Abstract
Background:
To assess the added value of biopsy factors, like maximum cancer length in a core (MCL), cumulative cancer length (CCL), cumulative length of positive cores (CLPC), percentage of cancer involvement in positive cores (CIPC) and the Prostate Cancer Research International: Active Surveillance (PRIAS) criteria in patients who underwent radical prostatectomy (RP) but eligible for active surveillance (AS).
Methods:
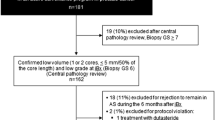
From January 2002 to December 2007, 750 consecutive subjects underwent RP. We identified 147 (19.07%) patients who were eligible for AS based on PRIAS criteria: clinical stage T1c or T2, PSA level of⩽10 ng ml−1, Gleason score ⩽6, PSA-D of <0.2 ng ml−2 and one or two positive biopsy cores. We calculated the diagnostic accuracy of biopsy factors in determining pathological confirmed unfavorable disease. Decision curve analysis (DCA) were performed.
Results:
Of all subjects, 95 patients (66.43%) had favorable whereas 48 had (33.57%) unfavorable disease. On multivariate analyses, the inclusion of MCL, CCL, CLPC and CIPC significantly increased the accuracy of the base multivariate model in predicting unfavorable disease. The gain in predictive accuracy for MCL in a core, CCL, CLPC and CIPC ranged from 13 to 27%. The DCA shows that adding MCL, CCL, CLPC and CIPC resulted in a greater net benefit when the probability of ranges between 15 and 50%. The models can be applied at the cost of missing not more than 16.83% of unfavorable disease.
Conclusions:
Our findings suggested that the addition of these biopsy factors to PRIAS criteria has the potential to significantly increase the ability to detect unfavorable disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
As reported by two recently published randomized-controlled trials, the diffusion of the screening of prostate cancer (PCa) has led to a reduction of PCa deaths.1, 2 Nevertheless, it resulted in a significant increase of over diagnosis in patients with low-risk PCa, that could not benefit from definitive treatment. Truly in this context, active surveillance (AS) has gained popularity with the intention of avoiding or postponing interventions in subjects with PCa of low biological potential.3, 4, 5
The rationale is that most low-risk PCa has an indolent course, and that the slow growth rate allows sufficient time during follow-up to detect cancers that are destined to become more aggressive during a window of curability.6
Unfortunately, several inclusion criteria have been proposed until now but many doubts still persist on their ability to predict favorable disease.7, 8 According to a recent comparison of different contemporary protocols, the Prostate Cancer Research International: Active Surveillance (PRIAS) study showed the highest ability to identify patients with organ-confined low-grade cancer, with an area under the curve (AUC) of 0.62.9 Furthermore, several tumor and biopsy factors have been evaluated in order to better identify the prediction of disease progression on AS: clinical stage, prostate volume, Gleason score, number of biopsy cores, number of positive cores, maximum percentage of tumor involvement and core length. We have recently reported that the percentage of cancer involvement in positive cores (CIPC) can be used to select men with low-risk PCa eligible for AS through a cutoff of 0.4 mm, strengthening PRIAS ability of avoiding significant cancer.10
However, statistical significance from a multivariable analysis and the gaining in predictive accuracy of the AUC do not mean that a marker is worth translation into clinics. Studies should provide evidence of decision curve analysis (DCA) thanks to its ability to compare several different models and to illustrate the net-benefits.11
In this study, we aimed to assess performance capabilities of biopsy factors when added to the PRIAS criteria in patients who underwent radical prostatectomy (RP) but eligible for AS.
