Abstract
Objective:
Neonates with Down’s syndrome (nDS) may have multiple medical issues that place them at increased risk for mortality during the newborn period. Goal of this study was to determine if there are differences in baseline characteristics, medical complications or procedures performed during hospitalization between nDS who survived versus those who died during initial hospitalization.
Study Design:
Data from 2000 to 2014 were reviewed using the Pediatric Health Information Systems (PHIS) database on all DS patients admitted to the hospital <30 days postnatal life. Baseline demographics, medical complications, procedures performed and mortality were recorded. Patients were divided into nDS patients who were discharged alive (nDS-a) versus nDS patients who died (nDS-d). Multivariate logistic analysis with odds ratios was performed to determine significant predictors of death. A P<0.05 was considered significant.
Results:
A total of 5737 nDS were evaluated. Overall mortality was 7.5% (431/5737). nDS-d were more likely than nDS-a to have a lower birth weight (1.0 (0.9 to 1.0)), presence of a diaphragmatic hernia (6.9 (1.9 to 25.1), or a cardiac diagnosis of a pulmonary venous abnormality (6.8 (1.9 to 24.4)), Ebstein’s anomaly (3.2 (1.2 to 8.5)) or left-sided obstructive lesion (2.0 (1.3 to 3.0). nDS-d were more likely to develop hydrops (5.7 (3.5 to 9.5)) and necrotizing enterocolitis (1.7 (1.2 to 2.6)). In addition, nDS-d had significantly higher odds of requiring mechanical ventilation (20.7 (9.9 to 43.1)) or extracorporeal membrane oxygenation (8.7 (4.7 to 16.1)).
Conclusions:
A number of characteristics, specifically certain cardiac diagnosis, place nDS at increased risk for mortality. Furthermore, development of specific medical complications or need for particular procedures increases the odds for mortality in nDS. Caregivers should be cognizant that they are taking care of a high-risk population nDS with an increased risk for mortality if these variables are present.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Down’s syndrome (DS) is the most viable and common of all the human trisomic syndromes.1 DS occurs in ~1 in 733 live births in the United States. Patients with DS have an increased risk for multiple congenital abnormalities.2, 3, 4, 5 In addition, neonates with DS (nDS) may be at an increased risk for physiologic abnormalities. This may especially be true when dealing with delayed extrauterine pulmonary vascular adaptation manifesting as persistent pulmonary hypertension of the newborn in nDS.6, 7 All these abnormalities may place nDS at increased risk for mortality during the newborn period.
Previous studies have investigated possible risk factors for mortality in the nDS population. These risk factors include, but are not limited to, ethnicity, prematurity, birth weight and presence of cardiac disease.8, 9, 10, 11, 12 In addition, development of medical complications or procedural variables during initial hospitalization has been associated with increased mortality in this population.13, 14, 15 Limited data exist in evaluating all these variables together to determine overall risk factors for mortality in this complex population.
The goal of this study was to determine whether there are differences in baseline characteristics, development of medical complications or procedures performed during hospitalization between nDS who survived (nDS-a) versus those who died (nDS-d) during their initial hospitalization.
Methods
This retrospective study involved data from the Pediatric Health Information Systems (PHIS) database of the Child Health Corporation of America (Shawnee Mission, KS) using de-identified information. Institutional Review Board (IRB) determined that this study did not fit the definition of human subjects research under 45 CFR part 46.102(f); therefore, IRB evaluation was waived.
PHIS database contains administrative, billing and record-review data, including patient demographics (for example, gender, birth weight and gestational age) as recorded in the patient chart, diagnoses, medications and procedures, from 43 freestanding US children’s hospitals, which account for 85% of all national freestanding children’s hospitals. To certify comparability of charge-level data among institutions, including medications and procedures, Thompson-Reuters Healthcare (Ann Arbor, MI, USA), the PHIS data processing partner, mapped each hospital’s daily charge codes to a common classification system, the Clinical Transaction Classification (CTC) codes.
