Abstract
The aryl hydrocarbon receptor (AhR) is a ligand-activated transcription factor and a member of the basic helix-loop-helix PER/ARNT/SIM family of chemosensors and developmental regulators. The AhR is widely known as a mediator of dioxin toxicity; however, it also suppresses cancer cell proliferation and recent findings have implicated its role as a tumor suppressor. We conducted a chemical library screen to identify nontoxic AhR ligands with anti-cancer effects and discovered flutamide (Eulexin) as a putative AhR ligand. Flutamide is an androgen receptor (AR) antagonist approved by the United States Food and Drug Administration for the treatment of prostate cancer. We found that flutamide inhibited the growth of several cancer cell lines independent of AR status, and that suppression of AhR expression reversed the anti-proliferative effects of flutamide. We investigated the AhR-dependent mechanism of action of flutamide in human hepatocellular carcinoma cells and identified that transforming growth factor-β1 (TGF-β1) is induced by flutamide in an AhR-dependent manner. In contrast, the potent AhR agonist 2,3,7,8-Tetrachlorodibenzo-p-dioxin had no effect on TGF-β1 expression, indicating the ligand specificity of AhR activation. We also determined that TGF-β1 induction is required for the AhR-dependent growth inhibitory effects of flutamide. Therefore, flutamide may be effective in AhR-positive cancers that are sensitive to TGF-β1 signaling, such as hepatocellular carcinoma.
Similar content being viewed by others
Introduction
The aryl hydrocarbon receptor (AhR) is a ligand-activated transcription factor and member of the PER/ARNT/SIM (PAS) domain family of transcription factors and developmental regulators.1, 2 Exogenous ligands of the AhR include polycyclic aromatic hydrocarbons, flavones, and dioxins such as 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD). The latent AhR is compartmentalized in the cytosol complexed with p23, XAP2 and heat shock protein 90, whose association is required for ligand binding.3, 4, 5, 6, 7 Ligand binding to the PAS-B domain of the AhR results in dissociation from heat shock protein 90 and nuclear translocation. Upon nuclear localization, the AhR heterodimerizes with the AhR nuclear translocator forming the active transcription factor complex. The activated AhR transcription factor complex then binds to Ah responsive elements, and concomitant recruitment of transcriptional machinery initiates target gene transcription. Classical AhR target genes have been characterized in response to TCDD exposure and include the cytochrome P450 family of drug metabolizing enzymes.2, 8, 9 In murine models, TCDD has been characterized as a potent tumor promoter,10, 11 although there is no clear evidence between TCDD exposure and increased incidences of cancer in humans.12, 13, 14 TCDD exposure leads to prolonged activation of the AhR in vivo, and can induce toxic effects such as immune suppression,15, 16 chloracne,12 oxidative stress,17, 18 severe weight loss, reproductive19, 20 and developmental toxicity;21, 22 although the molecular interactions that lead to these complex toxic responses remain unclear.23, 24
Separate from xenobiotic-associated toxicity, the AhR has important endogenous roles influencing embryonic development and cell cycle regulation,25, 26 and may also function as a tumor suppressor.27 In the transgenic adenocarcinoma of the mouse prostate mouse model, AhR null mice develop aggressive advanced onset of prostate tumors.28 The presence of the AhR has been shown to suppress hepatic carcinogen diethylnitrosamine induced liver tumors,29 supporting the possibility that the absence of AhR increases tumorigenicity in distinct organs. Recently, a study describing a cancer cell line encyclopedia showed that AhR expression is closely associated with MEK inhibitor efficacy in NRAS mutant lines.30 Furthermore, multiple studies have suggested that ligand-mediated modulation of AhR activity can inhibit endocrine signaling and cancer cell proliferation.31, 32, 33, 34
We performed a small molecule screen to identify ligands capable of specifically activating the tumor suppressive functions of the AhR,35 from which we identified flutamide (Eulexin) as a putative AhR ligand, consistent with published reports.9 Flutamide is approved by the FDA (Food and Drug Administration) for the treatment of androgen-dependent prostate cancers, due to its antagonism of the androgen receptor (AR), resulting in a blockade of testosterone signaling.36 Following our initial screening effort, we confirmed that flutamide is an AhR ligand and modeled its docking orientation into the AhR ligand-binding pocket.37 We also determined that flutamide brings the AhR into a transcriptionally active state, and that flutamide, but not its primary metabolite 2-hydroxy flutamide (2HFL), is responsible for AhR activation. We found that flutamide suppresses proliferation of cancer cells that do not express the AR. We examined the AhR dependency of flutamide-induced growth suppression and demonstrated that the AhR mediates the anti-proliferative effects of flutamide. We further determined that flutamide-activated AhR leads to upregulation of transforming growth factor-β1 (TGF-β1) and activation of TGF-β1-dependent signaling. Suppression of AhR expression or TGF-β1 expression abrogated the anti-proliferative effects of flutamide. We conclude that selective AhR ligands such as flutamide can promote the tumor suppressive functions of the AhR through activation of TGF-β signaling.
Results
Flutamide is an AhR ligand
Our group is interested in identifying and characterizing AhR ligands with potential therapeutic applications. To this end, we conducted a small molecule screen for transcriptional activators of the AhR,35 and identified flutamide as a potent activator of AhR-mediated transcription. Flutamide treatment inhibits testosterone signaling via antagonism of the AR,36 and is clinically utilized in the treatment of prostate cancer under the trademark name Eulexin. We confirmed that flutamide stimulated AhR-dependent transcriptional activity in a dose-dependent manner using an AhR reporter assay (Figure 1a). The endogenous AhR target gene CYP1A1 was also strongly upregulated in flutamide treated HepG2 human hepatocellular carcinoma cells (Figure 1b). We have previously shown that homology modeling of the AhR ligand-binding domain can successfully identify new AhR agonists.37 Molecular docking studies with flutamide in the AhR ligand-binding domain model revealed structural affinity to both the human and mouse AhR orthologs (Figure 1c and Supplementary Figure S1). As a member of the AhR transcription factor complex, the AhR translocates from the cytosol to the nucleus upon ligand binding. The compartmentalization of AhR was monitored in both human and mouse hepatoma cells upon flutamide treatment. Potent nuclear localization of the AhR upon treatment with flutamide was observed within 90 min in both human and mouse hepatoma cells (Figure 1d and Supplementary Figure S2). Therefore, we concluded that flutamide is able to bind to the AhR ligand-binding domain, resulting in AhR nuclear translocation and promotion of AhR-mediated transcriptional activity.
Flutamide is an AhR ligand. (a) Flutamide activates AhR-dependent transcriptional activity. AhRE-luciferase (luc) reporter activity was measured in Hepa1 cells. Cells were lysed and luciferase activity was measured after 24 h of treatment. TCDD (1 nM) was included as a positive control. Flutamide treatment resulted in a dose-dependent upregulation of the reporter activity. ***P⩽0.001; ****P⩽0.0001. (b) The AhR target gene CYP1A1 is induced in response to flutamide treatment. qPCR analysis after 16 and 36 h of treatment reveal that flutamide upregulates CYP1A1 mRNA in HepG2 cells. TCDD (1 nm) was included as a positive control. Values were normalized to GAPDH controls, and reported as fold change compared with vehicle (Veh). **P⩽0.01; ****P⩽0.0001. (c) Flutamide docks into the human AhR ligand-binding domain (hAhR-LBD). Docking orientation of flutamide into the homology model of the hAhR-LBD with the protein backbone displayed as ribbon and colored by secondary structure (ICM v3.5-1p). Flutamide is displayed as sticks and colored by atom type, with the carbon atoms in orange. Protein residues are labeled in black, colored by atom type with carbon atoms in green and displayed as sticks. (d) Flutamide treatment results in AhR nuclear translocation. Structures of TCDD, flutamide and the metabolite 2-hydroxyflutamide (2HFL) are shown. HepG2 cells were treated for 90 min with Veh, 1 nm TCDD, 50 μm flutamide, or 50 μm 2HFL. Cells were fixed and stained for AhR (FITC) and DNA (DAPI). Flutamide treated cells showed strong nuclear compartmentalization. (e) 2HFL does not activate AhR-dependent transcription. AhRE-luc activity was monitored in 2HFL-treated Hepa1 cells as described in a. TCDD (1nM) was included as a positive control. Several concentrations of 2HFL were tested, although none significantly upregulated the AhR-dependent reporter. ***P⩽0.001.
