Abstract
Positron emission tomography (PET) imaging of the 18 kDa translocator protein (TSPO) has been used to investigate whether microglial activation, an indication of neuroinflammation, is evident in the brain of adults with schizophrenia. Interpretation of these studies is confounded by potential modulatory effects of antipsychotic medication on microglial activity. In the first such study in antipsychotic-free schizophrenia, we have used [11C](R)-PK11195 PET to compare TSPO availability in a predominantly antipsychotic-naive group of moderate-to-severely symptomatic unmedicated patients (n=8), similarly symptomatic medicated patients with schizophrenia taking risperidone or paliperidone by regular intramuscular injection (n=8), and healthy comparison subjects (n=16). We found no evidence for increased TSPO availability in antipsychotic-free patients compared with healthy controls (mean difference 4%, P=0.981). However, TSPO availability was significantly elevated in medicated patients (mean increase 88%, P=0.032) across prefrontal (dorsolateral, ventrolateral, orbital), anterior cingulate and parietal cortical regions. In the patients, TSPO availability was also strongly correlated with negative symptoms measured using the Positive and Negative Syndrome Scale across all the brain regions investigated (r=0.651–0.741). We conclude that the pathophysiology of schizophrenia is not associated with microglial activation in the 2–6 year period following diagnosis. The elevation in the medicated patients may be a direct effect of the antipsychotic, although this study cannot exclude treatment resistance and/or longer illness duration as potential explanations. It also remains to be determined whether it is present only in a subset of patients, represents a pro- or anti-inflammatory state, its association with primary negative symptoms, and whether there are significant differences between antipsychotics.
Similar content being viewed by others
Introduction
Schizophrenia affects ~0.5–1% of the population worldwide.1 It can be characterised by three symptom domains: positive symptoms (delusions and hallucinations), negative symptoms (lack of motivation, anhedonia, flat affect, social withdrawal) and cognitive impairments, all of which can have profound effects on functioning and quality of life. The efficacy of antipsychotics is predominantly against positive symptoms, whereas the negative and cognitive symptoms remain relatively poorly modified and contribute significantly to the impaired functioning and wider burden of the disorder. Therefore, novel avenues of research need to be explored to elucidate the pathophysiological mechanisms underlying all symptom domains, and to inform the development of more effective and tolerable medications.
Convergent evidence suggests that inflammation may have a key role in the pathophysiology of schizophrenia and as a potential target for drug development.2, 3, 4, 5, 6, 7, 8, 9, 10 In particular, peripheral markers of inflammation are raised in patients with schizophrenia11 including first-episode antipsychotic-naive patients,12, 13 and there is some evidence for increased inflammatory markers post-mortem.14, 15, 16 A crucial question though, is whether there is evidence of neuroinflammation in schizophrenia in vivo.
Evidence for neuroinflammation can be measured in vivo using positron emission tomography (PET) and radioligands that bind to the 18 kDa translocator protein (TSPO), which is increasingly expressed when microglia become activated. So far, PET studies in schizophrenia have shown mixed results. Increased TSPO expression has been reported using the first-generation radiotracer [11C](R)-PK11195 (refs 17, 18) and the second-generation tracer [11C]PBR28,19 but not replicated in other second-generation tracer studies using [11C]DAA1106,20 [18F]FEPPA,21 and [11C]DPA-713.22 The discrepant findings may reflect differences in methodology, radiotracers, brain regions and aspects of the patient populations including severity and duration of illness. However, importantly, all of the schizophrenia patients in these PET studies were taking antipsychotic medication at the time of scanning, introducing a potential confound due to their effects on the immune system. The majority of in vitro studies of microglia suggest that antipsychotics are anti-inflammatory,23 although there are several contradictory reports23, 24 and the relevance of the in vitro data to the context of the in vivo brain in schizophrenia is not certain. In normal rats, the effect of chronic treatment with antipsychotics on post-mortem TSPO-binding density varies between brain regions and individual drugs,25 whereas morphological evidence for microglial activation has been found following treatment with either haloperidol or olanzapine at clinically-relevant doses.26 However, this study was unable to differentiate whether the activation represented a pro- or anti-inflammatory biochemical phenotype,27 and we are not aware of comparable published reports in non-human primates or humans.
The aims of the current study were therefore to further investigate the evidence for neuroinflammation in schizophrenia by comparing antipsychotic-free patients, medicated patients and matched-healthy volunteers, using increased TSPO availability measured by [11C](R)-PK11195 PET as evidence for microglial activation. To the best of our knowledge this is the first report of TSPO availability in vivo in drug-free schizophrenia using PET. Owing to the potential variability of effects across different antipsychotics, and to minimise additional variability from poor oral drug compliance, we studied patients taking risperidone by long acting intramuscular injection (LAI). Patients taking paliperidone LAI were also included on the basis that paliperidone is the main metabolite (9-OH-risperidone) of risperidone and is pharmacologically active in all patients taking risperidone.28 Longitudinal magnetic resonance imaging (MRI) studies of cerebral grey matter (GM) suggest that the pathological process in schizophrenia is widespread in frontal, temporal and parietal lobes,29 and it is of great topical importance to understand whether neuroinflammation is associated with this process. Our hypotheses were therefore based on these brain regions. On the basis of the literature available at the time of developing the protocol, we hypothesised that TSPO availability would be elevated in antipsychotic-free patients compared with healthy volunteers. For medicated patients, in the absence of a clear directional hypothesis from the literature, we further proposed to test the null hypothesis that TSPO availability does not significantly differ between medicated and drug-free patients. A secondary aim was to examine correlations between brain TSPO availability, symptom domains of schizophrenia, and peripheral (blood) markers of inflammation.
