Abstract
The omega-3 polyunsaturated fatty acid docosahexaenoic acid (DHA) has anti-inflammatory and anti-cancer properties. Among pro-inflammatory mediators, tumor necrosis factor α (TNFα) plays a paradoxical role in cancer biology with induction of cancer cell death or survival depending on the cellular context. The objective of the study was to evaluate the role of TNFα in DHA-mediated tumor growth inhibition and colon cancer cell death. The treatment of human colorectal cancer cells, HCT-116 and HCT-8 cells, with DHA triggered apoptosis in autocrine TNFα-dependent manner. We demonstrated that DHA-induced increased content of TNFα mRNA occurred through a post-transcriptional regulation via the down-regulation of microRNA-21 (miR-21) expression. Treatment with DHA led to nuclear accumulation of Foxo3a that bounds to the miR-21 promoter triggering its transcriptional repression. Moreover, inhibition of RIP1 kinase and AMP-activated protein kinase α reduced Foxo3a nuclear-cytoplasmic shuttling and subsequent increase of TNFα expression through a decrease of miR-21 expression in DHA-treated colon cancer cells. Finally, we were able to show in HCT-116 xenograft tumor-bearing nude mice that a DHA-enriched diet induced a decrease of human miR-21 expression and an increase of human TNFα mRNA expression limiting tumor growth in a cancer cell-derived TNFα dependent manner. Altogether, the present work highlights a novel mechanism for anti-cancer action of DHA involving colon cancer cell death mediated through autocrine action of TNFα.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common cancer and the fourth leading cause of cancer death worldwide. The etiology of CRC is linked to hereditary component and to environmental factors (diet, lifestyle and chronic inflammation). The inherited CRC account for about 20% of CRC including hereditary nonpolyposis colorectal cancer and familial adenomatous polyposis.1 Therefore, the vast majority of CRC are sporadic without any identified genetic predispositions. The chronic inflammation observed in ulcerative-colitis and Crohn’s disease increases the risk of CRC evidencing the connection between a pro-inflammatory context and colorectal carcinogenesis.2, 3 Actually a pro-inflammatory context promotes virtually all steps of colon carcinogenesis and patients with CRC present increased content of circulating pro-inflammatory mediators (that is, IL-6, IL-1β, IL-8 and TNFα).4, 5
Epidemiological and clinical studies suggest beneficial effects of anti-inflammatory omega-3 polyunsaturated fatty acid intake on the risk or treatment of CRC.6, 7, 8, 9 In addition, in vitro and in vivo preclinical models evidence anti-proliferative and anti-neoplastic functions of both omega-3 polyunsaturated fatty acids predominantly found in fish oil, eicosapentaenoic acid (C22:5) and docosahexaenoic acid (DHA, C22:6).9 Therefore, fish oil- or individual omega-3 polyunsaturated fatty acids-enriched diets are able to reduce the risk of CRC and to limit tumor growth from colon cancer cells transplanted in mice.10, 11 The anticancer effect of DHA might be a consequence of its ability to regulate the production of pro-inflammatory mediators (that is, TNFα, IL-17 and PGE2) in cancer cells and/or host cells changing the systemic or tumor microenvironment inflammatory status.11, 12, 13, 14, 15
Among pro-inflammatory mediators, TNFα is a paradoxical cytokine in cancer biology mainly detected in tumor infiltrating leukocytes in colitis-associated cancer and sporadic CRC.16, 17 In addition to leukocytes, colon cancer cells are also able to produce TNFα sustaining their own proliferation by autocrine action. Furthermore, neutralization of TNFα in a colitis-associated cancer model reduces tumor formation.17, 18 Although most studies underline a tumor promoting role for TNFα, its function remains elusive, since administration of exogenous TNFα might induce cancer cell death and inhibit tumor growth.19, 20, 21 Moreover, activation of TNFα signaling by malignant cell-derived TNFα production may be sufficient to trigger cancer cell death process.22, 23 Therefore, TNFα-mediated cell fate (cell death or survival) depends on cellular context and is controlled by the formation of different complexes following activation of death receptor TNFα-receptor I (TNFR-I). TNFα-mediated cell death relies on the formation of a cytosolic complex II composed of caspase 8, FADD, RIP1 kinase and the long form of cellular FLICE-like inhibitory protein.24
In the present study, we aimed to evaluate the regulation of TNFα expression by DHA in colon cancer cells and its potential role in DHA-mediated apoptosis. We confirmed that DHA treatment induced inhibition of tumor growth and activation of apoptosis in colon cancer cells. However, surprisingly, we found, that these effects originated from autocrine production of TNFα. Furthermore, we documented the molecular regulation of TNFα synthesis involving the decrease of microRNA-21 (miR-21) expression under the control of Foxo3a nuclear accumulation dictated by RIP1 kinase and AMP-activated protein kinase α (AMPKα).
Results
DHA induces TNFα-mediated cell death in human colon cancer cells
We evaluated the effect of DHA on growth of human colon cancer cells (HCT-116 and HCT-8 cells) using Cyquant assay and compared with ω-9 oleic (OA), ω-6 linoleic (LA) and arachidonic (AA) acids. We found that DHA treatment (50, 75 and 100 μM) for 48 h reduced cancer cell number in a dose-dependent manner while OA, AA acid and LA treatment did not in comparison with the control (CTRL) treatment (Figures 1a and b). In order to determine the cell death rate, we carried out analysis of Annexin V-7AAD staining. Addition of DHA for 48 h at indicated concentrations induced a dose-dependent increase of cell death in both colon cancer cells reaching 40.7% of HCT-116 and 26.1% of HCT-8 cells positive for cell death staining at 100 μM of DHA treatment (Figures 1c and d). Moreover, a treatment with the caspase inhibitor zVAD-FMK abolished DHA-mediated cell death, indicating that DHA at 100 μM for 48 h induced caspase-dependent apoptosis (Supplementary Figures S1A and B). We then evaluated the expression of pro-inflammatory cytokines in DHA-treated colon cancer cells. Expression of TNFα mRNA increased in HCT-116 and HCT-8 cells treated with DHA (50 and 100 μM) for 6 h, whereas, IL-6 and IL-8 expression decreased (Figures 1e and f). We quantified TNFα secretion in colon cancer cell culture medium treated by DHA using ELISA and we found that DHA administration for 14 h induced increase of TNFα in HCT-116 and HCT-8 supernatants (Figure 1g). A Trypan blue exclusion assay revealed that DHA did not trigger cell death at 14 h of treatment (data not shown) highlighting that the increased production of TNFα arrived before cell death. Because TNFα has ambivalent properties,17, 18, 19, 20, 21 we analysed the effect of TNFα neutralization on DHA-mediated cell death. We found that pre-treatment with blocking anti-human TNFα (anti-TNFα) (0.5 μg/ml) reduced the DHA-induced cell death in HCT-116 and HCT-8, while the co-treatment with CTRL IgG and DHA showed cell death level similar than administration of DHA alone (Figures 1h and i). The data here suggest that DHA inhibits cell growth by inducing autocrine TNFα-dependent cell death.