Flutamide is subject to first pass metabolism in vivo, where it is converted to 2-hydroxy flutamide (2HFL) via addition of a hydroxyl group (Figure 1d). Thus, we next examined whether the parent compound flutamide, or its metabolite 2HFL, is responsible for induction of AhR transcriptional activity. Treatment with 2HFL did not significantly increase AhR-mediated transcription (Figure 1e). In support of this observation, we found that 2HFL does not alter cytosolic localization of the AhR as determined by immunostaining (Figure 1d and Supplementary Figure S2). These observations indicate that flutamide, but not its metabolite 2HFL, is an AhR agonist.
Flutamide suppresses cancer cell growth independent of the AR
We next determined whether AhR activation contributes to the anti-cancer effects of flutamide in the absence of the AR. We examined multiple cell lines for expression of both AR and AhR by immunoblotting (Figure 2a). AR expression was observed in the hormone-dependent LNCaP human prostate and MCF-7 human breast cancer cell lines. In contrast, the AhR was expressed across multiple cell lineages regardless of tissue type and is consistent with our earlier findings (Figure 2a).38 We also compared the AR mRNA levels present in the human hepatocellular carcinoma cell lines HepG2 and HuH-7 with that of the LNCaP prostate cancer cell line, which is known to express the AR. We found that AR mRNA expression in hepatocellular carcinoma cell lines was ~1000-fold less than that of LNCaP cells (Figure 2b).
Androgen receptor (AR) independent effects of flutamide. (a) AhR-positive HepG2 cells do not express the AR. Immunoblotting was carried out to determine the AhR expression in cells that do not express the AR. Of the lines examined, only LNCaP and MCF-7 cells express both the AR and the AhR. The rat hepatoma cell line 5L express the AhR, while the 5L derived BP8 cells do not. Both human prostate cancer cell lines PC3 and LNCaP express the AhR. Tubulin was used as a loading control. Full-length blots are presented in Supplementary Figure S5. (b) AR mRNA levels were monitored in HepG2 and HuH-7 cells by real-time PCR. The relative expression of AR mRNA in HepG2 and HuH-7 was ~1000-fold less than that of LNCaP prostate cancer cells. (c) Several human cancer cell lines were examined for anti-proliferative responses to flutamide treatment by BrdU incorporation assay. Cells were exposed to the anti-androgen flutamide (50 μm) for 44 h, labeled with BrdU for 4 h and fixed. The AR dependent LNCaP and AR independent PC3 prostate cancer cells both exhibited sensitivity to flutamide treatment. The breast cancer cell line MCF-7 was also responsive to flutamide treatment. The hepatocellular carcinoma cell line HepG2 exhibited the most potent response to flutamide. *P⩽0.05; **P⩽ 0.01; ***P⩽0.001. (d) Flutamide effects are not antagonized by AR agonists. HepG2 cells were co-treated with flutamide and either dihydrotestosterone (DHT) or dehydroepiandrosterone (DHEA) to determine whether androgen signaling influences responses to flutamide. The effects of co-treatment are not statistically significant when compared to treatment with flutamide alone. (e) Ethidium monoazide (EMA) and carboxyfluorescein succinimidyl ester (CFSE) labeling was detected by flow cytometry to monitor apoptosis and proliferation, respectively. HepG2 cells were exposed to vehicle, 1 nm TCDD and 30 μm flutamide for 36 h. None of the treatments resulted in increased EMA uptake (cell death). The CFSE stain dilutes with every cell division, and proliferation is associated with decreased signal along the x axis. Flutamide showed less dilution of the CFSE label, indicating its anti-proliferative effects.
Having compared AhR and AR expression across a number of cell lines, we next examined the responses of these various cancer cell lines to flutamide. As expected, flutamide reduced proliferation of the AR expressing LNCaP prostate cancer cell line, and also that of MCF-7 breast cancer cells (Figure 2c and Supplementary Figure S3). Excitingly, we also observed decreased cell numbers in cell lines that do not express AR upon flutamide treatment (Figure 2c and Supplementary Figure S3). The most potent anti-proliferative effects of flutamide treatment were observed in HepG2 human hepatocellular carcinoma cells, which do not express the AR but express high levels of AhR (Figures 2a and c and Supplementary Figure S3). To ensure that these effects were not due to the low basal expression of AR, we conducted cell viability experiments in HepG2 cells in the presence of AR agonists dihydrotestosterone and dehydroepiandrosterone (Figure 2d and Supplementary Figure S3). The effect of flutamide alone on HepG2 cells was the same regardless of co-treatment with dihydrotestosterone or dehydroepiandrosterone, suggesting that any potential residual expression of AR did not influence flutamide-induced effects. Of note, flutamide also activated AhR-mediated transcription and inhibited the growth of AR-negative HuH-7 cells (Supplementary Figure S3). Together, these experiments illustrate the AR-independent growth suppression by flutamide.
The observed reduction in cell numbers could be due to apoptosis or decreased proliferation. In order to distinguish which endpoint was responsible for the observed effects of flutamide, we conducted apoptosis and proliferation assays. Flutamide induced a robust anti-proliferative response in HepG2 cells as determined by decrease in BrdU incorporation (Figure 2c), but did not induce apoptosis (Supplementary Figure S4). These observations were corroborated by flow cytometry using carboxyfluorescein succinimidyl ester and ethidium monoazide staining to monitor proliferation and apoptosis, respectively, in HepG2 cells (Figure 2e). Higher carboxyfluorescein succinimidyl ester fluorescence intensity, an indication of fewer cellular divisions, was observed in flutamide-treated cells compared with vehicle-treated cells. There was no change in ethidium monoazide positive cells after flutamide treatment. Taken together, these data indicated that flutamide causes AR-independent suppression of cancer cell growth through non-apoptotic pathways.
The AhR mediates anti-proliferative effects of flutamide in hepatoma cells
To investigate a potential role for the AhR in mediating the anti-proliferative effects of flutamide, we employed cell lines with or without AhR expression. 5L rat hepatoma cells express high levels of AhR, whereas BP8 cells (derived from 5L cells) are AhR negative (Figure 2a); AR is not expressed in either 5L or BP8 cells (Figure 2a). Treatment with flutamide induced potent growth inhibition of 5L cells in a dose and time-dependent manner, whereas flutamide had a minimal effect on BP8 cell proliferation (Figure 3a). In order to directly determine the role of AhR in flutamide-induced growth inhibition, we utilized small interfering RNAs (siRNAs) to suppress AhR expression in HepG2 cells (Figure 3b). In control luciferase siRNA transfected cells, flutamide treatment resulted in a strong decrease in proliferation (Figures 3c and d). On the other hand, suppression of the AhR expression by AhR siRNA transfection strongly reversed the growth inhibitory effects of flutamide (Figures 3c and d). Taken together, these data provide compelling evidence that the AhR mediates the anti-proliferative effects of flutamide in hepatoma cell lines from distinct species.
Anti-proliferative effects of flutamide are AhR-dependent. (a) Flutamide suppresses growth of AhR expressing 5L cells. Proliferation of the AhR expressing rat hepatoma 5L cells was monitored by BrdU incorporation assay. A potent dose-dependent reduction in BrdU incorporation was observed in 5L cells treated with flutamide (gray bars). BP8 cells (black bars), which do not express the AhR, were relatively insensitive to flutamide. 5L cells were sensitive to TCDD as reported.32 Cells were treated either for 24 or 48 h, followed by a 4 h pulse with BrdU. BrdU values for vehicle-treated cells are normalized to 100%. (b) Suppression of AhR expression in HepG2 cells. AhR-specific siRNA (siAhR) or control luciferase siRNA (siLuc) transfected cells were analyzed for AhR expression by western blotting. Full-length blots are presented in Supplementary Figure S6. (c) AhR mediates the anti-proliferative effects of flutamide. Proliferation of HepG2 cells treated with 50 μm flutamide was monitored using BrdU incorporation by immunostaining. HepG2 cells transfected with either siAhR or siLuc were treated with flutamide for 24 h, followed by a 4 h pulse with BrdU. BrdU was detected with alexafluor-488 conjugated antibody against BrdU. Flutamide reduced the number of cells incorporating BrdU (FITC) in siLuc transfected control cells compared with siAhR transfected cells. (d) Quantification of immunostaining experiment. Flutamide treatment resulted in drastic reduction of proliferating cells in the control siRNA treated cells (white bars). Upon AhR knockdown, flutamide treatment has reduced effect (black bars), indicating the AhR dependency of flutamide-induced responses in HepG2 cells. *P⩽0.05; **P⩽0.01; ***P⩽0.001; ****P⩽0.0001.