Materials and methods
Participants
Nineteen patients with a diagnosis of schizophrenia were recruited from mental health services in the Manchester region of the UK. PET data could not be acquired for 3 (1 failed intravenous cannulation, 2 anxiety before or during scan) and 16 patients (11 males; mean±s.d. age 33±9 year; range 18–46 year) completed the study. Of these, 8 were not taking antipsychotics (6 antipsychotic-naive and 2 antipsychotic-free for 12 and 60 months, respectively) and 8 were taking either risperidone (n=7) or paliperidone (n=1) by LAI. The majority of patients (11/16) were taking other medications, mainly antidepressants (for details of current and past medications, Supplementary Material Section B3).
Diagnosis was confirmed using the Structured Clinical Interview for the DSM-IV (SCID-I).30 Symptom severity was assessed using the Positive and Negative Syndrome Scale (PANSS).31 All patients had moderate to severe symptom severity (mean±s.d. PANSS total score 85±9) and were experiencing psychosis (PANSS positive score 21±4). For demographic and clinical characteristics, see Table 1. Patients were sex- and age-matched (±6 year) with 16 healthy volunteers (11 males; age 33±10 year; range 20–50 year) scanned with the same protocol. All participants were medically healthy on the basis of clinical history, physical examination, routine blood tests and negative urine toxicology. Additional measures included body mass index (BMI) and markers of inflammation in plasma (TNF-α, IFN-γ, IL-6, IL-8, IL-1β and CRP).
Exclusion criteria for all participants included substance abuse in the previous year, lifetime history of substance dependence, anti-inflammatory medications in the previous month, another Axis I disorder, pregnancy and history of neurological or autoimmune disorder. The study was approved by the Greater Manchester East Research Ethics Committee and the United Kingdom Administration of Radioactive Substances Advisory Committee. All subjects provided written informed consent.
MRI and PET acquisition
A 1.5 Tesla T1-weighted MRI brain scan, to exclude significant abnormality and for identification of regions of interest (ROI), was acquired as described previously.32 [11C](R)-PK11195 (1-(2-chlorophenyl)-N-methyl-N-(1-methylpropyl)-3-isoquinoline carboxamide) was synthesised onsite as described previously.33 Following intravenous injection of the radiotracer (dose range 400–740 MBq) PET emission data were acquired for 60 min on a high-resolution research tomograph (HRRT; Siemens/CTI, Knoxville, TN, USA) with intrinsic spatial resolution of ~2.5 mm full width at half the maximum, as described previously.34 PET data were reconstructed with 3D iterative ordered subset expectation maximisation35 (OSEM; 12 iterations and 16 subsets) without resolution modelling using the HRRT user community software which employs an ultrafast ordinary Poisson OSEM algorithm (OP-OSEM).36
PET image analysis
Individual MRI scans were co-registered with the summed PET images using a mutual information algorithm37 then segmented into GM and white matter probability maps.38 The inverse transformation parameters from segmentation were then used to spatially normalise a maximum probability brain atlas39, 40 into individual space. Binding potential (BPND), representing the ratio at equilibrium of specifically bound radioligand to that of non-displaceable radioligand in tissue,41 was calculated using a GM cerebellum reference input function and the simplified reference tissue model42 (Supplementary Material Sections A1-A3 for further methodological considerations, including support for the use of cerebellum as reference region). Parametric maps of BPND were generated with a basis-function implementation of the simplified reference tissue model using in-house kinetic modelling software.43 The individualised GM brain atlases were then projected onto these parametric maps to obtain mean BPND values for cortical ROIs. TSPO availability was too low in temporal cortex to accurately quantify44, 45 (Supplementary Material Section A4) so we report five cortical ROIs: dorsolateral prefrontal (DLPFC), ventrolateral (VLPFC), orbitofrontal (OFC), anterior cingulate (ACC) and parietal.
Statistical analysis
Statistical analysis was performed in SPSS Statistics Version 22 (IBM, Armonk, NY, USA). Independent samples t-tests and one-way analysis of variance (ANOVA) were used to assess differences between demographic, clinical and radiotracer characteristics across groups. Categorical data (sex, smoking status) were compared between groups using Fisher’s exact test (two-tailed). Differences in [11C](R)-PK11195 BPND (the dependent variable) between healthy controls and patients were assessed using a factorial repeated measures (‘split-plot’ or mixed between-within-subjects) ANOVA with group as between-subjects factor (three levels: healthy controls, antipsychotic-free patients and medicated patients) and brain region as within-subjects factor (five levels, one for each ROI, treated as repeated measures). The normal distribution of BPND for each combination of the levels of the between- and within-subjects factors was confirmed by Shapiro–Wilk’s test (P >0.05) and normal Q–Q plot. Equality of covariance was confirmed by Box’s test. Sphericity of the data was checked by Mauchly’s test and corrected by the Greenhouse–Geisser procedure if violated. Homogeneity of variances was checked by Levine’s test. Post hoc correction for multiple comparisons in the between-subjects factor (three groups) was by Tukey’s honest significant difference test. Correlations were measured by Pearson’s r (two-tailed). Findings were considered significant at the P<0.05 level, with correction for multiple comparisons where warranted.
Results
Patients and healthy controls were well matched for age and sex (Table 1). Patients had a higher BMI than controls, and the majority of patients (11 of 16) were smokers, whereas none of the controls smoked. However, antipsychotic-free and medicated patients were well matched for BMI and smoking status in addition to sex, age at onset of psychosis, PANSS positive and PANSS general score. Medicated patients were older and had a longer duration of illness than antipsychotic-free patients, and there was a trend for them to have lower PANSS positive and higher PANSS negative scores. The injected mass of PK11195 was very low (in the order of 2 μg per subject) and did not significantly differ between the antipsychotic-free, medicated and healthy control groups (F2,29=0.510, P=0.60). Combining all patients and controls there was no main effect of age (F1,28=1.376, P=0.251), BMI (F1,28=2.518, P=0.124) or sex (F1,28=0.379, P=0.543) so these were not included as factors or covariates in subsequent analyses.
