Abstract
Background:
The prevalence of vitamin D (vitD) deficiency presenting as rickets is increasing worldwide. Insufficient sun exposure, vitD administration, and/or calcium intake are the main causes. However, vitD system-related genes may also have a role.
Methods:
Prospective study: 109 rachitic children completed a 6-mo study period or until rachitic manifestations disappeared. Thirty children were selected as controls. Clinical and biochemical data were evaluated at baseline in patients and controls and biochemistry re-evaluated at radiological healing. Therapy was stratified in three different protocols. Fifty-four single-nucleotide polymorphisms (SNPs) of five vitD system genes (VDR, CP2R1, CYP27B1, CYP24A1, and GC) were genotyped and their association with clinical and biochemcial data was analyzed.
Results:
Therapy response was similar in terms of radiological healing although it was not so in terms of biochemical normalization. Only VDR gene (promoter, start-codon, and intronic genotypes) was rickets-associated in terms of serum 25-OH-D, calcium, radiological severity and time needed to heal. Eight patients with sufficient calcium intake and 25-OH-D levels carried a VDR genotype lacking minor allele homozygous genotypes at SNPs spread along the gene.
Conclusion:
Although patients presented epidemiologic factors strongly contributing to rickets, genetic modulation affecting predisposition, severity, and clinical course is exerted, at least in part, by VDR gene polymorphic variation.
Similar content being viewed by others
Main
The prevalence of vitamin D (vitD) deficiency presenting as rickets in children is increasing worldwide owing to insufficient vitD intake and lack of exposure to sunlight. However, considering that relatively few children with low serum 25-hydroxyvitamin D (25-OH-D) levels have symptoms, genetic factors may additionally be linked to the manifestation of vitD deficiency and rickets (1).
As natural food contains scant amounts of vitD, humans naturally obtain vitD through precursor photosynthesis of UVB-dependent vitamin D3. Sunlight exposure and skin pigmentation are therefore main determinants of circulating vitD levels (2) that can be increased through dietary vitD intake (3). Interindividual differences in aspects of the vitD endocrine system have been well documented. They could be caused by genetic differences in important proteins in the vitD endocrine system, such as VDR (4,5,6).
Multiple polymorphic variations exist in the VDR gene: 5’-promoter variations can affect mRNA expression patterns and levels while 3’-UTR sequence variations can affect mRNA stability and/or protein translation efficiency (7,8,9,10). Other genes encoding proteins in the vitD endocrine system (25-hydroxylase (CP2R1), 1-α-hydroxylase (CYP27B1), 24-hydroxylase (CYP24A1), and vitamin D binding globulin (GC)) also present polymorphic variations that could influence vitD synthesis efficiency and circulating 25-OH-D circulating levels (9).
It has long been speculated that genetic predisposition may influence the manifestations of vitD deficiency. Accordingly, in a prospective series of rickets patients, we attempted to analyze the role of genotypes of VDR and other genes related to the vitD system on rickets predisposition, severity, and response to therapy.
Methods
Patients and Controls
Rachitic infants and children attending the Pediatric Outpatient Clinic, Ain Shams University, Cairo, Egypt (latitude 30.01N) were included. Participation was voluntary and written informed consent was obtained from parents or guardians. The study protocol was approved by the Ethics Committee of the University.
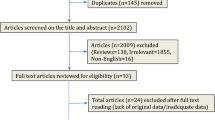
This was a prospective study: 168 consecutive rachitic patients presenting within a time frame of 12 mo were included (recruitment period included winter and summer, as the sun is shining all the year round in Egypt). Only 109 children either completed the 6-mo follow-up period or continued on treatment until their rachitic manifestations disappeared.
Inclusion criteria included clinical and radiological evidence of rickets and age from 7 mo to 3 y. Children were excluded if they had taken vitD or calcium supplements during the 6 mo prior to the study, if they had a history of kidney disease, tuberculosis, liver disease, prematurity, intestinal, cardiac, central nervous system, or other chronic disease. Bone disease (with the exclusion of rickets) or a history of hereditary forms of rickets together with weight <60% of the mean weight for height were also exclusion criteria.