DHA induces TNFα-dependent cell death in colon cancer cells. (a) and (b) Proliferation analysis with Cyquant assay for HCT-116 and HCT-8 treated for 48 h with indicated concentrations of DHA, OA and LA. (c) and (d) Cell death analysis by Annexin V-7AAD staining in HCT-116 and HCT-8 cells treated with DHA for 48 h. (e) and (f) Relative expression of TNFα, IL-6 and IL-8 mRNA in HCT-116 and HCT-8 cells treated with DHA for 6 h. (g) TNFα secretion measured by ELISA in HCT-116 and HCT-8 cells after 14 h of treatment with DHA. (h) and (i) Cell death analysis as (c) and (d) for HCT-116 and HCT-8 co-treated with DHA (100 μM) and blocking anti-TNFα or CTRL IgG (0.5 μg/ml). Data are expressed as the mean±s.d. of three independent experiments and compared with CTRL unless otherwise indicated. *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001.
RIP1 regulates TNFα mRNA expression in colon cancer cells
TNFα-mediated apoptosis involves the processing of pro-caspase-8 to active caspase-8 and depends on RIP1.24 In agreement with a previous study,25 we showed induction of active caspase 8 in DHA-treated cancer cells (Figure 2a). To determine the role of RIP1 in DHA effect, we investigated cell death level in colon cancer cells treated with DHA in RIP1-depleted cells using siRNA (Supplementary Figures S2A and B) or in presence of the RIP1 inhibitor necrostatin-1 (Nec-1). We found that silencing of RIP1 expression in HCT-116 and HCT-8 cells reduced DHA-mediated cell death analysed 48 h post-transfection (Figures 2b and c). Similarly, inhibition of RIP1 kinase activity with Nec-1 treatment attenuated DHA-induced cell death in colon cancer cells (Figures 2d and e). Altogether these results evidenced the role of RIP1 in the pro-cytotoxic effect of DHA. In addition to its downstream action after activation of TNFα signaling, RIP1 is able to induce TNFα expression in a feedforward manner.26 Hence, we analysed the regulation of TNFα expression by RIP1 in HCT-116 cells. Silencing of RIP1 expression and activity abolished DHA-mediated TNFα upregulation in colon cancer cells (Figures 2f and g).
RIP1 regulates TNFα production in colon cancer cells. (a) Caspase-8 activity in HCT-116 treated with DHA for 48 h. (b) and (c) Cell death analysis by Annexin V-7AAD staining of HCT-116 and HCT-8 transfected with siRNA CTRL or RIP1 (siRNA RIP1) and treated with DHA (100 μM) for 48 h. (d) and (e) Cell death analysis as (b) and (c) after co-treatment with Nec-1; 2.5 and 10 μM) and DHA. (f) and (g) Relative expression of TNFα mRNA in DHA-treated HCT-116 cells for 6 h transfected with siRNA CTRL and RIP1 (siRNA RIP1) (f) or treated with Nec-1 (g). Data are expressed as the mean±s.d. of three independent experiments and compared with CTRL unless otherwise indicated. *P<0.05; **P<0.01; ***P<0.001; ns, non-significant.
DHA increases TNFα expression through downregulation of miR-21
Recently, microRNAs appeared as novel regulators of cell functions (for example, proliferation and differentiation) by controlling gene expression through post-transcriptional action.27 Moreover, DHA is able to modify the profile of microRNA expression targeting cell death program in cancer cells.28, 29 Thus, in order to investigate the molecular pathway involved in TNFα-induced cell death in DHA-treated colon cancer cells, we evaluated the role of miR-21, which is a possible regulator of TNFα mRNA content.30 We observed that DHA (50 and 100 μM) repressed the expression of miR-21 in HCT-116 and HCT-8 cells (Figures 3a and b). We provided evidence that DHA might regulate the increase of TNFα mRNA through regulation of miR-21 expression. Indeed, transfection of pre-miR-21 (miR-21 mimic) in colon cancer cells decreased TNFα mRNA expression and abolished the DHA-induced upregulation of TNFα mRNA expression (Figures 3c and d). To validate the fact that DHA upregulated level of TNFα mRNA via miR-21 action, we used 3’-UTR of TNFα containing the miR-21 binding site cloned in a luciferase reporter vector. A significant increase of luciferase activity has been observed in colon cell lines treated with DHA (Figure 3e). Such data suggest that DHA-mediated inhibition of miR-21 expression alleviated post-transcriptional repression exerted on TNFα mRNA. Next, we wondered whether RIP1 participated in the regulation of miR-21 expression in DHA-treated colon cancer cells. We found that downregulation of miR-21 expression was lost in DHA-treated cancer cells lacking RIP1 expression or activity (Figures 3f and g). Furthermore, overexpression of miR-21 mimic counteracted DHA-induced cell death in both colon cancer cell lines (Figures 3h and i).
miR-21 contributes to DHA-mediated regulation of TNFα expression and cell death. (a) and (b) Relative miR-21 expression in DHA-treated HCT-116 and HCT-8 at indicated times. (c) and (d) Relative TNFα mRNA expression in HCT-116 and HCT-8 cells transfected with miR-21 or CTRL mimic and treated with DHA (100 μM) for 6 h. (e) Analysis of 3’-UTR TNFα luciferase activity in HCT-116 and HCT-8 cells normalized to Renilla luciferase activity. Relative 3’-UTR TNFα luciferase activity in DHA-treated cells is compared with CTRL-treated cells. (f) and (g) Analysis of relative miR-21 expression in DHA-treated cancer cells transfected with siRNA CTRL or RIP1 (siRNA RIP1) (f) or treated with Nec-1 (g). (h) and (i) Cell death analysis by Annexin V-7AAD staining of HCT-116 and HCT-8 transfected with miR-21 and CTRL mimic and treated with DHA for 48 h. Data are expressed as the mean±s.d. of three independent experiments and compared with CTRL unless otherwise indicated. *P<0.05; **P<0.01; ***P<0.001; ns, non-significant.
DHA-mediated nuclear translocation of Foxo3a regulates miR-21 and TNFα expression
The transcription factor Foxo3a has been described as a repressor of miR-21 expression through direct binding on miR-21 promoter, which has two Foxo3a response elements (BS1 and BS2).31 Expression of Foxo3a protein in HCT-8 and HCT-116 cells treated for 4 h with DHA was analysed and we observed an increase of Foxo3a expression in HCT-8, while remaining unchanged in HCT-116 (Supplementary Figures S3A and B). Then, we investigated the nuclear-cytoplasmic shuttling in both DHA-treated colon cancer cells. Immunofluorescence analysis evidenced an increase of nuclear translocation of endogenous Foxo3a in DHA-treated HCT-116 and HCT-8 cells using a rabbit polyclonal anti-Foxo3a (Figures 4a and b). Similar results were obtained with a goat polyclonal anti-Foxo3a and with overexpressed Flag-Foxo3a in HCT-116 cells (Supplementary Figures S3C and D). To gain further insight into the control of miR-21 expression by DHA, we analysed the DNA-binding of Foxo3a on miR-21 promoter using the CHIP assay. DHA led to a statistically significant increase of Foxo3a binding on BS1 (2.7 fold) and a trend increase on BS2 (1.3 fold), whereas no amplification after immunoprecipitation with CTRL IgG of BS1 and BS2 was detected (data not shown) (Figure 4c). We then studied the involvement of Foxo3a in the control of miR-21 expression in HCT-116 and HCT-8 cancer cells treated with DHA. For such experiment, we silenced Foxo3a expression using small-interfering RNA against Foxo3a (siRNA Foxo3a; Supplementary Figures S3E and F) and analysed miR-21 expression in CTRL and DHA-treated cells. Colon cancer cells transfected with siRNA CTRL and exposed to DHA had a decreased expression of miR-21 compared with untreated cells and to siRNA Foxo3a-transfected cells which were unable to induce the DHA-mediated downregulation of miR-21 expression (Figure 4d). This result indicates that Foxo3a is essential for repression of miR-21 expression in DHA-treated cancer cells. In the same way, the inhibition of Foxo3a expression with siRNA Foxo3a alleviated the DHA-induced TNFα mRNA expression in HCT-116 and HCT-8 cells (Figure 4e). We next evaluated the role of Foxo3a in cell death induced by DHA with analysis of Annexin V and 7AAD staining in siRNA Foxo3a- and siRNA CTRL-transfected colon cancer cells. The treatment with DHA induced cell death in HCT-116 and HCT-8 transfected with siRNA CTRL, whereas the knockdown of Foxo3a (siRNA Foxo3a) significantly reduced the DHA-mediated cell death (Figures 4f and g).