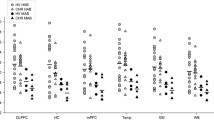
BPND was significantly different between the three groups (main effect of group: F1,29=3.843, P=0.033). Visual inspection of the data (Figure 1) suggested that BPND was higher in the medicated group compared with the other two groups and very similar between the unmedicated and control groups, across all ROIs. Pairwise comparisons showed that BPND in the medicated patients was significantly higher than in the controls (P=0.032) by a mean of 88% (Table 2; Figure 2a), not different between antipsychotic-free patients and controls (mean 4% higher; P=0.981), and although BPND was higher in medicated than antipsychotic-free patients by a mean of 83% this reached only trend statistical significance (P=0.097). Region*group interaction was not statistically significant (F5.7,82.3=1.399, P=0.216), confirming the visual impression from Figure 1 that the pattern of BPND differences between the groups did not differ across the five ROIs. Given the group differences, the significance of the elevations in individual ROIs in the medicated group was tested post hoc by t-test (one-tailed) for independent samples with unequal variance. BPND was significantly higher in the medicated than the control group in the ACC (P=0.035), DLPFC (P=0.035) and VLPFC (P=0.036), and reached trend significance in OFC (P=0.056) (Table 2; Figure 2b). BPND was significantly higher in the medicated than the antipsychotic-free patients in the OFC (P=0.043) and reached trend significance in the VLPFC (P=0.051) and DLPFC (P=0.068). For further data excluding age and BMI as significant factors in the finding, see Supplementary Material Section B1.
Regional [11C](R)-PK11195 BPND in antipsychotic-free patients with schizophrenia, patients with schizophrenia treated by risperidone or paliperidone long acting injection and healthy controls. Horizontal bars indicate means. Open circles represent controls (n=16), closed circles represent antipsychotic-free patients (n=8) and triangles represent medicated patients (n=8). ACC, anterior cingulate cortex; BPND, binding potential; DLPFC, dorsolateral prefrontal cortex; OFC, orbitofrontal cortex; VLPFC, ventrolateral prefrontal cortex.
[11C](R)-PK11195 binding in antipsychotic-free and medicated patients with schizophrenia compared with healthy controls. (a) Mean cortical BPND compared between groups, showing statistically significant elevation in medicated patients compared with controls, no difference between antipsychotic-free patients and controls, and trend difference between the two patient groups; (b) BPND in individual regions of interests (ROIs) compared between groups. *indicates a significant elevation in medicated patients compared with controls at P<0.05; #indicates significant elevation in medicated patients compared with antipsychotic-free patients at P<0.05. ACC, anterior cingulate cortex; BPND, binding potential; DLPFC, dorsolateral prefrontal cortex; OFC, orbitofrontal cortex; VLPFC, ventrolateral prefrontal cortex.
An assumption of ANOVA is that the variance of the dependent variable should be equal between the groups of the between-subjects factor. Observation of the data (Figure 1) suggested that the spread of the regional BPND values was moderately higher in the patient groups than the controls and this was confirmed by a significant Levene’s test (P-values: DLPFC 0.043; VLPFC <0.001; OFC 0.033; ACC 0.008; parietal cortex <0.001).
We found no significant correlations between [11C](R)-PK11195 BPND and scores on PANSS total, positive or general subscales. However, there were highly significant positive correlations with PANSS negative scores in DLPFC (r=0.651, P=0.006), VLPFC (r=0.741, P=0.001), OFC (r=0.706, P=0.002) and ACC (r=0.694, P=0.003). Figure 3 illustrates the correlation for VLPFC BPND. Separating the patients into medicated and unmedicated subgroups, correlations between regional BPND and PANSS negative score were significant in the medicated patient group (for example, for mean BPND across the five ROIs: r=0.819, P=0.013), but not the unmedicated patient group (mean BPND: r=0.290, P=0.486), suggesting that the correlation in the schizophrenia group as a whole (Figure 3) is predominantly due to the medicated patients. There were no significant correlations between BPND in any of the ROIs and duration of illness (whether in the medicated group, the antipsychotic-free group, or all patients together) (Supplementary Material Section B2) or any of the peripheral inflammatory markers. Nor did we find any differences in concentration of peripheral inflammatory markers between the two patient subgroups.
Correlation between [11C](R)-PK11195 BPND and scores on the negative subscale of the Positive and Negative Syndrome Scale (PANSS) in the ventrolateral prefrontal cortex (VLPFC) across antipsychotic-free (circles) and medicated (triangles) patients with schizophrenia. BPND, binding protein.
Discussion
This is the first PET study, to our knowledge, to investigate microglial activation in antipsychotic-free (predominantly antipsychotic-naïve) patients with schizophrenia and to compare the findings between antipsychotic-free and medicated patients. We found no evidence for increased TSPO availability in antipsychotic-free patients in the 2–6 year period following diagnosis. However, TSPO availability was significantly elevated in frontal and parietal cortical regions in patients taking risperidone or paliperidone LAI, providing evidence for neuroinflammation and associated microglial activation in this group. In the patients there was also a strong correlation between TSPO availability and PANSS negative score across these brain regions.