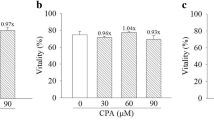
In an effort to determine whether a structural template from flutamide can be inferred for AhR activation, we identified a number of structural analogs (Figure 4). Specifically, we selected analogs based on a subtle chemical substitutions of the side groups. We also included the known AR antagonist nilutamide. Surprisingly, none of the analogs exhibited AhR agonist activity (Figure 4a), although some of the flutamide analogs were AhR antagonists (Figure 4b). We examined whether these AhR antagonists could exhibit growth inhibitory effects similar to flutamide. BrdU incorporation assays revealed that these analogs did not have anti-proliferative effects in HepG2 cells (Figure 4c). Thus, the absence of growth inhibitory effects coupled with the failure of flutamide analogs to activate AhR signaling suggests that transcriptional activation of the AhR is required for flutamide-induced growth suppression.
Flutamide (FLU) analogs do not activate the AhR. (a) Structural analogs of FLU do not activate AhR-dependent transcription. Hepa1 cells transfected with AhRE-luciferase (luc) were treated with 20 μm of the indicated compound, and AhR reporter activity was determined after 24 h. No appreciable transcriptional activity was observed for any of the analogs. (b) Structural analogs of FLU can act as AhR antagonists. Hepa1 cells transfected with AhRE-luc were treated with 20 μm of the indicated compounds. Four hours later cells were exposed to an additional treatment of either 300 pm TCDD, 20 μm FLU or vehicle to test for reductions in TCDD or FLU-induced transcriptional activation of the AhR. Several compounds reduced AhR-dependent transcription. (c) Agonist-induced transcriptional activity of the AhR may be required for anti-proliferative effects. HepG2 cells were treated with identified FLU analogs also determined to be transcriptional antagonists. After 48 h of treatment with 30 μm of the indicated compounds, cells were labeled with BrdU for 4 h and fixed. Only FLU significantly reduced proliferation. *P⩽0.05; **P⩽ 0.01; ***P⩽0.001; ****P⩽0.0001. (d) Structural analogs of FLU. FLU analogs were preferentially selected for subtle changes in side group chemistry. The anti-androgen drug nilutamide is also included due to the structural similarities with FLU.
AhR activation by flutamide results in increased levels of p27Kip1, p15INK and TGF-β1
To investigate the mechanism of the AhR-dependent effects of flutamide, we examined the ability of flutamide to alter expression of genes known to regulate cellular proliferation. Previous studies have shown that the p27Kip1 cell cycle inhibitor is upregulated in 5L cells in an AhR-dependent manner by TCDD.32 We monitored p27Kip1 protein levels upon flutamide treatment in 5L cells and observed increased p27Kip1 expression similar to TCDD treatment while BP8 cells (AhR negative) did not exhibit increased levels of p27Kip1 (Figure 5a). These data indicated that the increased expression of p27Kip1 by flutamide was AhR dependent. We next determined whether p27Kip1 levels were also increased in HepG2 cells treated with flutamide. Western blotting identified increased protein levels of both p27Kip1 and p15INK cell cycle inhibitors from flutamide treatment (Figure 5b). Examination of the transcript levels of p27Kip1 and p15INK in HepG2 cells revealed that p15INK, but not p27Kip1, was upregulated by flutamide (Figure 5c). Therefore, treatment of HepG2 cells with flutamide results in increased protein levels of both p27Kip1 and p15INK, but increased mRNA levels of only p15INK.
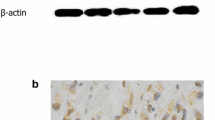
TGF-β signaling is activated by flutamide. (a) Flutamide increases p27kip1 protein levels in 5L cells. Increased protein levels of p27kip1 in 5L cells upon treatment with 1 nm TCDD or 50 μm flutamide. AhR-deficient BP8 cells show no appreciable increase in p27kip1. Full-length blots are presented in Supplementary Figure S6B. (b) Flutamide increases p15INK and p27kip1 protein levels in HepG2 cells. Flutamide treatment of HepG2 cells showed enhanced levels of p27kip1 and p15INK over a 24 h time period. Full-length blots are presented in Supplementary Figure S7. (c) Flutamide increases mRNA levels of p15INK but not p27kip1. qPCR analysis revealed that 50 μm flutamide upregulated p15INK but not p27kip1 mRNA in HepG2 cells. TCDD (1 nm) did not significantly alter p15INK or p27kip1 mRNA expression after 24 h. GAPDH expression was used for normalization across various treatments. (d) Flutamide increases mRNA levels of TGF-β1. Three isoforms of TGF-β were examined by qPCR analysis. TGF-β1 was upregulated in response to flutamide (50 μm) treatment in HepG2 cells. TCDD (1 nm) showed no effect on mRNA levels of TGF-β isoforms 1, 2 or 3. GAPDH expression was used for normalization across various treatments. (e) p15INK or TGF-β1 mRNA levels do not increase in growth-arrested cells. HepG2 cells were cultured in DMEM without FBS for 48 h, treated with vehicle, 1 nm TCDD or 50 μm flutamide for 24 h. Transcript levels were detected by qPCR analysis. Flutamide treatment resulted in upregulation of TGF-β1 and p15INK, and is thus not a consequence of inhibited cell growth. (f) Flutamide treatment results in increased TGF-β1 protein levels. Western blot detection of latency-associated peptide (hLAP) specific for TGF- β1 in HepG2 cells indicates that flutamide treatment (50 μm) results in increased protein levels when compared with the vehicle control. This upregulation was observed throughout the indicated time points. TCDD (1 nm) treatment for 36 h showed no appreciable increase in the TGF-β-hLAP protein levels. GAPDH is included as a loading control. Full-length blots are presented in Supplementary Figure S8. (g) Flutamide increases TGF-β1 levels in HepG2 cells. Immunostaining for the hLAP in HepG2 cells show that flutamide-treated cells (50 μm) have increased levels of the TGF-β-LAP complex. (h) Flow cytometric analysis of flutamide-treated cells showed increased hLAP protein staining upon treatment with flutamide. Cells were treated for 24 h with flutamide or TCDD (1nM) as indicated. Vehicle-treated cells (blue); TCDD (gray); flutamide (green). *P⩽0.05; ***P⩽0.001.
TGF-β is known to regulate p27Kip1 and p15INK expression39 by protein stabilization and transcriptional upregulation, respectively. TGF-β is an extracellular cytokine that can influence cell proliferation, differentiation and apoptosis.40 TGF-β is processed and secreted with its latency-associated peptide (LAP).40 Activated TGF-β binds to membrane-bound serine–threonine kinase receptors, which phosphorylate Smad family member proteins. Activated SMAD complexes compartmentalize to the nucleus where they stimulate expression of target genes contingent on expression profiles of master transcription factors,40 which can result in a variety of responses including decreased proliferation. We examined mRNA expression of the three known isoforms of TGF-β and discovered that TGF-β1, but not TGF-β2 or TGF-β3, was upregulated by flutamide (Figure 5d). We next asked whether the increase in p15INK and TGF-β1 mRNA was a consequence of cells undergoing growth arrest upon treatment with flutamide. To address this possibility, HepG2 cells were growth arrested by serum starvation for 48 h before treatment with flutamide for an additional 16 h. Flutamide significantly increased p15INK and TGF-β1 mRNA levels even in growth arrested HepG2 cells (Figure 5e), suggesting that TGF-β1 and p15INK upregulation is not a consequence of a halt in cell proliferation by flutamide.
The mature isoforms of human and bovine TGF-β1 share 100% sequence homology. Therefore, to detect TGF-β1 under culture conditions using fetal bovine serum, we utilized an latency associated peptide (hLAP) antibody specific to human TGF-β1 as a pro-form complex in HepG2 cells. Immunoblotting for hLAP specific to TGF-β1 also revealed increased expression of TGF-β1 in flutamide-treated cells for up to 48 h compared with vehicle (Figure 5f). Examination of the protein levels by immunostaining experiments also showed a strong increase in TGF-β1 detection upon flutamide treatment (Figure 5g). We further confirmed upregulation of TGF-β1 protein levels by flow cytometry in flutamide-treated cells (Figure 5h). Interestingly, TCDD did not affect TGF-β signaling in HepG2 cells (Figures 5b–f and h). These studies revealed that flutamide, but not TCDD, upregulates TGF-β1, providing further evidence of a ligand selective regulation of downstream target genes by the AhR.
