ECLS-K). All reported numbers about sample size were rounded to the nearest 50 for ECLS-B and 10 for ECLS-K according to the confidentiality policy of the US Department of Education.
Assessment and measures
Child demographic characteristics
We classified child ethnicity as non-Hispanic White, non-Hispanic African American (AA), Hispanic and Asian. For purposes of ethnic-specific analysis and to ensure sufficient statistical power, we excluded those children with multiple races or rare race (less than 3% of total population, including Native Hawaiian, other Pacific Islander, American Indian, or Alaska Native).
BMI and milestones of BMI trajectory characteristics
At each wave in ECLS-B or ECLS-K, each child’s weight and height were measured twice by trained test administrators during the direct child assessments to reduce measurement errors. Children’s BMIs were obtained as composite variables of ECLS [17] and we treated BMI < 10 or > 50 as implausible value/outliers for the analysis. Overweight/obesity for children aged ≥ 2 years was defined as the BMI ≥ 85th percentile for the same sex and age in the 2000 US CDC Growth Charts [18].
Childhood BMI trajectory is not easy to describe due to the fluctuation in childhood BMI curve with simple parameters. However, the major milestones–infancy peak (at the end of the first rapid increase of BMI; age at the infancy peak represents tempo of growth [19], and high infancy peak indicates accelerated postnatal growth and an accumulation of fat [20]) and adiposity rebound (AR, the nadir before the second rise in BMI [21]; early AR reflects accelerated growth and is associated with an increased risk of overweight [22]) has helped to describe the critical events of children’s growth, such as the time of high peaks and nadir and the degree of changes between the high and low points in previous research [12, 13, 15]. We used four parameters to characterize the two milestones in childhood BMI trajectory: (1) age and (2) BMI and (3) velocity (defined as difference in BMI divided by difference in age), and (4) area under curve (AUC, defined as the definite integral between the two age points; indicating child’s cumulative exposure to excessive body weight and predicting later risk of obesity and obesity-related diseases [14]) between infancy peak, AR and 16 years of age (the end point of data). According to previous findings, (1) earlier age at AR, (2) higher BMI at AR, (3) steeper velocity, and (4) wider AUC from AR to adolescence were defined as unfavorable BMI trajectory, which are associated with high risk of later obesity [12,13,14,15,16].
Household SES
We used the derived variable of ECLS SES scale Z-score, which incorporates information on parents’/primary caregivers’ education, occupation, and household income at the household level with mean of 0 and a standard deviation of 1. The SES scale Z-score reflects the household SES at the time of data collection.
Parenting practice
ECLS-B 2-year collection and the ECLS-K kindergarten spring collection shared three survey questions about parenting practice that may be related to childhood obesity. Parents/primary caregivers reported in a typical week: (1) whether they have routines about what time the child goes to bed (yes/ no); (2) which television programs the child can watch (yes/ no); and (3) the number of days the child has evening meals at a regular time. Accordingly, we defined three parenting practice based on whether the child had a regular bedtime, rules about TV program selections, and dinner at a regular time ≥ 5 days/week (according to the assumption that parents might keep regular dinner on weekdays and the distribution of children’s response).
Statistical analysis
First, we described socio-demographic characteristics of children and their families and presented mean BMI and prevalence of overweight and obesity by cohort, wave, sex, and ethnicity using SAS surveymeans and surveyfreq procedures to accounting the multistage stratified clustered sampling scheme in two ECLS cohorts with longitudinally consistent weights (Tables 1 and 2; Appendix 2).
Second, to define sex- and ethnic-specific children’s BMI growth curve, we pooled the ECLS-B and K data sets. We reasoned that combining the ECLS-B and ECLS-K data sets could yield a full perspective on childhood BMI trajectory from infancy to adolescence, given their similarities in nationally representative sampling as well as weight and height measures. And we used the best combination of fractional polynomial functions (using diverse combinations of age terms—Agepj; powers pj were selected from a fixed set of eight candidate values, including –2, –1, –0.5, or log, 0.5, 1, 2, and 3) from our previous work using a separate data set with more frequent BMI measures from ages at 1 week to 18 years old: [14] age(-2), age(-1), age(-0.5), log(age), age0.5, and age [14], mainly because it used frequent data points (at least a total of 18 BMI measures) for each child through the whole childhood from 1 week to 18 years. The best combination of fractional polynomial functions from our previous work is valid to reflect the whole childhood BMI trajectory among general US children. Appendix 1 presents the model fit with current data as predicted (curves) vs. observed (circles) childhood BMI trajectories.