A strength of our study is that the majority of the unmedicated patients were antipsychotic-naive and the two previously medicated patients had been antipsychotic-free for 1 and 5 years, respectively. Previous PET studies of microglial activation in schizophrenia17, 18, 19, 20, 21, 22 have all been in medicated patients, which may potentially confound their interpretation. Our finding suggests that schizophrenia is not associated with microglial activation, at least not in the relatively early stages. Nevertheless, PET evidence has recently been reported for microglial activation in antipsychotic-naive people at ultra-high risk for psychosis,19 a proportion of whom can be expected to develop schizophrenia over the following few years. Indeed, the one patient who had transitioned to schizophrenia by the time of report had the highest TSPO availability in the cohort. The method for determining TSPO availability in this study has been challenged,46 but if the interpretation is valid the apparent discrepancy with our findings prompts the conjecture that microglial activation may be a dynamic process along the timeline of the prodrome, early and established phases of schizophrenia, and that microglial activation in the prodrome may no longer be apparent in the early stages of schizophrenia. However, it emphasises the need for both studies to be independently replicated before drawing firm conclusions.
A further strength is that medication was standardised in the medicated patient group and variability in compliance was minimised by intramuscular LAI. Our finding of significantly increased TSPO availability in this group is consistent with several,17, 18, 19 but not all,20, 21, 22 of the previous PET studies, and the homogeneous nature of the increase seen across cortical regions is also consistent with the global increase in microglial activation seen in rats treated chronically (8 weeks) with clinically-relevant doses of antipsychotics.26 Although an earlier study in rats did not find increased cortical TSPO binding following chronic risperidone treatment,25 clinically comparable antipsychotic doses were not used47 and our study supports such an increase at clinical doses. We should be cautious about extrapolating uncritically to other drugs, nor can we exclude the possibility that the intramuscular route of administration contributed to our findings until a comparison is made with oral administration. Patients in the other PET studies were taking a diverse range of first and second-generation antipsychotics, and it may be hypothesised that the variability in the PET studies is at least in part due to variability in the effects on microglia of different antipsychotics or doses. Further variability may come from differences in radiotracer characteristics and clinical severity, and it will be important for future studies to investigate other antipsychotics while at the same time controlling for all these variables. In addition, Figure 1 shows extensive overlap between the medicated patients and the other groups but also several medicated patients with BPND values well above the normal range, suggesting that inflammation may only be evident in a subgroup of patients with schizophrenia, an idea supported by post-mortem data.15 The only conspicuous clinical characteristic of these patients was that they had the highest scores on the PANSS negative scale (see Figure 3 and further discussion below) and there were no other obvious clinical associations with high BPND that we could identify (Supplementary Materials Section B3).
TSPO are expressed predominantly,48 but not exclusively,48, 49 on microglia and increased TSPO availability is interpreted to indicate the presence of activated microglia. However, activated microglia have a range of pro- and anti-inflammatory chemical phenotypes including classical M1 (cytotoxic), M2a (repair and regeneration) and M2b/c (immunomodulatory).27 The majority of studies specifically investigating risperidone suggest it is anti-inflammatory,50, 51, 52, 53 though neutral25 and pro-inflammatory54 effects have also been reported. Current PET TSPO radioligands are unable to differentiate between these activation states and we are unable to determine whether the increased TSPO availability seen in the medicated patients in our study represents a pro- or anti-inflammatory state. It is now appreciated that at least a proportion of the longitudinal GM volume decreases in schizophrenia may be associated with higher cumulative exposure to antipsychotics over time.55 This is consistent with post-mortem data in non-human primates56 and in vivo MRI studies in rats57, 58, 59 reporting brain volume reductions following chronic exposure to clinically-relevant doses of antipsychotics, most prominently in frontal56, 57 and parietal56 cortices as well as ACC59 where evidence for microglial activation was also found. This cautions against an assumption that our finding of increased TSPO in these areas in the medicated patients is functionally benign. In this regard, the strong correlation between severity of negative symptoms and TSPO availability in the patients is predominantly due to an association in the medicated subgroup, which is not seen in the unmedicated patients. Identification of the chemical phenotype of antipsychotic-associated microglial activation should be a priority for future studies. In a preliminary post hoc analysis of BPND in the striatum, a critical site of therapeutic action of antipsychotics,60, 61 TSPO availability was increased in our medicated patient group to only a small and non-significant extent. Although limited to a single subcortical site, these data tentatively suggest that effects of antipsychotic medication on TSPO may be more prominent in cortical than subcortical regions (see Supplementary Materials Section B4 for further details).
Although the increased BPND in the medicated group may be a direct effect of medication, alternative explanations for this finding in our study are possible. To remove symptom severity as a confounding factor, both patient groups were similarly symptomatic. The medicated patients were therefore psychotic despite treatment and may be treatment-resistant. We therefore cannot exclude the possibility that the increased TSPO availability in the medicated group is related to a difference in schizophrenia pathophysiology between the groups rather than medication. Of potential relevance, a higher baseline inflammatory state has recently been shown to be predictive of worse clinical outcomes and poorer response to antipsychotics,62 although in our schizophrenia cohort concentrations of peripheral inflammatory markers were not higher in the medicated group. Also, the medicated patients had a longer duration of illness than the antipsychotic-free patients, and we are unable to exclude this as a possible cause of their increased TSPO availability. However, BPND was not correlated with duration of illness, potentially making medication or treatment resistance more likely explanations.
Our study has several other limitations. In the absence of prior data on medication-free patients in the literature, no formal a priori power calculation was performed and group sizes (n=16) were chosen in line with similar PET studies. However, the small size of our schizophrenia subgroups limits the power to identify small between-group differences in TSPO availability, and it is likely that our finding of only trend significant difference between them is a Type II error. Nevertheless, Type II error is unlikely to explain the lack of difference between the antipsychotic-free patients and healthy controls given the extremely small difference in BPND.