International Classification of Diseases, Ninth Edition diagnostic codes were used for identification purposes. The database was queried for all unique patients <30 days of age with the diagnosis of DS admitted to a children’s hospital participating in the PHIS database from the time period 2000 to 2014. Patients with additional chromosomal abnormalities in addition to DS were excluded.
Antenatal, perinatal and postnatal demographic data were recorded. Subsequent medical diagnosis/complications and procedural variables during hospitalization were also documented. Furthermore, overall mortality for nDS population studies was detailed.
Continuous variables are presented as means and s.d.’s, and dichotomous/categorical measures are presented as ‘n’s’. Univariate analysis examined differences between the groups using t-tests for continuous measures and χ2 tests with Fisher’s exact tests for categorical measures due to small cell sizes. All codes that were recorded for <10 patients were eliminated from analysis. Multivariate logistic analysis with odds ratios was performed to determine significant predictors of death. P<0.05 was considered significant. Statistics were performed using Stata S.E. 13.0 (Stata Corporation, College Station, TX, USA).
Results
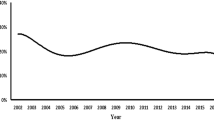
A total of 5737 nDS patients (2505 males: 3210 females) were admitted to a hospital participating in the PHIS database between 2000 and 2014. Gestational age was 36.8+2.8 weeks, and birth weight was 2.7+0.8 kg. Median admit age was 1 day (0 to 30 days) and median length of hospitalization was 18 days (1 to 582 days). Overall mortality was 7.5% (431/5737).
On univariate analysis, nDS-d were more likely to have oligohydramnios (21.7%) versus to not have oligohydramnios (7.4%). nDS-d had a significantly lower gestational age and birth weight than nDS-a. nDS-d were also admitted significantly earlier to the hospital than nDS-a cohort. nDS-d had a significantly longer hospital stay than the nDS-a had (38.0±52.0 days vs 28.6±34.7 days, respectively). There were no other significant differences between the two groups in perinatal factors (Table 1).
When evaluating baseline demographics, white race was significantly less common in the nDS-d (6.2%) versus all the other races combined (10.5%). nDS-d was more common in the ‘Other’ race category (11.0%) versus all the races combined (6.7%). There was a trend for nDS-d to be black (10.7%) versus all other races combined (6.9%) (P=0.06). nDS-d were less common in the New England region (3.9%) versus all other regions combined (7.7%), but more common in the Mountain region (11.4%) versus other regions combined (7.3%). nDS-d were less likely to have commercial insurance (6.4%) versus other payment codes (8.0%) and more likely to have a Medicaid code (8.8%) versus other payment codes (6.5%). No other significant differences between the two groups in baseline demographics were noted (Table 2).
From a cardiac standpoint, nDS-d were significantly more likely than not to have the diagnosis of complete transposition of the great vessels (37.5 vs 7.5%, respectively), double outlet right ventricle (17.7 vs 7.4%, respectively), Ebstein’s anomaly (29.4 vs 7.4%, respectively), left-sided obstructive lesion (14.9 vs 6.9%), or pulmonary venous abnormality (26.1 vs 7.5%, respectively). There were no other differences in cardiac diagnosis noted between the two groups (Table 3).
nDS-d were more likely to have the medical diagnosis of anomalies of the diaphragm (39.4 vs 7.4%, respectively), but less likely to have the diagnosis of atresia or stenosis of the small intestine (4.4 vs 8.1%, respectively) or Hirschsprung’s disease (2.3 vs 7.9%, respectively) than not have these medical conditions. In addition, nDS-d were more likely to develop hydrops (51.6 vs 6.3%, respectively), intraventricular hemorrhage (IVH) grade I (24.1 vs 7.3%, respectively), IVH grade II (29.6 vs 7.4%, respectively), IVH grade III (36.4 vs 7.5%, respectively), IVH grade IV (66.7 vs 7.4%, respectively) and necrotizing enterocolitis (15.5 vs 7.0%, respectively). Furthermore, nDS-d were more likely to undergo extracorporeal membrane oxygenation (46.6 vs 6.6%, respectively), mechanical ventilation (14.3 vs 0.5%, respectively), or require total parental nutrition (10.3 vs 3.0%, respectively; Table 4).
