Abstract
Several drugs have recently been reported to induce rapid antidepressant effects in clinical trials and rodent models. Although the cellular mechanisms involved remain unclear, reports suggest that increased glutamate transmission contributes to these effects. Here, we demonstrate that the antidepressant-like efficacy of three unique drugs, with reported rapid onset antidepressant properties, is coupled with a rapid transient rise in glutamate cycling in the medial prefronal cortex (mPFC) of awake rats as measured by ex vivo 1H-[13C]-nuclear magnetic resonance spectroscopy. Rats were acutely pretreated by intraperitoneal injection with a single dose of ketamine (1, 3, 10, 30 and 80 mg kg−1), Ro 25-6981 (1, 3 and 10 mg kg−1), scopolamine (5, 25 and 100 μg kg−1) or vehicle (controls). At fixed times after drug injection, animals received an intravenous infusion of [1,6-13C2]glucose for 8 min to enrich the amino-acid pools of the brain with 13C, followed by rapid euthanasia. The mPFC was dissected, extracted with ethanol and metabolite 13C enrichments were measured. We found a clear dose-dependent effect of ketamine and Ro 25-6981 on behavior and the percentage of 13C enrichment of glutamate, glutamine and GABA (γ-aminobutyric acid). Further, we also found an effect of scopolamine on both cycling and behavior. These studies demonstrate that three pharmacologically distinct classes of drugs, clinically related through their reported rapid antidepressant actions, share the common ability to rapidly stimulate glutamate cycling at doses pertinent for their antidepressant-like efficacy. We conclude that increased cycling precedes the antidepressant action at behaviorally effective doses and suggest that the rapid change in cycling could be used to predict efficacy of novel agents or identify doses with antidepressant activity.
Similar content being viewed by others
Introduction
A growing number of studies are now reporting that a novel class of antidepressant drugs is capable of inducing a rapid antidepressant response in patients with previously treatment-resistant mood disorders.1 The strongest evidence of this rapid-acting antidepressant (RAAD) effect has been established for ketamine, a non-selective N-methyl-d-aspartate receptor (NMDAR) antagonist.2 However, RAAD effects were also reported for other NMDAR targeting drugs, such as lanicemine, the low trapping non-subunit-selective NMDA receptor channel blocker,3 and CP-101 606,4 an NR2B-selective receptor antagonist. In addition, there is now evidence suggesting that the anticholinergic drug scopolamine (Scop) also possesses RAAD-like effects.5
Other findings suggest that a transient activation of AMPA receptors is a necessary event in the generation of the RAAD effects induced by NMDAR antagonists and Scop in rodent models.6, 7, 8, 9 In light of earlier work showing ketamine’s ability to rapidly increase glutamate efflux in the frontal cortex of the rat,10 possibly due to effects on inhibitory GABAergic interneurons,11 it has been hypothesized that this brief ketamine-induced surge in glutamate release is a critical event for the RAAD activity. However, the question remains whether this surge in glutamate release is a mechanism common to other drugs with RAAD-like properties, and whether the increase in glutamate release is related to the more durable antidepressant-like behavioral effects of these RAAD drugs.
Having previously found that subanesthetic doses of ketamine led to rapid increases in glutamate, GABA (γ-aminobutyric acid) and glutamine cycling,12 and considering previous reports of inverted-U-type dose–response relationships between ketamine-induced effects on glutamate efflux,10 as well as antidepressant-like behavioral responses and cellular changes in rats,6 we first sought to confirm and extend the dose–response relationship between RAAD properties of ketamine and glutamate cycling. We next sought to determine the time dependence of ketamine’s effect on glutamate/GABA-glutamine cycling in the medial prefrontal cortex (mPFC) of rats. Last, to determine whether the increase in glutamate cycling is generalizable to drugs of other classes with RAAD properties, we investigated the effects of Ro 25-6981, an NR2B-selective NMDAR antagonist, and Scop, a muscarinic receptor M1 antagonist13 that has been shown to require AMPA activation to produce the antidepressant-like effects in rodents,9 on both cycling and behavior.
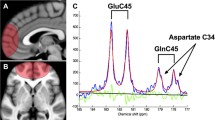
1H-[13C]-nuclear magnetic resonance (NMR) spectroscopy was used to examine the effects of the drugs on glutamate release in the mPFC of rats and recycling into glia (glutamate cycling), and neuronal and glial energy metabolism. 13C-labeled glucose is metabolized mainly in the neuronal TCA cycle and labels neuronal glutamate and GABA, which are released and taken up by astrocytes, followed by conversion to (and labeling of) glutamine, suggesting that 13C-labeled glucose studies provide information on glutamate and GABA neurotransmitter cycling as well as neuronal (mainly) and glial (partly) cell metabolism, reflecting the neurotransmitter activity12, 14, 15 (see Supplementary Figure S1). As several studies have specifically demonstrated increased rates of mPFC metabolism in rodents following treatment with subanesthetic doses of ketamine,16, 17, 18, 19 and similar regions are believed to mediate several of ketamine’s behavioral effects,20, 21, 22 all studies were performed in rat mPFC.