We are unable in our medicated patients to distinguish between primary negative symptoms and so-called ‘pseudo-negative’ symptoms secondary to antipsychotic side effects and untreated positive symptoms. Our data therefore cannot be used to support a link between activated microglia and whatever pathophysiology underlies primary negative symptoms. In separate clinical disorders minocycline has been shown to attenuate brain microglial activation63 and to reduce negative symptoms of schizophrenia in particular,3, 4, 5 so the association is plausible. A future TSPO PET study could investigate this in a large group of similarly medicated patients stratified by high and low PANSS negative score.
We were unable to accurately quantify TSPO availability in temporal cortex with our methodology. This is an important site of longitudinal grey matter loss in schizophrenia and changes in superior temporal gyrus volume have been related to positive symptom severity.29
Although we attempted to control medication as much as possible, some patients were taking other medications including antidepressants (Supplementary Materials Section B3). Antidepressants have anti-inflammatory effects on microglia in vitro,64 although this is unlikely to have confounded our conclusions as a similar proportion of patients in both groups were taking an antidepressant (antipsychotic-free n=3; medicated n=4). Where it could be determined, the reasons included relatively mild subjective low mood and as an augmentation strategy for the treatment of negative symptoms.65 Major depressive disorder, in which microglial activation has been reported,66 was an exclusion factor in our study. One patient in the medicated group was taking diazepam, which is a ligand at the TSPO. Extrapolation from in vitro data suggests that high doses of diazepam (>30 mg daily) may reduce TSPO availability by ~9% in human PET studies.67 This patient’s dose was 5 mg daily, wasn’t taken every day, and was omitted for 24 h before PET scanning, making an appreciable effect unlikely.
With regard to the lack of homogeneity of variances between the groups, ANOVA assumes that the means of the groups are the same (null hypothesis) and the variances within the groups are equal. Using these assumptions a P-value of <0.05 was obtained meaning that one of these assumptions is invalid. Failure of either of these assumptions still demonstrates differences between the groups. Looking at the data in Figure 1, it may well be the case that there is an increase in both the mean value and variance of the medicated group, for instance through inter-individual variation in the presence or extent of an inflammatory state. Nevertheless, the statistical test is valid in demonstrating that this distribution is not by chance, and is supported by the significant elevations found by t-test in the majority of the individual ROIs in the medicated group compared with controls.
As TSPO expression is ubiquitous throughout the brain there is no ideal reference region for PET studies with TSPO radioligands. However, a standard alternative is to use a pseudo-reference region and our methodology used the cerebellum, supported by studies showing its superiority over alternative data-driven approaches34, 68 and consistent with our previous [11C](R)-PK11195 studies on the HRRT.34, 69, 70, 71 We found no evidence in our data for a significant difference in cerebellar TSPO availability between the schizophrenic patients and controls, which is consistent with a similar finding in the PET study by Bloomfield et al.,19 and further validates the use of cerebellar GM in schizophrenia (for further details, see Supplementary Material Section A3).
In conclusion, our data in antipsychotic-free patients with schizophrenia suggest for the first time that significant microglial activation is not present in the early years of the disorder. In contrast, evidence for microglial activation is present in patients medicated with risperidone or paliperidone LAI and correlates with the severity of PANSS negative score. Although this may be a direct effect of the medication, our study cannot exclude treatment resistance and/or longer duration of illness as contributory or alternative explanations, and it will be important for future studies to clarify these issues. It will also be important to investigate whether microglial activation changes longitudinally in schizophrenia unrelated to medication; the pro- or anti-inflammatory phenotype of the microglial activation seen in our medicated patients and how that may differ across antipsychotic drugs; and any association between microglial activation and primary negative symptoms, offering a target for a symptom domain that is largely untreated by current antipsychotics.
References
McGrath J, Saha S, Welham J, El Saadi O, MacCauley C, Chant D . A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med 2004; 2: 13.
Brown AS, Derkits EJ . Prenatal infection and schizophrenia: a review of epidemiologic and translational studies. Am J Psychiatry 2010; 167: 261–280.
Chaudhry IB, Hallak J, Husain N, Minhas F, Stirling J, Richardson P et al. Minocycline benefits negative symptoms in early schizophrenia: a randomised double-blind placebo-controlled clinical trial in patients on standard treatment. J Psychopharmacol 2012; 26: 1185–1193.
Ghanizadeh A, Dehbozorgi S, OmraniSigaroodi M, Rezaei Z . Minocycline as add-on treatment decreases the negative symptoms of schizophrenia; a randomized placebo-controlled clinical trial. Recent Pat Inflamm Allergy Drug Discov 2014; 8: 211–215.
Levkovitz Y, Mendlovich S, Riwkes S, Braw Y, Levkovitch-Verbin H, Gal G et al. A double-blind, randomized study of minocycline for the treatment of negative and cognitive symptoms in early-phase schizophrenia. J Clin Psychiatry 2010; 71: 138–149.
Eaton WW, Byrne M, Ewald H, Mors O, Chen CY, Agerbo E et al. Association of schizophrenia and autoimmune diseases: linkage of Danish national registers. Am J Psychiatry 2006; 163: 521–528.
Irani SR, Bera K, Waters P, Zuliani L, Maxwell S, Zandi MS et al. N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 2010; 133: 1655–1667.
Purcell SM, Wray NR, Stone JL, Visscher PM, O'Donovan MC, Sullivan PF et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 2009; 460: 748–752.
Shi J, Levinson DF, Duan J, Sanders AR, Zheng Y, Pe'er I et al. Common variants on chromosome 6p22.1 are associated with schizophrenia. Nature 2009; 460: 753–757.
Stefansson H, Ophoff RA, Steinberg S, Andreassen OA, Cichon S, Rujescu D et al. Common variants conferring risk of schizophrenia. Nature 2009; 460: 744–747.