Table 5 presents the odds ratios and confidence intervals for the multivariate logistic regression analysis. All variables with adequate cases and not multi-collinear with the predictor measures were included. Neonates with lower birth weight or lower age at admission had higher odds of death. There was a trend for higher odds of death if neonates had a gestational age less than 34 weeks (3.56 (0.82 to 15.43), P<0.1), but no such findings were manifested with higher gestational ages. Shorter length of hospitalization had a decreased risk for death. All of the baseline demographics that were significant with univariate analysis were no longer significant with multivariate analysis. Presence of the cardiac diagnosis of Ebstein’s anomaly, left-sided obstructive lesions, or pulmonary venous abnormality increased the odds of death. Anomalies of the diaphragm also increased the odds of death; however, there was less risk for death if atresia or stenosis of the small intestine or Hirschsprung’s disease occurred. Finally, development of hydrops or necrotizing enterocolitis or requiring extracorporeal membrane oxygenation or mechanical ventilation also increased the odds of death in this patient population.
Discussion
nDS patients are at increased risk for mortality compared with that in the general population. Previous studies have evaluated differences between nDS-a and nDS-d cohorts and possible risk factors for death in this population.8, 9, 10, 11, 12, 14, 16 This study identified certain perinatal factors, specific cardiac diagnosis, other medical conditions, complications and procedures that may place this population at risk for mortality that has not been previously analyzed.
Analogous to previous studies, perinatal factors that were significantly different between the nDS-a and NDS-d included gestational age and birth weight with univariate analysis.9, 10, 12, 14, 17 In addition, presence of oligohydramnios and older age at admission was more prevalent in the n-DSd. However, on multivariate analysis, only lower birth weight and younger age were risk factors for mortality. The lower birth weight may signify that these patients are more vulnerable to mortality. The younger age admission for the nDS-d is not necessarily surprising, as the nDS-d group would likely have presented earlier with clinical deterioration such as respiratory distress requiring transfer to a children’s hospital for further treatment, whereas the nDS-a group would have been transferred for non-urgent reasons. Gestational age was not significantly associated with mortality, though there was a trend for increased risk for mortality for those infants born less than 34 weeks gestation, which is similar to a recent article.12 It appears in this study that gestational age, though important, is superseded by other risk factors for mortality.
There were racial differences between the two groups with nDS white race having improved survival and nDS ‘other’ having worse survival, but these variables were no longer significant in the multivariate analysis. Previous studies have noted worse outcomes on nDS infants that were identified as Hispanic or black;9, 11, 14, 17 however, those studies involved an earlier time period and spanned a longer time interval. It was noted in at least one study that survival improved and racial disparities narrowed in nDs during the more recent time period evaluated versus the earlier time periods.9 The time interval examined in this study is recent and it may hopefully be that racial disparities have continued to improve over time. There were also differences in payment codes between the two groups with commercial insurance payers having improved survival and medicare/Medicaid payers having worse survival on univariate analysis. These payment codes may signify socioeconomic status and possibly access to advanced care that may improve outcomes in the immediate postnatal period. This may be less of an issue since PHIS data arises from tertiary pediatric centers. That said, these variables were not significant on multivariate analysis. Again, this may possibly be due to improvements in care over time that make these variables less important.
One demographic variable that was different between the two groups was that nDS-d were more likely to live in the mountain region of the United States compared with all the other regions combined. High altitude, in general, is a possible risk factor for respiratory issues such as pulmonary hypertension in infants and children with and without DS.18, 19, 20, 21, 22 Previous reports have also documented an increased risk for persistent pulmonary hypertension in nDS patients that may be intrinsic to them.6, 7, 23 Combining these two factors may conceivably explain the higher incidence of nDS-d in this region likely due to respiratory compromise. The lower incidence of nDS-d in the New England region was unexpected, and no specific explanation at this time can be made. Regardless, all these baseline demographic variables were no longer risk factors with multivariate analysis.