Foxo3a regulates miR-21 and TNFα expression in DHA-treated cells. (a) and (b) Immunofluorescence with rabbit anti-Foxo3a in HCT-116 and HCT-8 cells treated with DHA for 4 h (scale bar=10 μm). Foxo3a nuclear distribution (%) was determined with Image J software (NIH) as described in Materials and methods. (c) CHIP analysis with anti-Foxo3a to determine binding of Foxo3a on BS1 and BS2 of miR-21 promoter in CTRL- and DHA-treated HCT-116 for 4 h. Foxo3a occupancy in DHA-treated cells is compared with Foxo3a occupancy on BS1 or BS2 in CTRL cells. (d) and (e) Relative expression of miR-21 (d) and TNFα mRNA (e) in HCT-116 and HCT-8 transfected with siRNA CTRL or Foxo3a (siRNA Foxo3a) and treated with DHA (100 μM) for 6 h. (f) and (g) Cell death analysis by Annexin V-7AAD staining of HCT-116 and HCT-8 transfected with siRNA CTRL or Foxo3a and treated with DHA for 48 h. Data are expressed as the mean±s.d. of three independent experiments and compared with CTRL unless otherwise indicated. *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001.
AMPKα controls nuclear localization of Foxo3a and TNFα expression in DHA-treated cancer cells
From the above results, we evidenced that the effect of DHA on miR-21 and TNFα mRNA expression involved RIP1 kinase and Foxo3a. Thereby, we evaluated the ability of DHA to regulate Foxo3a nuclear-cytoplasmic shuttling in a RIP1 kinase activity dependent manner. Subcellular distribution of Foxo3a was analysed in both colon cancer cell lines co-treated with DHA and Nec-1. Although treatment with Nec-1 impaired Foxo3a nuclear localization in DHA-treated HCT-116 cells for 4 h, Foxo3a distribution was not affected in HCT-8 cells demonstrating that RIP1-mediated regulation of Foxo3a nuclear translocation was not a common mechanism in colon cancer cells (Supplementary Figures S4A and B). Since AMP-activated protein kinase α (AMPKα)-Foxo3a axis does exist in stressed cells through phosphorylation of Foxo3a at Ser413 (p-Foxo3a S413) by AMPKα, we determined the p-Foxo3a S413 level in DHA-treated colon cancer cells.32 Administration of DHA increased p-Foxo3a S413 content in HCT-116 and HCT-8 cells in association with increase of AMPKα phosphorylation (p-AMPK T172) analyzed at 4 and 6 h, respectively (Figures 5a and b). In addition, immunofluorescence analysis of Foxo3a subcellular distribution showed that treatment of cells with AMPK activator induced nuclear Foxo3a accumulation (Supplementary Figure S4C). To precise the potential function of AMPKα activation in regulation of Foxo3a localization in DHA-treated cells, we inhibited AMPKα expression with siRNA AMPKα (Supplementary Figure S4D) and AMPK activity with compound C (0.5 μM). The loss of AMPK activity as well as inhibition of AMPKα expression reduced Foxo3a nuclear distribution in HCT-116 and HCT-8 exposed to DHA treatment (Figures 5c and d). Next, we evaluated the role of DHA-mediated AMPKα activation in regulation of miR-21 and TNFα expression. The DHA treatment in HCT-116 cells transfected with siRNA CTRL showed as expected a decrease of miR-21 expression and increase of TNFα mRNA content while abolition of AMPKα expression counteracted the DHA effect on miR-21 and TNFα mRNA (Figures 5e and f). We confirmed using compound C that prevention of DHA-induced AMPKα activation did not trigger the change of miR-21 and TNFα expression (Supplementary Figures S4E and F). Finally, we showed that AMPKα activation pathway is involved in DHA-induced colon cancer cell death. Indeed, we observed that extinction of AMPKα expression and inactivation of AMPKα pathway by compound C reduced cell death in HCT-116 and HCT-8 treated with DHA (Figure 5g, Supplementary Figures S4G and H).
DHA-triggered AMPKα activation regulates Foxo3a nuclear translocation. (a) and (b) Analysis of p-AMPKα (T172), total AMPKα, p-Foxo3a (S413) and total Foxo3a expression by western-blotting in HCT-116 (a) and HCT-8 (b) cells treated with DHA (50, 75 and 100 μM) for 4 or 6 h, respectively. (c) Subcellular distribution of Foxo3a in HCT-116 and HCT-8 treated with AMPK inhibitor (Comp C, 0.25 μM) and treated with DHA (100 μM) for 4 h (scale bar=10 μm). Foxo3a nuclear distribution (%) was determined with Image J software (NIH) as described in Materials and methods. (d) Subcellular distribution of Foxo3a in HCT-116 and HCT-8 transfected with siRNA CTRL or against AMPKα (siRNA AMPK) and treated with DHA (100 μM) for 4 h. Foxo3a nuclear distribution (%) was determined with Image J software (NIH) as described in Materials and methods. (e) and (f) Relative miR-21 (e) and TNFα mRNA (f) expression assessed by RT-qPCR in HCT-116 cells transfected with siRNA CTRL or against AMPKα (siRNA AMPK) followed by DHA treatment for 4 h. (g) Analysis of cell death by Annexin V-7AAD staining in HCT-116 cells transfected with siRNA CTRL or AMPK treated with DHA for 48 h. Data are expressed as the mean±s.d. of three independent experiments and compared with CTRL unless otherwise indicated. *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001.
DHA inhibits HCT-116 xenograft tumor growth through TNFα production
Activity of DHA has been evaluated in nude mice fed either a CTRL or a DHA-enriched diet after HCT-116 tumor xenografts were established. The monitoring of colon tumor growth showed that DHA diet limited the growth of implanted HCT-116 cells into nude mice compared with CTRL diet (Figure 6a). The in vitro studies underlined the contribution of TNFα and miR-21 in the cytotoxic effects of DHA. Therefore, we analysed the expression of TNFα and miR-21 in tumors of mice treated with CTRL or DHA-enriched diet. In order to discriminate between TNFα production from human malignant cells and mouse tumor microenvironment cells, we designed specific primers for analysis of human or mouse TNFα mRNA expression by RT-qPCR. In tumors from nude mice fed DHA diet, we observed an increase of human TNFα mRNA expression and a decrease of human miR-21 expression compared with tumors from mice-fed control diet confirming in vitro data (Figures 6b and c). Moreover, mouse TNFα mRNA content evaluated from tumor microenvironment cells did not significantly change with the DHA-enriched diet in comparison with the control diet, although a decreased trend has been observed (Figure 6d). To test the role of human TNFα produced by HCT-116 in DHA-mediated tumor growth inhibition, we administered neutralizing anti-TNFα or CTRL IgG in tumor-bearing mice fed a DHA diet. The CTRL IgG injection in mice fed DHA-enriched diet reduced tumor growth as well as mice fed DHA-enriched diet, whereas blocking anti-human TNFα administration abolished the anti-tumor action of DHA-enriched diet (Figure 6e). It is noteworthy that anti-TNFα alleviated the anti-tumoral effect of DHA diet as long as anti-TNFα has been daily injected. Altogether these observations clearly demonstrated that DHA exerted anti-cancer activity through colon cancer cell-derived TNFα production.