Potvin S, Stip E, Sepehry AA, Gendron A, Bah R, Kouassi E . Inflammatory cytokine alterations in schizophrenia: a systematic quantitative review. Biol Psychiatry 2008; 63: 801–808.
Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B . Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry 2011; 70: 663–671.
Upthegrove R, Manzanares-Teson N, Barnes NM . Cytokine function in medication-naive first episode psychosis: a systematic review and meta-analysis. Schizophr Res 2014; 155: 101–108.
Radewicz K, Garey LJ, Gentleman SM, Reynolds R . Increase in HLA-DR immunoreactive microglia in frontal and temporal cortex of chronic schizophrenics. J Neuropathol Exp Neurol 2000; 59: 137–150.
Fillman SG, Cloonan N, Catts VS, Miller LC, Wong J, McCrossin T et al. Increased inflammatory markers identified in the dorsolateral prefrontal cortex of individuals with schizophrenia. Mol Psychiatry 2013; 18: 206–214.
Bayer TA, Buslei R, Havas L, Falkai P . Evidence for activation of microglia in patients with psychiatric illnesses. Neurosci Lett 1999; 271: 126–128.
van Berckel BN, Bossong MG, Boellaard R, Kloet R, Schuitemaker A, Caspers E et al. Microglia activation in recent-onset schizophrenia: a quantitative (R)-[11C]PK11195 positron emission tomography study. Biol Psychiatry 2008; 64: 820–822.
Doorduin J, de Vries EF, Willemsen AT, de Groot JC, Dierckx RA, Klein HC . Neuroinflammation in schizophrenia-related psychosis: a PET study. J Nucl Med 2009; 50: 1801–1807.
Bloomfield PS, Selvaraj S, Veronese M, Rizzo G, Bertoldo A, Owen DR et al. Microglial activity in people at ultra high risk of psychosis and in schizophrenia: an [(11)C]PBR28 PET brain imaging study. Am J Psychiatry 2016; 173: 44–52.
Takano A, Arakawa R, Ito H, Tateno A, Takahashi H, Matsumoto R et al. Peripheral benzodiazepine receptors in patients with chronic schizophrenia: a PET study with [11C]DAA1106. Int J Neuropsychopharmacol 2010; 13: 943–950.
Kenk M, Selvanathan T, Rao N, Suridjan I, Rusjan P, Remington G et al. Imaging neuroinflammation in gray and white matter in schizophrenia: an in vivo PET study with [18F]-FEPPA. Schizophr Bull 2015; 41: 85–93.
Coughlin JM, Wang Y, Ambinder EB, Ward RE, Minn I, Vranesic M et al. In vivo markers of inflammatory response in recent-onset schizophrenia: a combined study using [(11)C]DPA-713 PET and analysis of CSF and plasma. Transl Psychiatry 2016; 6: e777.
Monji A, Kato TA, Mizoguchi Y, Horikawa H, Seki Y, Kasai M et al. Neuroinflammation in schizophrenia especially focused on the role of microglia. Prog Neuropsychopharmacol Biol Psychiatry 2013; 42: 115–121.
Kluge M, Schuld A, Schacht A, Himmerich H, Dalal MA, Wehmeier PM et al. Effects of clozapine and olanzapine on cytokine systems are closely linked to weight gain and drug-induced fever. Psychoneuroendocrinology 2009; 34: 118–128.
Danovich L, Veenman L, Leschiner S, Lahav M, Shuster V, Weizman A et al. The influence of clozapine treatment and other antipsychotics on the 18 kDa translocator protein, formerly named the peripheral-type benzodiazepine receptor, and steroid production. Eur Neuropsychopharmacol 2008; 18: 24–33.
Cotel MC, Lenartowicz EM, Natesan S, Modo MM, Cooper JD, Williams SC et al. Microglial activation in the rat brain following chronic antipsychotic treatment at clinically relevant doses. Eur Neuropsychopharmacol 2015; 25: 2098–2107.
Perry VH, Nicoll JA, Holmes C . Microglia in neurodegenerative disease. Nat Rev Neurol 2010; 6: 193–201.
Knegtering R, Baselmans P, Castelein S, Bosker F, Bruggeman R, van den Bosch RJ . Predominant role of the 9-hydroxy metabolite of risperidone in elevating blood prolactin levels. Am J Psychiatry 2005; 162: 1010–1012.
Vita A, De Peri L, Deste G, Sacchetti E . Progressive loss of cortical gray matter in schizophrenia: a meta-analysis and meta-regression of longitudinal MRI studies. Transl Psychiatry Psychiatry 2012; 2: e190.
First MB, Spitzer RL, Gibbon M, Williams JBW . Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). Biometrics Research, New York State Psychiatric Institute: New York, NY, USA, 2002.
Kay SR, Fiszbein A, Opler LA . The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13: 261–276.
Talbot PS, Bradley S, Clarke CP, Babalola KO, Philipp AW, Brown G et al. Brain serotonin transporter occupancy by oral sibutramine dosed to steady state: a PET study using (11)C-DASB in healthy humans. Neuropsychopharmacology 2010; 35: 741–751.
Shah F, Hume SP, Pike VW, Ashworth S, McDermott J . Synthesis of the enantiomers of [N-methyl-11C]PK 11195 and comparison of their behaviours as radioligands for PK binding sites in rats. Nucl Med Biol 1994; 21: 573–581.
Su Z, Herholz K, Gerhard A, Roncaroli F, Du Plessis D, Jackson A et al. [11C]-(R)PK11195 tracer kinetics in the brain of glioma patients and a comparison of two referencing approaches. Eur J Nucl Med Mol Imaging 2013; 40: 1406–1419.
