Abstract
Background:
Given the potential importance of epithelial plasticity (EP) to cancer metastasis, we sought to investigate biomarkers related to EP in men with localized prostate cancer (PC) for the association with time to PSA recurrence and other clinical outcomes after surgery.
Methods:
Men with localized PC treated with radical prostatectomy at the Durham VA Medical Center and whose prostatectomy tissues were included in a tissue microarray (TMA) linked to long-term outcomes. We performed immunohistochemical studies using validated antibodies against E-cadherin and Ki-67 and mesenchymal biomarkers including N-cadherin, vimentin, SNAIL, ZEB1 and TWIST. Association studies were conducted for each biomarker with baseline clinical/pathologic characteristics an risk of PSA recurrence over time.
Results:
Two hundred and five men contributed TMA tissue and had long-term follow-up (median 11 years). Forty-three percent had PSA recurrence; three died of PC. The majority had high E-cadherin expression (86%); 14% had low/absent E-cadherin expression. N-cadherin was rarely expressed (<4%) and we were unable to identify an E-to-N-cadherin switch as independently prognostic. No associations with clinical risk group, PSA recurrence or Gleason sum were noted for SNAIL, ZEB1, vimentin or TWIST, despite heterogeneous expression between patients. We observed an association of higher Ki-67 expression with Gleason sum (P=0.043), National Comprehensive Cancer Network risk (P=0.013) and PSA recurrence (hazard ratio 1.07, P=0.016).
Conclusions:
The expression of EP biomarkers in this cohort of men with a low risk of PC-specific mortality was not associated with aggressive features or PSA relapse after surgery.
Similar content being viewed by others
Introduction
Localized prostate cancer (PC) is a heterogeneous disease, in which men have widely disparate outcomes based on key clinical and pathologic factors including Gleason sum, PSA levels, tumor stage and extent of invasion.1, 2 Current models of risk of recurrence or PC mortality after surgery are reasonably accurate at assessing long-term outcomes.1 However, some low and intermediate risk tumors still relapse, whereas some high-risk tumors may be cured with surgery alone and our ability to predict these discordant results is imperfect, illustrating the biologic heterogeneity even within well-defined risk categories.3 Thus, additional biomarkers of biologic aggressiveness in localized PC are needed.
Epithelial plasticity (EP), defined as the ability of cells to reversibly undergo phenotypic changes, may underlie the ability of many solid tumors, including PC, to disseminate and resist commonly used therapies, including surgery, radiation, hormonal therapies and chemotherapy.4, 5 During the loss of the more differentiated epithelial phenotype, cancer cells may upregulate stemness biomarkers6 or biomarkers of a mesenchymal or invasive phenotype,7 associated with an epithelial-to-mesenchymal transition (EMT). An EMT has been associated with metastatic risk in multiple tumor types, and PC cell lines and human metastases expressing EMT biomarkers appear to be more androgen receptor independent and aggressive.8 We have shown that circulating tumor cells from men with metastatic castration-resistant PC commonly express these plasticity biomarkers, indicating their potential importance in lethal disease,9 and others have shown that loss of epithelial biomarkers and/or an increase in mesenchymal or stemness biomarkers in localized PC may be associated with recurrent disease and PC mortality.6, 7, 10
Several studies have specifically analyzed mesenchymal biomarker expression in radical prostatectomy specimens, identifying an E- to N-cadherin switch,7 loss of cytokeratin or PSA expression,6, 11 gain of hedgehog or NOTCH signaling6 or gain of expression of the EMT transcriptional regulators TWIST and SNAIL,10 as adversely prognostic and independently associated with recurrent disease. However, others have not found associations between SNAIL or vimentin expression and clinical outcomes,12, 13 and currently EP biomarkers are not routinely assessed during the pathologic examination of the prostate. We thus sought to evaluate the association of EP biomarker expression in a contemporary series of men with localized PC treated with radical prostatectomy and who had long-term follow-up for recurrence.