DHA inhibits HCT-116 xenograft tumor growth through colon cancer cell-derived TNFα production. (a) Monitoring of established HCT-116 xenograft tumor in athymic nude mice fed a CTRL diet (n=8, blue) or DHA-enriched diet (n=9, red). (b), (c) and (d) Relative expression of human TNFα mRNA (b), human miR-21 (c) and mouse TNFα mRNA (d), analyzed by RT-qPCR in HCT-116 xenograft tumor tissues from mice fed a CTRL diet or DHA-enriched diet. (e) Analysis of HCT-116 xenograft tumor growth in athymic nude mice (n=6 per group) fed CTRL diet (blue) or DHA-enriched diet (red) with intra-peritoneal injections (indicated with arrow) of 100 μg CTRL IgG (green) or anti-TNFα antibody (black). Data are expressed as the mean±s.e.m and compared with CTRL unless otherwise indicated. *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001; ns, non-significant.
Discussion
A large body of evidence sustains the fact that inflammation is associated with carcinogenesis and cancer progression, especially in colorectal cancer.2, 3, 4, 5, 33 However, the contribution of TNFα to the physiopathology of the disease remains unclear and conflicting. Indeed, TNFα is a multifunctional cytokine acting on immune cells, vasculature and cancer cells and is a major mediator of inflammation with pro- and anti-tumor properties. Literature reports an increase of circulating TNFα in colitis-associated cancer and the global neutralization of TNFα reduces colon tumor formation in the chronic inflammatory mouse model.17 However, TNFα production by tumor-associated myeloid cells activated with polyI:C or local TNFα administration suppress tumor growth.34, 35 We showed here that DHA-induced TNFα production and secretion by malignant cells that might generate both an unfavorable tumor microenvironment affecting infiltrated cell properties and triggering the autocrine TNFα production-mediated colon cancer cell death (Figures 1h and i and Figure 6e). Functional TNFα signaling in HCT-116 and HCT-8 colon cancer cells allowed a cytotoxic action through cancer cell-derived TNFα production that might be amplified by increased expression of TNFR-I previously described in DHA-treated colon cancer cells.21, 25, 36, 37 Therefore, a role of RIP1 in DHA-mediated cell death through autocrine TNFα action was not surprising. However, we found that the increase of TNFα mRNA content in DHA-treated colon cancer cells occurred via RIP1 activation suggesting a feedforward loop. A transcriptional regulation of TNFα in a RIP1 dependent manner but independent of the canonical NF-κB pathway has been demonstrated in cancer cells treated with a compound isolated from fungus (neoalbaconol) or with a pan-caspase inhibitor both activating necroptosis.38, 39 In our study, we evidenced that DHA treatment induced caspase-dependent apoptosis instead of necroptosis since zVAD-FMK addition prevented DHA-mediated cell death (Supplementary Figures S1A and B). DHA treatment triggered caspase 8 activation, which induced apoptosis commitment and likely blocked necroptosis through cleavage of key substrates involved in the necroptosis program.24, 40, 41 Moreover, we were interested in the role of peroxisome proliferator-activated receptors (PPARs) in DHA-mediated apoptosis. PPARs exist under three isoforms (PPARγ, PPARα and PPARβ/δ), which are DHA-activated nuclear receptors42 and their expression could be controlled by DHA.43, 44 In A549 lung and MCF-7 breast cancer cells, the inactivation of PPARγ counteracted the pro-apoptotic program induced by DHA.45, 46 Nevertheless, we confirmed a previous study evidencing that PPARγ is not involved in DHA-mediated colon cancer cell death.25 Similarly, PPARα and PPARβ/δ did not seem to be involved in pro-apoptotic effect of DHA in colon cancer cells (Supplementary Figure S5). Therefore, DHA-induced apoptosis in colon cancer cells would be independent of PPARs.
The anti-proliferative effect of DHA is not a common feature of unsaturated fatty acids. Indeed, OA belonging to ω-9 family or LA and AA belonging to ω-6 family did not exert any anti-proliferative action in colon cancer cells in the present study. It is noteworthy that previous studies already reported the effects of ω-3 and ω-6 polyunsaturated fatty acids (PUFA) on proliferation of cancer cells. They observed anti-proliferative action of fatty acids of both families on the colon, breast, lung and prostate cancer cells, which would depend on cell types and concentration of fatty acids.47, 48, 49, 50, 51 Studies on regulation of CRC by dietary fats showed that ω-3 and ω-6 PUFA-enriched diets exerted different action on tumor growth. Indeed, ω-6 PUFA-enriched diet promoted colon cancer development, whereas OA or DHA reduced colon cancer growth.52
The opposite effect of ω-3 and ω-6 PUFA on CRC would involve a different regulation of inflammatory status. PUFA of ω-3 family, especially DHA, have anti-inflammatory properties associated with anti-cancer action.11, 12, 53 Here, we found that administration of DHA on colon cancer cells led to a decreased expression of inflammatory cytokines (IL-6 and IL-8). However, the induction of TNFα expression highlighted a discrepancy in the regulation of the inflammatory status in DHA-treated colon cancer cells. Indeed, we found that regulation of TNFα bypassed the DHA-activated anti-inflammatory program through a post-transcriptional regulation dependent on miR-21 expression (Figures 1e and f and Figures 2f and g).