Materials and methods
From January 2002 to December 2013, 750 consecutive subjects underwent RP using open or laparoscopic techniques at our institution. All patients underwent clinical evaluation including digital rectal examination, serum PSA level measurement and transrectal ultrasound. We selected patients who were eligible for AS based on PRIAS criteria: clinical stage T1c or T2 disease, PSA level of ⩽10 ng ml−1, Gleason score ⩽6, PSA-D of <0.2 ng ml−1(ref. 2) and one or two positive biopsy cores. Patients with <10 cores taken at biopsy, neoadjuvant hormonal therapy, insufficient histo-pathological report and missing clinical data were excluded. All transperineal prostatic biopsies and RPs were performed at the same institution and RP specimens were evaluated by senior uropathologists. All prostate biopsies were performed with the same technique and by the use of a 18 G needle (cutting length 23 mm).
We recorded data from clinical evaluation (that is, clinical stage, PSA level, PSA-D and total prostate volume), from prostatic biopsy (that is, Gleason score, total number of biopsy cores, maximum cancer length (MCL) in the positive cores and total length of positive cores) and from RP specimens (that is, Gleason score, extra-capsular extension, seminal vesicle invasion and positive surgical margins. MCL in a core was defined as the longest length of continuous cancer lesion without gap of benign tissue in a given biopsy session. We incorporated histological parameters like the percentage of CIPC, calculated by dividing the cumulative cancer length (CCL) to the cumulative length of positive cores (CLPC). CCL was defined as the sum of the length of all cancerous lesions in mm whereas CLPC as sum of the length of all positive cores in mm. Unfavorable disease was considered as non-organ-confined disease (pathological stage >pT2) and/or upgraded disease (Gleason score>6) in the RP specimens as reported by previous reports.12
The protocol was approved by the Internal Institutional Review Board and an informed written consent was obtained from each patient before the initiation of the study.
Statistical analysis
All statistical analyses were completed using SPSS v. 19 software (SPSS, IBM, Somers, NY, USA) and R (R Foundation for Statistical Computing). The qualitative data were tested using the χ2 test or Fisher’s exact test as appropriate and the continous variables, presented as median, were tested by Mann–Whitney U-test. Multivariable logistic regression analysis was performed to identify the predictors of unfavorable disease. We performed a base model incorporating PSA levels, PSA density, clinical T stage (T2 vsT1), biopsy Gleason score (6 vs <6), number of positive cores (2 vs 1) and adjusted for age. Multivariable logistic regression analysis were complemented by calculating the AUC of the model. To test the ability of MCL, CCL, CLPC and CIPC to predict the outcome of interest, these variables were individually added to the base multivariable model. The gain in predictive accuracy was quantified, and AUCs were compared using the Wald test. One thousand bootstrap resamples were used for all accuracy estimates and to reduce overfit bias. To graphically evaluate the net benefit after incorporating the MCL, CCL, CLPC and CIPC into the base model, we performed DCA.11 For all statistical comparisons significance was considered as P <0.05.
Results
Of all subjects analyzed, 143 (19.07%) fulfilled the PRIAS criteria. Among these, 95 (66.43%) had favorable (Group A) and 48 (33.57%) had unfavorable disease (Group B) (Figure 1). Table 1 shows clinical and pathological outcomes of both groups in terms of PSA level, PSA-D, clinical stage, prostate volume, mean lengths of individual cores and any other difference that was observed between both the groups. When considering the biopsy histological features, MCL, CCL, CLPC and CIPC were significantly greater in Group B than in Group A (P<0.01). On multivariate analyses and after bootstrapping with 1000 resamples, the inclusion of MCL (Model 2), CCL (Model 3), CLPC (Model 4) and CIPC (Model 5) significantly increased the accuracy of the base multivariate model in predicting unfavorable disease. The gain in predictive accuracy for all biopsy factors ranged from 13 to 27% (Table 2). AUCs of models 2–5 that included biopsy factors were significantly greater than the base model (P<0.05; Figure 2).