Materials and methods
Animals
Male Sprague–Dawley rats (Charles River, Raleigh, NC, USA) weighing 180–220 g were group-housed and maintained under standard conditions of constant temperature (25 °C) and humidity with a 12-h light/dark cycle, with ad libitum access to food and water. All experiments were conducted in accordance with the National Institutes of Health guidelines and the protocols approved by the Yale University Animal Care and Use Committee.
Plasma ketamine measures
Separate groups of male rats (170–200 g at delivery; n=4 per group) were dosed intraperitoneally with ketamine (1, 3, 10, 30 and 80 mg kg−1) and plasma samples were collected at time points corresponding to the mid-point of glucose utilization determinations in the study. Plasma aliquots (50 μl) were treated with acetonitrile (200 μl) followed by vortex mixing for 2 min. The supernatant was then separated from the precipitated proteins by centrifugation (10 min at 1479 g), and 150 μl was transferred to a 96-well plate. An aliquot of supernatant (5 μl) was injected onto the ultra-high-performance liquid chromatography column for liquid chromatography/mass spectrometry/mass spectrometry-based analysis.
NMR experiments
Dose–response studies of ketamine, Ro 25-6981 and Scop
Rats (6–8 per group) were treated with different doses of ketamine reported to have antidepressant behavioral efficacy as well as lower and higher doses (1, 3, 10, 30 and 80 mg kg−1),6, 8 diluted in either saline (0.9%) or vehicle (vehicle) 10 min before the beginning of [1,6-13C2]glucose infusion. Ro 25-6981 (supplied by BMS) dissolved in vehicle was tested at doses of 1, 3 and 10 mg kg−1 intraperitoneally, based on previous reports of behavioral efficacy,6, 23, 24 alongside the ketamine studies at 1, 30 and 80 mg kg−1. Effects of all treatments were compared with unique control groups receiving intraperitoneal infusions of saline as described previously12 (for the ketamine 3 and 10 mg) and vehicle (for ketamine 1, 30 and 80 mg kg−1 and Ro 25-6981 1, 3 and 10 mg kg−1) as Ro 25-6981 was not soluble in saline. The vehicle consisted of 5% dimethyl sulfoxide (DMSO, Sigma, St Louis, MO, USA)/10% propylene glycol/0.0375% methylcellulose/70% water. Scop (Sigma) 25 μg kg−1 was studied based on behavioral findings and previous reports of behavioral efficacy.9 All drugs were administered intraperitoneally in volumes of 2 ml kg−1, with the exception of the highest ketamine dose (80 mg kg−1), which was 3 ml kg−1.
Time dependence of single-dose ketamine effects
Rats (six rats per time point) received a single injection of ketamine (30 mg kg−1, intraperitoneally) at 0, 10, 30 or 60 min before [1,6-13C2]glucose infusion. The 30 mg kg−1 dose of ketamine was chosen because it had the largest metabolic effect in the dose–response study. The effects of a single injection of ketamine (10 mg kg−1, intraperitoneally) at 24 h was also measured to match the dosing previously shown to have significant effects on dendritic spine density at 24 h.6, 25
[1,6-13C2]glucose infusions
Tail vein catheters were placed under brief isoflurane anesthesia and animals were allowed to recover for at least 30 min before drug/vehicle injections. Ten minutes after injection of ketamine, 7 min after injection of Scop and 30 min after injection of Ro 25-6981 or vehicle (times determined by the Cmax and onset of observable behavioral changes with each compound), a solution of [1,6-13C2]glucose (99 atom%; Cambridge Isotopes, Andover, MA, USA) dissolved in water (0.75 mol l−1 per 200 g body weight) was infused for 8 min as described previously.12 Immediately following the 8 min infusion of [1,6-13C2]glucose, the rats were quickly killed using focused-beam microwave irradiation as described in the Supplementary Material.
Tissue extraction and NMR sample preparation
Metabolites in the mPFC were extracted from frozen tissue (65–85 mg) as described by Chowdhury et al.12 (see Supplementary Material). Brain and plasma samples were loaded into 5 mm tubes for NMR analysis.
NMR spectroscopy analysis of 13C incorporation
Total concentrations and 13C enrichments of mPFC amino acids and metabolites and plasma glucose were determined from fully relaxed 1H-[13C]-NMR spectra acquired at 11.7 T (1H frequency of 500.13 MHz; Bruker AVANCE; Bruker Instruments, Billerica, MA, USA) as described in the Supplementary Material.