Such microRNA binds to the 3'-untranslated region of the target mRNA and triggers a repression of translation or degradation of the mRNA.27 Zhang X. et al.30 showed that the oncomiR miR-21 targets TNFα mRNA limiting the production of TNFα protein and promoting transformation of genotoxic-damaged cells underlying a pro-tumoral action of miR-21 and a subsequent loss of anti-tumoral action of TNFα. Thereby, aberrant increase in expression of miR-21 has been found in CRC tissues from two different cohorts and a positive association between expression of miR-21 and pro-inflammatory cytokines (IL-6 and IL-8) has been observed.54 Unlike IL-6 and IL-8, TNFα expression has been shown to be decreased in CRC tissues from the same cohorts, while miR-21 expression increased without significant negative association with TNFα expression.54 Although consistent data reported increase expression of miR-21, it is noteworthy that there are inconsistent results for TNFα expression in CRC tissues since increase of TNFα expression has also been reported.17, 55 Therefore, miR-21 appears as a good candidate target for anticancer action and the essential role of miR-21 in colon cancer cell proliferation has been already described with miR-21 inhibitor reducing xenograft tumor growth what we were able to mimic in athymic nude mice bearing tumors fed a DHA-enriched diet.56
Although NF-κB plays a central role in the transcriptional activation of pro-inflammatory program and miR-21 expression, we focused our study on Foxo3a-dependent regulation of miR-21 expression.57 We observed that DHA treatment led to Foxo3a nuclear translocation allowing transcriptional repression of miR-21 expression (Figures 4a and d). The suppression of Foxo3a expression with siRNA abolished the DHA-mediated down-regulation of miR-21 expression confirming a previous study that described the negative regulation of miR-21 promoter activity with increased binding of Foxo3a on its response elements in doxorubicin-treated lung cancer cells.31 However, we were not able to show that an enforced Foxo3a-TM (a mutated nuclear-targeted Foxo3a) expression regulated miR-21 expression in HCT-116 (Supplementary Figure S6A) suggesting that DHA would coordinate different pathways in order to repress miR-21 expression. The transcriptional function of Foxo3a depends on its nuclear translocation and activation controlled by kinases inducing phosphorylation on different residues.58 Since we showed that RIP1 is involved in miR-21 regulation by DHA and that Foxo3a participated to such regulation, we postulated that RIP1 could control the Foxo3a nuclear translocation. Although RIP1 partially contributed to the regulation of Foxo3a nuclear translocation in HCT-116, a RIP1-dependent mechanism was not observed in HCT-8 (Supplementary Figures S4A and B). Instead, we found that AMPKα is activated by DHA treatment and induced AMPKα-dependent Foxo3a nuclear translocation, which contributes to inhibition of miR-21 transcription and increase of TNFα mRNA expression. The role of AMPKα in Foxo3a regulation has been first described as a transcriptional regulation activity through phosphorylation on Ser413 of Foxo3a under nutrient deprivation without affecting subcellular distribution.32 However, recent data confirmed our observation that AMPKα controls Foxo3a subcellular localization. Indeed, Chou et al.59 showed that AMPKα activation by OSU53 induced Foxo3a nuclear distribution and suggested that this event depended on AKT regulation. The literature reported that DHA inhibits AKT signaling by regulation of its phosphorylation status and by change of its subcellular localization.60, 61 Therefore, Foxo3a nuclear translocation dependent on DHA-activated AMPKα might be through regulation of AKT and the regulation of the transcriptional activity through a direct action of AMPKα on Foxo3a. Activation of the AMPKα pathway in DHA-treated cells might originate from reactive oxygen species (ROS) overproduction as already described.62, 63 We analysed generation of ROS with chloromethyl 2′,7′-dichlorodihydrofluorescein diacetate (CM-H2DCFDA) and dihydroethidium at early time points and did not found ROS overproduction in DHA-treated cells (Supplementary Figures S7A and D) excluding a role of ROS in activation of AMPKα triggering production of TNFα through Foxo3a and miR-21 regulation. Although ROS overproduction were not detected in cells exposed to DHA for 30 min to 5 h, we observed lipid peroxide accumulation at 3 h of treatment (Supplementary Figure S7E). DHA has a great number of double bonds that would increase its susceptibility to endogenous peroxidation64 probably via ROS generated by basal metabolism of cancer cells. Lipid peroxidation has been observed in cancer cells treated by DHA50 and could result from anti-oxidant response alteration such as inhibition of phospholipid hydroperoxide glutathione peroxidase (GPX4),65 which has been shown to trigger lipid peroxidation before ROS detection.66 We showed that abolition of lipid peroxidation with α-tocopherol in DHA-treated cells did not prevent either AMPKα activation or increase of TNFα expression (Supplementary Figures S7F and G) indicating that activation of AMPKα pathway leading to TNFα induction was independent of lipid peroxide generation. Further investigations are needed to determine the mechanism that initiates activation of AMPKα pathway in DHA-treated colon cancer cells.
In summary, our work describes for the first time a regulation of Foxo3a-miR-21 signaling pathway by RIP1 and AMPKα controlling the production of TNFα in DHA-treated colon cancer cells leading to apoptosis and inhibition of tumor growth.
Materials and methods
Cell culture conditions
Human colorectal carcinoma HCT-116 and HCT-8 cells were obtained from the American Type Culture Collection and maintained in DMEM or RPMI supplemented with 6% and 10% heat inactivated fetal bovine serum, respectively. Cell lines were authenticated by examination of morphology and growth characteristics and confirmed to be mycoplasma free. Cells were treated with fatty acids bound to fatty acid free-bovine serum albumin (ratio 4:1) (BSA, Sigma-Aldrich, Lyon, France). Docosahexaenoic acid (DHA, C22:6 n-3), OA (C18:1 n-9), LA (C18:2 n-6) and AA (C20:4 n-6)were purchased from Sigma-Aldrich (USA). Nec-1 and compound C (Comp C) applied at 10 μM and 0.5 μM respectively were from Sigma-Aldrich (USA).
Cell proliferation assay
Cell proliferation analysis was carried out using CyQuant NF cell proliferation assay (Invitrogen, Courtaboeuf, France) as previously described.67
Cell death analysis
Cell death was determined by APC-Annexin V and 7-amino-actinomycin D (7AAD) staining with BioLegend's APC-Annexin V Apoptosis Detection Kit and analysed by flow cytometry (FACSCalibur, Becton Dickinson, Villebon sur Yvette, France). Cells with APC-AnnexinV+-7AAD− staining were considered as cells in early-stage apoptosis whereas cells with Annexin V+-7AAD+ or Annexin V−-7AAD+ staining were identified as cells in late-stage apoptosis or necrosis.
Caspase 8 activity
Colon cancer cells treated for 48 h with indicated concentrations of DHA were collected and analysed with FAM-FLICA Caspase 8 Assay Kit (Immunochemistry Technologies, Courtaboeuf, France).
siRNA and pre-miR transfection
Cells were transfected with siRNA against human Foxo3a (siRNA Foxo3a), human RIP1 (siRNA RIP1), human AMPKα (siRNA AMPK) and negative control siRNA (siRNA CTRL) purchased from Ambion (Life Technologies, Villebon sur Yvette, France) and Santa Cruz Biotechnology (Heidelberg, Germany) using Oligofectamine (Invitrogen). Human pre-miR-21 (miR-21 mimic) and pre-miR control (CTRL mimic) obtained from Ambion (Life Technologies) were transfected using Oligofectamine (Invitrogen). Treatment with fatty acid was performed 24 h post-transfection.
RNA purification and RT-qPCR
Total RNA was extracted with Trizol (Invitrogen) and reverse transcribed with M-MLV reverse transcriptase (Invitrogen) for analysis of mRNA expression or with TaqMan MicroRNA Reverse Transcription Kit (Invitrogen) for analysis of microRNA expression. Real-time RT-qPCR was performed with iQSYBR Green supermix (Bio-Rad, Marnes-la-Coquette, France) for mRNA expression analysis and TaqMan Universal PCR Master Mix II for microRNA expression analysis using a StepOnePlus Real-Time PCR System (Applied Biosystems, Villebon sur Yvette, France). The sequence of primers is indicated in Supplementary Table S1. Expression was normalized to β-actin for mRNA or RNU48 for microRNA. Relative expression of RNA targets was determined using the comparative ΔΔCt method.
Immunoblotting analysis
Immunoblotting was carried out as previously described.67 In brief, total protein extracts were resolved by SDS-PAGE and analysed by western-blotting with the following antibodies: anti-Foxo3a (H-144) from Santa Cruz Biotechnologies, anti-RIP1 from BD Biosciences (Villebon sur Yvette, France), anti-β-actin from Sigma-Aldrich, anti-phospho-AMPKα (Thr172), anti-AMPKα, anti-phospho-Foxo3a (Ser413), HRP-conjugated anti-mouse and anti-rabbit from Cell Signaling Technology (Saint Quentin Yvelines, France).