Receiver operating characteristic curves depicting the accuracy of individual predictors of unfavorable disease (a), Gleason⩾7 (b) or extra-capsular extension (c). Basic model includes: total PSA, number of positive cores, PSA density, clinical stage and biopsy Gleason score. Model 2 is a basic model that includes all the factors in Model 1 plus maximum cancer length in a core. Model 3 is a basic model that includes all the factors in Model 1 plus cumulative cancer length. Model 4 is a basic model that includes all the factors in Model 1 plus total length of positive cores. Model 5 is a basic model that includes all the factors in Model 1 plus percentage of cores involvement in positive cores.
Supplementary Table 1 shows sensitivity, specificity, positive predictive value, and negative predictive value at three levels of predictive variables: high sensitivity (Supplementary Table 1a), best combination (Supplementary Table 1b) and high specificity (Supplementary Table 1c).
In Figure 3, the DCA shows that models including MCL, CCL, CLPC and CIPC (models 2–5) clearly result in a greater net benefit when the probability of finding unfavorable disease ranges between 15 and 50%. The models can be applied at the cost of missing not more than 16.83% of unfavorable disease as predicted by the CIPC of 28.5 as cut-off for RP (Supplementary Table 2).
Decision curve analysis of the effect of prediction models on the detection of unfavorable disease. The net benefit is plotted against various threshold probabilities. The threshold probability is the minimum probability of prostate cancer at which a patient (or clinician) would opt for intervention. Basic model includes, includes total PSA, number of positive cores, PSA density, clinical stage and biopsy Gleason score. Model 2 is a basic model that includes all the factors in Model 1 plus maximum cancer length in a core. Model 3 is a basic model that includes all the factors in Model 1 plus cumulative cancer length. Model 4 is a basic model that includes all the factors in Model 1 plus total length of positive cores. Model 5 is a basic model that includes all the factors in Model 1 plus percentage of cores involvement in positive cores. Decision curve analysis consists of showing graphically the so-called net benefit obtained by applying the strategy of treating an individual if and only if his probability of having the disease is equal to or greater than the determined threshold probability. It facilitates the comparison among alternative prediction models used to calculate the probability of disease. Consequently, it may also facilitate the choice of which of the several prediction models to adopt to have the highest net benefit at the clinician’s or patient’s personally determined threshold probability.
Discussion
The main objectives of AS are to select patients with low-risk PCa and to monitor any changes in clinical and pathological variables. However, the capabilities of the current criteria in predicting significant PCa may significantly differ and it mainly depends on the heterogeneity of the inclusion parameters.
Unfortunately, because AS has been introduced in the clinical practice, those criteria have not been improved and the derived accuracies of these models in predicting insignificant cancer only range from 59 to 64%.9
In this intricate context, the PRIAS protocol offered the best balance between specificity and sensibility.9
Unfortunately, in the updated results from the PRIAS study, 28% of the cohort experienced disease reclassification (defined as Gleason score >6 and/or more than positive cores) at repeated biopsy during follow-up.13 These results confirmed that the risk of misclassification at the prostate biopsies still persist, a possibility that depends most likely on undersampling of more aggressive tumors than the progression of indolent ones.14
For all these premises, different challenges of biopsy factors have been proposed with the aim of strengthening the accuracy of the AS criteria.
One of them could consist in obtaining longer tissue pieces from each biopsy core. Boccon-Gibod et al.15 suggested that the average needle biopsy length should serve as a measure of quality control with 10 mm of tissue as the shortest acceptable length. A recent report demonstrated that obtaining biopsy cores longer than 11.9 mm was associated with a 2.5-times higher likelihood of PCa detection.16
The extent of cancer on biopsy, such as number of positive cores, cancer length and/or percentage of core involvement, were also shown in the majority of studies to be important predictors of disease progression or of the probability of remaining on AS.17 We have recently demonstrated that adding the percentage of CIPC significantly improved the accuracy of the PRIAS protocol in predicting unfavorable disease in men eligible for AS.10
However, limitations of the current literature data are mainly based on the lack of DCA that contributes to better compare different models and to illustrate the net-benefits.