Thirty age- and sex-matched children were selected as controls from siblings of nonrachitic patients attending the outpatient clinic or children with minor illnesses such as upper respiratory tract infections.
Data Collection
Nutritional data collection included: type of feeding, whether breast fed or not, duration of breast feeding, and weaning. Dietary calcium and caloric intake were calculated according to a food frequency questionnaire based on the pattern of diet in Egypt and compiled by the National Nutrition Institute (11). Calcium insufficiency was arbitrarily defined as an intake <50% of the recommended dietary allowance (RDI) (12). Parents were asked to report the whole dietary intake in detail on the preceding day on two separate occasions.
Nutritional status was determined according to the Wellcome Trust Classification (13).
Sunlight exposure evaluation included children’s type of clothing and time spent outdoors every day. Sun exposure of 2 h per week on the face and hands was considered sufficient to maintain normal 25-OH-D concentrations (14). The amount of sun exposure was measured by calculating the total body surface area exposed to the sun while wearing usual clothes using the Lund and Browder charts (15). Exposure duration was calculated by finding the average time spent outdoors per week (in hours) during the period of direct sunlight (0900–1500 h), where sun exposure index = hours of sun exposure per week × fraction of body surface area exposed to sunlight (16).
Assessment of socioeconomic status was done according to the criteria of El-Bohy (17), based on: paternal profession, educational level, type of housing, family income, income source (regular or irregular).
Patient Classifications and Therapeutic Groups
Patients were stratified from the start in three groups according to adequacy of sun exposure and calcium intake. The aim was to determine whether by history alone, the cause of nutritional rickets could be established and the appropriate treatment chosen.
Group 1: Thirty patients with adequate sun exposure (sun exposure ≥2 h/week) and inadequate calcium intake (<50% RDI). They received calcium supplementation (calcium carbonate) alone (40 mg elemental calcium/kg/day (if less than 1 y old) and 50 mg/kg/d (if older than 1 y) divided into two daily doses, PO) for 6 mo or till healing occurred.
Group 2: Forty-one patients with inadequate sun exposure (sun exposure <2 h/week) and inadequate calcium intake (<50% RDI). These patients received vitD (vitamin D3) as Stoss therapy (600,000 units IM) once, plus calcium supplementation (40 mg elemental calcium/kg/day (if less than 1 y old) and 50 mg/kg/d (if older than 1 y) divided into two daily doses, PO) for 6 mo or till healing occurred.
Group 3: Thirty-eight patients with inadequate sun exposure (sun exposure <2 h/week) and adequate calcium intake (≥50% RDI). These patients received vitD as Stoss therapy (600,000 units IM) once, plus calcium supplementation (40 mg elemental calcium/kg/d (if less than 1 y old) and 50 mg/kg/d (if older than 1 y) divided into two daily doses, PO) for 2 wk.
A subgroup of eight patients from Group 3 was characterized as having adequate calcium intake and sufficient 25-OH-D levels (≥20 ng/ml) despite inadequate sun exposure. This subgroup was separately analyzed for genotype characteristics.
Auxology
Length or height and weight were measured and the SD scores (SDS) for length or height and for weight for length/height were calculated (18).
Biochemical Measurements
In cases and controls, serum calcium, phosphorus, and alkaline phosphatase (ALP) were measured photometrically using Hitachi 917 autoanalyzer and Roche reagents. In patients, they were determined at diagnosis, 2 wk after the start of treatment and then monthly till healing (an X-ray score of zero). ALP level was considered normal if ≤471 IU/l (according to levels in age-matched controls with 99.1% sensitivity and 100% specificity).
Serum 25-OH-D was measured by an enzyme-linked immunoassay method (Immunodiagnostik AG, Bensheim, Germany). The detection limit of the assay was 2.24 ng/ml.