Chromatin immunoprecipitation (ChIP) analysis
Cells were fixed with 1% formaldehyde at room temperature for 10 min and quenched with 0.125 M glycine. Chromatin was isolated and sonicated into chromatin fragments with an average length of 100–500 bp. DNA was immunoprecipitated with anti-Foxo3a (Santa Cruz Biotechnology). After chromatin elution, crosslinking was reversed and PCR was performed to amplify Foxo3a binding sites (BS1 and BS2) of the human miR-21 promoter. PCR amplification with inputs was used for normalization. Data were expressed in fold change occupancy for DHA treatment relative to CTRL treatment. Primers are listed in Supplementary Table S1.
Dual-luciferase reporter assay
Cells were transfected with the 3’-UTR sequence of TNFα into psiCheck luciferase vector (generously provided by Dr Wang) and with Renilla luciferase vector using Lipofectamine 2000 (Invitrogen) and treated 24 h post-transfection with DHA for 6 h. Cells were harvested and luciferase activities were analysed with the Dual Glo Luciferase Reporter Assay kit (Promega, Charbonnières-les-Bains, France) using a Perkin Elmer Victor 3 Model 1420 Multi-label Microplate Reader.
Immunofluorescence staining
The cells were fixed with 4% paraformaldehyde solution for 10 min at 4 °C. Samples were incubated overnight at 4 °C with rabbit polyclonal anti-Foxo3a (H-144) followed with incubation with Alexa568-coupled anti-rabbit antibody. Cell nuclei were stained with DAPI (Duo82040, Sigma-Aldrich). Microscopy images were taken on an Axio Imager 2 (Carl Zeiss Microscopy GmbH, Jena, Germany) equipped with an Apotome.2 module (Carl Zeiss GmbH). Images were acquired using an AxioCam MRm monochrome CCD camera (Carl Zeiss GmbH) with filter sets 43 HE (Rhodamine/Alexa568) and 49 (DAPI). Quantitative Foxo3a nuclear staining was analysed with Image J software (NIH, Bethesda, MD, USA). Image masks were created for Foxo3a and DAPI positive staining to determine regions of interest (ROI). Nuclear ROI was defined by DAPI staining mask. With the image calculator, we quantified Foxo3a immunofluorescence intensity in nuclear ROI and obtained a percentage of nuclear Foxo3a staining over total cellular Foxo3a staining in a cell. Unless otherwise specified, three independent experiments were used to calculate the mean % of nuclear Foxo3a staining with at least 100 cells per experiment.
TNFα secretion analysis
Cell culture supernatants of colon cancer cells treated for 14 h with indicated concentrations of DHA were collected and analysed with Human TNF-α ELISA MAX Standard kit (Biolegend, Saint Quentin Yvelines, France) according to the manufacturer's protocol.
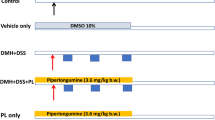
Xenograft tumor growth experiments
Mice were bred and maintained according to both the Federation of Laboratory Animal Science Associations and the Animal Experimental Ethics Committee Guidelines (University of Burgundy, Dijon, France). In order to induce tumor formation, 106 HCT-116 colon cancer cells were subcutaneously injected into male athymic nude mice (Charles River Laboratories, Saint-Germain sur l'Abresle, France). Once tumors were measurable, tumor-bearing mice were randomly assigned to either a group of mice fed a control diet containing sunflower oil or a group of mice fed a DHA-enriched diet containing Omegavie DHA90 TG (Polaris Nutritional Lipids).12 The tumor volume was calculated as follows: larger diameter × (smaller diameter)2/2. Human TNFα neutralization was achieved by daily intraperitoneal injection of 100 μg of CTRL IgG or anti-human TNFα (#1825; R&D systems, Lille, France) from day 0 to 5 after assignment of mice to CTRL or DHA-enriched diet group and then every two days.
Statistical analysis
Statistical analysis was conducted using GraphPad Prism software (GraphPad Software, Inc., CA, USA). Results were presented as mean±s.d. As applicable, Student’s t-test or the Mann–Whitney U-test were used for pairwise comparisons whereas one-way ANOVA was used to compare multiple groups.
References
Jasperson KW, Tuohy TM, Neklason DW, Burt RW . Hereditary and familial colon cancer. Gastroenterology 2010; 138: 2044–2058.
Beaugerie L, Itzkowitz SH . Cancers complicating inflammatory bowel disease. N Engl J Med 2015; 372: 1441–1452.
Brenner H, Kloor M, Pox CP . Colorectal cancer. Lancet 2014; 383: 1490–1502.
Krzystek-Korpacka M, Diakowska D, Kapturkiewicz B, Bebenek M, Gamian A . Profiles of circulating inflammatory cytokines in colorectal cancer (CRC), high cancer risk conditions, and health are distinct. Possible implications for CRC screening and surveillance. Cancer Lett 2013; 337: 107–114.
Maihofner C, Charalambous MP, Bhambra U, Lightfoot T, Geisslinger G, Gooderham NJ . Expression of cyclooxygenase-2 parallels expression of interleukin-1beta, interleukin-6 and NF-kappaB in human colorectal cancer. Carcinogenesis 2003; 24: 665–671.
Anti M, Marra G, Armelao F, Bartoli GM, Ficarelli R, Percesepe A et al. Effect of omega-3 fatty acids on rectal mucosal cell proliferation in subjects at risk for colon cancer. Gastroenterology 1992; 103: 883–891.
Bartoli GM, Palozza P, Marra G, Armelao F, Franceschelli P, Luberto C et al. n-3 PUFA and alpha-tocopherol control of tumor cell proliferation. Mol Aspects Med 1993; 14: 247–252.
Anti M, Armelao F, Marra G, Percesepe A, Bartoli GM, Palozza P et al. Effects of different doses of fish oil on rectal cell proliferation in patients with sporadic colonic adenomas. Gastroenterology 1994; 107: 1709–1718.
Cockbain AJ, Toogood GJ, Hull MA . Omega-3 polyunsaturated fatty acids for the treatment and prevention of colorectal cancer. Gut 2012; 61: 135–149.
Bathen TF, Holmgren K, Lundemo AG, Hjelstuen MH, Krokan HE, Gribbestad IS et al. Omega-3 fatty acids suppress growth of SW620 human colon cancer xenografts in nude mice. Anticancer Res 2008; 28: 3717–3723.
Calviello G, Di Nicuolo F, Gragnoli S, Piccioni E, Serini S, Maggiano N et al. n-3 PUFAs reduce VEGF expression in human colon cancer cells modulating the COX-2/PGE2 induced ERK-1 and -2 and HIF-1alpha induction pathway. Carcinogenesis 2004; 25: 2303–2310.
Berger H, Vegran F, Chikh M, Gilardi F, Ladoire S, Bugaut H et al. SOCS3 transactivation by PPARgamma prevents IL-17-driven cancer growth. Cancer Res 2013; 73: 3578–3590.
Gravaghi C, La Perle KM, Ogrodwski P, Kang JX, Quimby F, Lipkin M et al. Cox-2 expression, PGE(2) and cytokines production are inhibited by endogenously synthesized n-3 PUFAs in inflamed colon of fat-1 mice. J Nutr Biochem 2011; 22: 360–365.
Liang B, Wang S, Ye YJ, Yang XD, Wang YL, Qu J et al. Impact of postoperative omega-3 fatty acid-supplemented parenteral nutrition on clinical outcomes and immunomodulations in colorectal cancer patients. World J Gastroenterol 2008; 14: 2434–2439.