Behavioral tests
Drug administration for behavioral tests
Animals received a single intraperitoneal injection of vehicle (saline and/or DMSO); ketamine at 3, 30 and 80 mg kg−1; Ro 25-6981 at 3 and 10 mg kg−1; or Scop at 5, 25 and 100 μg kg−1, 24 h after the first day of swimming. Ketamine and Scop were dissolved with saline (0.9%). Ro 25-6981 was dissolved in a solution mixed with saline: DMSO (v:v=5.6:1). Animals for each drug treatment were tested for behavior using assays at different time points.
Forced swim test
Antidepressant effects of ketamine, Ro 25-6981 and Scop were assessed using the forced swim test (FST). Each rat was placed in the plexiglass cylinder (65 cm in height and 30 cm in diameter) filled with 24–25 °C water to a depth of 45 cm for 15 min on day 1 and 10 min on day 3. On day 3 and 24 h after the drug injections, animals were recorded from the side with a video camcorder. Time immobile was scored, separating two blocks of 5 min for analysis. Immobility was defined as minimum movement to stay afloat.
Stereotypy
Effects of ketamine, Ro 25-6981 and Scop on stereotypic behaviors were assessed immediately after the injection on day 2. Animals were placed in a new cage and videotaped from the side. Orofacial and aspecific stereotypy was scored by bins of 1 min every 5 min (i.e. minutes 5–6 and 10–11). Occurrence of each stereotypic behavior and not their frequency for each minute bin was scored. The stereotypy counts for each animal represent the sum of stereotypic occurrence for the five bins. Orofacial stereotypy included mouth movement, bite, self-gnaw, jaw tremor and aspecific head stereotypy including head bob, head sway and taffy pull.
Statistical analysis
The statistical significance of differences in concentrations and 13C enrichments between control and ketamine, Ro 25-6981 or Scop in treated rats were assessed using analysis of variance (ANOVA) followed by Dunnett's multiple comparisons procedure where each treatment is compared with a single control group. Overall, ANOVA effects were considered significant at P<0.05 and post hoc tests significant at Padj⩽0.05 using Dunnett’s test. FST immobility times were separated into two bins (first 5 min and last 5 min), and were analyzed using linear models with treatment assignment included as a between-subjects factor and time as a within-subjects factor. The group by time interaction was modeled. Stereotypic behavioral outcomes were analyzed using one-way ANOVA followed by Dunnett’s test.
Results
Plasma levels for all doses of ketamine at each time point examined are shown in Supplementary Table 1. Glucose concentrations were similar in plasma samples from all groups (ranging from mean±s.e.m.; 15.1±1.0 to 17.8±0.5 mmol l−1, n=6–8 per group). Similar results were found for the percent 13C enrichments: ranging from mean±s.e.m.; 45.7±1.5 to 49.4±2.4%). In addition, total levels of amino acids and metabolites were determined in the different groups by averaging the respective [1,6-13C2]glucose infusion data; total mPFC concentrations of the metabolites examined were similar in all animal groups (see Supplementary Tables S1 and S2). These results indicate that changes in mPFC levels of the 13C-labeled amino acids found in this study are not related to general metabolic alterations or changes in total amino-acid concentrations.
Dose–response effects of ketamine and Ro 25-6981 on rat mPFC glutamate/GABA-glutamine cycling
Figures 1a and c illustrate the dose–response relationships between the percent 13C enrichment of treatment relative to controls for ketamine and Ro 25-6981, respectively. Lower doses of ketamine and Ro 25-6981 (1 mg kg−1 each) had no effect on 13C-labeled incorporation into glutamate-C4 (F(2,21)=0.53, P=0.60), GABA-C2 (F(2,21)=0.35, P=0.71) or glutamine-C4 (F(2,21)=1.78, P=0.19) (Supplementary Figure S2A). At the mid-dose, there was a significant main effect of treatment on both glutamate-C4 (F(2,20)=3.5, P<0.05) and glutamine-C4 13C enrichment (F(2,20)=15.0, P<0.0001) (Supplementary Figure S2B). Specifically, ketamine at 30 mg kg−1 increased glutamate-C4 enrichment by 9% above vehicle (Padj<0.05), and increased glutamine-C4 enrichment by 38% above vehicle (Padj<0.0001). There was a trend suggesting that the mid-doses altered GABA-C2 enrichment (F(2,20)=2.68, P=0.09), with the 30 mg kg−1 dose of ketamine increasing enrichment by 22% (Padj=0.06). R0 25-6981 at 3 mg kg−1 did not show any effect on 13C enrichment of any of the amino acids (Padj>0.6, for all). There was a significant main effect of treatment on the 13C enrichment of all three amino acids, glutamate-C4 (F(2,23)=3.92, P<0.05), GABA-C2 (F(2,23)=8.16, P<0.01) and glutamine-C4 enrichment (F(2,23)=3.56, P<0.05) at the highest dose of the drugs tested (Supplementary Figure S2C). Here it was Ro 25-6981 10 mg kg−1 that significantly increased 13C enrichment (Padj<0.05) of all three amino acids, whereas the higher anesthetic dose of ketamine (80 mg kg−1) showed no effect on the enrichment (Padj⩾0.3, for all).