Herein, we tried to prevent these questions by performing DCA of four different models that included common biopsy features in men eligible for AS: MCL in a core, CCL, CLPC and CIPC.
We reported that the addition of one of the previous biopsy factors to the PRIAS model increased its performance.
The models showed a net benefit when the probability of finding unfavorable disease ranges between 15 and 50% with at least a risk of near 17% of missing non-organ-confined and high-grade PCa.
All these findings could be considered relevant taking into account the increased risk of diagnosis and treatment for PCa. A cautious approach on men with low-risk PCa could avoid them from an overtreatment and consequent detrimental effect on quality-of-life. Thus, strategies that distinguish indolent cancers from aggressive cancers are necessary, using either biomarker combinations or novel biomarkers, like prostate health index, 4K score and magnetic resonance. Our findings suggest that models including biopsy factors could not only predict unfavorable disease in men eligible for AS but could also minimize the risk of missing high-grade and non-organ-confined cancers.
However, this study contains potential limitations that need to be considered. First, measurement of tumor volume by a computerized morphometric analyzer would be more accurate to estimate the correct prostate biopsy features. Just to this regard, image-targeted biopsy of the prostate has being increasingly adopted.18, 19 The targeted biopsy strategies, in fact, demonstrated a higher disease burden, expressed by the increase of maximum cancer core length and the proportion of positive cores.20 It should be taken into account, therefore, that these new methods are not too easy to be performed in daily practice and that further studies should be conducted before approving them. Second, all subjects of our study underwent transperineal prostate biopsy. A different study including men examined by transrectal biopsy may offer new contributes. In fact, because the cores of the transperineal approach are directed longitudinally to the peripheral zone of the prostate, this approach should have a better PCa detection ability than the transrectal approach. Moreover, the transperineal approach should allow more accurate sampling of the anterior part of the gland.
Third, the inclusion of patients operated on before the 2005 International Society of Urological Pathology modified Gleason score system, who may have more aggressive tumors, could be possible limitations of our study.
Fourth, it should be noted that different criteria have been used to define ‘unfavorable’ disease, for example, not necessarily the presence of Gleason score of 7 may be associated with more aggressive PCa. Anyway, we used the statement of previous reports.12
Finally, the lack of a central pathologist revision (ongoing for a further investigative study) is a potential limitation for determining outcomes.
Our study has some strengths. First, we use a contemporary, well-characterized cohort who underwent RP but eligible for AS according to PRIAS criteria. This means that our results can be translated in a relevant, contemporary clinical setting. Second, we validated contemporary common biopsy features in an entirely independent cohort. Finally, performed DCA demonstrating improvement of clinical decision making with the observed low rate of unfavorable disease risk in this cohort when introducing the biomarker models. These results could be translated in an AS decision situation with clinical net-benefits.
Conclusion
A proportion of patients still remain at risk of misclassification despite of their initial eligibility for PRIAS criteria. The adding of some biopsy factors, like MCL, CCL, CLPC and CIPC, in clinical practice has the potential to significantly increase the ability of PRIAS inclusion criteria to detect unfavorable disease with low cost of missing non-organ-confined and high-grade cancer.
References
Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med 2012; 366: 981–990.
Hugosson J, Carlsson S, Aus G, Bergdahl S, Khatami A, Lodding P et al. Mortality results from the Goteborg randomised population-based prostate-cancer screening trial. Lancet Oncol 2010; 11: 725–732.
Wong LM, Ferrara S, Alibhai SM, Evans A, Van der Kwast T, Trottier G et al. Diagnostic prostate biopsy performed in a non-academic center increases the risk of re-classification at confirmatory biopsy for men considering active surveillance for prostate cancer. Prostate Cancer Prostatic Dis 2015; 18: 69–74.
Wong LM, Neal DE, Finelli A, Davis S, Bonner C, Kapoor J et al. Evaluation of models predicting insignificant prostate cancer to select men for active surveillance of prostate cancer. Prostate Cancer Prostatic Dis 2015; (e-pub ahead of print).