Materials and methods
Patient population
The current cohort includes men with localized PC treated, with radical prostatectomy performed between 1993–2004 at the Durham Veteran’s Affairs (VA) Medical Center in Durham, NC. Clinical data were extracted and included in the Shared Equal Access Research Center Hospital database, under Duke University and Durham VA Medical Center Institutional Review Board approval. Data recorded included age, demographics, PSA levels at diagnosis and recurrence, prostatectomy pathologic characteristics, stage and National Comprehensive Cancer Network (NCCN) risk score, prior and subsequent therapies, biopsy information, and long-term recurrence, metastasis and survival outcomes. PSA recurrence was defined as a single PSA >0.2 ng ml−1, two values at 0.2 ng ml−1 or secondary treatment for a rising PSA prior to reaching 0.2 ng ml−1 and were typically followed every 6–12 months with serial PSA monitoring after surgery. Men who received adjuvant therapy with an undetectable PSA were censored for PSA recurrence at that time. A tissue microarray (TMA) on a random subset of patients in the Shared Equal Access Research Center database treated at the Durham VA was developed after institutional review board approval in which prostatectomy histologic sections were arrayed on slides for biomarker evaluation with four cores of cancer per patient on each microarray, along with benign-negative control tissues. We focused on the dominant highest grade lesion in a given patient for the TMA creation for biomarker development.
Antibodies and validation
We performed antibody optimization and analytic validation for all antibodies tested, determining the optimal concentration using both negative and positive control tissues prior to application to the TMA. Antibodies against E-cadherin, Ki-67, N-cadherin, vimentin, SNAIL1/2, TWIST and ZEB1 were evaluated in parallel with hematoxylin and eosin by an expert PC pathologist blinded to outcomes and other biomarker results (RV). Scoring of each biomarker followed an ordinal scale ranging from 0 to 2 (E-cadherin, ZEB1, vimentin) or 0 to 3 (SNAIL, TWIST) based on intensity and frequency of expression in each TMA section. The scoring range for each biomarker was selected by the pathologist based on the heterogeneity and range of expression between patients. Ki-67 was scored on a 0–100% scale based on frequency of expression in tumor cells. To account for tumor heterogeneity for each biomarker, four tumor containing TMA sections were obtained from radical prostatectomy tissue per patient, which was then linked back to the subject ID by a master code for clinical database association studies. For each biomarker, minimum and maximum expression levels per subject as well as average expression was associated with outcomes and pathologic/clinical features. Scoring of epithelial tumor cells rather than benign stroma was performed for all EP biomarkers. Table 1 provides a listing of each antibody used, the source and clone, isotype, positive and negative controls, and concentrations used.
Statistical methods and analysis plan
The primary objective was to assess the association of each EP biomarker with PSA recurrence over time. PSA recurrence was defined as the time from the date of RP to PSA recurrence, with an increase in recurrence hypothesized for higher levels of Ki-67 and mesenchymal biomarkers (SNAIL, TWIST, N-cadherin, vimentin), and lower levels of epithelial biomarkers (E-cadherin). Secondary objectives included the association of each EP biomarker with adverse clinical/pathologic characteristics (PSA, Gleason sum, NCCN risk, stage, survival and risk of metastasis). Descriptive statistics were generated for each marker. Patients who had not failed biochemically as of last follow-up were censored at time of last follow-up or death, whichever occurred first. Survival and recurrence was documented through annual updates to the Shared Equal Access Research Center database and chart review. The Kaplan–Meier approach was used to estimate the PSA recurrence and overall survival distributions. In addition, the proportional hazards model was used to determine the association between the markers and PSA recurrence. Univariate hazard ratios and 95% confidence intervals were estimated.