Effects of ketamine and Ro 25-6981 on medial prefronal cortex (mPFC) glutamate/γ-aminobutyric acid (GABA)-glutamine metabolism and forced swim test (FST) behavior. (a) Percent change in PFC glutamate-C4, GABA-C2 and glutamine-C4 fractional enrichments over an interval from 10 to 18 min after intraperitoneal doses of 1, 3, 10, 30 and 80 mg kg−1 compared with vehicle-injected animals. (b) Ketamine 30 mg kg−1 decreased average time immobile in the FST but not 3 and 10 mg kg−1. The effect was more pronounced in the last 5 min of the test. (c) Percent change in PFC glutamate-C4, GABA-C2 and glutamine-C4 enrichments over an interval from 30 to 38 min after intraperitoneal doses of 1, 3 and 10 mg kg−1 Ro 25-6981 relative to vehicle-treated controls. (d) Averaged over the two blocks of 5 min, the Ro 25-6981 10 mg kg−1 animal group shows a trend for decreased time immobile with a more pronounced effect for the last 5 min (#Punadj=0.05; PBonferroni=0.1). Interrogation time is the 8-min interval after ketamine injection during which the 13C-glucose was infused (means+/-s.e.m.) (#P<0.1; *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001).
Two additional studies examining intermediate ketamine doses of 3 (Supplementary Figure S2D) and 10 mg kg−1 (Supplementary Figure S2E) demonstrated effects of treatment on the 13C enrichment of glutamate-C4 (P<0.01 for both), GABA-C2 (P<0.05 for both) and glutamine-C4 (P<0.05 and P<0.01, respectively) compared with their respective saline control.
Dose–response effects of ketamine and Ro 25-6981 on behavior
We were further able to align the changes in cycling with the RAAD effects of ketamine by demonstrating that the measured antidepressant-like performances in the FST 24 h after the ketamine administration mirrors the dose-dependent effects on cycling (Figure 1b). A significant overall ketamine effect was observed (F(3,25)=5.08, P<0.01) owing to decreased average time immobile in the FST at 30 mg kg−1 (Padj=0.002) but not 3 and 80 mg kg−1 (all Padj>0.14). There was a significant interaction between group and time ((F3,25)=5.37, P<0.01) where the observed ketamine 30 mg kg−1 effects were more pronounced during the last 5 min (PBonferroni<0.001).
An ANOVA analysis of the effects of Ro 25-6981 in the FST test revealed a significant group effect (F(2,42)=5.02, P<0.05). Averaged over the two blocks of 5 min, Ro 25-6981 at 10 mg kg−1 animal group showed a trend difference from control (Punadj=0.04; Padj=0.08), with a more pronounced effect for the last 5 min (Punadj=0.05; PBonferroni=0.1) (Figure 1d).
Time dependence of ketamine effect on glutamate/GABA-glutamine cycling in rat mPFC and behavior
To examine the duration of ketamine’s effects on cycling, we chose to examine the effects of a single 30 mg kg−1 intraperitoneal injection of ketamine, the dose showing the largest magnitude of effect in the dose–response study above. Ketamine injection led to an elevation in glutamine-C4 13C enrichment over the 8-min interval from 0.5 to 8.5 min (P<0.05), 10 to 18 min (P<0.001) and 30 to 38 min (NS, P=0.17) compared with vehicle-injected rats, but not the 60 to 68 min (P=0.81) time point (Figure 2a). 13C labeling of glutamate-C4 (P<0.01) and GABA-C2 (P<0.05) was significantly increased only at the 10 to 18 min time point (see Supplementary Figure 3 for individual 13C fractional enrichments). Thus, this postinjection period of increased 13C labeling of mPFC amino acids was transient, with a peak rise occurring in <30 min and disappearing within 1 h.
Effects of time after ketamine injection on glutamate, γ-aminobutyric acid (GABA) and glutamine 13C labeling compared with control animals. (a) The figure depicts the percent change in fractional enrichment compared with vehicle-injected animals over time. Amino-acid labeling reflects the interval from 0.5 to 8.5 min, 10 to 18 min, 30 to 38 min and 60 to 68 min after intraperitoneal injection of ketamine 30 mg kg−1. (b) There was no significant effect of a single 10 mg kg−1 intraperitoneal dose of ketamine on glutamate, GABA and glutamine 13C labeling from 13C-glucose when interrogated for 8 min at 24 h (#P<0.1; *P<0.05; **P<0.01; ***P<0.001).