Previous studies have noted that nDS have an increased risk for death if there is a presence of a congenital heart disease,9, 10, 11, 14, 17 yet this is a very broad category in this population. These previous studies did not specify a specific congenital heart disease that placed this population at risk. There is an approximately 50% incidence of congenital heart disease in the DS population.4 In general, cardiac defects in the DS population do not require neonatal surgery with the most common lesions of atrioventricular septal defects and ventricular septal defects being repaired outside of the neonatal time period. On multivariate analysis, only three congenital heart defects were noted to be more prevalent in the nDS-d group: Ebstein’s anomaly,24 left-sided obstructive lesions and pulmonary venous abnormalities. These lesions have a spectrum of severity such that some of these defects may present with significant cardiac compromise that may require neonatal cardiac intervention. Again, PHIS data do not document the severity of the cardiac diagnosis or the cause of death, but it is not unreasonable to assume that these three lesions were significant enough to cause some cardiac compromise, eventually leading to death. The other cardiac defects evaluated are less likely to cause neonatal compromise, regardless of their severity and thus less likely to be a risk factor for mortality.
nDS-d patients had a higher incidence of diaphragmatic hernias compared with the nDS-a patients. It was not surprising that diaphragmatic hernias were more prevalent in the nDS-d. Mortality in neonates with congenital diaphragmatic hernias is high in general.25 There was no reason to believe that a DS diagnosis would be protective. Conversely, Hirschsprung’s disease and atresia/stenosis of the small intestine was lower in the nDS-d patients. There is a significantly increased risk for both diseases in DS patients versus non-DS patients;2, 26, 27, 28, 29 however, significant morbidity such as death for these corrective procedures is extremely low to non-existent.26, 30, 31 This likely explains the finding that these diseases were more prevalent in the nDS-d group as it is unlikely that they would have died after their surgical correction.
The development of hydrops or NEC was also noted to increase the odds of death in this population. Again, it was not necessarily unforeseen that hydrops was more prevalent in the nDS-d group. The finding of hydrops likely just represented the overall unwell status of these patients who died. The presence of NEC likewise has been described previously as being more prevalent in nDS-d compared with other groups.14 Mortality for neonates who develop NEC is relatively high, and the presence of DS would only likely increase this risk.32, 33 Furthermore, the need for mechanical ventilation or extracorporeal membrane oxygenation inferred greater odds of death in this population. Once more, these forms of support merely represent the general illness of the nDS patient likely due to multiple medical conditions previously described.2, 4, 7, 8, 13, 14, 34
There are multiple limitations to this study. First, this was a retrospective study with all the inherent shortcomings of such a design. Data were limited by what was available via the PHIS database, which includes only children’s hospitals. As these hospitals are usually not birth hospitals, nDS patients were presumably transferred for specialized care, thus not all nDS patients would be represented in this data set. Severity of medical conditions could not be ascertained. In addition, medical conditions are not able to be temporally related to mortality, thus cause and effect cannot be determined. As clinical information is primarily from ICD-9 codes, nonbillable data are likely to not be recorded. PHIS has a robust quality control procedure; however, we cannot verify that diagnosis was made and coded in a similar way across hospitals. The risk factors noted are somewhat intuitive. This study, however, did not specifically evaluate whether the presence of DS itself increased the risk for overall morbidity or mortality compared with those neonates without DS when controlling for other baseline variables. Only further analysis of large databases will be able to answer that question.
In conclusion, there are baseline characteristics, including specific cardiac diagnosis, which place nDS at increased risk for mortality. Furthermore, development of specific medical complications or need for particular procedures increases the odds for mortality in nDS. Caregivers should be cognizant that they are taking care of a high-risk population with an increased risk for mortality if these variables are present.
References
Canfield MA, Honein MA, Yuskiv N, Xing J, Mai CT, Collins JS et al. National estimates and race/ethnic-specific variation of selected birth defects in the United States, 1999-2001. Birth Defects Res A Clin Mol Teratol 2006; 76 (11): 747–756.