Intact PTH was assayed by enzyme-linked immunoassay using reagents supplied by Biosource (Biosource Europe SA, Nivelles, Belgium). Assay sensitivity was 2 pg/ml (range 15–1,040 pg/ml).
In patients, 25-OH-D and intact PTH were measured in baseline samples and again at the end of the study (X-ray score of zero). In controls, 25-OH-D and intact PTH were measured in baseline samples.
Radiological Evaluation
Assessment of rickets severity was made using standard X-rays of both wrists and knees. A 10-point scoring system was used (zero “normal”) to a maximum score of 10 (19). Radiographs were examined by two independent observers and the score was taken as the mean of their scores. X-ray scores were determined at baseline, 2 wk after the start of treatment and then monthly till radiological healing. The criterion for healing was an X-ray score of zero and time to healing was calculated as months needed to achieve a null X-ray score.
Vitamin D System Gene Polymorphisms
Genotyping of 28 single-nucleotide polymorphisms (SNP) of VDR ( Table 1 ), 4 SNPs of CP2R1 (25-hydroxylase: rs10741657, rs12794714, rs10500804 and rs1993116), 1 SNP of CYP27B1 (1-α-hydroxylase: rs4646536), 10 SNPs of CYP24A1 (24-hydroxylase: rs4809960, rs2181874, rs6022994, rs6022993, rs912505, rs751089, rs1570670, rs927651, rs927650, and rs4809957), and 11 SNPs of GC (vitamin D binding globulin: rs222020, rs222016, rs1491719, rs4364228, rs4752, rs222035, rs7041, rs4588, rs2298850, rs3755967, and rs2282679), was performed using Applied Biosystems TaqMan and OpenArray technologies (Life Technologies, Carlsbad, CA).
Statistical Analysis
JMP 7.01 (SAS Institute, Cary, NC) was used for data entry and analysis. Numeric variables were expressed as mean ± SD when normally distributed and as median and interquartile range when nonparametric. Comparison of variables between groups was made using Student’s t-test and Mann Whitney U-test for normal and nonparametric variables, respectively. Multiple subgroups were compared using Kruskall Wallis test. Chi-square (χ2) test was used to compare the frequency of qualitative variables among the different groups. Spearman’s correlation test was used to correlate nonparametric variables. Genotype frequencies were compared among groups by χ2 Pearson test. In the entire rickets population, a stepwise regression analysis was applied to predict the contribution of VDR genotypes to baseline serum 25-OH-D and calcium levels, baseline X-ray score and time to radiologic healing, and ALP normalization. A P value < 0.05 was considered statistically significant for all tests.
Results
Demographic and Biochemical Characteristics of the Three Groups
The demographic, anthropometric, and biochemical characteristics of patients (at diagnosis and after healing) and controls are shown in Table 2 .
At diagnosis, in the whole rickets population, serum calcium correlated positively with height-SDS (r2 = 0.02; P = 0.03), sun exposure (r2 = 0.13; P < 0.0001), calcium intake (r2 = 0.11; P < 0.0001) and serum phosphorus (r2 = 0.03; P = 0.01), and negatively with serum PTH (r2 = −0.04; P = 0.008) and ALP (r2 = −0.06; P = 0.001); serum 25-OH-D correlated positively with sun exposure (r2 = 0.25; P < 0.0001), calcium intake (r2 = 0.04; P = 0.008) and serum phosphorus (r2 = 0.03; P = 0.0003) and negatively with serum PTH (r2 = −0.13; P < 0.0001) and ALP (r2 = −0.08; P = 0.03); radiological score correlated positively with serum ALP (r2 = 0.11; P = 0.0002).
The time elapsed to achieve an X-ray score of zero (healing) did not differ among the three therapeutic groups. At healing, serum calcium, phosphorus, and 25-OH-D were significantly higher and ALP significantly lower in groups 2 and 3 compared to group 1; PTH did not differ among groups ( Table 2 ). However, time to ALP normalization differed significantly among groups, with group 1 needing the longest time ( Table 2 ).