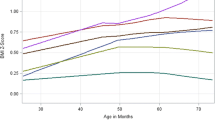
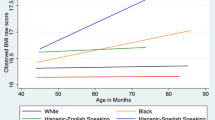
Then a specific fixed effect of each fractional polynomial term was estimated, which reflected the population-average trend for each of the eight subgroups by child sex and ethnicity (i.e., White boys/girls, AA boys/girls, Hispanic boys/girls, and Asian boys/girls). With the subgroup-specific fixed beta coefficients for fractional polynomial terms, we fit and plotted eight BMI trajectory curves to present sex- and ethnic-specific predicted mean BMI by age (in months, Fig. 1). To estimate each child’s BMI trajectory characteristics from his or her fitted mixed model we included the random effects of fractional polynomial terms with autoregressive correlation structure (the lowest BIC value among several candidate structures) to reflect his or her deviation from his or her sex and ethnic group average. From the model, we derived the parameters (age, BMI, velocity, and area under the curve) of two milestones for each individual and compared their mean levels by sex-ethnic groups (Table 3). To facilitate estimation of the two BMI milestones related parameters, we chose fractional polynomial model over other alternatives such as piecewise linear model and cubic spline model. We recognized its limitation of unstraightforward interpretation of the polynomial terms, which was not the focus of this study.
Sex- and ethnic-specific predicted mean BMI from 7 months to 16 years among the US children: the ECLS-B and ECLS-K cohorts (n = 29,250). Data collected during 1998–2008 from ECLS-B and ECLS-K were pooled and analyzed. The mixed effect model with fractional polynomial functions was used for the sex- and ethnic-specific BMI growth curves with considering the complex sample design of ECLS. The US CDC 2000 Growth Charts, the WHO child Growth Standards 2006 (birth to 5 years old) and the WHO Reference 2007 (5 to 19 years old) were used as references: 1) In White boys, expected value of BMI = 4465.1 – 9232.0*age(-2) + 11,336.0*age(-1) – 11,197.0*age(-0.5) – 1085.7*log(age) + 183.2*age0.5 – 2.7*age; 2) In AA boys, expected value of BMI = 1735.6 – 2614.1*age(-2) + 3822.1*age(-1) – 4132.2*age(-0.5) – 433.0*log(age) + 76.2*age0.5 – 1.1*age; 3) In Hispanic boys, expected value of BMI = 3733.7 – 7070.9*age(-2) + 9025.0*age(-1) – 9191.7*age(-0.5) – 924.0*log(age) + 161.7*age0.5 – 2.5*age; 4) In Asian boys, expected value of BMI = 4435.5 – 7541.3*age(-2) + 10,357.0*age(-1) – 10,815.0*age(-0.5) – 1109.1*log(age) + 198.3*age0.5 – 3.1*age; 5) In White girls, expected value of BMI = 2685.6 – 5699.2*age(-2) + 6795.1*age(-1) – 6702.3*age(-0.5) – 653.0*log(age) + 110.3*age0.5 – 1.6*age; 6) In AA girls, expected value of BMI = 4913.2 – 10,888.0*age(-2) + 12,809.0*age(-1) – 12,426.0*age(-0.5) – 1188.8*log(age) + 198.6*age0.5 – 2.9*age; 7) In Hispanic girls, expected value of BMI = 5647.5 – 12,254.0*age(-2) + 14,575.0*age(-1) – 14,236.0*age(-0.5) – 1374.2*log(age) + 233.0*age0.5 – 3.5*age; 8) In Asian girls, expected value of BMI = 1901.8 – 3475.6*age(-2) + 4615.0*age(-1) – 4689.2*age(-0.5) – 459.0*log(age) + 75.4*age0.5 – 1.0*age)
Based on the causal step method for the mediation criteria [23], a substantial mediation effect was defined as a 10% or greater reduction in the estimated coefficient for ethnic disparities in a BMI trajectory characteristic after adjusting for a potential mediator. Since parenting practice for the child’s regular meal times and TV program selections were not significantly associated with milestones of childhood BMI trajectory in bivariate regression analysis (p > 0.1), they were not included in the final model. Therefore, we assessed the mediating roles of household SES and parenting practice for child’s bedtime on the ethnic disparities in major milestones of BMI trajectory characteristics with a series of multivariable linear regression models with different sets of covariates: model 1 adjusted for cohort effect, child sex, number of siblings, and family structure; model 2 additionally adjusted for household SES level after model 1; model 3 additionally adjusted for parenting practice for child’s regular bedtime after model 1; model 4 simultaneously adjusted for all covariates (Table 4 and Appendix 3). Each parameter of BMI trajectory characteristics had a separate model to test the mediation effect and ethnic dummy variables were used to compare ethnic difference in BMI trajectory characteristics. Analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC).