Hudson HM, Larkin RS . Accelerated image reconstruction using ordered subsets of projection data. IEEE Trans Med Imaging 1994; 13: 601–609.
Hong IK, Chung ST, Kim HK, Kim YB, Son YD, Cho ZH . Ultra fast symmetry and SIMD-based projection-backprojection (SSP) algorithm for 3-D PET image reconstruction. IEEE Trans Med Imaging 2007; 26: 789–803.
Cizek J, Herholz K, Vollmar S, Schrader R, Klein J, Heiss WD . Fast and robust registration of PET and MR images of human brain. Neuroimage 2004; 22: 434–442.
Ashburner J, Friston KJ . Unified segmentation. Neuroimage 2005; 26: 839–851.
Hammers A, Allom R, Koepp MJ, Free SL, Myers R, Lemieux L et al. Three-dimensional maximum probability atlas of the human brain, with particular reference to the temporal lobe. Hum Brain Mapp 2003; 19: 224–247.
Gousias IS, Rueckert D, Heckemann RA, Dyet LE, Boardman JP, Edwards AD et al. Automatic segmentation of brain MRIs of 2-year-olds into 83 regions of interest. Neuroimage 2008; 40: 672–684.
Innis RB, Cunningham VJ, Delforge J, Fujita M, Gjedde A, Gunn RN et al. Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J Cereb Blood Flow Metab 2007; 27: 1533–1539.
Lammertsma AA, Hume SP . Simplified reference tissue model for PET receptor studies. Neuroimage 1996; 4: 153–158.
Gunn RN, Lammertsma AA, Hume SP, Cunningham VJ . Parametric imaging of ligand-receptor binding in PET using a simplified reference region model. Neuroimage 1997; 6: 279–287.
Doble A, Malgouris C, Daniel M, Daniel N, Imbault F, Basbaum A et al. Labelling of peripheral-type benzodiazepine binding sites in human brain with [3H]PK 11195: anatomical and subcellular distribution. Brain Res Bull 1987; 18: 49–61.
Kumar A, Muzik O, Shandal V, Chugani D, Chakraborty P, Chugani HT . Evaluation of age-related changes in translocator protein (TSPO) in human brain using (11)C-[R]-PK11195 PET. J Neuroinflammation 2012; 9: 232.
Narendran R, Frankle WG . Comment on analyses and conclusions of "microglial activity in people at ultra high risk of psychosis and in schizophrenia: an [(11)C]PBR28 PET brain imaging study". Am J Psychiatry 2016; 173: 536–537.
Kapur S, VanderSpek SC, Brownlee BA, Nobrega JN . Antipsychotic dosing in preclinical models is often unrepresentative of the clinical condition: a suggested solution based on in vivo occupancy. J Pharmacol Exp Ther 2003; 305: 625–631.
Dickens AM, Vainio S, Marjamaki P, Johansson J, Lehtiniemi P, Rokka J et al. Detection of microglial activation in an acute model of neuroinflammation using PET and radiotracers 11C-(R)-PK11195 and 18F-GE-180. J Nucl Med 2014; 55: 466–472.
Varga B, Marko K, Hadinger N, Jelitai M, Demeter K, Tihanyi K et al. Translocator protein (TSPO 18kDa) is expressed by neural stem and neuronal precursor cells. Neurosci Lett 2009; 462: 257–262.
Cazzullo CL, Sacchetti E, Galluzzo A, Panariello A, Adorni A, Pegoraro M et al. Cytokine profiles in schizophrenic patients treated with risperidone: a 3-month follow-up study. Prog Neuropsychopharmacol Biol Psychiatry 2002; 26: 33–39.
Kato T, Monji A, Hashioka S, Kanba S . Risperidone significantly inhibits interferon-gamma-induced microglial activation in vitro. Schizophr Res 2007; 92: 108–115.
Zhang XY, Zhou DF, Cao LY, Zhang PY, Wu GY, Shen YC . Changes in serum interleukin-2, -6, and -8 levels before and during treatment with risperidone and haloperidol: relationship to outcome in schizophrenia. J Clin Psychiatry 2004; 65: 940–947.
Sugino H, Futamura T, Mitsumoto Y, Maeda K, Marunaka Y . Atypical antipsychotics suppress production of proinflammatory cytokines and up-regulate interleukin-10 in lipopolysaccharide-treated mice. Prog Neuropsychopharmacol Biol Psychiatry 2009; 33: 303–307.
Kim DJ, Kim W, Yoon SJ, Go HJ, Choi BM, Jun TY et al. Effect of risperidone on serum cytokines. Int J Neurosci 2001; 111: 11–19.
Fusar-Poli P, Smieskova R, Kempton MJ, Ho BC, Andreasen NC, Borgwardt S . Progressive brain changes in schizophrenia related to antipsychotic treatment? A meta-analysis of longitudinal MRI studies. Neurosci Biobehav Rev 2013; 37: 1680–1691.
Dorph-Petersen KA, Pierri JN, Perel JM, Sun Z, Sampson AR, Lewis DA . The influence of chronic exposure to antipsychotic medications on brain size before and after tissue fixation: a comparison of haloperidol and olanzapine in macaque monkeys. Neuropsychopharmacology 2005; 30: 1649–1661.
Vernon AC, Natesan S, Modo M, Kapur S . Effect of chronic antipsychotic treatment on brain structure: a serial magnetic resonance imaging study with ex vivo and postmortem confirmation. Biol Psychiatry 2011; 69: 936–944.
Vernon AC, Natesan S, Crum WR, Cooper JD, Modo M, Williams SC et al. Contrasting effects of haloperidol and lithium on rodent brain structure: a magnetic resonance imaging study with postmortem confirmation. Biol Psychiatry 2012; 71: 855–863.