Gorin MA, Eldefrawy A, Ekwenna O, Soloway MS . Active surveillance for low-risk prostate cancer: knowledge, acceptance and practice among urologists. Prostate Cancer Prostatic Dis 2012; 15: 177–181.
Tseng KS, Landis P, Epstein JI, Trock BJ, Carter HB . Risk stratification of men choosing surveillance for low risk prostate cancer. J Urol 2010; 183: 1779–1785.
Louie-Johnsun M, Neill M, Treurnicht K, Jarmulowicz M, Eden C . Final outcomes of patients with low-risk prostate cancer suitable for active surveillance but treated surgically. BJU Int 2009; 104: 1501–1504.
Mufarrij P, Sankin A, Godoy G, Lepor H . Pathologic outcomes of candidates for active surveillance undergoing radical prostatectomy. Urology 2010; 76: 689–692.
Iremashvili V, Pelaez L, Manoharan M, Jorda M, Rosenberg DL, Soloway MS . Pathologic prostate cancer characteristics in patients eligible for active surveillance: a head-to-head comparison of contemporary protocols. Eur Urol 2012; 62: 462–468.
Russo GI, Cimino S, Castelli T, Favilla V, Urzi D, Veroux M et al. Percentage of cancer involvement in positive cores can predict unfavorable disease in men with low-risk prostate cancer but eligible for the prostate cancer international: active surveillance criteria. Urol Oncol 2014; 32: 291–296.
Vickers AJ, Elkin EB . Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making 2006; 26: 565–574.
El Hajj A, Ploussard G, de la Taille A, Allory Y, Vordos D, Hoznek A et al. Analysis of outcomes after radical prostatectomy in patients eligible for active surveillance (PRIAS). BJU Int 2013; 111: 53–59.
Bul M, Zhu X, Valdagni R, Pickles T, Kakehi Y, Rannikko A et al. Active surveillance for low-risk prostate cancer worldwide: the PRIAS study. Eur Urol 2013; 63: 597–603.
Cantiello F, Russo GI, Ferro M, Cicione A, Cimino S, Favilla V et al. Prognostic accuracy of prostate health index and urinary prostate cancer antigen 3 in predicting pathologic features after radical prostatectomy. Urol Oncol 2015; 33: 163.e15–23.
Boccon-Gibod L, van der Kwast TH, Montironi R, Bono A . Handling and pathology reporting of prostate biopsies. Eur Urol 2004; 46: 177–181.
Obek C, Doganca T, Erdal S, Erdogan S, Durak H . Core length in prostate biopsy: size matters. J Urol 2012; 187: 2051–2055.
Loeb S, Bruinsma SM, Nicholson J, Briganti A, Pickles T, Kakehi Y et al. Active surveillance for prostate cancer: a systematic review of clinicopathologic variables and biomarkers for risk stratification. Eur Urol 2014; pii S0302-2838(14)01018-5.
Moore CM, Robertson NL, Arsanious N, Middleton T, Villers A, Klotz L et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol 2013; 63: 125–140.
Pinto F, Totaro A, Calarco A, Sacco E, Volpe A, Racioppi M et al. Imaging in prostate cancer diagnosis: present role and future perspectives. Urol Int 2011; 86: 373–382.
Robertson NL, Hu Y, Ahmed HU, Freeman A, Barratt D, Emberton M . Prostate cancer risk inflation as a consequence of image-targeted biopsy of the prostate: a computer simulation study. Eur Urol 2014; 65: 628–634.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Supplementary information
Rights and permissions
About this article
Cite this article
Russo, G., Castelli, T., Favilla, V. et al. Performance of biopsy factors in predicting unfavorable disease in patients eligible for active surveillance according to the PRIAS criteria. Prostate Cancer Prostatic Dis 18, 338–342 (2015). https://doi.org/10.1038/pcan.2015.26
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2015.26
- Springer Nature Limited