Vitamin D System Gene Frequencies
Only two VDR genotype frequencies showed statistically significant differences among patient and control groups: in group 1 compared to groups 2 and 3 and controls, major allele homozygous genotypes at VDR-18 (rs7305032) and VDR-21 (rs2525044) were increased and minor allele homozygous genotypes were absent ( Figure 1a , c ). VDR-18 and VDR-21 were in linkage disequilibrium (96.7%). Allele frequencies were significantly different ( Figure 1b , d ), with group 1 presenting increased frequency of the T and C alleles at VDR-18 and VDR-21, respectively, compared to groups 2 and 3 and controls.
VDR-18 and VDR-21 genotype and allele frequencies in control and the three rickets patient groups. (a) VDR-18 genotype frequencies in control and the three rickets patient groups. In rickets 1 group, the major allele homozygous genotype (TT) is significantly increased (P = 0.02) and the minor allele homozygous genotype (CC) is absent. (b) Allele frequencies at VDR-18 in rickets and control groups. Major allele T is significantly increased in rickets 1 group (P < 0.0001). (c) VDR-21 genotype frequencies in control and the three rickets patient groups. In rickets 1 group, the major allele homozygous genotype (CC) is significantly increased (P = 0.03) and the minor allele homozygous genotype (TT) is absent. (d) Allele frequencies at VDR-21 in rickets and control groups. Major allele C is significantly increased in rickets 1 group (P < 0.0001).
Vitamin D System Genotype Association With Clinical Data
Only VDR genotypes showed several significant associations with clinical data.
In the entire rickets population, stepwise regression analysis between VDR genotypes and baseline 25-OH-D, calcium and X-ray score, and time to radiologic healing and ALP normalization showed that:
-
Baseline 25-OH-D was significantly associated with genotypes at three VDR promoter SNPs (VDR-3, VDR-4, and VDR-9), explaining 29% of variation with the minor allele AA genotype at VDR-3 and the major allele TT genotypes at VDR-4 and VDR-9 presenting the lowest 25-OH-D levels ( Table 3 ).
Table 3 Association between VDR genotypes and baseline data in rickets patients -
Baseline calcium was significantly associated with genotypes at eight VDR SNPs (two in the promoter region and six intronic), explaining 54% of variation ( Table 3 ). VDR-9 and -10 (77.2%), VDR-18 and -21 (96.7%), and VDR-23 and -24 (57.1%) were in linkage disequilibrium. Homozygous minor allele combined genotypes at VDR-18 and VDR-21 were associated with the lowest calcium (CCTT = 6.5 ± 1.5 mg/dl; n = 6), the heterozygotes had intermediate concentrations (TCTC = 8.0 ± 1.1 mg/dl; n = 42) (P = 0.0026) and the major allele homozygous presented the highest values (TTCC = 8.4 ± 1.0 mg/dl; n = 56) (P = 0.0001).
-
X-ray score was associated (37%) with genotypes at VDR-12 (rs2228570, start codon, Fok1) and VDR-18 (rs7305032, intron 5). The lowest scores were associated with the VDR-12 minor allele homozygous TT and the VDR-18 minor allele homozygous CC genotypes ( Table 3 ).
-
Time to radiologic healing was only associated (12%) with genotype at intron 8 VDR-24 SNP (rs7975232, Apa1), with the minor allele homozygous genotype GG showing the shortest time ( Table 3 ).
-
Time to ALP normalization was associated (22%) with genotypes at VDR promoter (VDR-7) and intron 8 (VDR-24, rs7975232, Apa1), with the minor allele homozygous genotype GG showing the shortest time ( Table 3 ).
The subgroup of patients from Group 3 with sufficient calcium intake (>50% RDI) and 25-OH-D levels (≥20 ng/ml) consisted of eight patients. They only differed from all other patients by age (0.8 ± 0.3 vs. 1.4 ± 0.6 y; P = 0.002), calcium intake (128.4 ± 71.6 vs. 49.7 ± 40.2%RDI; P = 0.0002), and 25-OH-D serum levels (27.9 ± 5.9 vs. 19.1 ± 13.3; P = 0.019). This subgroup was genetically different from the rest because all lacked the minor allele homozygous genotypes at VDR-3 (AA), -4 (CC), -6 (AA), -9 (CC), -10 (TT), -12 (TT), -13 (CC), -14 (TT), -17 (CC), and -27 (TT).