Results
Two-hundred and five men with localized PC were identified and included in this analysis who contributed tissue to the TMA. The median age was 63 years (range 47–73). Fifty percent of men were white and 48% of men were black. By D’Amico/NCCN risk classification, 47% were low risk, 33% intermediate risk and 20% high risk (Table 2). At surgery, 12 had Gleason 8–10 tumors, 67% were Gleason 7 and 21% were Gleason 6 or under. Fifteen percent had seminal vesicle invasion, 27% had extracapsular extension, and PSA at the time of surgery was a median of 7.4 (range 0.6–75.4). Over a median follow-up period of 11.3 years, 71 (35%) men died, with 3 men (1.4%) dying of metastatic PC out of 4 men (2%) who developed metastatic disease. Eighty-nine (43.4%) had biochemical (PSA) recurrence and 77 (38%) of men were treated with adjuvant or salvage radiation to the prostate bed. Fifteen percent of men (n=32) required androgen deprivation therapy at any time; however, no patients received androgen deprivation therapy prior to surgery. Table 2 provides demographic and clinical characteristics, and Supplementary Figure 1 shows the REMARK diagram for patient and specimen/biomarker analysis.
We initially examined Ki-67 as a biomarker of tumor proliferation rate, given the association of higher Ki-67 expression with recurrence and adverse pathology in multiple prior studies.14, 15, 16, 17, 18 Median Ki-67 expression was 2.5% (range 0–18.7%), whereas the median maximum Ki-67 expression was 4.7% (range 0–21.7%), and was evaluable in 178/205 men. Of these 178, we identified 14 men who had Ki-67 scores of 0, in which benign prostate tissue was likely scored in the present study, leaving 164 men evaluable for Ki-67 analysis (see Supplementary Figure 1 for REMARK diagram). Supplementary Figure 2 presents a spaghetti plot, demonstrating the variability of Ki-67 expression levels by site of the core on a per patient basis. Using the median maximum Ki-67 score (0–100% range) as a continuous variable, Ki-67 percentage was associated with PSA recurrence (hazard ratio 1.07 for each unit increase in Ki-67, P=0.016, 95% confidence interval 1.01–1.14). In multivariable analysis adjusting for NCCN risk, Ki-67 remained associated with PSA recurrence (hazard ratio 1.07 per unit increase, 95% confidence interval 1.01–1.14), although risk was not uniform across Ki-67 tertiles (Figure 1a). NCCN risk was also associated with PSA recurrence (hazard ratio 1.91 and 2.20 for high and intermediate vs low risk, respectively, Figure 1b). The time to PSA recurrence was similar in the two lowest tertiles as compared with the highest tertile (median 9.9 years, not reached, vs 3.6 years, respectively) and 10-year recurrence-free proportion was 46%, 64% and 38%, respectively. These data suggest that men in the highest tertile of Ki-67 have a higher risk of PSA recurrence over time. Although patients with low-risk PC had favorable outcomes (73% of men were free of PSA progression at 5 years, median time to recurrence not yet reached), men with intermediate or high PC had a higher risk of recurrence (49 and 45% of men free of PSA progression at 5 years, respectively, and median time to recurrence of 4.9 and 4.6 years). The differences in PSA recurrence across NCCN risk groups was statistically significant (log-rank P=0.0057 and 0.0005 for low vs high and low vs intermediate risk, respectively).
Association of Ki-67 biomarker expression (average score per subject across TMA) and NCCN clinical risk group with PSA relapse. (a) Association of Ki-67 expression by tertiles with recurrence-free survival (PSA relapse), shown in a Kaplan–Meier survival plot. (b) Association of NCCN risk groups with PSA relapse, shown in a Kaplan–Meier survival plot. Low risk includes PSA<10, Gleason 6 or less and pT2a or less-pathologic stage. Intermediate risk includes PSA 10–20, Gleason 7 or pT2b. High risk includes PSA>20, Gleason 8–10 or stage T2c or higher. NCCN, National Comprehensive Cancer Network; TMA, tissue microarray.