There was no significant effect of a single 10 mg kg−1 intraperitoneal dose of ketamine (dose most frequently shown to have delayed behavioral effects in tests of antidepressant action) at 24 h on glutamate-C4, GABA-C2 and glutamine-C4 13C labeling from 13C-glucose (Figure 2b and Supplementary figure 4 for individual fractional enrichments).
Scop effects on rat mPFC glutamate/GABA-glutamine behavior and cycling
We first examined the antidepressant-like effects of Scop in the FST using three doses. Scop decreased average time immobile in the FST at 25 μg kg−1 but not 5 and 100 μg kg−1. There was a significant interaction between drug and time (F(3,48)=4.03, P<0.05), with a more pronounced effect with Scop 25 μg kg−1 during the last 5 min (Punadj=0.007; PBonferroni =0.04) (Figure 3a).
Effects of Scopolamine (Scop) on forced swim test (FST) immobility and glutamate, γ-aminobutyric acid (GABA) and glutamine 13C labeling compared with control animals. (a) Scop decreased average time immobile in the FST at 25 μg kg−1 but not 5 and 100 μg kg−1. Averaged over the two blocks of 5 min, there was a significant interaction between drug and time (F3,48=4.03, P<0.05), with a more pronounced effect with Scop 25 μg kg−1 for the last 5 min (*PBonferroni <0.05) when compared with the vehicle-injected animal group. (b) Effects of a single 25 μg kg−1 intraperitoneal dose of Scop on magnitude change of glutamate, GABA and glutamine 13C labeling from glucose over control (*P<0.05 when compared with vehicle-injected animal group).
A single 25 μg kg−1 intraperitoneal dose of Scop increased 13C enrichment of glutamate-C4, GABA-C2 and glutamine-C4 over control from 13C-glucose for all three amino acids (P<0.05 for all) (Figure 3b and see Supplementary Figure 5 for individual fractional enrichments).
Effect of ketamine, Ro 25-6981 and Scop on orofacial and aspecific head stereotypy
The effect of rapid-acting antidepressant drugs on orofacial and head stereotypy is described in Supplementary Figure S6. Ketamine increased stereotypy counts within 30 min after injection; the effect was significant at the dose of 30 mg kg−1 (Padj<0.05) when compared with the vehicle-injected group. It is important to note that animals receiving ketamine at 80 mg kg−1 were practically asleep 20 min after the injection; however, they showed occurrence of more diverse stereotypic behaviors during the first few bins. In contrast, Ro 25-6981 injections had no effect on stereotypy, whereas Scop's slight numeric increase in stereotypic behaviors at the dose of 25 μg kg−1 was not significant.
Discussion
To the best of our knowledge, this study provides the first experimental evidence directly suggesting that a transient surge in amino-acid neurotransmitter cycling is associated with the induction of RAAD-like effects. The study found evidence of inverted U-shaped dose–response relationship between ketamine and amino-acid neurotransmitter cycling. We also found similar evidence of an inverted U-shaped dose–response relationship between ketamine and immobility on the FST. These findings are generally similar to previously established dose–response relationships for ketamine-induced effects on glutamate efflux,10 ketamine-associated antidepressant-like behavioral responses and a variety of accompanying cellular changes in rats.6 The plasma levels obtained at the 14 min time point for 10 mg kg−1 ketamine dose are consistent with the levels reported in Li et al.6 for the same intraperitoneal dose adjusted for time, and are in the similar range of the peak concentrations seen in the human studies dosing at 0.5 mg kg−1 (typically around 100–200 ng ml−1 at the 40 min time point, see Shaffer et al26). However, the 30 mg kg−1 dose of ketamine, which induces clear increases in labeling and antidepressant-like effects in the rats, produces plasma levels that are well above that typically seen with doses used in the treatment of mood disorders, and more in line with anesthetic doses as reported by Domino et al.27 In spite of this, the 30 mg kg−1 dose did not produce hypnotic effects in the rats, indicating that there are species-specific dose effects related to the hypnotic and anesthetic properties of ketamine. Interpretation of the plasma level results at the lower dose range are limited by the variability of the individual measures, making it difficult to show meaningful differences in the plasma levels between the 1 and 3 mg kg−1 doses. Taken together, these studies provide evidence that the subanesthetic doses of ketamine are associated with rapid increases in amino-acid neurotransmitter cycling and antidepressant-like effects on the FST, whereas higher anesthetic doses fail to have the same effects on either measure.