Discussion
The present study was designed to ascertain the epidemiological and genetic factors involved in rickets development and therapy response in young Egyptian children.
The therapeutic results in terms of time to healing according to the X-ray score were similar in the three treatment groups, indicating that elucidating the cause of rickets by history-taking and the subsequent treatment were similarly effective. However, it was not so in terms of time to ALP normalization, which was longer in group 1, and clinical data at X-ray score normalization demonstrated a poorer biochemical profile in terms of serum calcium, phosphorus, ALP and 25-OH-D (although only 3 of 30 patients in group 1, treated with calcium alone, presented 25-OH-D levels between 14 and 15 ng/ml; data not shown). In groups 2 and 3, 25-OH-D levels reached a maximum concentration of 140 ng/ml with no signs of toxicity.
With a view to establishing whether socioeconomic and nutritional factors accounted fully for the development of rickets in Egyptian children, we also aimed to ascertain whether genetic variations in several genes of the vitD system could predispose to or modify the clinical course.
Several epidemiological studies have analyzed the impact of genetic variation on vitD insufficiency determination: Suaini et al. (20) described increased frequency of vitD insufficiency in carrier children of a minor allele in 6 vitamin D binding globulin gene (GC) SNPs, comprising 4 of the SNPs analyzed in the present study. However, our study detected no genotype frequency difference among groups or any association with clinical and biochemical data for the CPR2, CYP27B1, CYP24A1, and GC SNPs analyzed. Only VDR proved to be associated with rickets and several promoter and intronic VDR genotypes were associated with baseline serum 25-OH-D and calcium, X-ray score and time to radiologic healing and ALP normalization.
At diagnosis, up to 29% of serum 25-OH-D levels could be explained by genotypes at three VDR promoter SNPs: VDR-3 (rs11568820, Cdx2), VDR-4 (rs4760658), and VDR-9 (rs2853564). VDR-3 is located at the site interacting with the intestinal-specific transcription factor Cdx2, which has been investigated for its association with BMD and fracture risk: individuals that are homozygous GG have lower BMD than homozygous AA individuals (21), the A allele has a protective effect on fracture risk (22,23) and the G allele has diminished transcriptional activity (21). In our rickets patients, the minor allele homozygous AA (n = 7) presented the lowest 25-OH-D levels, although they normalized ALP levels in the shortest time (AA = 1.9 ± 1.1; GA = 2.5 ± 1.3; GG = 3.1 ± 1.4 mo; P = 0.025). These results concur with recently published data in Chinese women in whom serum 25-OH-D was highest in GG carriers and lowest in the AA (24). VDR-4 and VDR-9 minor allele homozygous CC genotypes showed the highest 25-OH-D levels. The three VDR promoter genotypes had been included together with several skin color-genes in two multilocus networks identified as displaying strong latitudinal clines (6). VDR-3 was included together with two other VDR promoter (VDR-7 and -8) and MC1R, SLC24A5, and SLC45A2 genotypes in a network showing the strongest cline with population geographical origin latitudes, and the three VDR promoter SNP haplotype showed a dramatic in- vs. out-of Africa frequency pattern, with a frequency of 0.2 in sub-Saharan Africa, and an average frequency of 0.9 with no latitudinal association outside of Africa. The haplotype containing VDR-3 G allele (linked to higher 25-OH-D in our present study) showed the lowest frequency in dark skin Sub-Saharan populations, highest in light skin European populations and intermediate in Egyptian. VDR-4 and -9 were included with two other skin color-genes (TYR and TYRP1) in another network showing a significant linear regression against latitude (6). The haplotype containing the VDR-4 and VDR-9 T allele (linked to lower 25-OH-D levels in our present study) presented the highest frequency in dark skin populations and the lowest in the light skin ones. These previously published results demonstrated that VDR promoter adapted with skin color genes to the need to use ultraviolet (UVR) for vitamin D synthesis or to protect from intense UVR radiation (6). Egyptian rickets children presenting the lowest 25-OH-D levels had VDR-3, -4, and -9 promoter genotypes that are more frequent in dark skin populations, although Egyptian rickets patients and controls in the present study had similar skin colors (light brown).