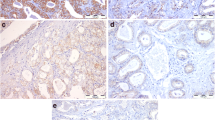
Having validated Ki-67 and NCCN risk in our clinical data set, we next evaluated a series of EP biomarkers in primary PC tissues. Examples of representative immunohistochemical images of each biomarker are shown in Figure 2 and Supplementary Figure 3. We found that only 1.5 and 12.7% of patients had absent or low E-cadherin expression, respectively; the majority (85.6%) had high E-cadherin expression. For all mesenchymal biomarkers, we used the maximal expression between cores, given the heterogeneity of expression between cores. For all epithelial biomarkers, we used the minimum expression between cores. Of evaluable tissue, N-cadherin was rarely expressed, and was present in only 3.9% of PCs, whereas 96.0% had absent N-cadherin expression. We observed vimentin expression to be largely stromal in distribution and only tumor cell vimentin was scored. We found that 22.4 and 5.9% of patients expressed intermediate and high vimentin, respectively, and most cancers had absent vimentin expression (70.7%). Zeb1 was expressed in 15.3% of cases, with only three cases demonstrating intense staining. SNAIL was expressed more heterogeneously among 188 evaluable men for this biomarker, with 31%, 39%, 24% and 5% of PCs having 0, 1, 2 and 3+ SNAIL expression, respectively. Finally, TWIST expression was also heterogeneously expressed in the 148 evaluable men, with 1, 45, 29 and 64% of PCs having 0, 1, 2 and 3+ TWIST expression.
Representative prostate cancer tissue microarray immunohistochemical staining examples from the Durham VA SEARCH database, stained for (a) E-cadherin (2+), (b) N-cadherin (1+) and (c) vimentin (2+). (d–f) shows ZEB1 expression (0, 1 and focal 2 (arrow), respectively). (g–i) shows SNAIL expression (0, 1, 2 respectively). Images of TWIST expression are available in Supplementary Figure 1.
In univariate analysis, we found no association with any EP biomarker with PSA recurrence (Table 3). When examined using mean expression, minimum expression or maximum expression, we likewise found no associations with outcome for low E-cadherin, high N-cadherin, high SNAIL, high vimentin, high ZEB1 or high TWIST expression. In several cases, higher mesenchymal protein expression was numerically associated with improved outcome, although this was not statistically significant. For example, men with high levels of SNAIL expression had a 5-year PSA progression-free probability of 69% as compared with 53% for men with low SNAIL expression. Similar trends were seen for vimentin (5-year PSA recurrence-free probability of 68% for high vimentin, vs 57% for absent vimentin). High E-cadherin was associated with a greater probability of PSA relapse at 5 years (43%) as compared with men with low to absent E-cadherin in their PC (24% risk of PSA relapse). N-cadherin was not evaluated for associations with PSA recurrence given the low number of men who had high N-cadherin expression (n=8). TWIST expression was also not associated with PSA relapse (Table 3). In addition, we found no statistically significant prognostic associations for composites of EP biomarkers (0, 1 vs 2 or more EP biomarkers) for PSA recurrence. Finally, there was little concordance between individual EP biomarkers (kappa <0.05). Given the low number of PC-specific deaths or metastatic events over time, we were unable to identify an association of EP biomarker expression with these endpoints.
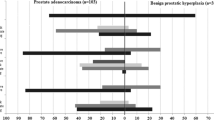
We next examined whether EP biomarkers were associated with known prognostic clinical/pathologic risk factors. Ki-67 was directly linked to NCCN risk groups, with 40, 53 and 69% of low, intermediate and high-risk cases having Ki-67 expression levels over the median value (Figure 3). The median Ki-67 expression (using median score across the TMA for each subject) was 2.0, 2.9 and 4.7% for low, intermediate, and high NCCN risk (P=0.013 by Kruskal–Wallis test, Figure 3). Ki-67 was also associated with Gleason sum (P=0.043 by Kruskal–Wallis testing). Plots of the proportion of men with high Ki-67 (>median), TWIST (2–3+), SNAIL (2–3+), vimentin (1–2+) and ZEB1 (1–2+) and low E-cadherin (0-1+) expression according to NCCN/classic D’Amico risk groups are shown in Figure 3. Although Ki-67 increased with NCCN risk, we did not observe any associations of EP biomarkers with increasing NCCN risk. Other mesenchymal biomarkers decreased with NCCN risk (vimentin) or had no association with risk group (SNAIL, loss of E-cadherin, TWIST, N-cadherin).