We further examined the relationship between glutamate cycling and antidepressant-like behavior by also analyzing the effects of an NR2B-selective NMDA receptor antagonist, Ro 25-6981. Although the dose range with Ro 25-6981 was truncated by the limited solubility of the drug, there was a dose-dependent increase in cycling and, to a lesser extent, behavior in the FST. Only the highest dose of Ro 25-6981 (10 mg kg−1) induced significant increases in glutamate-C4, GABA-C2 and glutamine-C4 13C enrichment and immobility on the FST over vehicle-treated animals. The dose effect of Ro 25-6981 in the FST was similar to that previously reported in mice,23 with the largest behavioral response being seen at the highest dose, 10 mg kg−1. These studies demonstrate that both ketamine and Ro 25-6981 can dose-dependently induce changes in amino-acid neurotransmitter cycling, and suggest that NMDAR antagonist-induced increases in mPFC glutamate release and cycling are critical events in generating the antidepressant-like response of the drugs.
The studies also revealed the effect of the treatment on amino-acid neurotransmitter cycling to be transient. Consistent with the dose–response studies, the effect of ketamine (30 mg kg−1) on cycling was highly significant over the first 18 min after drug injection. Glutamine enrichment is increased within the first 8 min, and the effect is maintained for at least 18 min after injection. However, the effect dissipates over the course of 1 h, and no differences in cycling was found at 24 h, a time point when the antidepressant-like activity of ketamine was seen and repeatedly documented in rodent models.6, 7, 25, 28 These findings are consistent with other reports demonstrating rapid changes in phencyclidine-induced effects on glutamine levels,29 and metabolism30 in rodents that normalize or even reverse by 24 h, and a report suggesting that glutamine levels are rapidly but transiently increased in healthy control subjects receiving a subanesthetic dose of ketamine.31 The fact that no effects on cycling were observed an hour after the administration of 30 mg kg−1 ketamine, despite having blood levels consistent with that found 14 min after 10 mg kg−1 dose that did increase cycling, suggest the existence of a hysteresis-like effect. In sum, the findings suggest that although a transient effect on glutamate cycling is associated with initiation of the antidepressant response, maintenance of the effect is not required for the delayed antidepressant-like effects of the treatments.
Another recent study found that Scop increases glutamate efflux, and induces synaptogenesis through AMPA receptor activation in rodent models,9 suggesting that the surge in glutamate release is also involved in the drugs mechanism of RAAD action. Consistent with that report, we found the 25 μg kg−1 dose to produce an antidepressant-like effect and demonstrated that the same dose of Scop increased glutamate cycling rates. These results support the hypothesis that the rapid transient induction of cycling is common to drugs with RAAD properties.
Although the highest stereotypy counts were seen at the doses of ketamine and Scop that were associated with the greatest antidepressant-like effects, this effect was not seen with Ro 25-6981. This suggests that the neuronal mechanisms underlying the onset of stereotypy, behaviors considered related to the psychotomimetic effects of NMDAR antagonists,32 are not necessarily the same as those underlying the antidepressant-like action.
There are several factors that limit the interpretation of the findings presented in this manuscript. Measures of 13C enrichment are not direct measures of glutamate release. However, the fact that the results align so closely with previous reports of glutamate efflux suggest that the method is reflecting changes in amino-acid release. Moreover, it was not possible to examine the effects of higher doses of Ro 25-6981 because of its limited solubility, precluding the determination of a full dose–response curve for this compound. We also did not examine the time-dependent effects of Ro 25-6981 and Scop, limiting conclusions on the duration of their effects on glutamate cycling. Last, although the temporal and dose–response relationships between the increase in amino-acid neurotransmitter cycling and the cellular6 and electrophysiological33 effects of NMDAR antagonists suggest the rapid increase in cycling is a critical step in the initiation of the antidepressant response, the study does not provide direct mechanistic evidence for this relationship.
Conclusion
In sum, these findings are consistent with the hypothesis that a transient glutamate surge is critical in initiating RAAD action. This work defines a timeline of signaling events whereby RAAD drugs initially stimulate a rapid increase in synaptic glutamate release and cycling, but suggests that the effects on amino-acid cycling is not required for the maintenance of the antidepressant-like effects. Rather, the enduring effects of these agents could be related to the sustained effects on synapse number and function that is dependent on glutamate signaling.34 The novel use of 13C-NMR spectroscopy outlined in the present study can be relatively easily translated to human studies and may be helpful in future attempts to optimize dosing for treatment response in clinical populations.
References
Martinowich K, Jimenez DV, Zarate CA Jr, Manji HK . Rapid antidepressant effects: moving right along. Mol Psychiatry 2013; 18: 856–863.
Newport DJ, Carpenter LL, McDonald WM, Potash JB, Tohen M, Nemeroff CB et al. Ketamine and other NMDA antagonists: early clinical trials and possible mechanisms in depression. Am J Psychiatry 2015; 172: 950–966.
Sanacora G, Smith MA, Pathak S, Su HL, Boeijinga PH, McCarthy DJ et al. Lanicemine: a low-trapping NMDA channel blocker produces sustained antidepressant efficacy with minimal psychotomimetic adverse effects. Mol Psychiatry 2014; 9: 978–985.