At diagnosis, 54% of serum calcium could be explained by genotypes at eight VDR SNPs, two in the promoter region and six intronic. Promoter VDR-9 and VDR-10 (77% linked) genotypes showed the lowest calcium in parallel with the lowest 25-OH-D levels and these haplotypes were included, as previously indicated, together with several skin color genes in a network showing a significant linear regression against latitude (6). Intronic VDR-14 (rs2238138) and VDR-24 (rs7975232, Apa1 site) were also included in a haplotype network not associated with latitude, with the minor allele homozygous genotypes showing the lowest calcium levels. VDR-18 (rs7305032) and VDR-21 (rs2525044) (96.7% linked) were also included in another network with the minor allele homozygous genotypes carrying the lowest serum calcium levels, and this genotype was absent in rickets patients Group 1. This genotype may predispose patients to rickets and was absent in Group 1 patients who combined adequate sun exposure and insufficient calcium intake.
At diagnosis, X-ray score was associated to VDR-18 (see above) and VDR-12 (rs2228570, start codon, Fok1 site) with the minor allele homozygous TT genotype (ff according to Fok1 restriction enzyme site) at VDR-12 showing the lowest score. The TT genotype encodes a longer VDR protein which has been demonstrated to be transcriptionally less active (25), has been shown to be associated with higher concentrations of 25-OH-D (26) and was less frequent than in controls in our previously studied rickets population (27).
VDR-24 (rs7975232, Apa1 site) genotype was also significantly linked to time to radiologic healing and ALP normalization and the minor allele homozygous genotype (AA according to the Apa1 restriction enzyme site) presented the shortest time to healing. Intron 8 VDR-22 (BsmI) and VDR-24 (ApaI) genotypes were the first to be described as associated with bone mineral density (BMD) variation and their bb (GG nucleotides) and AA (GG nucleotides) genotypes had been shown to be associated with higher BMD values (28,29,30). The present study confirms that VDR-24 modulate serum calcium levels as well as bone involvement in a situation of clinical rickets. Other studies reported similar or different associations between VDR intronic genotypes and haplotype frequencies or clinical data: Kitanaka et al. (1) showed that some haplotype frequencies at VDR-22, -24, and -25 (among which was the VDR-22 B allele associated to the highest X-ray scores and the lowest 25-OH-D levels in our previous (27) and present studies) were increased in rickets patients compared to controls.
When different patient classification criteria were applied, in particular according to calcium intake adequacy and sufficiency of 25-OH-D serum levels, a subgroup of 8 patients emerged with the striking characteristics of presenting sufficient calcium intake and 25-OH-D levels despite inadequate sun exposure. In terms of VDR genotypes, they were the only ones to lack several of the minor allele homozygous genotypes at SNPs spread along the gene: five in the promoter region, one in the start codon, three intronic, and one in the 3’UTR region. The lacking genotype at VDR-3 (AA) encodes the most active protein in terms of intestinal calcium absorption and protection against fracture risk (21,22,23) and was associated with increased risk of T2DM (31), with lower 25-OH-D levels (24) and the lowest 25-OH-D levels in the present study. The lacking promoter genotypes at VDR-4, VDR-6, VDR-9, and VDR-10 are associated with the highest 25-OH-D and calcium levels in the present study. The lacking minor allele homozygous genotype (TT) at the start codon VDR-12 (rs2228570, FokI) encodes a longer and transcriptionally less active VDR (25), which has been shown to be associated with higher concentrations of 25-OH-D (26), was less frequent in our previously studied rickets population (27) and is associated with lower X-ray score in the present study.
