Abstract
Objective:
To compare the neurodevelopmental outcomes at 18 to 21 months corrected age (CA) of infants born at <29 weeks that received room air, an intermediate oxygen concentration or 100% oxygen at the initiation of resuscitation.
Study design:
In this retrospective cohort study, we compared neonatal and neurodevelopmental outcomes at 18 to 21 months CA among inborn infants born before 29 weeks’ gestation that received room air, intermediate oxygen concentration or 100% oxygen at the initiation of resuscitation.
Results:
Of 1509 infants, 445 received room air, 483 received intermediate oxygen concentrations and 581 received 100% oxygen. Compared to infants that received room air, the primary outcome of death or neurodevelopmental impairment (NDI) was not different in intermediate oxygen (adjusted odds ratio (aOR) 1.01; 95% confidence interval (CI) 0.77, 1.34) or 100% oxygen (aOR 1.03; 95% CI 0.78, 1.35). Compared to room air, there was no difference in odds of death or severe NDI in intermediate oxygen (aOR 1.14; 95% CI 0.82, 1.58) or 100% oxygen group (aOR 1.22; 95% CI 0.90, 1.67). The odds of severe NDI among survivors were significantly higher in infants that received 100% oxygen as compared to room air (aOR 1.57, 95% CI 1.05, 2.35).
Conclusions:
We observed no significant difference in the primary composite outcomes of death or NDI and death or severe NDI at 18 to 21 months CA between infants that received room air, intermediate oxygen concentration or 100% oxygen at the initiation of resuscitation. However, use of 100% oxygen was associated with increased odds of severe NDI among survivors as compared to room air.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Oxygen is a vital element for human survival and plays a major role in a diverse range of biological and physiological processes. However, exposure to high oxygen concentrations can lead to a release of toxic free radicals and reactive oxygen species, often resulting in oxidative stress-induced cellular injury.1, 2, 3, 4 Currently, there is good evidence for using room air instead of 100% oxygen to initiate resuscitation for full-term asphyxiated infants.5, 6 Preterm infants are especially prone to oxygen toxicity as they frequently require resuscitation at birth and have inadequate antioxidant defense systems.7, 8 Despite advances in neonatal care, the optimal initial fraction of inspired oxygen (FiO2) for delivery room resuscitation in preterm infants is not known, although several changes in the guidelines for oxygen therapy in the neonatal resuscitation program have been proposed in the last few years. In 2010, the International Liaison Committee on Resuscitation recommended that preterm infants <32 weeks’ gestation should receive blended oxygen and air during resuscitation.9 However, if not available, the recommendation has been to start resuscitation with room air, while no specific oxygen concentration was recommended.
Three systematic reviews and meta-analyses on preterm infants resuscitated with room air versus oxygen supplementation have been conducted.10, 11, 12 In the latest meta-analysis, there was no significant difference in mortality, bronchopulmonary dysplasia (BPD), intraventricular hemorrhage (IVH), retinopathy of prematurity (ROP) or necrotizing enterocolitis (NEC) between infants randomized to resuscitation with low oxygen (FiO2 ⩽0.3) and those receiving high oxygen (FiO2 ⩾0.60) at delivery.12 Mortality was lower in low oxygen arm of masked studies and higher in low oxygen arms of unmasked studies. Such difference in mortality between masked and unmasked studies may suggest the possibility of a type 1 error.
Information on the long-term neurodevelopmental outcomes of infants resuscitated with varying degrees of oxygen concentrations has been limited, as few studies have compared neurodevelopmental outcomes between two groups—low or high oxygen for initiation of resuscitation.13, 14, 15, 16 Saugstad et al. reported no significant differences in neurological handicap or developmental milestones at 18 to 24 months in infants resuscitated with either room air or 100% O2 at birth.13 Similarly, a meta-analysis of three studies did not show any significant difference in the neurological outcome between infants resuscitated with room air and 100% oxygen.14 However, it should be noted that infants were assessed at different follow-up ages and most participants were late preterm and term infants. Recently, Boronat et al.16 reported no difference in neuromotor or neurosensory outcome at 2 years between preterm infants resuscitated with initial low oxygen (FiO2 0.30) and high oxygen (FiO2 0.60 to 0.65) concentrations. As of yet, the effect of different oxygen concentrations at initiation of delivery room resuscitation on neurodevelopmental outcomes in preterm infants remains uncertain. The objective of this study was to compare the neurodevelopmental outcomes at 18 to 21 months corrected age (CA) of infants born at <29 weeks gestational age (GA) who received room air, intermediate oxygen concentration or 100% oxygen at the start of delivery room resuscitation.