Freeman SB, Torfs CP, Romitti PA, Royle MH, Druschel C, Hobbs CA et al. Congenital gastrointestinal defects in Down syndrome: a report from the Atlanta and National Down Syndrome Projects. Clin Genet 2009; 75 (2): 180–184.
Weijerman ME, de Winter JP . Clinical practice. The care of children with Down syndrome. Eur J Pediatr 2010; 169 (12): 1445–1452.
Freeman SB, Taft LF, Dooley KJ, Allran K, Sherman SL, Hassold TJ et al. Population-based study of congenital heart defects in Down syndrome. Am J Med Genet 1998; 80 (3): 213–217.
Zachor DA, Mroczek-Musulman E, Brown P . Prevalence of celiac disease in Down syndrome in the United States. J Pediatr Gastroenterol Nutr 2000; 31 (3): 275–279.
Cua CL, Blankenship A, North AL, Hayes J, Nelin LD . Increased incidence of idiopathic persistent pulmonary hypertension in Down syndrome neonates. Pediatr Cardiol 2007; 28 (4): 250–254.
Weijerman ME, van Furth AM, van der Mooren MD, van Weissenbruch MM, Rammeloo L, Broers CJ et al. Prevalence of congenital heart defects and persistent pulmonary hypertension of the neonate with Down syndrome. Eur J Pediatr 2010; 169 (10): 1195–1199.
Weijerman ME, van Furth AM, Vonk Noordegraaf A, van Wouwe JP, Broers CJ, Gemke RJ . Prevalence, neonatal characteristics, and first-year mortality of Down syndrome: a national study. J Pediatr 2008; 152 (1): 15–19.
Kucik JE, Shin M, Siffel C, Marengo L, Correa A . Trends in survival among children with Down syndrome in 10 regions of the United States. Pediatrics 2013; 131 (1): e27–e36.
Goldman SE, Urbano RC, Hodapp RM . Determining the amount, timing and causes of mortality among infants with Down syndrome. J Intellect Disabil Res 2011; 55 (1): 85–94.
Shin M, Kucik JE, Correa A . Causes of death and case fatality rates among infants with down syndrome in metropolitan Atlanta. Birth Defects Res A Clin Mol Teratol 2007; 79 (11): 775–780.
Sparks TN, Griffin E, Page J, Pilliod R, Shaffer BL, Caughey AB . Down syndrome: perinatal mortality risks with each additional week of expectant management. Prenat Diagn 2016; 36 (4): 368–374.
Backes CH, Nicholson L, Rivera BK, Swier N, Marshall W, Cua CL . Extracorporeal membrane oxygenation incidence, characteristics, and outcomes in neonatal down syndrome patients. ASAIO J 2016; 62 (4): 477–481.
Boghossian NS, Hansen NI, Bell EF, Stoll BJ, Murray JC, Laptook AR et al. Survival and morbidity outcomes for very low birth weight infants with Down syndrome. Pediatrics 2010; 126 (6): 1132–1140.
Cashen K, Thiagarajan RR, Collins JW Jr, Rycus PT, Backer CL, Reynolds M et al. Extracorporeal membrane oxygenation in pediatric trisomy 21: 30 years of experience from the extracorporeal life support organization registry. J Pediatr 2015; 167 (2): 403–408.
Frid C, Drott P, Otterblad Olausson P, Sundelin C, Anneren G . Maternal and neonatal factors and mortality in children with Down syndrome born in 1973-1980 and 1995-1998. Acta Paediatr 2004; 93 (1): 106–112.
Rasmussen SA, Wong LY, Correa A, Gambrell D, Friedman JM . Survival in infants with Down syndrome, Metropolitan Atlanta, 1979-1998. J Pediatr 2006; 148 (6): 806–812.
de Meer K, Heymans HS, Zijlstra WG . Physical adaptation of children to life at high altitude. Eur J Pediatr 1995; 154 (4): 263–272.
Durmowicz AG . Pulmonary edema in 6 children with Down syndrome during travel to moderate altitudes. Pediatrics 2001; 108 (2): 443–447.