Preskorn SH, Baker B, Kolluri S, Menniti FS, Krams M, Landen JW . An innovative design to establish proof of concept of the antidepressant effects of the NR2B subunit selective N-methyl-d-aspartate antagonist, CP-101,606, in patients with treatment-refractory major depressive disorder. J Clin Psychopharmacol 2008; 28: 631–637.
Drevets WC, Zarate CA Jr, Furey ML . Antidepressant effects of the muscarinic cholinergic receptor antagonist scopolamine: a review. Biol psychiatry 2013; 73: 1156–1163.
Li N, Lee B, Liu RJ, Banasr M, Dwyer JM, Iwata M et al. mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science 2010; 329: 959–964.
Autry AE, Adachi M, Nosyreva E, Na ES, Los MF, Cheng PF et al. NMDA receptor blockade at rest triggers rapid behavioural antidepressant responses. Nature 2011; 475: 91–95.
Koike H, Iijima M, Chaki S . Involvement of AMPA receptor in both the rapid and sustained antidepressant-like effects of ketamine in animal models of depression. Behav Brain Res 2011; 224: 107–111.
Voleti B, Navarria A, Liu RJ, Banasr M, Li N, Terwilliger R et al. Scopolamine rapidly increases mammalian target of rapamycin complex 1 signaling, synaptogenesis, and antidepressant behavioral responses. Biol Psychiatry 2013; 74: 742–749.
Moghaddam B, Adams B, Verma A, Daly D . Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci 1997; 17: 2921–2927.
Homayoun H, Moghaddam B . NMDA receptor hypofunction produces opposite effects on prefrontal cortex interneurons and pyramidal neurons. J Neurosci 2007; 27: 11496–11500.
Chowdhury GM, Behar KL, Cho W, Thomas MA, Rothman DL, Sanacora G . (1)H-[(1)(3)C]-nuclear magnetic resonance spectroscopy measures of ketamine's effect on amino acid neurotransmitter metabolism. Biol Psychiatry 2012; 71: 1022–1025.
Witkin JM, Overshiner C, Li X, Catlow JT, Wishart GN, Schober DA et al. M1 and m2 muscarinic receptor subtypes regulate antidepressant-like effects of the rapidly acting antidepressant scopolamine. J Pharmacol Exp Ther 2014; 351: 448–456.
Chowdhury GM, Patel AB, Mason GF, Rothman DL, Behar KL . Glutamatergic and GABAergic neurotransmitter cycling and energy metabolism in rat cerebral cortex during postnatal development. J Cereb Blood Flow Metab 2007; 27: 1895–1907.
Hyder F, Patel AB, Gjedde A, Rothman DL, Behar KL, Shulman RG . Neuronal–glial glucose oxidation and glutamatergic–GABAergic function. J Cereb Blood Flow Metab 2006; 26: 865–877.
Breier A, Malhotra AK, Pinals DA, Weisenfeld NI, Pickar D . Association of ketamine-induced psychosis with focal activation of the prefrontal cortex in healthy volunteers. Am J Psychiatry 1997; 154: 805–811.
Nishizawa N, Nakao S, Nagata A, Hirose T, Masuzawa M, Shingu K . The effect of ketamine isomers on both mice behavioral responses and c-Fos expression in the posterior cingulate and retrosplenial cortices. Brain Res 2000; 857: 188–192.
Littlewood CL, Jones N, O'Neill MJ, Mitchell SN, Tricklebank M, Williams SC . Mapping the central effects of ketamine in the rat using pharmacological MRI. Psychopharmacology 2006; 186: 64–81.
Stone JM, Erlandsson K, Arstad E, Squassante L, Teneggi V, Bressan RA et al. Relationship between ketamine-induced psychotic symptoms and NMDA receptor occupancy: a [(123)I]CNS-1261 SPET study. Psychopharmacology 2008; 197: 401–408.
Miyamoto S, Leipzig JN, Lieberman JA, Duncan GE . Effects of ketamine, MK-801, and amphetamine on regional brain 2-deoxyglucose uptake in freely moving mice. Neuropsychopharmacology 2000; 22: 400–412.
Miyamoto S, Mailman RB, Lieberman JA, Duncan GE . Blunted brain metabolic response to ketamine in mice lacking D(1 A) dopamine receptors. Brain Res 2001; 894: 167–180.
Duncan GE, Moy SS, Knapp DJ, Mueller RA, Breese GR . Metabolic mapping of the rat brain after subanesthetic doses of ketamine: potential relevance to schizophrenia. Brain Res 1998; 787: 181–190.
Maeng S, Zarate CA Jr, Du J, Schloesser RJ, McCammon J, Chen G et al. Cellular mechanisms underlying the antidepressant effects of ketamine: role of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptors. Biol Psychiatry 2008; 63: 349–352.