Yao L, Han C, Song K, Zhang J, Lim K, Wu T . Omega-3 Polyunsaturated Fatty Acids Upregulate 15-PGDH Expression in Cholangiocarcinoma Cells by Inhibiting miR-26a/b Expression. Cancer Res 2015; 75: 1388–1398.
Naylor MS, Stamp GW, Balkwill FR . Investigation of cytokine gene expression in human colorectal cancer. Cancer Res 1990; 50: 4436–4440.
Popivanova BK, Kitamura K, Wu Y, Kondo T, Kagaya T, Kaneko S et al. Blocking TNF-alpha in mice reduces colorectal carcinogenesis associated with chronic colitis. J Clin Invest 2008; 118: 560–570.
Zins K, Abraham D, Sioud M, Aharinejad S . Colon cancer cell-derived tumor necrosis factor-alpha mediates the tumor growth-promoting response in macrophages by up-regulating the colony-stimulating factor-1 pathway. Cancer Res 2007; 67: 1038–1045.
Balkwill FR, Lee A, Aldam G, Moodie E, Thomas JA, Tavernier J et al. Human tumor xenografts treated with recombinant human tumor necrosis factor alone or in combination with interferons. Cancer Res 1986; 46: 3990–3993.
Kreeger PK, Mandhana R, Alford SK, Haigis KM, Lauffenburger DA . RAS mutations affect tumor necrosis factor-induced apoptosis in colon carcinoma cells via ERK-modulatory negative and positive feedback circuits along with non-ERK pathway effects. Cancer Res 2009; 69: 8191–8199.
Wang P, Qiu W, Dudgeon C, Liu H, Huang C, Zambetti GP et al. PUMA is directly activated by NF-kappaB and contributes to TNF-alpha-induced apoptosis. Cell Death Differ 2009; 16: 1192–1202.
Cianchi F, Papucci L, Schiavone N, Lulli M, Magnelli L, Vinci MC et al. Cannabinoid receptor activation induces apoptosis through tumor necrosis factor alpha-mediated ceramide de novo synthesis in colon cancer cells. Clin Cancer Res 2008; 14: 7691–7700.
Petersen SL, Wang L, Yalcin-Chin A, Li L, Peyton M, Minna J et al. Autocrine TNFalpha signaling renders human cancer cells susceptible to Smac-mimetic-induced apoptosis. Cancer Cell 2007; 12: 445–456.
Ofengeim D, Yuan J . Regulation of RIP1 kinase signalling at the crossroads of inflammation and cell death. Nat Rev Mol Cell Biol 2013; 14: 727–736.
Giros A, Grzybowski M, Sohn VR, Pons E, Fernandez-Morales J, Xicola RM et al. Regulation of colorectal cancer cell apoptosis by the n-3 polyunsaturated fatty acids Docosahexaenoic and Eicosapentaenoic. Cancer Prev Res (Phila) 2009; 2: 732–742.
Biton S, Ashkenazi A . NEMO and RIP1 control cell fate in response to extensive DNA damage via TNF-alpha feedforward signaling. Cell 2011; 145: 92–103.
van Kouwenhove M, Kedde M, Agami R . MicroRNA regulation by RNA-binding proteins and its implications for cancer. Nat Rev Cancer 2011; 11: 644–656.
Farago N, Feher LZ, Kitajka K, Das UN, Puskas LG . MicroRNA profile of polyunsaturated fatty acid treated glioma cells reveal apoptosis-specific expression changes. Lipids Health Dis 2011; 10: 173.
Gil-Zamorano J, Martin R, Daimiel L, Richardson K, Giordano E, Nicod N et al. Docosahexaenoic acid modulates the enterocyte Caco-2 cell expression of microRNAs involved in lipid metabolism. J Nutr 2014; 144: 575–585.
Zhang X, Ng WL, Wang P, Tian L, Werner E, Wang H et al. MicroRNA-21 modulates the levels of reactive oxygen species by targeting SOD3 and TNFalpha. Cancer Res 2012; 72: 4707–4713.
Wang K, Li PF . Foxo3a regulates apoptosis by negatively targeting miR-21. J Biol Chem 2010; 285: 16958–16966.
Greer EL, Oskoui PR, Banko MR, Maniar JM, Gygi MP, Gygi SP et al. The energy sensor AMP-activated protein kinase directly regulates the mammalian FOXO3 transcription factor. J Biol Chem 2007; 282: 30107–30119.
Chung H, Lee YS, Mayoral R, Oh DY, Siu JT, Webster NJ et al. Omega-3 fatty acids reduce obesity-induced tumor progression independent of GPR120 in a mouse model of postmenopausal breast cancer. Oncogene 2014; 34: 3504–3513.
Al-Zoubi M, Salem AF, Martinez-Outschoorn UE, Whitaker-Menezes D, Lamb R, Hulit J et al. Creating a tumor-resistant microenvironment: cell-mediated delivery of TNFalpha completely prevents breast cancer tumor formation in vivo. Cell Cycle 2013; 12: 480–490.
Shime H, Matsumoto M, Oshiumi H, Tanaka S, Nakane A, Iwakura Y et al. Toll-like receptor 3 signaling converts tumor-supporting myeloid cells to tumoricidal effectors. Proc Natl Acad Sci USA 2012; 109: 2066–2071.
Bansal T, Alaniz RC, Wood TK, Jayaraman A . The bacterial signal indole increases epithelial-cell tight-junction resistance and attenuates indicators of inflammation. Proc Natl Acad Sci USA 2010; 107: 228–233.
Verbeke H, De Hertogh G, Li S, Vandercappellen J, Noppen S, Schutyser E et al. Expression of angiostatic platelet factor-4var/CXCL4L1 counterbalances angiogenic impulses of vascular endothelial growth factor, interleukin-8/CXCL8, and stromal cell-derived factor 1/CXCL12 in esophageal and colorectal cancer. Human Pathol 2010; 41: 990–1001.
Christofferson DE, Li Y, Hitomi J, Zhou W, Upperman C, Zhu H et al. A novel role for RIP1 kinase in mediating TNFalpha production. Cell Death Dis 2012; 3: e320.
Yu X, Deng Q, Li W, Xiao L, Luo X, Liu X et al. Neoalbaconol induces cell death through necroptosis by regulating RIPK-dependent autocrine TNFalpha and ROS production. Oncotarget 2015; 6: 1995–2008.
O'Donnell MA, Perez-Jimenez E, Oberst A, Ng A, Massoumi R, Xavier R et al. Caspase 8 inhibits programmed necrosis by processing CYLD. Nat Cell Biol 2011; 13: 1437–1442.
Shalini S, Dorstyn L, Dawar S, Kumar S . Old, new and emerging functions of caspases. Cell Death Differ 2015; 22: 526–539.
Varga T, Czimmerer Z, Nagy L . PPARs are a unique set of fatty acid regulated transcription factors controlling both lipid metabolism and inflammation. Biochim Biophys Acta 2011; 1812: 1007–1022.
Calviello G, Resci F, Serini S, Piccioni E, Toesca A, Boninsegna A et al. Docosahexaenoic acid induces proteasome-dependent degradation of beta-catenin, down-regulation of survivin and apoptosis in human colorectal cancer cells not expressing COX-2. Carcinogenesis 2007; 28: 1202–1209.
