Abstract
Background:
Hypothermia is a common problem in preterm infants immediately following delivery.
Local problem:
The rate of admission hypothermia in our neonatal intensive care unit (NICU) was above the rate of comparable NICUs in the Vermont Oxford Network.
Methods:
To reduce the rate of preterm admission hypothermia, a quality improvement (QI) project was implemented, utilizing the plan-do-study-act (PDSA) methodology. A guideline for delivery room thermoregulation management in <35-week infants at the University of Virginia was created and put into practice by a multidisciplinary team.
Interventions:
Clinical practice changes in the guideline included: increasing operating room temperatures, obtaining a 10-min axillary temperature, using an exothermic mattress for all infants <35 weeks, and using a polyethylene wrap for infants <32 weeks.
Results:
The baseline rate of hypothermia (<36.5 °CC) was 63%. Three PDSA cycles data were completed on 168 consecutive preterm births. The post-implementation rate of hypothermia (<36.5 °C) was reduced to 30% (P<0.001). The incidence of moderate hypothermia (< 36 °C) was reduced from a baseline of 29% to a rate of 9% (P<0.001).
Conclusion:
Use of a multidisciplinary guideline to increase preterm NICU admission temperatures resulted in a decrease in hypothermic infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Hypothermia is a common occurrence in preterm neonates immediately following delivery that can lead to hypoglycemia, respiratory distress, increased rates of intraventricular hemorrhage and even death.1 Preterm infants are at an increased risk secondary to decreased brown fat, higher skin surface area to weight and relative immaturity and thinness of preterm skin.2, 3 The World Health Organization (WHO) breaks down hypothermia into the following three categories: mild 36.0 to 36.5 °C, moderate 32.0 to 35.9 °C, and severe <32.0 °C. As the severity of hypothermia increases, so do the morbidities and mortalities, with one study showing that, for every 1 °C decrease in admission temperature, mortality increases by 28% and late-onset sepsis by 11%.4 At the University of Virginia, <40% of the infants with a very low birth weight (birth weight <1500 g) in 2013 had a normal admission temperature (36.5 to 37.5 °C), which was well below the Vermont Oxford Network (VON) average. Other large studies have shown similar rates of hypothermia, ranging from 36 to 50% depending on the birth weight and gestational age studied.4, 5, 6
Despite the severity and potential impact of hypothermia on preterm infants, recommendations for standard thermoregulation techniques in the delivery room may not be uniformly followed. The Sixth edition of the Neonatal Resuscitation Program recommended to maintain delivery room temperatures 25 to 26 °C, preheat the radiant warmer, place a portable warmer pad under layers of towels and use a polyethylene plastic wrap for babies delivered at <29 weeks’ gestation.7 The WHO recommends keeping the delivery room set at 25 °C, but this often is lower in the delivery and operating rooms and is adjusted to the comfort of providers and/or the mother.3 However, recent evidence supported by two studies show that if rooms are kept at 25 °C the rates of hypothermia decrease dramatically.5, 8 Radiant warmers and warm blankets are routinely used in most locations, but the secondary methods to promote decreased heat loss continue to be studied. A recent Cochrane review has shown that plastic wraps for infants born <28 weeks decreases the rate of hypothermia; and another study has shown that using a polyurethane bag (PB) for infants up to 36 weeks also reduces the rate of admission hypothermia.9, 10 Exothermic mattresses (EMs) have also been shown to decrease hypothermia in infants <32 weeks.11 Two studies have examined the use of both EMs and PBs with conflicting results. One showed significantly decreased rates of hypothermia, while the other produced significantly increased rates of hyperthermia in the <31 week population.12, 13
Although the evidence of how best to provide optimal thermoregulation for preterm infants in the first few minutes after birth remains controversial, it is clear from the published studies that focusing on the problem and developing a guideline promotes decreased hypothermia. Given our 2013 rate of very low birth weight admission temperatures falling below the 25th percentile of the VON centers, we developed the following problem statement: Preterm very low birth weight newborns at the University of Virginia have a normal admission temperature <40% of the time, well below national benchmarks and potentially contributing to increased morbidity and mortality for these infants. To address this problem, a multidisciplinary team, including nurses, managers, neonatal nurse practitioners and physicians, from both neonatology, obstetrics and maternal fetal medicine was organized. The target population included all preterm neonates <35 weeks as all of these infants are admitted to the University of Virginia Neonatal Intensive Care Unit (NICU). The specific aim for our quality improvement (QI) project was to increase the rate of normal admission temperatures to >60% for preterm infants <35 weeks at the University of Virginia by December 2015 without increasing the rates of hyperthermia. Our plan to accomplish this aim was to utilize the plan–do–study–act (PDSA) methodology of QI.