TGF-β signaling is activated by flutamide in an AhR-dependent manner
We postulated that flutamide activates the AhR, leading to increased levels of TGF-β1, which in turn upregulates p15INK and other TGF-β regulated genes to suppress cellular proliferation. To test this, we examined the temporal transcriptional profile of TGF-β1 and p15INK upon treatment with flutamide. As expected, TGF-β1 upregulation preceded the induction of its target gene, p15INK (Figure 6a). We next examined whether activation of the AhR by flutamide was required for upregulation of TGF-β1. Suppression of AhR expression by AhR-specific siRNA inhibited flutamide-induced TGF-β1 upregulation (Figures 6b and c). We also examined induction of p15INK by flutamide in the absence of AhR, and found that flutamide-induced upregulation of p15INK mRNA was abrogated upon suppression of AhR expression (Figure 6c). To provide an additional line of evidence confirming these observations, we transduced HepG2 cells with an short hairpin RNA (shRNA) targeting the AhR. While flutamide-induced TGF-β1 protein could be detected by immunostaining followed by flow cytometry, a similar induction was not seen in HepG2 cells with shRNA-mediated AhR knockdown (Figure 6d and Supplementary Figure S9). Likewise, TCDD failed to induce expression of TGF-β1 in the presence or absence of AhR, which was consistent with the data presented in Figures 5f and h. Taken together, these data indicated that flutamide, but not TCDD, induces TGF-β1 both at the transcript (Figure 6c) and protein levels (Figure 6d) in an AhR-dependent manner. To determine whether the AhR is a direct transcriptional activator of TGF-β1, we co-treated cells with the protein synthesis inhibitor cycloheximide. Interestingly, cycloheximide treatment blocked flutamide-induced upregulation of both TGF-β1 and p15INK mRNA (Figure 6e), suggesting that TGF-β1 may be a secondary target gene of the AhR.
Activation of TGF-β1 signaling by flutamide is AhR-dependent. (a) TGF-β1 upregulation precedes p15INK mRNA increase in response to flutamide. HepG2 transcript levels for TGF-β1 and one of its downstream targets, p15INK, were monitored by qPCR. Flutamide (50 μm) treatment resulted in maximal induction of TGF-β1 at 18 h and mRNA levels decreased after that time point. TGF-β target p15INK transcript levels were highest at 36 h. GAPDH expression was used for normalization across various treatments. Fold inductions were calculated relative to vehicle controls. (b) Suppression of AhR expression in HepG2 cells. Western blot analysis of AhR knockdown cells used for qPCR experiments showing strong reduction in AhR protein expression in the siAhR transfected HepG2 cells compared with the control siLuc transfected cells. Full-length blots are presented in Supplementary Figure S8. (c) AhR mediates flutamide-induced increases of TGF-β1 and p15INK mRNA. HepG2 cells were transfected with AhR siRNA to suppress AhR expression or control siRNA (luciferase; siLuc) for 48 h. TGF-β1 transcript levels were highly upregulated in flutamide-treated cells (50 μm) compared with vehicle-treated cells. TCDD treatment did not change TGF-β1 transcript levels. Upon suppression of AhR expression (dark bars), the upregulation of TGF-β1 and p15INK was strongly inhibited, indicating AhR dependency. (d) TGF-β1 protein levels are increased by flutamide in an AhR-dependent manner. HepG2 cells were transfected with a shRNA specific to AhR and were treated with flutamide. TGF-β1 (hLAP) protein levels were analyzed by flow cytometry and found to be increased by flutamide (blue) as compared to vehicle control (red) only when AhR was expressed. AhR knockdown data is shown in Supplementary Figure S9. (e) Protein synthesis is required for AhR-dependent upregulation of TGF-β1. Co-treatment with the protein synthesis inhibitor cycloheximide abolished flutamide-induced upregulation of TGF-β1 and p15INK mRNA levels. (f) TGF-β signaling is activated in flutamide treated HepG2 cells. TGF-β responsive genes were examined by qPCR after 36 h of vehicle, 1 nm TCDD or 50 μm flutamide treatment. Several genes known to be regulated by TGF-β were transcriptionally upregulated upon flutamide treatment in HepG2 cells. VEGFA expression did not change by TCDD as well as flutamide treatments (data also presented in Supplementary Figure S11). *P⩽0.05; **P⩽0.01; ***P⩽0.001; ****P⩽0.0001.
As a secreted cytokine that initiates a SMAD signaling cascade, TGF-β activation upregulates a variety of downstream target genes governed by SMAD interactions with tissue-specific master transcription factors.40 In order to determine what other target genes are perturbed by TGF-β1 induction, we examined 84 TGF-β regulated genes using a targeted quantitative PCR array. We observed a number of TGF-β targets that were either up or downregulated after flutamide treatment and importantly, the quantitative PCR array independently confirmed upregulation of TGF-β1 and p15INK. In addition, several TGF-β downstream genes including latent-TGF-β-binding protein 2 (LTBP2), urokinase-type plasminogen activator (PLAU), bone morphogenic protein-6 (BMP6), and insulin-like growth factor-binding protein 3 (IGFBP3; Figure 6f and Supplementary Figure S11) were also upregulated by flutamide. Vascular endothelial growth factor-A mRNA levels remained unaltered by both TCDD and flutamide (Figure 6f and Supplementary Figure S11). These data provide compelling evidence that AhR activation by flutamide results in upregulation of TGF-β1, subsequent activation of TGF-β signaling, and induction of p15INK and several other TGF-β regulated genes. Importantly, this AhR regulated transcriptional signature was unique to flutamide as compared to TCDD.
Disruption of TGF-β1 expression attenuates growth suppressive effects of flutamide
The result of increased secretion of TGF-β has proven to be enigmatic in the context of cellular growth. Increases in TGF-β can have both tumor promoting and suppressive effects depending on the tissue and tumor profile.40 To determine the effect of TGF-β1 activation on HepG2 cells, we used recombinant TGF-β1 and found that HepG2 cells are sensitive to TGF-β1-induced growth suppression (Figure 7a). To directly interrogate the relationship of increased TGF-β1 expression with increased levels of p27Kip1, we treated HepG2 cells with TGF-β1 and monitored changes in the expression of p27Kip1. We observed increased p27Kip1 protein expression in both TGF-β1- and flutamide-treated cells (Figure 7b). As described above, we hypothesized that activation of the AhR by flutamide leads to increased expression of TGF-β1, which in turn is responsible for the observed anti-proliferative effects. To address this possibility, we generated stable TGF-β1 shRNA expressing HepG2 cells. Specifically, we utilized five different shRNA constructs from which three independent lines with substantially reduced levels of TGF-β were obtained, designated as HepG2ΔTGFβ (Figure 7c). We monitored flutamide-induced TGF-β protein levels in the HepG2ΔTGFβ clones by western blot. Flutamide induced increased expression of TGF-β protein levels at 24 and 48 h in control HepG2 cells but not in HepG2ΔTGFβ cells (Figure 7d), while CYP1A1 was induced regardless of TGF-β status (Supplementary Figures S12 and 13). Having shown that flutamide does not induce TGF-β in the HepG2ΔTGFβ lines, we next evaluated the response of these cells to flutamide. The three independent HepG2ΔTGFβ lines displayed a significant reduction in sensitivity to flutamide treatment (Figure 7e) compared with the parental line. Specifically, BrdU incorporation followed by flow cytometry of the control (HepG2ΔTGFβ#4) cells and TGF-β1 shRNA expressing cells (HepG2ΔTGFβ#3) confirmed the requirement of TGF-β1 for flutamide-induced growth inhibition (Figure 7f). Thus, flutamide induces TGF-β1 expression in an AhR-dependent manner, and this increased expression of TGF-β1 inhibits HepG2 cellular proliferation.
TGF-β mediates the anti-proliferative effect of flutamide. (a) TGF-β1 causes anti-proliferative effects in HepG2 cells. BrdU incorporation analysis revealed that HepG2 cells are responsive to TGF-β1 treatment in a dose-dependent manner. (b) TGF-β1 treatment of HepG2 cells increases p27kip1 protein levels. Western blotting revealed increases in p27kip1 levels in HepG2 cells treated with 1 ng/ml TGF-β1, flutamide (50 μm). Full-length blots are presented in Supplementary Figure S10. (c) Generation of stable TGF-β1 knockdown lines. Lentiviral transduction of TGF-β1 shRNA constructs in HepG2 cells resulted in generation of three independent HepG2ΔTGFβ lines with low expression of TGF-β1 as detected by western blotting. Full-length blots are presented in Supplementary Figure S10. (d) HepG2ΔTGFβ lines do not show appreciable increases of TGF-β1 when treated with flutamide. Western blot analysis indicates that TGF-β1 protein levels were not upregulated in HEPG2ΔTGFβ1 cell lines when treated with flutamide (50 μm). Parent HepG2 cells showed a potent increase in TGF-β1 protein levels when treated with flutamide. Full-length blots are presented in Supplementary Figure S13. (e) HepG2ΔTGFβ lines are less sensitive to flutamide treatment. Analysis of BrdU incorporation in HepG2ΔTGFβ lines showed decreased sensitivity to flutamide (50 μm) treatment after 48 h. (f) HepG2ΔTGFβ1 clone #3 (ΔTGFβ#3) and HepG2 clone #4 control (ΔTGFβ #4) cells were treated with vehicle or 50 μm flutamide for 96 h. BrdU incorporation assay showing that cells without TGFβ1 knockdown (TGFβ#4, panel c) do not have active proliferating populations when exposed to flutamide for prolonged treatment times. HepG2ΔTGFβ#3 lacking TGF-β1 expression are not sensitive to flutamide. *P⩽0.05; **P⩽ 0.01; ***P⩽0.001; ****P⩽0.0001.