These patients were the only ones in our study to present a lack of each of these minor allele homozygous genotypes, thus suggesting that their VDR genotype could have predisposed them to rickets in terms of low calcium, elevated PTH and bone disease, despite adequate calcium intake and 25-OH-D serum levels.
In summary, although Egyptian patients showed epidemiological factors strongly contributing to rickets such as low SEL and inadequate sun exposure and calcium intake, genetic modulation affecting predisposition and/or severity is exerted, at least in part, by VDR gene polymorphic variation.
Our study further strengthens the conclusion that rickets development, severity, and response to therapy in children depend not only on epidemiologic factors but also on genetic conditioning.
Author Contributions
All authors contributed substantially to the design, analysis, and interpretation of data. All authors provided important intellectual input in drafting or revising the manuscript.
Statement of Financial Support
This study was partly supported by a research grant from the Research Unit of the European Society for Pediatric Endocrinology to M.E.K. and L.A., the Instituto de Salud Carlos III, Madrid, Spain CIBERER U-712 to M.F.C., and the AGAUR (University and Research Management and Evaluation Agency), Barcelona, Spain (2009SGR31) to L.A.
Disclosure
The authors have nothing to disclose.
References
Kitanaka S, Isojima T, Takaki M, Numakura C, Hayasaka K, Igarashi T. Association of vitamin D-related gene polymorphisms with manifestation of vitamin D deficiency in children. Endocr J 2012;59:1007–14.
Jablonski NG, Chaplin G. Human skin pigmentation, migration and disease susceptibility. Philos Trans R Soc Lond B Biol Sci 2012;367:785–92.
Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol 2014;21:319–29.
Uitterlinden AG, Fang Y, van Meurs JB, van Leeuwen H, Pols HA. Vitamin D receptor gene polymorphisms in relation to Vitamin D related disease states. J Steroid Biochem Mol Biol 2004;89-90:187–93.
Lucock M, Yates Z, Martin C, et al. Vitamin D, folate, and potential early lifecycle environmental origin of significant adult phenotypes. Evol Med Public Health 2014;2014:69–91.
Tiosano D, Audi L, Climer S, et al. Latitudinal Clines of the Human Vitamin D Receptor and Skin Color Genes. G3 (Bethesda) 2016;6:1251–66.
Uitterlinden AG, Fang Y, Bergink AP, van Meurs JB, van Leeuwen HP, Pols HA. The role of vitamin D receptor gene polymorphisms in bone biology. Mol Cell Endocrinol 2002;197:15–21.
Saccone D, Asani F, Bornman L. Regulation of the vitamin D receptor gene by environment, genetics and epigenetics. Gene 2015;561:171–80.
Berlanga-Taylor AJ, Knight JC. An integrated approach to defining genetic and environmental determinants for major clinical outcomes involving vitamin D. Mol Diagn Ther 2014;18:261–72.
Uitterlinden AG, Fang Y, Van Meurs JB, Pols HA, Van Leeuwen JP. Genetics and biology of vitamin D receptor polymorphisms. Gene 2004;338:143–56.
National Nutrition Institute. Food Composition Tables for Egypt. 2nd edn. Cairo, ARE: National Nutrition Institute, 2006.
Baker SS, Cochran WJ, Flores CA, et al. American Academy of Pediatrics. Committee on Nutrition. Calcium requirements of infants, children, and adolescents. Pediatrics 1999;104(5 Pt 1):1152–7.
Wellcome Trust Working Party. Classification of infantile malnutrition. Lancet 1970;2:302–3.
Specker BL, Valanis B, Hertzberg V, Edwards N, Tsang RC. Sunshine exposure and serum 25-hydroxyvitamin D concentrations in exclusively breast-fed infants. J Pediatr 1985;107:372–6.
Lund CC, Browder NC. The estimation of areas of burns. Surg Gynaecol Obstet 1944;79:352–8.