Jensen KM, Sevick CJ, Seewald LA, Halbower AC, Davis MM, McCabe ER et al. Greater risk of hospitalization in children with Down syndrome and OSA at higher elevation. Chest 2015; 147 (5): 1344–1351.
Niermeyer S, Andrade Mollinedo P, Huicho L . Child health and living at high altitude. Arch Dis Child 2009; 94 (10): 806–811.
Niermeyer S, Shaffer EM, Thilo E, Corbin C, Moore LG . Arterial oxygenation and pulmonary arterial pressure in healthy neonates and infants at high altitude. J Pediatr 1993; 123 (5): 767–772.
Cua CL, Rogers LK, Chicoine LG, Augustine M, Jin Y, Nash PL et al. Down syndrome patients with pulmonary hypertension have elevated plasma levels of asymmetric dimethylarginine. Eur J Pediatr 2011; 170 (7): 859–863.
Freud LR, Escobar-Diaz MC, Kalish BT, Komarlu R, Puchalski MD, Jaeggi ET et al. Outcomes and predictors of perinatal mortality in fetuses with ebstein anomaly or tricuspid valve dysplasia in the current era: a multicenter study. Circulation 2015; 132 (6): 481–489.
Hagadorn JI, Brownell EA, Herbst KW, Trzaski JM, Neff S, Campbell BT . Trends in treatment and in-hospital mortality for neonates with congenital diaphragmatic hernia. J Perinatol 2015; 35 (9): 748–754.
Choudhry MS, Rahman N, Boyd P, Lakhoo K . Duodenal atresia: associated anomalies, prenatal diagnosis and outcome. Pediatr Surg Int 2009; 25 (8): 727–730.
Friedmacher F, Puri P . Hirschsprung's disease associated with Down syndrome: a meta-analysis of incidence, functional outcomes and mortality. Pediatr Surg Int 2013; 29 (9): 937–946.
Kallen B, Mastroiacovo P, Robert E . Major congenital malformations in Down syndrome. Am J Med Genet 1996; 65 (2): 160–166.
Best KE, Addor MC, Arriola L, Balku E, Barisic I, Bianchi F et al. Hirschsprung's disease prevalence in Europe: a register based study. Birth Defects Res A Clin Mol Teratol 2014; 100 (9): 695–702.
Mustafawi AR, Hassan ME . Congenital duodenal obstruction in children: a decade's experience. Eur J Pediatr Surg 2008; 18 (2): 93–97.
Suita S, Taguchi T, Ieiri S, Nakatsuji T . Hirschsprung's disease in Japan: analysis of 3852 patients based on a nationwide survey in 30 years. J Pediatr Surg 2005; 40 (1): 197–201.
Kessler U, Schulte F, Cholewa D, Nelle M, Schaefer SC, Klimek PM et al. Outcome in neonates with necrotizing enterocolitis and patent ductus arteriosus. World J Pediatr 2016; 12 (1): 55–59.
Knott EM, Gasior A St, Peter S, Snyder C . Mortality of necrotizing enterocolitis and isolated ileal perforation at a single institution over the past 40 years. Eur J Pediatr Surg 2014; 24 (5): 394–397.
Southgate WM, Annibale DJ, Hulsey TC, Purohit DM . International experience with trisomy 21 infants placed on extracorporeal membrane oxygenation. Pediatrics 2001; 107 (3): 549–552.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cua, C., Haque, U., Santoro, S. et al. Differences in mortality characteristics in neonates with Down’s syndrome. J Perinatol 37, 427–431 (2017). https://doi.org/10.1038/jp.2016.246
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.246
- Springer Nature America, Inc.
This article is cited by
-
Congenital heart disease in Down syndrome – A review of temporal changes
Journal of Congenital Cardiology (2021)
-
Impact of prenatal screening on congenital heart defects in neonates with Down syndrome in the US
Pediatric Research (2021)
-
Usefulness of Postnatal Echocardiography in Patients with Down Syndrome with Normal Fetal Echocardiograms
Pediatric Cardiology (2019)