Discussion
AhR biology has been historically characterized in the context of TCDD, a potent metabolically stable ligand that causes aberrant and constitutive activation of the AhR, although the endogenous role of the AhR is not completely understood. The standard measurement of AhR activation is the induction of CYP1A1, which is highly upregulated by TCDD.2 CYP1A1 is a non-specific biomarker for AhR activation, in that CYP1A1 induction is not synonymous with functional consequences of AhR activation or responsible for TCDD-induced toxicity.9, 41 Our independently conducted screens for AhR ligands have identified several putative AhR ligands including leflunomide, raloxifene and benzimidazoisoquinolines.35, 38, 42, 43 In this study, we found that the FDA-approved AR antagonist flutamide (Eulexin) is also an AhR ligand that initiates distinct AhR transcriptional activity and AhR-dependent growth inhibitory effects in human hepatocellular carcinoma cells. We carefully characterized these AR-independent effects of flutamide as AhR-dependent in order to build upon the emerging paradigm for the AhR as a therapeutic target in cancer.
Flutamide is utilized for the treatment of androgen-responsive prostate cancers. In the present study, we found that flutamide is an AhR ligand that induces AhR transcriptional activity and has AhR-dependent anti-proliferative effects on hepatocellular carcinoma cells. Specifically, we observed that flutamide induces nuclear translocation of the AhR as well as increased expression of the AhR target gene CYP1A1 (Figure 1). Because flutamide undergoes first pass metabolism, we also investigated the ability of 2HFL, the primary metabolite of flutamide, to activate the AhR. We showed that 2HFL did not cause nuclear translocation or increased transcriptional activity of the AhR, indicating that the parent compound flutamide, but not its metabolite 2HFL, is an AhR agonist (Figure 1e and Supplementary Figure S2).
Flutamide is known to reduce cellular growth in AR-positive cancer cells (Figure 2c).36 Therefore, we examined the potential role of AhR in mediating the effects of flutamide in AR-negative cells (Figures 2a and b). We established that even in the absence of the AR, flutamide exhibits growth-suppressive effects in distinct cancer cell lines (Figures 2c–e). Our studies also identified the AhR as the mediator of flutamide-induced effects in AR-negative hepatoma cells (Figure 3a). Specifically, transient knockdown of AhR in HepG2 cells confirmed that the AhR mediates the growth-suppressive effects of flutamide (Figures 3b–d). Likewise, flutamide analogs that acted as AhR antagonists did not exhibit growth-inhibitory effects (Figures 4b–d).
To identify the potential downstream mediators of flutamide-induced AhR-dependent growth inhibition, we began with the previous observation that AhR regulates expression of p27Kip1, a cyclin dependent kinase inhibitor.32 We examined p27Kip1 protein levels in 5L rat hepatoma cells and observed that flutamide treatment upregulated p27Kip1 similar to TCDD,32 and that these changes were AhR dependent (Figure 5a). We also found that flutamide upregulated cyclin dependent kinase inhibitor p15INK expression in addition to p27Kip1 in HepG2 cells (Figure 5b). This observation led us to investigate the role of TGF-β in mediating the effects of flutamide, as TGF-β is reported to mediate expression of p27Kip1 and p15INK at the protein and transcript levels, respectively.44, 45, 46 We discovered that TGF-β1 is upregulated by flutamide in HepG2 cells (Figure 5d) and showed that while expression of p27Kip1 was increased at the protein level by flutamide, there was no appreciable increase in p27Kip1 mRNA. Likewise, p15INK mRNA was upregulated by flutamide in accordance with known TGF-β1 signaling pathways.44 We also demonstrated that upregulation of TGF-β1 and p15INK mRNA by flutamide was not simply a consequence of a halt in cell proliferation, but rather due to AhR activation (Figure 5e). Importantly, loss of AhR expression attenuated TGF-β1 and p15INK upregulation, indicating that TGF-β1 expression is downstream of AhR activation (Figures 6b and c). Further investigation of the TGF-β pathway revealed that other downstream TGF-β1 target genes, including IGFBP3 and BMP6, were also upregulated in response to flutamide treatment (Figure 6f and Supplementary Figure S11). We determined that flutamide-induced TGF-β1 induction preceded upregulation of p15INK mRNA (Figure 6a) and BMP6 (Supplementary Figure S11). Specifically, siRNA knockdown of AhR demonstrated its requirement for induction of TGF-β signaling in response to flutamide treatment (Figures 6b–d and Supplementary Figure S9). HepG2 cells stably expressing a TGF-β1 shRNA (HepG2ΔTGFβ) were significantly less responsive to flutamide (Figure 7e), confirming that the TGF-β1 pathway is involved in the AhR-dependent anti-proliferative endpoints of flutamide. The residual effects of flutamide in HepG2ΔTGFβ cells may have been due to other proteins such as BMP6, a member of the TGF-β superfamily, which was also induced by flutamide (Figure 6f and Supplementary Figure S11). In accordance with this possibility, we also found that flutamide increased levels of IGFBP3 (Figure 6f), which is also known to interact with TGF-β signaling and influence cellular growth.47 Thus, these data strongly indicate that the AhR indirectly regulates a number of genes related to the TGF-β pathway.
There have been reports implicating the AhR in the regulation of TGF-β signaling.48, 49, 50, 51, 52 AhR null fibroblasts grow slower and secrete TGF-β1, and inhibition of TGF-β/Smad signaling rescues the growth rates of AhR null fibroblasts.48, 49, 50, 51, 52 In addition, the AhR ligand Benzo(a)pyrene, but not TCDD, induces the expression of TGF-β1 in human placental choriocarcinoma JEG-3 cells.53 In this study, we found that flutamide induced AhR-dependent upregulation of TGF-β1, which we in turn linked to suppression of hepatocellular carcinoma cell proliferation. Although both TCDD and flutamide upregulated the AhR target gene CYP1A1, only flutamide upregulated TGF-β1, providing significant evidence for ligand selective outcomes of AhR activation (Figures 1b and 5d). In addition, pretreatment of HepG2 cells with the protein synthesis inhibitor cycloheximide abolished flutamide-induced TGF-β1 mRNA upregulation, suggesting that TGF-β1 may be a secondary target gene of the AhR (Figure 6e). We showed that HepG2 cells were sensitive to TGF-β1, and that upregulation of TGF-β1 by flutamide transcriptionally activated TGF-β1 target genes associated with cell cycle regulation (Figure 6f).
We previously characterized the AhR ligand-binding pocket and showed that a remarkable number of compounds are able to dock into the AhR ligand-binding pocket.37, 58 Importantly, virtual ligand screening utilizing such AhR ligand-binding pocket models can help to identify new AhR ligands with desired functionality.37, 54 In addition, numerous compounds currently used in the clinic including leflunomide, raloxifene, flutamide, tranilast, 4-hydroxytamoxifen and omeprazole have been reported to influence AhR signaling, and the effects of these compounds appear to be cell-type dependent.9, 35, 38, 43, 55, 56, 57, 58 We previously reported that leflunomide is an AhR agonist and that it induces AhR-dependent growth inhibition of A375 melanoma cells.38 Certain AhR agonists have been reported to induce differentiation of breast cancer cells31 and an antimetastic microRNA-335 has been reported to be upregulated by 6-methyl-1,3,-trichlorodibenzofuran and TCDD in BT474 and MDA-MB-231 cells.57 We also recently reported that raloxifene, an FDA-approved drug for breast cancer chemoprevention and treatment of osteoporosis, activates AhR-mediated transcription and induces AhR-dependent apoptosis in both hepatoma and estrogen receptor-negative breast cancer cells.43 In the same study, we reported the expression of AhR in different breast cancer subtypes, and that higher AhR expression is associated with both increased overall survival and distant metastasis-free survival.43 Taken together, these studies suggest a role for AhR in tumor suppression as well as the exciting possibility of utilizing AhR ligands for cancer prevention and treatment.
The ability of certain AhR ligands to induce regulatory T cells has generated interest in developing AhR ligands for therapeutic treatment of immune-mediated diseases, and has provided further evidence that the downstream effects of AhR activation can vary for different AhR ligands and are dependent on cell type. Specifically, we recently reported identification and detailed characterization of 10-chloro-7H-benzimidazo[2,1-a]benzo[de]Iso-quinolin-7-one (10-Cl-BBQ) as a nanomolar-affinity AhR ligand and potent inducer of AhR-dependent regulatory T cells.42 Non-toxic AhR ligands such as 10-Cl-BBQ are promising compounds for treatment of autoimmune diseases.42 We are also currently investigating the functional consequences of AhR activation by 10-Cl-BBQ in cancer cells.