Methods
Study design
In this retrospective cohort study, we included inborn infants who were born at <29 weeks’ GA, admitted to level III neonatal intensive care units (NICUs) participating in the Canadian Neonatal Network (CNN) between 1 January 2010 and 30 September 2011, and were assessed at 18 to 21 months CA in a follow-up program associated with the Canadian Neonatal Follow-up Network (CNFUN). We excluded infants with major congenital or chromosomal anomalies, those with planned palliative care before delivery, those lost to follow-up and those with missing oxygen data at delivery. During this study period, as there was no specific recommendation regarding the concentration of oxygen to begin resuscitation in preterm infants, starting oxygen concentration was guided by local protocol in each institution. However, infants receiving supplemental oxygen were titrated using pulse oximetry to achieve saturation targets as per neonatal resuscitation program. Based on the starting oxygen concentration at delivery room resuscitation, we divided the cohort into three groups: room air, intermediate oxygen concentration and 100% oxygen.
During the study period, the CNN included all 28 participating tertiary NICUs in the country, while the CNFUN consisted of all 26 neonatal follow-up programs across Canada. Data were collected as part of the Canadian Institute of Health Research team in Maternal Infant Care study. Ethics or appropriate regulatory committee approval was obtained for the Maternal Infant Care study at all participating sites and written informed consent for the follow-up assessment was obtained as per local research ethics board requirements. This study was approved by the research ethics board at the University of Calgary and the executive committees of both networks.
Data collection
Data were transmitted electronically to the CNN and CNFUN, which were linked using a single identifier. Maternal and birth characteristics, in addition to neonatal outcomes were abstracted. These included maternal age, maternal education, antenatal risk factors, antenatal steroid use, prolonged rupture of membranes (>24 h), intrapartum antibiotics, mode of delivery, birth weight, GA, sex, small for GA, multiple births, Apgar score at 1 and 5 min, Score for Neonatal Acute Physiology-version II (SNAP-II) score, initial gas used during resuscitation, respiratory distress syndrome, pneumothorax, BPD, IVH, periventricular leukomalacia (PVL), NEC stage ⩾2, intestinal perforation, ROP ⩾ stage 3, duration of ventilation, duration of hospitalization and mortality.
Definitions
Indices of neonatal outcomes were defined according to the CNN and CNFUN Data Abstractor Manuals.17, 18 Diagnosis and severity of IVH was based on the criteria of Papile.19 Severe neurological injury was defined as radiological evidence of parenchymal brain injury or ventriculomegaly with or without IVH (that is, ⩾ grade 3 IVH) and/or PVL. NEC was defined according to modified Bell's criteria (⩾ stage 2).20 Patent ductus arteriosus was defined as clinical and echocardiographic diagnosis plus treatment with indomethacin/ibuprofen, surgical ligation or both. BPD was defined as any supplemental oxygen and/or respiratory support at 36 weeks post-menstrual age or at discharge from the participating unit.21 ROP was diagnosed according to the International Classification of Retinopathy of Prematurity.22
Neurodevelopmental assessment
The neurodevelopmental assessment at 18 to 21 months CA for this study is described previously.23 The assessment included a standardized history, physical examination, neurological examination and the Bayley Scales of Infant and Toddler Development-Third Edition (Bayley III).24 The members of the multidisciplinary team in the follow-up clinic were not aware of the concentration of oxygen used during initiation of resuscitation. The Gross Motor Function Classification System (GMFCS) was used to classify the functional impairment in children with cerebral palsy.25 Hearing and visual outcomes were also assessed.