Results
Sample characteristics at baseline
Sex and ethnicity distributions were similar between the two cohorts, but ECLS-K had a higher proportion of full-time working mothers (46.9% vs. 32.6%) and a lower proportion of families under the federal poverty threshold (19.5% vs. 23.4%) than ECLS-B (Appendix 2).
Mean BMI and overweight and obesity by cohort and survey wave
Table 1 shows overall mean BMI and overweight and obesity prevalence by cohort and wave. Mean BMI of ECLS-K increased from 16.3 (2.2) kg/m2 at Kindergarten fall to 23.0 (5.2) kg/m2 at 8th grade. ECLS-B did not show a clinically considerable change in mean BMI (between 16.7 kg/m2 at preschool and 17.9 kg/m2 at 9 months).
Overweight and obesity rates ranged from 25.6% to 38.9% by age and cohort; the 5th graders had the highest prevalence (38.9%, Table 1). Hispanic boys and AA girls had the highest prevalence of overweight and obesity in most of the waves (e.g., Hispanic boy: 52.5%, AA girl: 49.1% at 5th grade [around the age of 11]) (Table 2).
Sex- and ethnic-specific BMI trajectory
Figure 1 shows sex- and ethnic-specific BMI trajectory curves from ages of 7 months to 16 years by the best fit mixed effect models using pooled data from the two cohorts (N = 29,250).
The BMI trajectories of different ethnic groups crossed each other several times between 7 months of age and 16 years old due to different ages of infancy peak and AR and BMI growth velocity between milestones. However, after AR, ethnic disparities on BMI trajectory became clear.
Overall, Hispanic boys and AA girls maintained the highest mean BMI after AR than did others of the same sex. The BMI curve of Asian boys showed a level-off tendency at 13.6 years of age.
Compared to the US CDC 2000 Growth Charts (2 to 20 years of age), the WHO 2006 Child Growth Standards (birth to 5 years of age), and WHO Reference 2007 (5–19 years of age), our fitted childhood BMI trajectories of US children were higher after infant peak.
Table 3 shows the diverse characteristics of BMI trajectory by sex and ethnicity. Hispanic boys and AA girls had a similarity of early AR (mean (SD) = 57.9 (7.8) and 59.0 (7.2) month) and high AUC (2724.5 (489.8) and 2681.2 (426.7) kg/m2*month) from AR to 16 years of age. AAs had the steepest increase in the BMI growth after AR (boy: 6.2 (1.5); girl: 7.0 (1.5) 10-2 kg/m2/month). Asian boys and girls had the earliest infancy peak compared to other ethnic groups. Their velocity and AUC from AR to 16 years of age were lower than those of Hispanic and AA children.
Factors associated with ethnic disparities in childhood BMI trajectory characteristics
As indicated in Table 4, overall, household SES level and child’s regular bedtime significantly influenced child BMI trajectory characteristics. Children with higher household SES and regular bedtimes were more likely to have later AR (e.g., 1.3 (0.3) month in the 3rd tertile vs. the 1st tertile in household SES; 1.4 (0.5) month when having bedtime rule vs. no rule, both p < 0.05; Model 4), lower BMI at AR, lower velocity and AUC between AR and 16 years of age.
After adjusting for covariates, AA children had the earliest age of AR and steepest BMI growth, and Hispanic children had the largest AUC between adiposity and 16 years of age (Model 1). Adjustment of household SES and to a lesser extent, a family routine for child’s bedtime, led to substantial reductions in ethnic disparities in childhood BMI trajectory characteristics (Models 2–4 in Table 4). These reductions were consistently the largest in Hispanic children (Appendix 3). For example, their 16.9% of age at AR difference, 38.5% of velocity difference and 18.5% of AUC difference between AR and 16 years of age compared to those in White children were attenuated by household SES and child’s regular bedtime (AA: 8.0, 5.5, 11.0%, respectively, Appendix 3).
Asian children had the latest age at AR and lowest BMI growth velocity from adiposity to 16 years of age. The differences in these characteristics between Asians and whites were not mediated by household SES or child’s regular bedtime (Table 4 and Appendix 3).