Bar graph demonstrating the association of epithelial plasticity biomarkers with National Comprehensive Cancer Network risk group. Low risk includes PSA<10, Gleason 6 or less, and pT2a or less-pathologic stage. Intermediate risk includes PSA 10–20, Gleason 7 or pT2b. High risk includes PSA>20, Gleason 8–10 or stage T2c or higher. Biomarkers are classified by the proportion high: average Ki-67 above median, maximum SNAIL 2–3+, maximum TWIST 2–3+, maximum vimentin 1–2+, maximum ZEB1 2–3+. For E-cadherin, classification is by the proportion low (0–1+) using the minimum value per subject across the tissue microarray.
Discussion
We examined the association of a range of EP biomarkers for their prognostic association with PSA recurrence in a contemporary series of men with localized PC treated with curative intent radical prostatectomy. The outcomes in this cohort of VA men were excellent, with only three deaths from PC and four patients developing metastatic disease with over 11 year median follow-up despite a relatively high 43% PSA recurrence rate. Although a biomarker of proliferation, Ki-67, was validated as being associated with NCCN risk and risk of PSA relapse after surgery, we found no associations of EP biomarkers with clinical risk groups or PSA recurrence in our study.
There are several possible explanations for the lack of association of mesenchymal biomarker expression with outcomes after surgery.7, 10, 19 The first is the overall excellent long-term outcomes in our cohort, limiting the ability to demonstrate associations of biomarkers with PC metastasis or death due to low event rates. This reflects the improving prognosis of men treated for localized PC over time, and the limitations of any biomarker for improving upon clinical risk stratification. In addition, we could not validate the prognostic relevance of E/N-cadherin switch given the low level N-cadherin expression observed. Although the E- to N-cadherin switch data7 have not yet been validated externally, a larger cohort of high-risk men followed long-term through metastatic relapse and death would be needed.
Second, we found several mesenchymal biomarkers to be quite commonly expressed in low-grade tumors. For example, loss of E-cadherin or low E-cadherin expression was more commonly seen in low-grade Gleason 6 disease, whereas most high-grade tumors had abundant and intense E-cadherin staining. Similarly, TWIST expression was ubiquitous across NCCN risk groups, and vimentin expression in PC cells actually decreased with increasing grade. SNAIL and ZEB1 expression was not associated with grade or clinical risk in our series. These data suggest that in localized PC, broad mesenchymal biomarker expression in high-grade disease is not common or associated with recurrence.
There are several limitations present in our study. The first includes the lack of rare cell isolation within tumors that lack epithelial biomarker expression. These alternative and more complex histologic methods, using quantitative imaging and dual-color immunofluorescence, have associated a loss of PSA expression or cytokeratin staining with high-grade, poor-risk disease and adverse outcomes after surgery.6, 11 Second, a TMA is unable to assess regional or geographic variability of biomarkers, for example, mesenchymal biomarker expression only at the invasive tumor front. Our TMA did not include this geographic distribution information, and future studies should consider annotation of biomarker expression according to geographic distribution (central, peripheral, invasive strands, capsular invasion regions) and heterogeneity/multifocality of individual tumors to better ascertain the relationship of a given biomarker distribution with outcome, similar to that described in other solid tumors.20, 21, 22
Finally, our cohort of men was relatively small and despite the long-term follow-up, the number of metastatic and PC-specific mortality events was low, limiting our power to observe associations of EP biomarkers with more clinically relevant outcomes. Our prior work identified the common presence of these EP biomarkers in circulating tumor cells from men with castration-resistant PC, suggesting the importance of EP with lethal forms of the disease.4, 9, 23 Others have confirmed these findings, but suggested that these EP biomarkers may be less prevalent in hormone-sensitive disease.24 Castration itself may promote an EMT, possibly linked to the development of androgen receptor alterations such as splice variants.25, 26, 27 Our cohort of men was unexposed to androgen deprivation therapy and had a low metastatic rate, limiting our ability to detect an EMT if EP is more relevant to castration-resistant progression and/or metastasis. Only 12% of our patients had high-grade Gleason 8–10 disease, which limits our ability to determine associations within this high-risk subpopulation. Nevertheless, we observed that the majority of high-grade tumors had an epithelial phenotype, and that mesenchymal biomarker expression was often more commonly expressed in lower risk cancers. These data suggest the importance of a mesenchymal to epithelial transition in PC, or that the majority of primary PCs, have largely not undergone an EMT, at least in the majority of their cells. We cannot rule out rare cellular events relevant to EMT and cancer dissemination in this study, however.