Outcomes measures
The primary outcomes for this study were (a) the composite of death or neurodevelopmental impairment (NDI) and (b) death or severe NDI at 18 to 21 months CA. These outcomes were selected because infants who died before neurodevelopmental assessment could not be classified as having NDI. Our pre-specified secondary outcomes included mortality (during NICU stay and after discharge), NDI among survivors, severe NDI among survivors and individual components of the primary composite outcome. NDI was defined as the presence of any one of the following: cerebral palsy with GMFCS > I, Bayley III score of <85 on any one of the components (cognitive, language, motor composite score), sensorineural or mixed hearing loss, and visual impairment. Severe NDI was defined as presence of any one or more of the following: cerebral palsy with GMFCS III, IV or V, Bayley III score of <70 on any of the components (cognitive, language or motor composite score), hearing impairment requiring hearing aids or cochlear implant, and bilateral visual impairment (diagnosed by an ophthalmologist as presence of macular drag, traction or detachment, visual acuity of 20/70 or worse). Children who could not be tested using the Bayley III but who had a Bayley III General Adaptive Composite score <70 or were assessed to have a severe developmental delay were also diagnosed with severe NDI.
Statistical analyses
Statistical analyses were performed with SAS version 9.2 software package (SAS Institute Inc, Cary, NC, USA). Descriptive statistics were performed to compare infants who received room air, intermediate oxygen and 100% oxygen at the initiation of resuscitation. Pearson χ2 or Fisher’s exact test for categorical variables and Student’s t-test or analysis of variance F-test for continuous variables was used for the analyses. Multivariable logistic regression analyses were performed to adjust for other potential confounding factors that may have an independent effect on NDI. Confounding variables adjusted for in the multivariate analyses include GA, antenatal steroid, sex, maternal education, SNAP-II score, maternal antibiotics and small for GA. All P-values were two-sided and P<0.05 was considered statistically significant.
Results
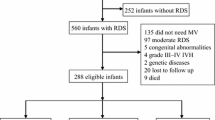
Of the 2760 preterm infants were admitted to NICUs, 1825 infants were eligible for the study. Figure 1 shows the flow diagram of the study participants. Of the 1509 infants included in the study, 445 (29%) started with room air, 483 (32%) with intermediate oxygen and 581(39%) with 100% oxygen at the initiation of resuscitation. A total of 264 infants died, 252 before discharge and 12 infants died after discharge before follow up. The baseline demographic characteristics are shown in Table 1. Compared with room air group, the rate of maternal hypertension was significantly higher in the intermediate oxygen group. Maternal intrapartum antibiotic therapy was higher in the room air group as compared to the 100% oxygen group. Compared with infants in the room air group, 100% oxygen group infants had lower mean birth weight and GA and displayed higher SNAP-II scores.
Table 2 shows the comparison of neonatal outcomes between the groups. Compared with the room air group, 100% oxygen group infants had significantly higher rates of BPD, IVH (all grades), patent ductus arteriosus, longer duration of mechanical ventilation and overall mortality. Nosocomial sepsis was significantly lower in the intermediate oxygen group.
Primary outcome
Of the 1825 eligible infants, 252 died during the NICU stay, 12 died post discharge and 316 were lost to follow-up. A total of 1245/1561(80%) surviving infants were seen at the follow-up assessment. Compared to infants who attended follow-up assessment, infants that were lost to follow-up had a higher mean birth weight, mean GA, 1 and 5 min Apgar scores and lower SNAP-II scores.
Bivariate analysis revealed that the primary outcome of composite of death or NDI was significantly higher in the 100% oxygen group as compared to those in room air (59 versus 51%, P=0.02). Similarly, the composite outcome of death or severe NDI was significantly higher in the 100% oxygen group as compared to the room air group (37 versus 26%, P<0.01). However, there was no significant difference in the composite outcome of death or NDI, as well as death or severe NDI between room air and intermediate oxygen concentration groups. Among survivors, severe NDI was significantly higher among 100% oxygen groups as compared to room air group. (Table 3) The median cognitive and language score was significantly lower in 100% oxygen group, when compared to room air.
After controlling for confounders, multivariable logistic regression analysis revealed that the primary outcome of death or NDI was not different between either intermediate oxygen (adjusted odds ratio (aOR) 1.01, 95% confidence interval (CI) 0.77, 1.34) or 100% oxygen groups (aOR 1.03, 95% CI 0.78, 1.35) compared to the 21% oxygen group (Table 4).