Discussion
For the first time, using unique data from two large nationally representative cohorts, we constructed the recent US children’s BMI trajectory curves from ages of 7 months to 16 years. We reported considerable ethnic disparities in BMI trajectories and obesity rates. Hispanic boys and AA girls maintained the highest overweight and obesity rate and mean BMI after AR vs. others of the same sex. The ethnic disparities in BMI trajectory characteristics became attenuated significantly after adjusting for individual household SES level and child’s regular bedtime. In particular, the difference between White children and Hispanic children was largely mediated by household SES. Childhood BMI levels including obesity status track into adulthood and childhood BMI affect later chronic disease risks [24,25,26].
However, due to the nature of fluctuation in childhood BMI curve and the lack of data sets with repeated anthropometric measurements from infancy to adolescence, only few studies have been able to identify individual’s BMI milestones in relation to later risk of obesity, including infancy peak, AR, and some features of BMI change [12,13,14,15,16]. Evidence from these studies has indicated that children with early AR, fast increase in BMI and longer exposure to high BMI are at increased risk for subsequent obesity. In particular, AAs and Hispanics showed this adverse characteristics in BMI trajectory from early ages [7, 14, 27], and have been identified as the ethnic groups with the highest risk of childhood obesity in the US [28,29,30].
Our study also found that AA children had all of the adverse BMI trajectory characteristics after adjusting for the effects of child sex, household SES level, children’s regular bedtime, and other covariates. In contrast, as the second most adverse group for childhood BMI trajectory characteristics, Hispanics had the largest attenuation of the differences between their BMI trajectory characteristics and those of White children after adjusting for the effects of household SES and the child’s regular bedtime (e.g., 38.5% of Hispanic-White difference in BMI growth velocity from AR to 16 years old).
Moreover, for all ethnic groups, household SES had a larger mediating contribution on BMI disparities than did child’s regular bedtime. Previous evidence also supports that ethnic disparities in obesity could be substantially due to household SES status (e.g., 38% of Black-White differences in risk of overweight/obesity was reduced after adjustment for educational level and income) [31], especially in Hispanic children (e.g., attenuated AAs-Whites and Hispanics-Whites difference in BMI Z-score after adjusting for parental and household socio-economic factors: Hispanics: 37.7%, AAs: 27.1%) [7]. A US study reported that among the independent contribution of socio-demographic, cultural and family routine factors to observed disparities in childhood BMI and obesity, disparities for Hispanic children were explained by socio-economic disadvantage [32]. Further studies are needed to examine the underlying mechanisms of adverse BMI trajectory characteristics in AA children.
We found that Asian American children had the healthiest BMI trajectory among all ethnic groups in the US. They had the latest AR and slowest BMI growth from AR to 16 years of age. Other studies also reported that Asian children had the healthiest BMI in the US [27, 33]. In particular, Asian boys show decreased BMI at the end of the BMI curve (0.03 lower after 190 months compared to 189 months in our study). Similarly, Chinese boys’ BMI curve has a lower and level-off tendency after age 15 [34]. However, the relatively small sample size of Asian boys of older ages in our sample may affect the robustness of our results.
In general, our findings suggested that low-SES US children had a higher risk for developing obesity [10, 11]. We also found parenting practices on children’s bedtime seemed to affect childhood BMI in all ethnic groups. Another longitudinal study of US children found that low parental income and education were risk factors for gradual onset of overweight after beginning kindergarten (OR (95% CI) of overweight: 0.91 (0.82–1.0) by logged base year income; 0.59 (0.47–0.74) in college vs. high school degree) [10]. Parental education can be related to health knowledge and lead to better daily routines for children (e.g., appropriate bedtime, balanced meals) [35]. On the other hand, the potential influences of household income could be bidirectional: families with greater household incomes may spend more money on children’s access to healthier foods and recreational activities, or they may buy a greater variety of foods and smart screen devices for their children, with the latter causing excessive calorie intake and more sedentary time [36]. Nevertheless, results from previous studies suggest that childhood BMI is affected by household SES [7, 11]. Efforts to reduce ethnic disparities in obesity should focus on preventing early life risk factors related to socio-demographic characteristics and parenting practices.