Vernon AC, Crum WR, Lerch JP, Chege W, Natesan S, Modo M et al. Reduced cortical volume and elevated astrocyte density in rats chronically treated with antipsychotic drugs-linking magnetic resonance imaging findings to cellular pathology. Biol Psychiatry 2014; 75: 982–990.
Agid O, Mamo D, Ginovart N, Vitcu I, Wilson AA, Zipursky RB et al. Striatal vs extrastriatal dopamine D2 receptors in antipsychotic response—a double-blind PET study in schizophrenia. Neuropsychopharmacology 2007; 32: 1209–1215.
Kegeles LS, Slifstein M, Frankle WG, Xu X, Hackett E, Bae SA et al. Dose-occupancy study of striatal and extrastriatal dopamine D2 receptors by aripiprazole in schizophrenia with PET and [18F]fallypride. Neuropsychopharmacology 2008; 33: 3111–3125.
Mondelli V, Ciufolini S, Belvederi Murri M, Bonaccorso S, Di Forti M, Giordano A et al. Cortisol and inflammatory biomarkers predict poor treatment response in first episode psychosis. Schizophr Bull 2015; 41: 1162–1170.
Dodel R, Spottke A, Gerhard A, Reuss A, Reinecker S, Schimke N et al. Minocycline 1-year therapy in multiple-system-atrophy: effect on clinical symptoms and [(11)C] (R)-PK11195 PET (MEMSA-trial). Mov Disord 2010; 25: 97–107.
Tynan RJ, Weidenhofer J, Hinwood M, Cairns MJ, Day TA, Walker FR . A comparative examination of the anti-inflammatory effects of SSRI and SNRI antidepressants on LPS stimulated microglia. Brain Behav Immun 2012; 26: 469–479.
Singh SP, Singh V, Kar N, Chan K . Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: meta-analysis. Br J Psychiatry 2010; 197: 174–179.
Setiawan E, Wilson AA, Mizrahi R, Rusjan PM, Miler L, Rajkowska G et al. Role of translocator protein density, a marker of neuroinflammation, in the brain during major depressive episodes. JAMA Psychiatry 2015; 72: 268–275.
Kalk NJ, Owen DR, Tyacke RJ, Reynolds R, Rabiner EA, Lingford-Hughes AR et al. Are prescribed benzodiazepines likely to affect the availability of the 18 kDa translocator protein (TSPO) in PET studies? Synapse 2013; 67: 909–912.
Kropholler MA, Boellaard R, van Berckel BN, Schuitemaker A, Kloet RW, Lubberink MJ et al. Evaluation of reference regions for (R)-[(11)C]PK11195 studies in Alzheimer's disease and mild cognitive impairment. J Cereb Blood Flow Metab 2007; 27: 1965–1974.
Drake C, Boutin H, Jones MS, Denes A, McColl BW, Selvarajah JR et al. Brain inflammation is induced by co-morbidities and risk factors for stroke. Brain Behav Immun 2011; 25: 1113–1122.
Su Z, Roncaroli F, Durrenberger PF, Coope DJ, Karabatsou K, Hinz R et al. The 18-kDa mitochondrial translocator protein in human gliomas: an 11C-(R)PK11195 PET imaging and neuropathology study. J Nucl Med 2015; 56: 512–517.
Hunter HJA, Hinz R, Gerhard A, Talbot PS, Su Z, Holland G et al. Brain inflammation and psoriasis: a [11C]-(R)-PK11195 positron emission tomography study. Br J Dermatol 2016; doi:10.1111/bjd.13788.
Acknowledgements
This study was partly funded by the award of the Margaret Temple grant from the British Medical Association’s Board of Science to SEH, and financial support was provided by Professor Karl Herholz and the University of Manchester’s Magnetic Resonance Imaging Facility (MRIF). AG and RH have received funding from the European Union’s Seventh Framework Programme (FP7/2007-2013) under Grant Agreement Number HEALTH-F2-2011-278850 (INMiND). The authors acknowledge the contributions of operational staff at the Wolfson Molecular Imaging Centre, including Elizabeth Barnett and Carrie-Anne Mellor for processing of blood samples; Michael Green, Team Leader for Radiochemistry Production; PET radiographers Mike Godfrey, Eleanor Duncan-Rouse and Gerrit Helms van der Vegte; and MR Radiographers Amy Watkins and Barry Whitnall. Recruitment was supported by staff of the National Institute for Health Research Clinical Research Network: Greater Manchester.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Molecular Psychiatry website
Supplementary information
Rights and permissions
About this article
Cite this article
Holmes, S., Hinz, R., Drake, R. et al. In vivo imaging of brain microglial activity in antipsychotic-free and medicated schizophrenia: a [11C](R)-PK11195 positron emission tomography study. Mol Psychiatry 21, 1672–1679 (2016). https://doi.org/10.1038/mp.2016.180
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2016.180
- Springer Nature Limited
This article is cited by
-
Microglia sequelae: brain signature of innate immunity in schizophrenia
Translational Psychiatry (2022)
-
The utility of PET imaging in the diagnosis and management of psychosis: a brief review
Clinical and Translational Imaging (2022)
-
Increased levels of midbrain immune-related transcripts in schizophrenia and in murine offspring after maternal immune activation
Molecular Psychiatry (2021)
-
Haploinsufficiency of the schizophrenia and autism risk gene Cyfip1 causes abnormal postnatal hippocampal neurogenesis through microglial and Arp2/3 mediated actin dependent mechanisms
Translational Psychiatry (2021)
-
Neuroinflammation as measured by positron emission tomography in patients with recent onset and established schizophrenia: implications for immune pathogenesis
Molecular Psychiatry (2021)