Methods
Setting
The University of Virginia Children’s Hospital NICU is a 51-bed unit with approximately 200 <35 week admissions per year. All babies born <35 weeks are admitted to the NICU. The labor and delivery unit as well as the cesarean section (C-section) operating rooms are located one floor above the NICU. Infants are resuscitated in either the operating room suite or the delivery room, depending on the method of delivery, and transported to the NICU when stabilized (about 15 to 20 min after birth). Standard of care during this project was to perform 30 to 60 s of delayed cord clamping or cord milking. Prior to initiation of this project, the resuscitation was directed by the fellow or attending physician and the methodology used for those babies born <27 weeks was standardized (EM+PB); however, for infants ⩾27 weeks there was no standardized thermoregulation method. Timing of admission temperature recording prior to this project varied from checking in the transport incubator to within 10 min following transition to NICU incubator.
Intervention
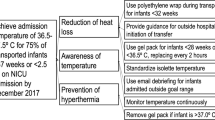
Prior to establishing the intervention, data on the previous 168 infants born <35 weeks was gathered and broken down by gestational age groups and delivery method (Table 1). This data was then presented at the first multidisciplinary meeting where the problem statement and smart aim of the project were developed. The first step of the QI project was to observe a series of preterm deliveries to assess areas for improvement. Any member of the team not actively involved in the resuscitation performed these observations. Following 22 observations, the multidisciplinary team met again to determine the major issues needing to be addressed. The primary issues were noted and plans to address them based on a thorough review of the literature were developed (Table 2). These plans were incorporated into a guideline that was posted throughout the NICU, in each C-section room and attached to each clipboard present at all <35 week deliveries for documentation. The admission temperature was standardized to be the temperature of the infant on arrival to the NICU while still in the transport incubator. The timing of this admission temperature varied dependent on the resuscitation required in the delivery room but was generally around 20 min—although time of admission temperature was not recorded. Education regarding the guideline was delivered through both team and nursing meetings. This guideline was then revised at each multidisciplinary meeting that occurred every 2 to 3 months. The final revision (after all PDSA cycles) of the guideline can be seen in Figure 1.
Measures/data/analysis
To evaluate the effectiveness of the guideline, the fellow present at each delivery <35 weeks collected the following data: gestational age, type of birth, location of birth, room temperature on arrival to the birthing room, use of EM, use of PB, transport method, 10 min temperature, admission temperature, and whether the guideline was not followed. Following 3 months of deliveries, data were analyzed and PDSA methodology was instituted for guideline changes.
Data analysis was performed using GraphPad Prism (Graph Pad Software; San Diego, CA, USA). T-tests were used for continuous data and Mann–Whitney U-test for continuous data with unknown distributions. Data are presented as mean/s.d. if normally distributed and median/interquartile range if distribution was unknown. A statistical process chart or ‘run chart’ was created for admission temperatures. An X bar R chart was used with a sample size of 7 admission temperatures, an A2 of 0.419, D3 of 0.08 and D4 of 1.924.
Ethical considerations
This project was approved by the University of Virginia institutional review board as a QI project and exempt from the need for informed consent.
Results
A series of 22 consecutive preterm deliveries <35 weeks were observed. Data were accumulated and delivery room temperatures graphed compared with admission temperatures (Figure 2). The median delivery room temperature was 21.9 °C and the median admission temperature was 36.2 °C. This group of patients had a median gestational age of 31 weeks and 82% of the deliveries took place in the operating room. Further analysis revealed a significant correlation between delivery room temperature and admission temperature (r2=0.3, P=0.009). Only 14% of infants had a PB used and 36% had an EM used for thermoregulation.
Using the initial observation data, an initial guideline was developed to address the primary issues of room temperature and inconsistent use of PB and EM for thermoregulation. Additionally, plans were made to check a 10-min axillary temperature as well as standardize the method of transportation to the NICU. The new guideline was distributed to all NICU, obstetric and maternal fetal medicine staff members and educational sessions were held.