In conclusion, our data suggest that EP biomarker expression in men with localized PC does not add clinical utility or prognostic information. Further study of rare de-differentiated cellular populations and geographic distribution of EP biomarkers in PC and the association with PC-specific mortality or metastasis is warranted however.
References
Stephenson AJ, Kattan MW, Eastham JA, Bianco FJ Jr, Yossepowitch O, Vickers AJ et al. Prostate cancer-specific mortality after radical prostatectomy for patients treated in the prostate-specific antigen era. J Clin Oncol 2009; 27: 4300–4305.
D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Schnall M, Tomaszewski JE et al. A multivariate analysis of clinical and pathological factors that predict for prostate specific antigen failure after radical prostatectomy for prostate cancer. J Urol 1995; 154: 131–138.
Irshad S, Bansal M, Castillo-Martin M, Zheng T, Aytes A, Wenske S et al. A molecular signature predictive of indolent prostate cancer. Sci Transl Med 2013; 5: 202ra122.
Bitting RL, Schaeffer D, Somarelli JA, Garcia-Blanco MA, Armstrong AJ . The role of epithelial plasticity in prostate cancer dissemination and treatment resistance. Cancer Metastasis Rev 2014; 33: 441–468.
Kalluri R, Weinberg RA . The basics of epithelial-mesenchymal transition. J Clin Invest 2009; 119: 1420–1428.
Domingo-Domenech J, Vidal SJ, Rodriguez-Bravo V, Castillo-Martin M, Quinn SA, Rodriguez-Barrueco R et al. Suppression of acquired docetaxel resistance in prostate cancer through depletion of notch- and hedgehog-dependent tumor-initiating cells. Cancer Cell 2012; 22: 373–388.
Gravdal K, Halvorsen OJ, Haukaas SA, Akslen LA . A switch from E-cadherin to N-cadherin expression indicates epithelial to mesenchymal transition and is of strong and independent importance for the progress of prostate cancer. Clin Cancer Res 2007; 13: 7003–7011.
Tanaka H, Kono E, Tran CP, Miyazaki H, Yamashiro J, Shimomura T et al. Monoclonal antibody targeting of N-cadherin inhibits prostate cancer growth, metastasis and castration resistance. Nat Med 2010; 16: 1414–1420.
Armstrong AJ, Marengo MS, Oltean S, Kemeny G, Bitting RL, Turnbull JD et al. Circulating tumor cells from patients with advanced prostate and breast cancer display both epithelial and mesenchymal markers. Mol Cancer Res 2011; 9: 997–1007.
Behnsawy HM, Miyake H, Harada K, Fujisawa M . Expression patterns of epithelial-mesenchymal transition markers in localized prostate cancer: significance in clinicopathological outcomes following radical prostatectomy. BJU Int 2013; 111: 30–37.
Qin J, Liu X, Laffin B, Chen X, Choy G, Jeter CR et al. The PSA(-/lo) prostate cancer cell population harbors self-renewing long-term tumor-propagating cells that resist castration. Cell Stem Cell 2012; 10: 556–569.
Heeboll S, Borre M, Ottosen PD, Dyrskjot L, Orntoft TF, Torring N . Snail1 is over-expressed in prostate cancer. APMIS 2009; 117: 196–204.
Ayala G, Tuxhorn JA, Wheeler TM, Frolov A, Scardino PT, Ohori M et al. Reactive stroma as a predictor of biochemical-free recurrence in prostate cancer. Clin Cancer Res 2003; 9: 4792–4801.
Khor LY, Bae K, Paulus R, Al-Saleem T, Hammond ME, Grignon DJ et al. MDM2 and Ki-67 predict for distant metastasis and mortality in men treated with radiotherapy and androgen deprivation for prostate cancer: RTOG 92-02. J Clin Oncol 2009; 27: 3177–3184.