Similarly, there was no difference in odds of death or severe NDI in intermediate oxygen (aOR 1.14; 95% CI 0.82, 1.58) or 100% oxygen groups (aOR 1.22; 95% CI 0.90, 1.67) when compared to room air. However, the odds of severe NDI among survivors remained significantly higher among infants that received 100% oxygen as compared to room air (aOR 1.57, 95% CI 1.05, 2.35).
Discussion
In this large multicenter study involving extremely preterm infants, we observed that during the years of 2010 to 2011, initial oxygen concentration used during resuscitation of extremely preterm neonates was variable. We identified that there were no significant differences in the primary composite outcomes of (a) death or NDI and (b) death or severe NDI at 18 to 21 months CA between infants who received room air, intermediate oxygen concentration or 100% oxygen at the initiation of resuscitation. However, we observed a 1.6-fold increase in the odds of severe NDI among survivors that received 100% oxygen as compared to room air.
There are many small randomized control trials examining low versus high oxygen concentration at delivery room resuscitation.3, 26, 27, 28, 29 However, limited data are available regarding the early childhood developmental outcomes of infants resuscitated with varying oxygen concentrations. Previous studies including a meta-analysis found no difference in the neuromotor or neurosensory outcomes between infants resuscitated with initial low oxygen and high oxygen.13, 14, 16 In a study presented as an abstract, Kapadia et al.15 reported a higher incidence of severe NDI among preterm infants started with 100% oxygen as compared to room air. They also observed a lower Bayley III motor composite score <70 in 100% oxygen group after adjusting for potential confounding variables. Similarly, in the current study, we also observed increased odds of severe NDI among infants that started 100% oxygen at the initiation of resuscitation compared to room air.
Potential mechanisms suspected for NDI associated with excessive oxygen exposure include: excessive production of reactive oxygen species, fluctuations in blood oxygen levels and brain injury. It has been shown that even a brief 100% oxygen exposure during resuscitation can increase oxidative stress and reduce antioxidant capacity as measured using biomarkers such as total hydroperoxide, biological antioxidant potential, reduced glutathione/oxidized glutathione ratio and superoxide dismutase activity.3 Oxidative stress increases neonatal morbidities such as BPD, ROP,30 IVH, PVL and lower mental developmental index.31 With increasing evidence from laboratory and biochemical data, guidelines and recommendations were modified in practically all countries. However, data on infancy or childhood outcomes in previous studies have derived from very small sample sizes. Ours is the largest cohort to provide such data; however, we were unable to demonstrate differences in any of the composite outcomes. The difference in severe NDI among survivors between room air and 100% oxygen could be a real difference or a type 1 error as we compared multiple outcomes in this analysis.
Recent studies have raised some concern about increasing mortality with use of lower oxygen at delivery room resuscitation.32, 33 In a retrospective study of infants ⩽27 weeks, Rabi et al. reported that severe neurological injury or death was higher among infants resuscitated with room air as compared to 100% oxygen.32 This study addressed outcomes following a policy change in NICUs regarding oxygen use in the delivery room between 2004 and 2009. We would like to point out that the study by Rabi et al. was based on the survey data from each unit when they switch to different oxygen concentration and data were analyzed based on the timing of change and not based on what the infants received. The most important difference is that previous study was asking question of 'what is unit practice/guideline' whereas current study is data based on 'what the individual baby received'. Current study is an extension and improvement over previous study. Recently, Oei et al. reported a randomized trial of preterm <32 weeks who were initiated with either room air or 100% O2 and titrated to achieve a target oxygen saturation of 65 to 95% at 5 min and 85% to 95% until NICU admission.33 The authors observed no significant difference in the overall mortality rate between the two groups. However, subgroup analysis of infants <28 weeks’ gestation showed higher neonatal mortality in the group resuscitated with room air compared to 100% oxygen group (22 versus 6%). The primary outcome of the study was death and major disability at 2 years CA, the results are still awaited. The authors cautioned while interpreting the above results because of small sample size as the study was stopped after recruiting only 15% of the targeted sample size due to slow enrollment. In contrast, our study includes infants who were actually treated with specific oxygen concentrations at the beginning of resuscitation, where we observed no significant difference in mortality after adjustment for confounding factors.