Following the application of the initial guideline, 43 infants were observed. Protocol compliance was analyzed and showed that the delivery room temperature was properly set at ⩾22.8 °C 81% of the time. The median admission temperature had increased to 36.5 °C from the preguideline data of 36.3 °C (P<0.001). An EM was used in 91% of deliveries and a PB was used for the <28 week gestational age group 100% of the time and was inappropriately used for one 29 week delivery. A 10 min axillary temperature was taken 77% percent of the time and the median 10 min temperature was 36.7 °C. Given the 0.2 °C decrease in 10 min temperature during transport to admission temperature, the next PDSA cycle involved the increase in transport incubator temperature to 37.5 °C in an effort to maintain the temperature during transport to the NICU.
Cycle 2 data consisted of a total of 59 infants, with 9 deliveries missing room temperature and thermoregulation method information. Protocol compliance showed the delivery room temperature to be maintained ⩾22.8 °C 94% of the time. The median admission temperature had increased to 36.7 °C from the preguideline data of 36.3 °C (P<0.001). An EM was used in 96% of deliveries and a PB was used for the <28 week gestational age group 100% of the time and was inappropriately used for one 32 week delivery. A 10 min axillary temperature was taken 90% of the time and the median 10 min temperature was 36.7 °C. Further subanalysis of the data showed that the 28 to 31 6/7 week gestational age group continued to have significant hypothermia for >40% of admissions. The next PDSA cycle involved the use of PBs during resuscitation for all infants <32 weeks’ gestation. Also, during cycle 2, the number of hyperthermic infants (>37.5 °C) increased from 2% baseline to 8.4% (P=0.053). Although this was not statistically significant, the trend was concerning and two changes were made to the guideline—transport incubators were decreased back to 37 °C, and if the 10 min temperature was >37 °C, the EM was removed prior to transport.
Cycle 3 data consisted of a total of 55 infants. For this subset of infants, no other delivery information was collected other than the admission temperature. The median admission temperature for this cycle was 36.8 °C. The percentage of hyperthermic infants was 9% for this cycle, not statistically different than cycle 2 or the baseline group (P=0.12). The percentage of 28 to 31 6/7 week gestational age infants who were hypothermic decreased to 25% from 40% in cycle 2.
The complete data set consisted of 168 babies (10 months) in the group prior to starting the QI project and a total of 157 babies (9 months) in the three PDSA cycles. All of the infants born <35 weeks were included in the results for the study period and no babies were excluded. Figure 3 displays the entirety of both the pre-QI data and the PDSA cycles in a X Bar R run chart. No significant clinical associations were tracked during the project. The X bar chart shows that the mean sample temperature increased significantly following the institution of the QI project. When evaluating Figure 3 for special causes, there were no significant findings. The R bar chart shows that in the pre-QI data the process is out of control as one point falls outside of the upper control limits. During the PDSA cycles, there is less variation of admission temperatures with no significant special causes indicating that the process is in control. Additionally, each PDSA cycle had significantly improved admission temperatures compared with baseline (Table 3). When evaluating hypothermic and moderately hypothermic infants, there was a significant reduction in the number of infants in those groups after initiation of the PDSA cycles compared with baseline (Table 4). Although there was not a statistically significant increase, there was a trend towards an increased number of infants who were hyperthermic on admission.
Discussion
The implementation of a multidisciplinary guideline aimed at improving admission temperatures in neonates <35 weeks resulted in decreased rates of hypothermia, moderate hypothermia and resulted in no significant increase in rates of hyperthermia. By observing a small subset of deliveries and resuscitations prior to developing a guideline, we were able to focus on the factors most likely associated with hypothermia: delivery room temperatures, inconsistent use of supplemental thermoregulation methods, and lack of temperature monitoring in the delivery room. The use of multiple PDSA cycles at 3 month intervals and changes to the guideline allowed incremental improvements over a short time period. Multidisciplinary involvement in the project and particularly buy-in from nursing staff resulted in quick changes that were implemented in a short period of time and focused on issues vital to patient safety and optimal outcomes. By instituting a standard method of focusing on thermoregulation, we were able to reduce the rates of moderate hypothermia to <10%, in the lowest quartile of the 2015 VON data.