In summary, our data indicate ligand selective coordination of AhR transcriptional programs. Specifically, we showed that the FDA-approved drug flutamide is an AhR ligand, and that the AhR mediates the growth-suppressive effects of flutamide in the absence of its known target, the AR. In terms of its mechanism of action, flutamide upregulated TGF-β1 via AhR and suppressed the growth of human hepatocellular carcinoma cells. Therefore, flutamide may be effective not only in AR-positive prostate cancers, but also in other AhR-positive cancers such as hepatocellular carcinomas that are sensitive to TGF-β1 signaling. Several compounds that have been used safely in the clinic for many years activate AhR signaling and have anti-cancer effects, raising the exciting possibility of repurposing some of these compounds or their higher affinity analogs as AhR-selective anti-cancer therapeutics.
Materials and methods
Cell culture
Human HepG2 hepatocellular carcinoma cells, mouse Hepa1, mouse Hepa1c1c7, 5L, BP8, HuH-7, MCF-7 and MDA-MB-231 cells were cultured in Dulbecco's Modified Eagle's medium with l-glutamine (Mediatech, Manassas, VA, USA) supplemented with 10% fetal bovine serum (Tissue Culture Biologicals, Tulare, CA, USA) with 10 000 U/ml penicillin streptomycin (Mediatech) in a humidified 5% CO2 atmosphere. LNCaP and PC3 cells were cultured in RPMI 1640 (Mediatech). Cells were typically passaged every 3 days at a dilution of 1:4. Cell lines were obtained from ATCC(Manassas, VA, USA), with the exception of the C12/C12 AhR and 5L/BP8 cell lines, which were described previously.26, 37
Chemicals
Flutamide was purchased from Sigma (St Louis, MO, USA) (Cat#F9397-1G), and all other compounds were obtained from Sigma unless otherwise noted. All stock solutions were prepared in dimetyl sulfoxide and stored at −20 °C.
Viability and reporter gene assays
Cells were seeded in 96-well plates at a density of 10 000 cells/well in 100 μl of media. Cells were treated 24 h after plating as indicated. For reporter gene assays cells were lysed 24 h after treatment and reporter activity was measured. Values were presented as fold inductions relative to vehicle-treated cells. A TR717 microplate luminometer (Berthold Technologies, Bad Wildbad, Germany) was used to detect luciferase activity. Each experiment included at least three replicate wells, and three independent experimental replicates were evaluated. Viability assays utilized the MTS viability kit (Promega, Madison, WI, USA) and were assayed with a spectrophotometer according to the manufacturer’s instructions.
Gene inductions studies
HepG2 cells were seeded in 6-well plates and treated 24 h after plating as indicated. RNA was prepared using the GenElute Mammalian total RNA miniprep kit (Sigma). First strand synthesis of complementary DNA was generated using Superscript III reverse transcriptase kit (Invitrogen, Carlsbad, CA, USA). Transcript levels were monitored using the following pairs of primers: CYP1A1: FP 5′-GTCCCCTTCACCATCCC-3′, RP 5′-CAGGAAGAGAAAGACCTCC-3′, IGFBP3: FP 5′-CACTGAATCACCTGAAGTTCCTC-3′, RP 5′-AGGGCGACACTGCTTTTTCTT-3′; BMP6: FP 5′-AGCGACACCACAAAGAGTTCA-3′, RP 5′-GCTGATGCTCCTGTAAGACTTGA-3′; LTBP2: FP 5′-AGCACCAACCACTGTATCAAAC-3′, RP 5′-CTCATCGGGAATGACCTCCTC-3′; PLAU: FP 5′-GGGAATGGTCACTTTTACCGAG-3′, RP 5′-GGGCATGGTACGTTTGCTG-3′; GAPDH: FP 5′-ACCTTTGACGCTGGGGCTGG-3′, RP 5′-CTCTCTTCCTCTTGTGCTCTTGCTGG-3′; p27: FP 5′-AAGAGGCGAGCCAGCGCAAG-3′, RP 5′-ACCGGCATTTGGGGAACCGTC-3′; p15: FP 5′-GCCCCAAGCCGCAGAAGGAC-3′, RP 5′-GCCCATCATCATGACCTGGATCGC-3′; TGFβ1: FP 5′-CAAGCAGAGTACACACAGCAT-3′, RP 5′-TGCTCCACTTTTAACTTGAGCC-3′; TGFβ2: FP 5′-CCCCGGAGGTGATTTCCATC-3′, RP 5′-CAGACAGTTTCGGAGGGGA-3′; TGFβ3: FP 5′-TCAGCCTCTCTCTGTCCACTT-3′, RP 5′-CATCACCGTTGGCTCAGGG-3′; AR set 1: FP 5′-GACGACCAGATGGCTGTCATT-3′, RP 5′-GGGCGAAGTAGAGCATCCT-3′; AR set 2: FP 5′-GCTGCCTCACAGTATGGGAA-3′, RP 5′-CCCAGGCACTTCACTGTAGG-3′. Three experimental replicates were each normalized to housekeeping genes and compared with the vehicle-treated samples using the ΔΔCT method.
AhR localization and immunostaining
HepG2 cells were seeded at 20 000 cells/well in 8-well chamber slides. The following day, cells were treated with the indicated compounds for 90 min. At the end of the treatment, cells were fixed with 3.7% paraformaldehyde, followed by a 10-min incubation with 0.1% Triton X-100. After fixing, 1% bovine serum albumin (Fraction V) was used as the blocking reagent overnight at 4 °C. Primary staining was performed with an AhR antibody (1:600, ENZO, Farmingdale, NY, USA). Cells were washed 3 times with phosphate-buffered saline, and re-blocked for 1 h at room temperature. Cells were then stained with a fluorescein isothiocyanate-conjugated goat-anti-rabbit secondary antibody (Southern Biotech, Birmingham, AL, USA) for 1 h at room temperature. Slides were then washed with phosphate-buffered saline three times and stained with Pro-Fade staining reagent with DAPI (4',6-diamidino-2-phenylindole; Invitrogen), and slides were sealed. Cells were imaged with an Axiovert 200 IM (Zeiss, Jena, Germany) equipped with Metamorph image capture software. For detection of the AR, we utilized the AR (N-20): sc 816 from Santa Cruz Biotechnology (Dallas, TX, USA), which detects AR of mouse, rat and human origin. For detection of TGF-β, we utilized the hLAP antibody AF-246-NA from R&D systems (Minneapolis, MN, USA), which is specific to TGF-β1. Additional antibodies: CYP1A1 (AB1258 from EMD Millipore, Billerica, MA, USA; AHP611Z from AbD Serotech, Raleigh, NC, USA), p15 INK4B and p27Kip1 antibodies are from sampler kit 9867 from Cell Signaling Technology (Danvers, MA, USA).
BrdU incorporation and immunostaining assays
HepG2 and HepG2ΔTGFβ1 cells were seeded at 7000 cells/well in 96-well plates. 5L and BP8 cells were seeded at 5000 cells/well in 96-well plates. Cells were then treated with compounds for the indicated time points after which the cells were pulsed with BrdU for 4 h and fixed. Plates were typically stored overnight at 4 °C followed by detection of incorporated BrdU with primary and secondary antibodies. BrdU was then detected with a Molecular Devices (Sunnyvale, CA, USA) spectramax 250 at 450 and 540 nm. The difference (450–540 nm) of the two wavelengths were used as raw data and values were normalized to the vehicle-treated wells.
For the immunostaining experiments cells were seeded at 25 000 cells/well in 8-well chamber slides. Treatments began the next day for 20 h and BrdU (10 μm) labeled for an additional 4 h. Cells were fixed using the BrdU fixative/denaturing solution (Calbiochem, Billerica, MA, USA) for 20 min at room temperature. Cells were then washed with phosphate-buffered saline and blocked with 1% bovine serum albumin (Fraction V) for 4 h at room temperature. Fixed samples were incubated with a BrdU antibody conjugated with Alexaflour 488 for 2 h at room temperature. Cells were washed with phosphate-buffered saline three times and stained with Pro-Fade staining reagent with DAPI (Invitrogen), and slides were then sealed. Cells were imaged with an Axiovert 200 IM (Zeiss) equipped with Metamorph image capture software.