The strengths of our study include: a large population-based sample of inborn neonates admitted to level III NICUs with prospective data collection, uniform definitions, standardized neurodevelopmental outcome evaluations and sufficient follow-up rates. However, our study has some limitations due to the retrospective nature of this secondary analysis. The centers participated in Canadian Neonatal Network follow the neonatal resuscitation program guidelines including titration of oxygen to meet targeted saturation. However, for the duration of the study, there was no uniform policy for oxygen initiation or titration and it was left to the individual sites. The exact concentration of starting FiO2 in the intermediate O2 group was not recorded. Most NICUs that used an intermediate oxygen concentration used a FiO2 of 0.30 to 0.60. The database also did not have information regarding the indication for choice of initial oxygen concentration and whether it was center, practitioner or neonate dependent.
Conclusions
In conclusion, marked variation in start-up oxygen concentration in the resuscitation of extremely preterm neonates was identified. There was no significant difference in the primary composite outcomes of (a) death or NDI and (b) death or severe NDI at 18 to 21 months CA between infants who received room air, intermediate oxygen concentration or 100% oxygen at the initiation of resuscitation. However, use of 100% oxygen at the initiation of delivery room resuscitation was associated with increased odds of severe NDI at 18 to 21 months CA among survivors. The correct oxygen concentration to initiate resuscitation of extremely preterm infants has yet to be determined and future randomize trials should focus on the assessment of long-term neurodevelopmental outcomes.
References
Barazzone C, Horowitz S, Donati YR, Rodriguez I, Piguet PF . Oxygen toxicity in mouse lung: pathways to cell death. Am J Respir Cell Mol Biol 1998; 19: 573–581.
Saugstad OD, Sejersted Y, Solberg R, Wollen EJ, Bjørås M . Oxygenation of the newborn: a molecular approach. Neonatology 2012; 101: 315–325.
Kapadia VS, Chalak LF, Sparks JE, Allen JR, Savani RC, Wyckoff MH . Resuscitation of preterm neonates with limited versus high oxygen strategy. Pediatrics 2013; 132: e1488–e1496.
Tataranno ML, Oei JL, Perrone S, Wright IM, Smyth JP, Lui K et al. Resuscitating preterm infants with 100% oxygen is associated with higher oxidative stress than room air. Acta Paediatr 2015; 104: 759–765.
Tan A, Schulze A, O'Donnell CP, Davis PG . Air versus oxygen for resuscitation of infants at birth. Cochrane Database Syst Rev 2005; (2): CD002273.
Rabi Y, Rabi D, Yee W . Room air resuscitation of the depressed newborn: a systematic review and meta-analysis. Resuscitation 2007; 72: 353–363.
Chen Y, Whitney PL, Frank L . Comparative responses of premature versus full-term newborn rats to prolonged hyperoxia. Pediatr Res 1994; 35: 233–237.
O’Donovan DJ, Fernandes CJ . Free radicals and diseases in premature infants. Antioxid Redox Signal 2004; 6: 169–176.
Perlman JM, Wyllie J, Kattwinkel J, Atkins DL, Chameides L, Goldsmith JP et al. Neonatal resuscitation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Pediatrics 2010; 126: e1319–e1344.
Brown JV, Moe-Byrne T, Harden M, McGuire W . Lower versus higher oxygen concentration for delivery room stabilisation of preterm neonates: systematicreview. PLoS ONE 2012; 7: e52033.
Saugstad OD, Aune D, Aguar M, Kapadia V, Finer N, Vento M . Systematic review and meta-analysis of optimal initial fraction of oxygen levels in the delivery room at ≤32 weeks. Acta Paediatr 2014; 103: 744–751.
Oei JL, Vento M, Rabi Y, Wright I, Finer N, Rich W et al. Higher or lower oxygen for delivery room resuscitation of preterm infants below 28 completed weeks gestation: a meta-analysis. Arch Dis Child Fetal Neonatal Ed 2017; 102: F24–F30.
Saugstad OD, Ramji S, Irani SF, El-Meneza S, Hernandez EA, Vento M et al. Resuscitation of newborn infants with 21% or 100% oxygen: follow-up at 18 to 24 months. Pediatrics 2003; 112: 296–300.
Saugstad OD, Vento M, Ramji S, Howard D, Soll RF . Neurodevelopmental outcome of infants resuscitated with air or 100% oxygen: a systematic review and meta-analysis. Neonatology 2012; 102: 98–103.