All of our sex- and ethnic-specific mean BMIs for these ECLS US children are higher than those of the 2000 US CDC Growth Charts (describe the growth of children in the US based on data collected during 1963–1994 [37]), the WHO 2006 Child Growth Standards (based on data collected from six countries during 1997–2003 with optimal growth environment [34]) and WHO Reference 2007 (developed based on data collected in the US and the WHO 2006 Child Growth Standards [37]). US children have relatively higher mean BMIs than those of the old reference/standards, which were comprised of earlier birth cohorts and breastfed children in other countries. In addition, different modeling methods could cause differences between results for the current study and the previous reference/standards (which used a variant of the lambda-mu-sigma (LMS) statistical method with data specific statistical smoothing techniques [37]).
This study had some limitations, including no consideration of biological, cultural or environmental determinants of obesity, considerable attrition with child age in both cohorts, and few parenting practices as risk factors for obesity disparities. Another limitation was the use of combined household SES Z-scores within the study population, which did not allow us to estimate the individual effects of parental education, occupation, and household income independently.
Nevertheless, this study is the first to define ethnic disparities in childhood BMI trajectory with visualization as well as parameterized BMI trajectory characteristics using the most recent nationally representative cohort data for the US, which yielded a large analytic sample. Also, we found the mediating effects of parenting practice (i.e., regular bedtime) and household SES level on ethnic disparities in child BMI trajectory, which could potentially contribute to prevention and intervention efforts to reduce ethnic disparities in childhood obesity.
In conclusion, among children in the US, ethnic disparities in obesity rates and BMI trajectory are large and become apparent after adiposity rebound. Hispanic boys and African-American girls have unfavorably higher BMI and obesity rates when compared to other groups. Household SES level and parenting practice seem to contribute to the disparities. Efforts to reduce disparities in childhood obesity should focus on modifiable risk factors including parenting.
Disclaimer
The content of the paper is solely the responsibility of the authors and does not necessarily represent the official views of the funder.
References
Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5(Suppl 1):4–104.
Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A potential decline in life expectancy in the United States in the 21st century. New Engl J Med. 2005;352:1138–45.
Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? estimating the progression and cost of the US obesity epidemic. Obes (Silver Spring). 2008;16:2323–30.
Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–14.
Taveras EM, Gillman MW, Kleinman KP, Rich-Edwards JW, Rifas-Shiman SL. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA Pediatr. 2013;167:731–8.
Dixon B, Pena MM, Taveras EM. Lifecourse approach to racial/ethnic disparities in childhood obesity. Adv Nutr. 2012;3:73–82.
Parkes A, Sweeting H, Young R, Wight D. Does parenting help to explain socioeconomic inequalities in children’s body mass index trajectories? Longitudinal analysis using the Growing Up in Scotland study. J Epidemiol Community Health. 2016;70:868–73.
Balistreri KS, Van Hook J. Trajectories of overweight among US school children: a focus on social and economic characteristics. Matern Child Health J. 2011;15:610–9.
Morris TT, Northstone K, Howe LD. Examining the association between early life social adversity and BMI changes in childhood: a life course trajectory analysis. Pediatr Obes. 2016;11:306–12.
Guo SS, Huang C, Maynard LM, Demerath E, Towne B, Chumlea WC, et al. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. Int J Obes Relat Metab Disord. 2000;24:1628–35.
Siervogel RM, Roche AF, Guo SM, Mukherjee D, Chumlea WC. Patterns of change in weight/stature2 from 2 to 18 years: findings from long-term serial data for children in the Fels longitudinal growth study. Int J Obes. 1991;15:479–85.
Wen X, Kleinman K, Gillman MW, Rifas-Shiman SL, Taveras EM. Childhood body mass index trajectories: modeling, characterizing, pairwise correlations and socio-demographic predictors of trajectory characteristics. BMC Med Res Methodol. 2012;12:38.
Silverwood RJ, De Stavola BL, Cole TJ, Leon DA. BMI peak in infancy as a predictor for later BMI in the Uppsala Family Study. Int J Obes (Lond). 2009;33:929–37.
Chivers P, Hands B, Parker H, Beilin L, Kendall G, Bulsara M. Longitudinal modelling of body mass index from birth to 14 years. Obes Facts. 2009;2:302–10.
Tourangeau K, Nord C, Lê T, Sorongon AG, Najarian M. Early Childhood Longitudinal Study, kindergarten class of 1998–99 (ECLS-K), combined user’s manual for the ECLS-K eighth-grade and K–8 full sample data files and electronic codebooks (NCES 2009–004). Washington, DC: National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education; 2009.
The US CDC 2000 Growth Charts. Defining childhood obesity. [19 Jul 2016]. Available from: https://www.cdc.gov/obesity/childhood/defining.html.