Haller J, Nagy R, Toth M, Pelczer KG, Mikics E . NR2B subunit-specific NMDA antagonist Ro25-6981 inhibits the expression of conditioned fear: a comparison with the NMDA antagonist MK-801 and fluoxetine. Behav Pharmacol 2011; 22: 113–121.
Li N, Liu RJ, Dwyer JM, Banasr M, Lee B, Son H et al. Glutamate N-methyl-d-aspartate receptor antagonists rapidly reverse behavioral and synaptic deficits caused by chronic stress exposure. Biol Psychiatry 2011; 69: 754–761.
Shaffer CL, Osgood SM, Smith DL, Liu J, Trapa PE . Enhancing ketamine translational pharmacology via receptor occupancy normalization. Neuropharmacology 2014; 86: 174–180.
Domino EF, Zsigmond EK, Domino LE, Domino KE, Kothary SP, Domino SE . Plasma levels of ketamine and two of its metabolites in surgical patients using a gas chromatographic mass fragmentographic assay. Anesth Analg 1982; 61: 87–92.
Lucki I . The forced swimming test as a model for core and component behavioral effects of antidepressant drugs. Behav Pharmacol 1997; 8: 523–532.
Iltis I, Koski DM, Eberly LE, Nelson CD, Deelchand DK, Valette J et al. Neurochemical changes in the rat prefrontal cortex following acute phencyclidine treatment: an in vivo localized (1)H MRS study. NMR Biomed 2009; 22: 737–744.
Gao XM, Shirakawa O, Du F, Tamminga CA . Delayed regional metabolic actions of phencyclidine. Eur J Pharmacol 1993; 241: 7–15.
Rowland LM, Bustillo JR, Mullins PG, Jung RE, Lenroot R, Landgraf E et al. Effects of ketamine on anterior cingulate glutamate metabolism in healthy humans: a 4-T proton MRS study. Am J Psychiatry 2005; 162: 394–396.
Homayoun H, Jackson ME, Moghaddam B . Activation of metabotropic glutamate 2/3 receptors reverses the effects of NMDA receptor hypofunction on prefrontal cortex unit activity in awake rats. J Neurophysiol 2005; 93: 1989–2001.
Nagy D, Stoiljkovic M, Menniti FS, Hajos M . Differential effects of an NR2B NAM and ketamine on synaptic potentiation and gamma synchrony: relevance to rapid-onset antidepressant efficacy. Neuropsychopharmacology 2015; e-pub ahead of print 21 October 2015.
Duman RS, Aghajanian GK . Synaptic dysfunction in depression: potential therapeutic targets. Science 2012; 338: 68–72.
Acknowledgements
We thank Amy Newton and Yulia Benitex of Bristol-Myers Squibb for the execution of the rat ketamine PK studies, and Terry Nixon, Peter Brown and Scott McIntyre for their support in maintaining the NMR spectrometer. This work was supported by National Institute of Mental Health R01-MH095104 and R01-MH081211, NARSAD, QNMR Core Center P30-NS052519, The VA National Center for PTSD and funding from Bristol-Myers Squib.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
Dr Sanacora has received consulting fees from AstraZeneca, Avanier Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly & Co., Hoffman La-Roche, Merck, Navigen, Naurex, Noven Pharmaceuticals, Servier Pharmaceuticals, Takeda, Teva and Vistagen therapeutics over the past 24 months. He has also received additional research contracts from AstraZeneca, Bristol-Myers Squibb, Eli Lilly & Co., Johnson & Johnson, Hoffman La-Roche, Merck & Co., Naurex and Servier over the past 24 months. Free medication was provided to Dr Sanacora for an NIH-sponsored study by Sanofi-Aventis. In addition, he holds shares in BioHaven Pharmaceuticals Holding Company and is a coinventor on a US patent (no. 8 778 979) held by the Yale University. Dr Duman has received consulting fees from Taisho, Naurex, Sunovion and Johnson & Johnson, and investigator-initiated grants from Forest, Naurex, Sunovion and Eli Lilly & Co. Dr Bristow is an employee of Bristol-Myers Squibb. Dr Schaeffer was an employee of Bristol-Myers Squibb at the time the research was completed and is currently an employee of Janssen Research and Development. Dr Banasr has received research contracts from BioHaven Pharmaceuticals and Servier Pharmaceuticals. Dr Behar holds common stock in Pfizer. The remaining authors declare no conflicts of interest.
Additional information
Supplementary Information accompanies the paper on the Molecular Psychiatry website
Rights and permissions
About this article
Cite this article
Chowdhury, G., Zhang, J., Thomas, M. et al. Transiently increased glutamate cycling in rat PFC is associated with rapid onset of antidepressant-like effects. Mol Psychiatry 22, 120–126 (2017). https://doi.org/10.1038/mp.2016.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2016.34
- Springer Nature Limited