AhR knockdown experiments
For AhR knockdown experiments HepG2 cells were seeded at 20 000 cells/well in 8-well chamber slides. After overnight incubation, cells were transfected with 400 ng AhR siRNA (Dharmacon, Lafayette, CO, USA, target sequence GAACAGAGCAUUUACGAA) or luciferase siRNA (Dharmacon) using the Dharmafect transfection reagent. Approximately 30 h after transfection with siRNAs, cells were treated as indicated. Twenty-four hours post treatment, cells were pulsed with BrdU (Calbiochem) for 4 h, fixed with BrdU fixative/denaturing solution (Calbiochem), and incubated overnight with 1% bovine serum albumin (Fraction V) at 4 °C.
Generation of HepG2ΔTGF-β1 cells
HepG2 cells stably expressing shRNAs (Open Biosystems, Lafayette, CO, USA) for constitutive knockdown of TGF-β1 were generated by a method described previously.38 TGF-β1 knockdown was confirmed by western blot.
Homology modeling and molecular Docking
The homology model of human and mouse AhR ligand-binding domain bound to agonist TCDD was used as described in our previous work.37 Molecular Docking was performed as previously reported.37
Carboxyfluorescein succinimidyl ester staining
Carboxyfluorescein succinimidyl ester staining was performed as previously described.38 The flow cytometry data were acquired on an FC500 instrument (Beckman Coulter, Brea, CA, USA) and the data were analyzed using WinList 7.0 (Verity Software House, Topsham, ME, USA) or FlowJo (FLOWJO, LLC, Ashland, OR, USA).
Statistical analysis
Data were analyzed with Prism software Version 5.0 (GraphPad, La Jolla, CA, USA) using one-way analysis of variance with Bonferroni’s post-test. Values of P<0.05 were considered statistically significant. Results were subjected to one-way analysis of variance statistical comparisons (*P⩽0.05, **P⩽ 0.01, ***P⩽0.001 and ****P⩽0.0001).
References
Burbach KM, Poland A, Bradfield CA . Cloning of the Ah-receptor cDNA reveals a distinctive ligand-activated transcription factor. Proc Natl Acad Sci USA 1992; 89: 8185–8189.
Denison MS, Fisher JM, Whitlock JP . Inducible, receptor-dependent protein-DNA interactions at a dioxin-responsive transcriptional enhancer. Proc Natl Acad Sci USA 1988; 85: 2528–2532.
Perdew GH, Bradfield CA . Mapping the 90 kDa heat shock protein binding region of the Ah receptor. Biochem Mol Biol Int 1996; 39: 589–593.
Felts SJ, Toft DO . P23, a simple protein with complex activities. Cell Stress Chaperones 2003; 8: 108–113.
Perdew GH . Association of the Ah receptor with the 90-kda heat-shock protein. J Biol Chem 1988; 263: 13802–13805.
Carver LA, Bradfield CA . Ligand-dependent interaction of the aryl hydrocarbon receptor with a novel immunophilin homolog in vivo. J Biol Chem 1997; 272: 11452–11456.
Meyer BK, Pray-Grant MG, Vanden Heuvel JP, Perdew GH . Hepatitis B virus X-associated protein 2 is a subunit of the unliganded aryl hydrocarbon receptor core complex and exhibits transcriptional enhancer activity. Mol Cell Biol 1998; 18: 978–988.
Beischlag TV, Morales JL, Hollingshead BD, Perdew GH . The aryl hydrocarbon receptor complex and the control of gene expression. Crit Rev Eukaryot Gene Expr. 2008; 18: 207–250.
Hu W, Sorrentino C, Denison MS, Kolaja K, Fielden MR . Induction of cyp1a1 is a nonspecific biomarker of aryl hydrocarbon receptor activation: results of large scale screening of pharmaceuticals and toxicants in vivo and in vitro. Mol Pharmacol 2007; 71: 1475–1486.
Puga A, Ma C, Marlowe JL . The aryl hydrocarbon receptor cross-talks with multiple signal transduction pathways. Biochem Pharmacol 2009; 77: 713–722.
Safe S . Molecular biology of the Ah receptor and its role in carcinogenesis. Toxicol Lett 2001; 120: 1–7.
Bertazzi PA, Zocchetti C, Guercilena S, Consonni D, Tironi A, Landi MT et al. Dioxin exposure and cancer risk: a 15-year mortality study after the ''Seveso accident''. Epidemiology 1997; 8: 646–652.
Warner M, Eskenazi B, Mocarelli P, Gerthoux P, Samuels S, Needham L et al. Serum dioxin concentrations and breast cancer risk in the Seveso Women’s Health Study. Am J Epidemiol 2002; 155: s102–s102.
Hsu EL, Yoon D, Choi HH, Wang F, Taylor RT, Chen N et al. A proposed mechanism for the protective effect of dioxin against breast cancer. Toxicol Sci 2007; 98: 436–444.
Funatake CJ, Marshall NB, Kerkvliet NI . 2,3,7,8-tetrachlorodibenzo-p-dioxin afters the differentiation of alloreactive CD8(+) T cells toward a regulatory T cell phenotype by a mechanism that is dependent on aryl hydrocarbon receptor in CD4(+) T cells. J Immunotoxicol 2008; 5: 81–91.
Fernandez-Salguero P, Pineau T, Hilbert DM, McPhail T, Lee SS, Kimura S et al. Immune system impairment and hepatic fibrosis in mice lacking the dioxin-binding Ah receptor. Science 1995; 268: 722–726.
Bock KW, Kohle C . Ah receptor: dioxin-mediated toxic responses as hints to deregulated physiologic functions. Biochem Pharmacol 2006; 72: 393–404.
Lai IK, Dhakal K, Gadupudi GS, Li M, Ludewig G, Robertson LW et al. N-acetylcysteine (NAC) diminishes the severity of PCB 126-induced fatty liver in male rodents. Toxicology 2012; 302: 25–33.
Egeland GM, Sweeney MH, Fingerhut MA, Wille KK, Schnorr TM, Halperin WE . Total serum testosterone and gonadotropins in workers exposed to dioxin. Am J Epidemiol 1994; 139: 272–281.
Rier SE, Martin DC, Bowman RE, Dmowski WP, Becker JL . Endometriosis in rhesus-monkeys (Macaca-Mulatta) following chronic exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin. Fund Appl Toxicol 1993; 21: 433–441.
Abbott BD, Perdew GH, Birnbaum LS . Ah receptor in embryonic mouse palate and effects of TCDD on receptor expression. Toxicol Appl Pharm 1994; 126: 16–25.
Schmidt JV, Su GHT, Reddy JK, Simon MC, Bradfield CA . Characterization of a murine Ahr null allele: involvement of the Ah receptor in hepatic growth and development. Proc Natl Acad Sci USA 1996; 93: 6731–6736.
Fernandez-Salguero PM, Hilbert DM, Rudikoff S, Ward JM, Gonzalez FJ . Aryl-hydrocarbon receptor-deficient mice are resistant to 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced toxicity. Toxicol Appl Pharm 1996; 140: 173–179.
Gasiewicz TA, Henry EC, Collins LL . Expression and activity of aryl hydrocarbon receptors in development and cancer. Crit Rev Eukaryot Gene Expr 2008; 18: 279–321.
Mitsuhashi T, Yonemoto J, Sone H, Kosuge Y, Kosaki K, Takahashi T . In utero exposure to dioxin causes neocortical dysgenesis through the actions of p27(Kip1). Proc Natl Acad Sci USA 2010; 107: 16331–16335.
Weiss C, Kolluri SK, Kiefer F, Gottlicher M . Complementation of Ah receptor deficiency in hepatoma cells: negative feedback regulation and cell cycle control by the Ah receptor. Exp Cell Res 1996; 226: 154–163.
Puga A, Xia Y, Elferink C . Role of the aryl hydrocarbon receptor in cell cycle regulation. Chem Biol Interact 2002; 141: 117–130.
Fritz WA, Lin TM, Cardiff RD, Peterson RE . The aryl hydrocarbon receptor inhibits prostate carcinogenesis in TRAMP mice. Carcinogenesis 2007; 28: 497–505.
Fan YX, Boivin GP, Knudsen ES, Nebert DW, Xia Y, Puga A . The aryl hydrocarbon receptor functions as a tumor suppressor of liver carcinogenesis. Cancer Res 2010; 70: 212–220.
Barretina J, Caponigro G, Stransky N, Venkatesan K, Margolin AA, Kim S et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature 2012; 483: 603–607.
Hall JM, Barhoover MA, Kazmin D, McDonnell DP, Greenlee WF, Thomas RS . Activation of the aryl-hydrocarbon receptor inhibits invasive and metastatic features of human breast cancer cells and promotes breast cancer cell differentiation. Mol Endocrinol 2010; 24: 359–369.