Kapadia V, Ofman G, Savani R, Heyne R, Wyckoff M Delivery Room Resuscitation Using 2011 Neonatal Resuscitation Program Oxygen Guidelines and Neurodevelopmental Outcomes in Preterm neonates. Proceedings of the Pediatric Academic Societies Meeting, April 2015, San Diego, CA, USA. E-PAS 2015; 3585: 7..
Boronat N, Aguar M, Rook D, Iriondo M, Brugada M, Cernada M et al. Survival and neurodevelopmental outcomes of preterms resuscitated with different oxygen fractions. Pediatrics 2016; 138, pii: e20161405.
Canadian Neonatal Network. Abstractor’s manual v2.1.2:2014. Available at: http://www.canadianneonatalnetwork.org/portal/CNNHome/Publications.aspx. Accessed on January 2016.
Canadian Neonatal Follow-Up Network. 18 month corrected age assessment manual. September 2012, version 5. Available at: http://www.cnfun.ca/Resources.aspx. Accessed on January 2016.
Papile LA, Munsick-Bruno G, Schaefer A . Relationship of cerebral intraventricular hemorrhage and early childhood neurologic handicaps. J Pediatr 1983; 103 (2): 273–277.
Walsh MC, Kliegman RM . Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am 1986; 33: 179–201.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82: 527–532.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol 2005; 123: 991–999.
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed 2017; 102: F235–F243.
Bayley N Manual for the Bayley Scales of Infant and Toddler Development, 3rd edn. The Psychological Corporation: San Antonio, TX, USA, 2006.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B . Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997; 39: 214–223.
Wang CL, Anderson C, Leone TA, Rich W, Govindaswami B, Finer NN . Resuscitation of preterm neonates by using room air or 100% oxygen. Pediatrics 2008; 121: 1083–1089.
Escrig R, Arruza L, Izquierdo I, Villar G, Sáenz P, Gimeno A et al. Achievement of targeted saturation values in extremely low gestational age neonates resuscitated with low or high oxygen concentrations: a prospective, randomized trial. Pediatrics 2008; 121: 875–881.
Vento M, Moro M, Escrig R, Arruza L, Villar G, Izquierdo I et al. Preterm resuscitation with low oxygen causes less oxidative stress, inflammation, and chronic lung disease. Pediatrics 2009; 124: e439–e449.
Rabi Y, Singhal N, Nettel-Aguirre A . Room-air versus oxygen administration for resuscitation of preterm infants: the ROAR study. Pediatrics 2011; 128: e374–e381.
Hartnett ME, Penn JS . Mechanisms and management of retinopathy of prematurity. N Engl J Med 2012; 367: 2515–2526.
Shoji H, Ikeda N, Hosozawa M, Ohkawa N, Matsunaga N, Suganuma H et al. Oxidative stress early in infancy and neurodevelopmental outcome in very low-birth weight infants. Pediatr Int 2014; 56: 709–713.
Rabi Y, Lodha A, Soraisham A, Singhal N, Barrington K, Shah PS . Outcomes of preterm infants following the introduction of room air resuscitation. Resuscitation 2015; 96: 252–259.
Oei JL, Saugstad OD, Lui K, Wright IM, Smyth JP, Craven P et al. Targeted oxygen in the resuscitation of preterm infants, a randomized clinical trial. Pediatrics 2017; 139, pii: e20161452..