Several previous studies have reported on the use of QI projects to decrease the rates of hypothermia in different subsets of the preterm population.12, 14, 15 Manani et al.15 focused on a similar subset of patients, those <33 weeks, and used the same PDSA methodology. They found a similar set of problems based on an observation period, primarily the lack of close monitoring of temperature after the initial assessment, no standard of use for thermal equipment and room temperatures that were frequently <20 °C. To address these issues, they developed a standard of care that addressed the same issues as our QI project: room temperature, use of chemical warmer mattress, use of polyethylene bag, and monitoring of axillary temperatures. They used a definition of hypothermia as <36 °C and were able to reduce their rate from 44% to 0% over the course of 3 years. They similarly showed no increase in hyperthermia. DeMauro et al.14 also instituted the same changes but in a population with a birth weight <1250 g. They found similar improvement in median admission temperature as our study, an increase from 36.4 to 36.7 °C. Our three studies combined show that with >400 infants, a guideline designed to focus on delivery room temperature, standardized use of EMs and PBs and close attention to infants’ temperature in the delivery room results in significant reduction in rates of moderate hypothermia without increasing rates of hyperthermia.
Russo et al.12 similarly performed a multidisciplinary QI project in neonates <35 weeks aimed at reducing the rates of moderate hypothermia. Their plan also included standardizing the use of an EM and PB; however, their guideline suggested using the PB in all infants <35 weeks while our guideline suggested its use in those <32 weeks. They showed a similar decrease in rates of moderate hypothermia, 55% to 6.2%, while we showed a decrease from 29% to 9%. They were also able to show a decrease in rates of intubation at 24 h, from 39% to 17.6%, data that were not collected in our project. They had similar rates of compliance, up to 88% at full implementation, which was similar to the rates in this study of 90%. However, a recent study has suggested that the combination use of a PB and EM results in increased rates of hyperthermia.13 They found that the combined use of PB and EM in those infants <31 weeks resulted in an increased rate of hyperthermia from 17% to 46%. In our study, we saw a trend toward increased rates of hyperthermia (2% to 7%, P=0.06). This trend was apparent at cycle 2 and steps were taken to decrease the temperature of the transport incubator and remove the EM if the 10 min temperature was >37 °C. These steps resulted in a stable rate of hyperthermia for cycle 3 but no clear reduction in the number of hyperthermic infants. Clearly, close monitoring of axillary temperatures is required when combining both forms of thermoregulation in this vulnerable population to avoid hyperthermia.
Our study is not the first to show that the delivery room temperature correlates strongly to admission temperature. In 2014, de Almeida et al.5 showed that, in neonates <33 weeks, a delivery room temperature <25 °C was associated with admission hypothermia. They also showed that admission temperature <36 °C was associated with an increased risk of early neonatal death by 1.64 fold. Jia et al.8 in 2013 compared the admission temperatures of babies <32 weeks and found that 35% of those born in a room set to 24 to 26 °C had hypothermia compared with 69% of those born in a room set to 20 to 23 °C. During the planning phase of our study, the multidisciplinary aspect allowed us to present these previous studies regarding delivery room temperatures and neonatal outcomes to the obstetric staff and resulted in productive discussions on how to raise the room temperature while keeping the obstetric staff comfortable. Ultimately, owing to hospital operating room policy, we were not able to raise the room temperatures to the WHO recommendation of 25 °C but were able to raise them to 22.8 °C (73 °F—a temperature the obstetric staff also deemed comfortable and was significantly higher than our previous room temperatures). Given our data and several recent publications, the WHO recommendation of increasing delivery room temperatures is an easy and effective first step toward reducing rates of hypothermia.
Finally, although we did not collect data on the major morbidities associated with prematurity in our QI project, several previous publications have shown an association of moderate hypothermia with increased rates of morbidities. The largest review to date that analyzed >9000 infants born <33 weeks in Canada looked at the association of admission temperatures with adverse outcomes.6 After adjusting for infant and maternal data, they found that the rate of composite outcome was the lowest at an admission temperature of 36.8 °C or a range of 36.5 to 37.2 °C. Again, this emphasizes the need to monitor temperatures closely in the delivery room as both hypothermia and hyperthermia are associated with worse outcomes.
This QI study has several limitations. First, the results may not be generalizable to other populations as the delivery circumstances at other centers are unique and need to be accounted for when designing a thermoregulation guideline. Second, we did not track compliance rates during the third cycle to show a consistent improvement in application of the guideline. Finally, as with all QI projects, it will be important to continue to track admission temperatures to monitor for sustained improvement to determine the need for re-education.