Yu H, Liu Y, Pan W, Shen S, Das UN . Polyunsaturated fatty acids augment tumoricidal action of 5-fluorouracil on gastric cancer cells by their action on vascular endothelial growth factor, tumor necrosis factor-alpha and lipid metabolism related factors. Arch Med Sci 2015; 11: 282–291.
Martinasso G, Oraldi M, Trombetta A, Maggiora M, Bertetto O, Canuto RA et al. Involvement of PPARs in cell proliferation and apoptosis in human colon cancer specimens and in normal and cancer cell lines. PPAR Res 2007; 2007: 93416.
Sun H, Berquin IM, Owens RT, O'Flaherty JT, Edwards IJ . Peroxisome proliferator-activated receptor gamma-mediated up-regulation of syndecan-1 by n-3 fatty acids promotes apoptosis of human breast cancer cells. Cancer Res 2008; 68: 2912–2919.
Begin ME, Das UN, Ells G, Horrobin DF . Selective killing of human cancer cells by polyunsaturated fatty acids. Prostaglandins Leukot Med 1985; 19: 177–186.
Begin ME, Ells G, Das UN, Horrobin DF . Differential killing of human carcinoma cells supplemented with n-3 and n-6 polyunsaturated fatty acids. J Natl Cancer Inst 1986; 77: 1053–1062.
Béguin ME, Das UN, Ells G . Cytotoxic effects of essential fatty acids (EFA) in mixed cultures of normal and malignant human cells. Prog Lipid Res 1986; 25: 573–576.
Das UN . Tumoricidal action of cis-unsaturated fatty acids and their relationship to free radicals and lipid peroxidation. Cancer Lett 1991; 56: 235–243.
Monjazeb AM, High KP, Connoy A, Hart LS, Koumenis C, Chilton FH . Arachidonic acid-induced gene expression in colon cancer cells. Carcinogenesis 2006; 27: 1950–1960.
Bartoli R, Fernandez-Banares F, Navarro E, Castella E, Mane J, Alvarez M et al. Effect of olive oil on early and late events of colon carcinogenesis in rats: modulation of arachidonic acid metabolism and local prostaglandin E(2) synthesis. Gut 2000; 46: 191–199.
Zou Z, Bellenger S, Massey KA, Nicolaou A, Geissler A, Bidu C et al. Inhibition of the HER2 pathway by n-3 polyunsaturated fatty acids prevents breast cancer in fat-1 transgenic mice. J Lipid Res 2013; 54: 3453–3463.
Schetter AJ, Nguyen GH, Bowman ED, Mathe EA, Yuen ST, Hawkes JE et al. Association of inflammation-related and microRNA gene expression with cancer-specific mortality of colon adenocarcinoma. Clin Cancer Res 2009; 15: 5878–5887.
Gattolliat CH, Uguen A, Pesson M, Trillet K, Simon B, Doucet L et al. MicroRNA and targeted mRNA expression profiling analysis in human colorectal adenomas and adenocarcinomas. Eur J Cancer 2015; 51: 409–420.
Iliopoulos D, Jaeger SA, Hirsch HA, Bulyk ML, Struhl K . STAT3 activation of miR-21 and miR-181b-1 via PTEN and CYLD are part of the epigenetic switch linking inflammation to cancer. Mol Cell 2010; 39: 493–506.
Zhou R, Hu G, Gong AY, Chen XM . Binding of NF-kappaB p65 subunit to the promoter elements is involved in LPS-induced transactivation of miRNA genes in human biliary epithelial cells. Nucleic Acids Res 2010; 38: 3222–3232.
Chiacchiera F, Simone C . The AMPK-FoxO3A axis as a target for cancer treatment. Cell Cycle 2010; 9: 1091–1096.
Chou CC, Lee KH, Lai IL, Wang D, Mo X, Kulp SK et al. AMPK reverses the mesenchymal phenotype of cancer cells by targeting the Akt-MDM2-Foxo3a signaling axis. Cancer Res 2014; 74: 4783–4795.
Gu Z, Wu J, Wang S, Suburu J, Chen H, Thomas MJ et al. Polyunsaturated fatty acids affect the localization and signaling of PIP3/AKT in prostate cancer cells. Carcinogenesis 2013; 34: 1968–1975.
Chen Z, Zhang Y, Jia C, Wang Y, Lai P, Zhou X et al. mTORC1/2 targeted by n-3 polyunsaturated fatty acids in the prevention of mammary tumorigenesis and tumor progression. Oncogene 2014; 33: 4548–4557.
Cardaci S, Filomeni G, Ciriolo MR . Redox implications of AMPK-mediated signal transduction beyond energetic clues. J Cell Sci 2012; 125: 2115–2125.
Jung SN, Yang WK, Kim J, Kim HS, Kim EJ, Yun H et al. Reactive oxygen species stabilize hypoxia-inducible factor-1 alpha protein and stimulate transcriptional activity via AMP-activated protein kinase in DU145 human prostate cancer cells. Carcinogenesis 2008; 29: 713–721.
Else PL, Kraffe E . Docosahexaenoic and arachidonic acid peroxidation: It's a within molecule cascade. Biochim Biophys Acta 2015; 1848: 417–421.
Ding WQ, Lind SE . Phospholipid hydroperoxide glutathione peroxidase plays a role in protecting cancer cells from docosahexaenoic acid-induced cytotoxicity. Mol Cancer Ther 2007; 6: 1467–1474.
Seiler A, Schneider M, Forster H, Roth S, Wirth EK, Culmsee C et al. Glutathione peroxidase 4 senses and translates oxidative stress into 12/15-lipoxygenase dependent- and AIF-mediated cell death. Cell Metab 2008; 8: 237–248.
Pierre AS, Minville-Walz M, Fevre C, Hichami A, Gresti J, Pichon L et al. Trans-10, cis-12 conjugated linoleic acid induced cell death in human colon cancer cells through reactive oxygen species-mediated ER stress. Biochim Biophys Acta 2013; 1831: 759–768.
Acknowledgements
The authors would like to thank the lipidomic plateform and the flow cytometry plateform facilities of Université de Bourgogne. The present work was supported by Ligue contre le cancer comité Grand-Est and by a French Government grant managed by the French National Research Agency under the program 'Investissements d’Avenir' with reference ANR-11-LABX-0021 (Lipstic Labex).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Oncogene website
Supplementary information
Rights and permissions
About this article
Cite this article
Fluckiger, A., Dumont, A., Derangère, V. et al. Inhibition of colon cancer growth by docosahexaenoic acid involves autocrine production of TNFα. Oncogene 35, 4611–4622 (2016). https://doi.org/10.1038/onc.2015.523
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2015.523
- Springer Nature Limited
This article is cited by
-
TNFα-induced IDH1 hyperacetylation reprograms redox homeostasis and promotes the chemotherapeutic sensitivity
Oncogene (2023)
-
Krill oil extract inhibits the migration of human colorectal cancer cells and down-regulates EGFR signalling and PD-L1 expression
BMC Complementary Medicine and Therapies (2020)
-
Krill oil extract suppresses the proliferation of colorectal cancer cells through activation of caspase 3/9
Nutrition & Metabolism (2019)
-
The forkhead-box family of transcription factors: key molecular players in colorectal cancer pathogenesis
Molecular Cancer (2019)
-
Docosahexaenoic acid inhibits both NLRP3 inflammasome assembly and JNK-mediated mature IL-1β secretion in 5-fluorouracil-treated MDSC: implication in cancer treatment
Cell Death & Disease (2019)