Kolluri SK, Weiss C, Koff A, Gottlicher M . p27(Kip1) induction and inhibition of proliferation by the intracellular Ah receptor in developing thymus and hepatoma cells. Gene Dev 1999; 13: 1742–1753.
Ge NL, Elferink CJ . A direct interaction between the aryl hydrocarbon receptor and retinoblastoma protein—Linking dioxin signaling to the cell cycle. J Biol Chem 1998; 273: 22708–22713.
Kharat I, Saatcioglu F . Antiestrogenic effects of 2,3,7,8-tetrachlorodibenzo-p-dioxin are mediated by direct transcriptional interference with the liganded estrogen receptor. Cross-talk between aryl hydrocarbon- and estrogen-mediated signaling. J Biol Chem 1996; 271: 10533–10537.
O’Donnell EF, Saili KS, Koch DC, Kopparapu PR, Farrer D, Bisson WH et al. The anti-inflammatory drug leflunomide is an agonist of the aryl hydrocarbon receptor. PLos One 2010; 5: e13128.
Raghow S, Kuliyev E, Steakley M, Greenberg N, Steiner MS . Efficacious chemoprevention of primary prostate cancer by flutamide in an autochthonous transgenic model. Cancer Res 2000; 60: 4093–4097.
Bisson WH, Koch DC, O’Donnell EF, Khalil SM, Kerkvliet NI, Tanguay RL et al. Modeling of the aryl hydrocarbon receptor (AhR) ligand binding domain and its utility in virtual ligand screening to predict new AhR ligands. J Med Chem 2009; 52: 5635–5641.
O’Donnell EF, Kopparapu PR, Koch DC, Jang HS, Phillips JL, Tanguay RL et al. The aryl hydrocarbon receptor mediates leflunomide-induced growth inhibition of melanoma cells. PLos One 2012; 7: e40926.
Robson CN, Gnanapragasam V, Byrne RL, Collins AT, Neal DE . Transforming growth factor-beta 1 up-regulates p15, p21 and p27 and blocks cell cycling in G1 in human prostate epithelium. J Endocrinol 1999; 160: 257–266.
Mullen AC, Orlando DA, Newman JJ, LovÈn J, Kumar RM, Bilodeau S et al. Master transcription factors determine cell-type-specific responses to TGF-β signaling. Cell 2011; 147: 565–576.
Kolluri SK, Balduf C, Hofmann M, Gottlicher M . Novel target genes of the Ah (dioxin) receptor: transcriptional induction of N-myristoyltransferase 2. Cancer Res 2001; 61: 8534–8539.
Punj S, Kopparapu P, Jang HS, Phillips JL, Pennington J, Rohlman D et al. Benzimidazoisoquinolines: a new class of rapidly metabolized aryl hydrocarbon receptor (AhR) ligands that induce AhR-dependent Tregs and prevent murine graft-versus-host disease. PLoS One 2014; 9: e88726.
O’Donnell EF, Koch DC, Bisson WH, Jang HS, Kolluri SK . The aryl hydrocarbon receptor mediates raloxifene-induced apoptosis in estrogen receptor-negative hepatoma and breast cancer cells. Cell Death Dis 2014; 5: e1038.
Hannon GJ, Beach D . pl5INK4B is a potentia| effector of TGF-[beta]-induced cell cycle arrest. Nature 1994; 371: 257–261.
Massague J, Blain SW, Lo RS . TGF beta signaling in growth control, cancer, and heritable disorders. Cell 2000; 103: 295–309.
Reynisdottir I, Polyak K, Iavarone A, Massague J . Kip/Cip and Ink4 Cdk inhibitors cooperate to induce cell-cycle arrest in response to TGF-beta. Gene Dev 1995; 9: 1831–1845.
Fanayan S, Firth SM, Baxter RC . Signaling through the Smad pathway by insulin-like growth factor-binding protein-3 in breast cancer cells—relationship to transforming growth factor-beta 1 signaling. J Biol Chem 2002; 277: 7255–7261.
Fan Y, Boivin GP, Knudsen ES, Nebert DW, Xia Y, Puga A . The aryl hydrocarbon receptor functions as a tumor suppressor of liver carcinogenesis. Cancer Res 2010; 70: 212–220.
Gomez-Duran A, Carvajal-Gonzalez JM, Mulero-Navarro S, Santiago-Josefat B, Puga A, Fernandez-Salguero PM . Fitting a xenobiotic receptor into cell homeostasis: how the dioxin receptor interacts with TGF beta signaling. Biochem Pharmacol 2009; 77: 700–712.
Chang XQ, Fan YX, Karyala S, Schwemberger S, Tomlinson CR, Sartor MA et al. Ligand-independent regulation of transforming growth factor beta 1 expression and cell cycle progression by the aryl hydrocarbon receptor. Mol Cell Biol 2007; 27: 6127–6139.
Elizondo G, Fernandez-Salguero P, Sheikh MS, Kim GY, Fornace AJ, Lee KS et al. Altered cell cycle control at the G(2)/M phases in aryl hydrocarbon receptor-null embryo fibroblast. Mol Pharmacol 2000; 57: 1056–1063.
Carvajal-Gonzalez JM, Roman AC, Cerezo-Guisado MI, Rico-Leo EM, Martin-Partido G, Fernandez-Salguero PM . Loss of dioxin-receptor expression accelerates wound healing in vivo by a mechanism involving TGF beta. J Cell Sci 2009; 122: 1823–1833.
Dohr O, Abel J . Transforming growth factor-beta(1) coregulates mRNA expression of aryl hydrocarbon receptor and cell-cycle-regulating genes in human cancer cell lines. Biochem Biophys Res Commun 1997; 241: 86–91.
Perkins A, Phillips J, Kerkvliet N, Tanguay R, Perdew G, Kolluri S et al. A structural switch between agonist and antagonist bound conformations for a ligand-optimized model of the human aryl hydrocarbon receptor ligand binding domain. Biology 2014; 3: 645–669.
Murray IA, Patterson AD, Perdew GH . Aryl hydrocarbon receptor ligands in cancer: friend and foe. Nat Rev Cancer 2014; 14: 801–814.
Safe S, Lee SO, Jin UH . Role of the aryl hydrocarbon receptor in carcinogenesis and potential as a drug target. Toxicol Sci 2013; 135: 1–16.
Zhang S, Kim K, Jin UH, Pfent C, Cao HJ, Amendt B et al. Aryl hydrocarbon receptor agonists induce microRNA-335 expression and inhibit lung metastasis of estrogen receptor negative breast cancer cells. Mol Cancer Ther 2012; 11: 108–118.
Jin UH, Lee SO, Safe S . Aryl hydrocarbon receptor (AhR)-active pharmaceuticals are selective AhR modulators in MDA-MB-468 and BT474 breast cancer cells. J Pharmacol Exp Ther 2012; 343: 333–341.
Acknowledgements
This work was supported by American Cancer Society (RSG-13-132-01-CDD), the National Institute of Environmental Health Sciences (NIEHS) grant numbers ES016651 and ES019000, The US Army Medical Research and Material Command and The Cell Imaging and Analysis Facility Cores of the Environmental Health Sciences Center, NIEHS grant number P30 ES00210. DCK was supported by a National Research Service Award (1F31CA144571-01) pre-doctoral fellowship from the National Cancer Institute. DCK is currently supported by the Burroughs Wellcome Fund post-doctoral enrichment program. EFO was supported by a pre-doctoral fellowship from the Department of Defense Breast Cancer Research Program (W81XWH-10-1-0160). DCK and EFO were previously supported by NIEHS training grant (T32ES07060). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. We thank Samuel Bradford for excellent flow cytometry assistance, Sammy Khalil, Cathy Duong and Viktor Dikov for laboratory assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Oncogene website
Supplementary information
Rights and permissions
About this article
Cite this article
Koch, D., Jang, H., O'Donnell, E. et al. Anti-androgen flutamide suppresses hepatocellular carcinoma cell proliferation via the aryl hydrocarbon receptor mediated induction of transforming growth factor-β1. Oncogene 34, 6092–6104 (2015). https://doi.org/10.1038/onc.2015.55
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2015.55
- Springer Nature Limited
This article is cited by
-
Role of miR-653 and miR-29c in downregulation of CYP1A2 expression in hepatocellular carcinoma
Pharmacological Reports (2022)
-
Discovery and Mechanistic Characterization of a Select Modulator of AhR-regulated Transcription (SMAhRT) with Anti-cancer Effects
Apoptosis (2021)
-
Design and synthesis of anticancer 1-hydroxynaphthalene-2-carboxanilides with a p53 independent mechanism of action
Scientific Reports (2019)
-
Role of the aryl hydrocarbon receptor in carcinogenesis and potential as an anti-cancer drug target
Archives of Toxicology (2017)