Jensen SM, Ritz C, Ejlerskov KT, Molgaard C, Michaelsen KF. Infant BMI peak, breastfeeding, and body composition at age 3 y. Am J Clin Nutr. 2015;101:319–25.
Hof MH, Vrijkotte TG, de Hoog ML, van Eijsden M, Zwinderman AH. Association between infancy BMI peak and body composition and blood pressure at age 5-6 years. PLoS ONE. 2013;8:e80517.
Wang Y. Epidemiology of childhood obesity--methodological aspects and guidelines: what is new? Int J Obes Relat Metab Disord. 2004;28(Suppl 3):S21–8.
Rolland-Cachera MF, Deheeger M, Maillot M, Bellisle F. Early adiposity rebound: causes and consequences for obesity in children and adults. Int J Obes (Lond). 2006;30(Suppl 4):S11–17.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82.
Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76:653–8.
Raitakari OT, Juonala M, Kahonen M, Taittonen L, Laitinen T, Maki-Torkko N, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–83.
Janssen I, Katzmarzyk PT, Srinivasan SR, Chen W, Malina RM, Bouchard C, et al. Utility of childhood BMI in the prediction of adulthood disease: comparison of national and international references. Obes Res. 2005;13:1106–15.
Guerrero AD, Mao C, Fuller B, Bridges M, Franke T, Kuo AA. Racial and ethnic disparities in early childhood obesity: Growth trajectories in body mass index. J Racial Ethn Health Disparities. 2016;3:129–37.
Claire Wang Y, Gortmaker SL, Taveras EM. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976-2006. Int J Pediatr Obes: IJPO: Off J Int Assoc Study Obes. 2011;6:12–20.
Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obes (Silver Spring). 2006;14:301–8.
Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303:242–9.
Wang Y, Chen X. How much of racial/ethnic disparities in dietary intakes, exercise, and weight status can be explained by nutrition- and health-related psychosocial factors and socioeconomic status among US adults? J Am Diet Assoc. 2011;111:1904–11.
Zilanawala A, Davis-Kean P, Nazroo J, Sacker A, Simonton S, Kelly Y. Race/ethnic disparities in early childhood BMI, obesity and overweight in the United Kingdom and United States. Int J Obes (Lond). 2015;39:520–9.
Centers for Disease CP. Obesity prevalence among low-income, preschool-aged children-United States, 1998-2008. MMWR Morb Mortal Wkly Rep. 2009;58:769–73.
Ji CY. Working Group on Obesity in C. Report on childhood obesity in China (1)--body mass index reference for screening overweight and obesity in Chinese school-age children. Biomed Environ Sci. 2005;18:390–400.
Cochrane SH, Leslie J, O’Hara DJ. Parental education and child health: intracountry evidence. Health Policy Educ. 1982;2:213–50.
Roberts JD, Rodkey L, Ray R, Knight B, Saelens BE. Electronic media time and sedentary behaviors in children: Findings from the Built Environment and Active Play Study in the Washington DC area. Prev Med Rep. 2017;6:149–56.
Centers for Disease Control and Prevention. Use of World Health Organization and CDC Growth Charts for children aged 0-59 months in the United States. MMWR Morb Mortal Wkly Rep. 2010;59(RR-9):1–13.
Acknowledgements
The present study is funded in part by a research grant from the US National Institutes of Health (NIH), the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD, 1R01HD064685-01A1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Min, J., Wen, X., Xue, H. et al. Ethnic disparities in childhood BMI trajectories and obesity and potential causes among 29,250 US children: Findings from the Early Childhood Longitudinal Study-Birth and Kindergarten Cohorts. Int J Obes 42, 1661–1670 (2018). https://doi.org/10.1038/s41366-018-0091-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0091-4
- Springer Nature Limited
This article is cited by
-
Body Mass Index Trajectories among the Healthy Communities Study Children: Racial/Ethnic and Socioeconomic Disparities in Childhood Obesity
Journal of Racial and Ethnic Health Disparities (2024)
-
BMI Growth Profiles Among Black Children from Immigrant and US-Born Families
Journal of Immigrant and Minority Health (2024)
-
Racial and Ethnic Disparities in Childhood Growth Trajectories
Journal of Racial and Ethnic Health Disparities (2022)
-
Adherence to index-based dietary patterns in childhood and BMI trajectory during the transition to adolescence: the EPOCH study
International Journal of Obesity (2021)
-
Longitudinal trajectories of adiposity-related measures from age 2–5 years in a population of low-income Hispanic children
Pediatric Research (2021)