Parker AS, Heckman MG, Wu KJ, Crook JE, Hilton TW, Pisansky TM et al. Evaluation of ki-67 staining levels as an independent biomarker of biochemical recurrence after salvage radiation therapy for prostate cancer. Int J Radiat Oncol Biol Phys 2009; 75: 1364–1370.
Pollack A, DeSilvio M, Khor LY, Li R, Al-Saleem TI, Hammond ME et al. Ki-67 staining is a strong predictor of distant metastasis and mortality for men with prostate cancer treated with radiotherapy plus androgen deprivation: Radiation Therapy Oncology Group Trial 92-02. J Clin Oncol 2004; 22: 2133–2140.
Verhoven B, Yan Y, Ritter M, Khor LY, Hammond E, Jones C et al. Ki-67 is an independent predictor of metastasis and cause-specific mortality for prostate cancer patients treated on Radiation Therapy Oncology Group (RTOG) 94-08. Int J Radiat Oncol Biol Phys 2013; 86: 317–323.
Berney DM, Gopalan A, Kudahetti S, Fisher G, Ambroisine L, Foster CS et al. Ki-67 and outcome in clinically localised prostate cancer: analysis of conservatively treated prostate cancer patients from the Trans-Atlantic Prostate Group study. Br J Cancer 2009; 100: 888–893.
Mak P, Leav I, Pursell B, Bae D, Yang X, Taglienti CA et al. ERbeta impedes prostate cancer EMT by destabilizing HIF-1alpha and inhibiting VEGF-mediated snail nuclear localization: implications for Gleason grading. Cancer Cell 2010; 17: 319–332.
Brabletz T, Jung A, Reu S, Porzner M, Hlubek F, Kunz-Schughart LA et al. Variable beta-catenin expression in colorectal cancers indicates tumor progression driven by the tumor environment. Proc Natl Acad Sci USA 2001; 98: 10356–10361.
Haffner MC, Mosbruger T, Esopi DM, Fedor H, Heaphy CM, Walker DA et al. Tracking the clonal origin of lethal prostate cancer. J Clin Invest 2013; 123: 4918–4922.
Haffner MC, De Marzo AM, Yegnasubramanian S, Epstein JI, Carter HB . Diagnostic challenges of clonal heterogeneity in prostate cancer. J Clin Oncol 2014; 33: e38–e40.
Bitting RL, Boominathan R, Rao C, Kemeny G, Foulk B, Garcia-Blanco MA et al. Development of a method to isolate circulating tumor cells using mesenchymal-based capture. Methods 2013; 64: 129–136.
Chen CL, Mahalingam D, Osmulski P, Jadhav RR, Wang CM, Leach RJ et al. Single-cell analysis of circulating tumor cells identifies cumulative expression patterns of EMT-related genes in metastatic prostate cancer. Prostate 2013; 73: 813–826.
Cottard F, Asmane I, Erdmann E, Bergerat JP, Kurtz JE, Ceraline J . Constitutively active androgen receptor variants upregulate expression of mesenchymal markers in prostate cancer cells. PLoS One 2013; 8: e63466.
Sun F, Chen HG, Li W, Yang X, Wang X, Jiang R et al. Androgen receptor splice variant AR3 promotes prostate cancer via modulating expression of autocrine/paracrine factors. J Biol Chem 2014; 289: 1529–1539.
Sun Y, Wang BE, Leong KG, Yue P, Li L, Jhunjhunwala S et al. Androgen deprivation causes epithelial-mesenchymal transition in the prostate: implications for androgen-deprivation therapy. Cancer Res 2012; 72: 527–536.
Acknowledgements
This work was supported by the Robert B Goergen Prostate Cancer Foundation Young Investigator Award, and the Department of Defense Physician Research Training Award (W81XWH-10-1-0483) (AJA) and NIH 1K24CA160653 (SJF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Rights and permissions
About this article
Cite this article
Armstrong, A., Healy, P., Halabi, S. et al. Evaluation of an epithelial plasticity biomarker panel in men with localized prostate cancer. Prostate Cancer Prostatic Dis 19, 40–45 (2016). https://doi.org/10.1038/pcan.2015.46
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2015.46
- Springer Nature Limited