In conclusion, the development of a multidisciplinary guideline aimed at improving admission temperatures in preterm infants <35 weeks significantly decreased the rates of hypothermia and moderate hypothermia on admission. By using multiple PDSA cycles, we were able to quickly adapt our guideline to develop the best approach for thermoregulation immediately following delivery at our center. The major areas addressed by our guideline were delivery room temperature and standardization of the use of EM and PB, as well as close monitoring of the infant’s temperature in the delivery room. Our guideline now aligns with the recent publication of the Neonatal Resuscitation Program’s new thermoregulation guidelines: maintain delivery room temperatures 23 to 25 °C and for infants <32 weeks use a plastic bag, hat and thermoregulation mattress.16 Our study does show that caution is needed to avoid hyperthermia when using multiple forms of thermoregulation as our rates of hyperthermia trended higher and near statistical significance. A randomized clinical trial to further evaluate the possibility of increased hyperthermia with multiple warming modalities is indicated.
References
Miller SS, Lee HC, Gould JB . Hypothermia in very low birth weight infants: distribution, risk factors and outcomes. J Perinatol 2011; 31 (Suppl 1 (S1): S49–S56.
Ringer SA . Core concepts: thermoregulation in the newborn part I: basic mechanisms. Neoreviews 2013; 14 (4): e161–e167.
Ringer SA . Core concepts: thermoregulation in the newborn, part II: prevention of aberrant body temperature. Neoreviews 2013; 14 (5): e221–e226.
Laptook AR, Salhab W, Bhaskar B . Admission temperature of low birth weight infants: predictors and associated morbidities. Pediatrics 2007; 119 (3): e643–e649.
de Almeida MFB, Guinsburg R, Sancho GA, Rosa IRM, Lamy ZC, Martinez FE et al. Hypothermia and early neonatal mortality in preterm infants. J Pediatr 2014; 164 (2): 271–5.e1.
Lyu Y, Shah PS, Ye XY, Warre R, Piedboeuf B, Deshpandey A et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks’ gestation. JAMA Pediatr 2015; 169 (4): e150277.
Zaichkin J, Kattwinkel J, McGowan J . American Heart Association, American Academy of Pediatrics Textbook of Neonatal Resuscitation,6th edn. American Academy of Pediatrics: Elk Grove Village, IL,2011.
Jia Y-S, Lin Z-L, Lv H, Li Y-M, Green R, Lin J . Effect of delivery room temperature on the admission temperature of premature infants: a randomized controlled trial. J Perinatol 2013; 33 (4): 264–267.
McCall EM, Alderdice F, Halliday HL, Jenkins JG, Vohra S . Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane database Syst Rev 2010; 17 (3): CD004210.
Leadford AE, Warren JB, Manasyan A, Chomba E, Salas AA, Schelonka R et al. Plastic bags for prevention of hypothermia in preterm and low birth weight infants. Pediatrics 2013; 132 (1): e128–e134.
Chawla S, Amaram A, Gopal SP, Natarajan G . Safety and efficacy of Trans-warmer mattress for preterm neonates: results of a randomized controlled trial. J Perinatol 2011; 31 (12): 780–784.
Russo A, McCready M, Torres L, Theuriere C, Venturini S, Spaiǵht M et al. Reducing hypothermia in preterm infants following delivery. Pediatrics 2014; 133 (4): e1055–e1062.
McCarthy LK, Molloy EJ, Twomey AR, Murphy JFA, O’Donnell CPF . A randomized trial of exothermic mattresses for preterm newborns in polyethylene bags. Pediatrics 2013; 132 (1): e135–e141.
DeMauro SB, Douglas E, Karp K, Schmidt B, Patel J, Kronberger A et al. Improving delivery room management for very preterm infants. Pediatrics 2013; 132 (4): e1018–e1025.
Manani M, Jegatheesan P, DeSandre G, Song D, Showalter L, Govindaswami B . Elimination of admission hypothermia in preterm very low-birth-weight infants by standardization of delivery room management. Perm J 2013; 17 (3): 8–13.
Weiner GM, Zaichkin J, Kattwinkel J,American Academy of Pediatrics, American Heart AssociationTextbook of neonatal resuscitation, 7th Edition.American Academy of Pediatrics: Elk Grove Village, IL, 2016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Harer, M., Vergales, B., Cady, T. et al. Implementation of a multidisciplinary guideline improves preterm infant admission temperatures. J Perinatol 37, 1242–1247 (2017). https://doi.org/10.1038/jp.2017.112
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.112
- Springer Nature America, Inc.