Acknowledgements
We would like to acknowledge the staff of the Canadian Neonatal Network and Canadian neonatal Follow-up Network coordinating center for their tireless and diligent work and Natasha Musrap, PhD, (Maternal Infant Care Research Centre, Mount Sinai Hospital) for editorial assistance. The Maternal-Infant Care Research Centre is supported by the Ontario Ministry of Health and Long-Term Care. Organizational support to the Canadian Neonatal Network is provided by the Canadian Institutes of Health Research-funded Team in Maternal-Infant Care. We thank the data abstractors of the CNN, staff of the CNN and CNFUN coordinating centers for providing organizational support, and all CNN and CNFUN site investigators. Administrative and statistical support for the study was provided by the Canadian Neonatal Network Coordinating Centre at the Maternal-Infant Research Centre, Mount Sinai Hospital, Toronto, Ontario. The Maternal-Infant Research Centre is supported by funding from the Canadian Institutes of Health Research (CIHR) (CTP87518) and the Ministry of Health and Long-Term Care, Ontario, Canada.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Members of the investigators of the Canadian Neonatal Network and Canadian Neonatal Follow up Network
A Synnes5, PS Shah6, A Harrison7, T Pillay7, Z Cieslak8, T Sorokan9, R Sherlock9, J Ting10, W Yee11, R Sauve11, K Aziz12, Z Kalapesi13, J Bodani13, K Sankaran14, S Daspal14, M Seshia15 and D Moddemann15, R Alvaro16, S Shivananda17, S el Helou17, O DaSilva18, D Lee18, C Nwaesei19, KS Lee20, L Ly20, E Kelly21, M Dunn22, P Church22, N Rouvinez-Bouali23, Brigitte Lemyre23, T Daboval23, K Dow24, E Pelausa25, K Barrington26, F Lefebvre26, C Drolet27, S Belanger27, P Riley28, M Claveau28, D Faucher29, V Bertelle30, E Masse30, C Demers30, R Canning31, B Bulleid32, H Makary32, C Ojah33, L Monterrosa33, A Deshpandey34, P Murphy34, J Afifi35, M Vincer35, A Kajetanowicz36, SK Lee37
5Children’s & Women’s Health Centre of British Columbia, Vancouver, BC, Canada; 6Mount Sinai Hospital, Toronto, Ontario; 7Victoria General Hospital, Victoria, BC, Canada; 8Royal Columbian Hospital, New Westminster, BC, Canada; 9Surrey Memorial Hospital, Surrey, BC, Canada; 10Children’s & Women’s Health Centre of British Columbia, Vancouver, BC, Canada; 11Foothills Medical Centre, Calgary, AB, Canada; 12Royal Alexandra Hospital, A. Reichert, Glenrose Rehabilitation Hospital, Edmonton, AB, Canada; 13Regina General Hospital, Regina, SK, Canada; 14Royal University Hospital, Saskatoon, SK, Canada; 15Winnipeg Health Sciences Centre, Winnipeg, MB, Canada; 16St. Boniface General Hospital, Winnipeg, MB, Canada; 17Hamilton Health Sciences Centre, Hamilton, ON, Canada; 18London Health Sciences Centre, London, ON, Canada; 19Windsor Regional Hospital, Windsor, ON, Canada; 20Hospital for Sick Children, Toronto, ON, Canada; 21Mount Sinai Hospital, Toronto, ON, Canada; 22Sunnybrook Health Sciences Centre, Toronto, ON, Canada; 23Children’s Hospital of Eastern Ontario and Ottawa General Hospital, Ottawa, ON, Canada; 24Kingston General Hospital, Kingston, ON, Canada; 25Jewish General Hospital, Montreal, QC, Canada; 26Hopital Sainte-Justine, Montreal, QC, Canada; 27Centre Hospitalier Universitaire de Quebec, Sainte-Foy, QC, Canada; 28Montreal Children’s Hospital, Montreal, QC, Canada; 29Royal Victoria Hospital, Montreal, QC, Canada; 30Centre Hospitalier Universitaire de Sherbrooke, Sherbrooke, QC, Canada; 31Moncton Hospital, Moncton, NB, Canada; 32Dr Everett Chalmers Hospital, Fredericton, NB, Canada; 33Saint John Regional Hospital, Saint John, NB, Canada; 34Janeway Children’s Health and Rehabilitation Centre, St. John’s, NL, Canada; 35IWK Health Centre, Halifax, NS, Canada; 36Cape Breton Regional Hospital, Sydney, NS, Canada; 37Mount Sinai Hospital, Toronto, ON, Canada.
Rights and permissions
About this article
Cite this article
Soraisham, A., Rabi, Y., Shah, P. et al. Neurodevelopmental outcomes of preterm infants resuscitated with different oxygen concentration at birth. J Perinatol 37, 1141–1147 (2017). https://doi.org/10.1038/jp.2017.83
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.83
- Springer Nature America, Inc.
This article is cited by
-
Oxygen therapy of the newborn from molecular understanding to clinical practice
Pediatric Research (2019)