Barger-Lux MJ, Heaney RP. Effects of above average summer sun exposure on serum 25-hydroxyvitamin D and calcium absorption. J Clin Endocrinol Metab 2002;87:4952–6.
El-Bohy FS. Tool for socioeconomic level. Journal of Modern Education 1983:434–43.
Tanner JM, Whitehouse RH, Takaishi M. Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. II. Arch Dis Child 1966;41:613–35.
Thacher TD, Fischer PR, Pettifor JM, Lawson JO, Manaster BJ, Reading JC. Radiographic scoring method for the assessment of the severity of nutritional rickets. J Trop Pediatr 2000;46:132–9.
Suaini NH, Koplin JJ, Ellis JA, et al.; HealthNuts Study Investigators. Environmental and genetic determinants of vitamin D insufficiency in 12-month-old infants. J Steroid Biochem Mol Biol 2014;144 Pt B:445–54.
Arai H, Miyamoto KI, Yoshida M, et al. The polymorphism in the caudal-related homeodomain protein Cdx-2 binding element in the human vitamin D receptor gene. J Bone Miner Res 2001;16:1256–64.
Uitterlinden AG, Ralston SH, Brandi ML, et al.; APOSS Investigators; EPOS Investigators; EPOLOS Investigators; FAMOS Investigators; LASA Investigators; Rotterdam Study Investigators; GENOMOS Study. The association between common vitamin D receptor gene variations and osteoporosis: a participant-level meta-analysis. Ann Intern Med 2006;145:255–64.
Fang Y, van Meurs JB, Bergink AP, et al. Cdx-2 polymorphism in the promoter region of the human vitamin D receptor gene determines susceptibility to fracture in the elderly. J Bone Miner Res 2003;18:1632–41.
Ling Y, Lin H, Aleteng Q, et al. Cdx-2 polymorphism in Vitamin D Receptor gene was associated with serum 25-hydroxyvitamin D levels, bone mineral density and fracture in middle-aged and elderly Chinese women. Mol Cell Endocrinol 2016;427:155–61.
Arai H, Miyamoto K, Taketani Y, et al. A vitamin D receptor gene polymorphism in the translation initiation codon: effect on protein activity and relation to bone mineral density in Japanese women. J Bone Miner Res 1997;12:915–21.
McGrath JJ, Saha S, Burne TH, Eyles DW. A systematic review of the association between common single nucleotide polymorphisms and 25-hydroxyvitamin D concentrations. J Steroid Biochem Mol Biol 2010;121:471–7.
Baroncelli GI, Bereket A, El Kholy M, et al. Rickets in the Middle East: role of environment and genetic predisposition. J Clin Endocrinol Metab 2008;93:1743–50.
Kiel DP, Myers RH, Cupples LA, et al. The BsmI vitamin D receptor restriction fragment length polymorphism (bb) influences the effect of calcium intake on bone mineral density. J Bone Miner Res 1997;12:1049–57.
Ferrari SL, Rizzoli R, Slosman DO, Bonjour JP. Do dietary calcium and age explain the controversy surrounding the relationship between bone mineral density and vitamin D receptor gene polymorphisms? J Bone Miner Res 1998;13:363–70.
Giguère Y, Rousseau F. The genetics of osteoporosis: ‘complexities and difficulties’. Clin Genet 2000;57:161–9.
Sentinelli F, Bertoccini L, Barchetta I, et al. The vitamin D receptor (VDR) gene rs11568820 variant is associated with type 2 diabetes and impaired insulin secretion in Italian adult subjects, and associates with increased cardio-metabolic risk in children. Nutr Metab Cardiovasc Dis 2016;26:407–13.
Acknowledgements
The authors would like to thank Shaheen KY (Clinical Pathology Department, Ain Shams University, Cairo, Egypt).
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
El Kholy, M., Elsedfy, H., Fernández-Cancio, M. et al. Nutritional rickets: vitamin D, calcium, and the genetic make-up. Pediatr Res 81, 356–363 (2017). https://doi.org/10.1038/pr.2016.222
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.222
- Springer Nature America, Inc.