Abstract
Cadmium (Cd) is an environmental pollutant that has been associated with cardiovascular disease in populations, but the relationship of Cd with hypertension has been inconsistent. We studied the association between urinary Cd concentrations, a measure of total body burden, and blood pressure in American Indians, a US population with above national average Cd burden. Urinary Cd was measured using inductively coupled plasma mass spectrometry, and adjusted for urinary creatinine concentration. Among 3714 middle-aged American Indian participants of the Strong Heart Study (mean age 56 years, 41% male, 67% ever-smokers, 23% taking antihypertensive medications), urinary Cd ranged from 0.01 to 78.48 μg g−1 creatinine (geometric mean=0.94 μg g−1) and it was correlated with smoking pack-year among ever-smokers (r2=0.16, P<0.0001). Participants who were smokers were on average light-smokers (mean 10.8 pack-years), and urinary Cd was similarly elevated in light- and never-smokers (geometric means of 0.88 μg g−1 creatinine for both categories). Log-transformed urinary Cd was significantly associated with higher systolic blood pressure in models adjusted for age, sex, geographic area, body mass index, smoking (ever vs never, and cumulative pack-years) and kidney function (mean blood pressure difference by lnCd concentration (β)=1.64, P=0.002). These associations were present among light- and never-smokers (β=2.03, P=0.002, n=2627), although not significant among never-smokers (β=1.22, P=0.18, n=1260). Cd was also associated with diastolic blood pressure among light- and never-smokers (β=0.94, P=0.004). These findings suggest that there is a relationship between Cd body burden and increased blood pressure in American Indians, a population with increased cardiovascular disease risk.
Similar content being viewed by others
Introduction
Hypertension is a common clinical condition contributing substantially to poor health outcomes, including cardiovascular disease (CVD) and mortality.1 Hypertension risk varies by age, sex, lifestyle and behaviors, and increasing evidence suggests that blood pressure is influenced by toxic metal environmental pollutants including cadmium (Cd).2, 3, 4 Experimental evidence associates Cd with endothelial dysfunction, oxidative stress, atherosclerosis, hypertension and kidney dysfunction.5, 6, 7, 8, 9 These data are supported by research demonstrating a relationship between Cd body burden and CVD in populations.9, 10, 11 However, the epidemiology evidence for association of Cd with hypertension has been inconsistent.2, 4, 12, 13, 14, 15, 16, 17, 18, 19 Little research has been carried out in populations with low-to-moderate Cd exposure for associations with increased systolic and diastolic blood pressures. Blood Cd but not urine Cd was associated with increased blood pressure in the Second National Health and Nutrition Examination Survey (NHANES II) (1976–1988)2 and NHANES 1999–2004.13 A prospective study in Belgium showed associations of changes in blood Cd levels with diastolic blood pressure among women.12 However, a Croatian study showed associations of urinary, but not blood Cd, with diastolic blood pressure.17 These studies varied on the choice of Cd measurement (blood, urine, nails), study design and definition of outcomes. In addition, the relationship between Cd and blood pressure is complicated by the fact that smoking, a major source of Cd exposure in populations, is associated with Cd levels but also independently associated with hypertension.20, 21, 22, 23, 24
American Indians suffer disproportionally from hypertension-related morbidity and CVD.25, 26 Prior research in American Indian communities from the Strong Heart Study (SHS) has demonstrated an association of Cd burden with incident CVD and mortality.10 Middle-aged American Indians recruited from the same communities have higher Cd body burden compared with national averages from individuals 35 years old or older from the Third National Health and Nutrition Examination Survey (NHANES III).10, 27 Therefore, American Indians are a population at risk of diseases related to Cd toxicity.
We studied the association of Cd body burden, as measured in urine, with blood pressure and hypertension in SHS American Indians. Urinary Cd represents Cd concentrations in the renal cortex and has a half-life of decades, representing a suitable biomarker for cumulative Cd exposure or body burden.28 Because environmental exposures are amenable to public health interventions, this research could inform on the Cd-related burden of hypertension and its complications in this population.
Materials and methods
SHS design and population
The SHS recruited a population-based sample of 4545 unrelated tribal members 45 years or older without regard to disease status from 13 tribal communities in Arizona, Oklahoma and North and South Dakota.29 This study uses data from a clinical visit in 1989–1991, which is the SHS visit that has measures of urinary Cd. During the clinical visit, information on demographic characteristics (age, sex, education), lifestyle/behaviors (including smoking initiation, duration and quantity) and medical history were obtained through interviews. Physical exams included anthropometrics (body mass index (BMI), waist and hip girth) and blood pressure. Resting sitting blood pressure was measured in the brachial artery three consecutive times by trained personnel using a calibrated mercury column sphygmomanometer and size-adjusted cuff, and the last two measures were averaged. Participants were instructed to bring all medications taken regularly, including both prescribed and over-the-counter. All medications were categorized according to the American Hospital Formulary Service Pharmacologic-Therapeutic Classification System and summarized by therapeutic class as described previously.30 A fasting blood sample and urine samples were obtained for biomarker measures, which were assayed using standard methods. The SHS/SHFS protocols were approved by the Indian Health Services Institutional Review Board, by Institutional Review Boards of all Institutions and by the Indian communities.29, 31 All participants gave informed consent for participation.
From the initial sample, we excluded individuals with kidney failure defined as on dialysis or receiving a transplant, missing covariates or phenotypes, or urinary Cd measures. The final data set included 3714 SHS participants for whom urinary Cd measures were available.
Urinary Cd measurements
Cd was measured in spot urine samples (stored at −80 °C) using inductively coupled plasma spectrometry.32 The analytic methods and quality control criteria have been described previously.32 The limit of detection was 0.0015 μg l−1. In one participant where Cd was below the limit of detection (0.03% of the total sample), the concentration was imputed as the limit of detection divided by the square root of two.32 The intra- and interassay coefficients of variation for Cd in the SHS were 1.3% and 8.7%, respectively. To account for urine dilution, urine Cd concentrations are expressed in μg per g of urine creatinine. Urine creatinine was measured by an alkaline picrate method.
Blood pressure outcomes
The main outcomes assessed in this study are quantitative blood pressure traits of systolic and diastolic blood pressures. For hypertensive individuals taking antihypertensive medications, measured blood pressure is expected to be lower than if not treated. Adjusting for hypertension treatment as a covariate is not recommended, as it has shown to shrink estimated effects and reduce power in simulation studies.33 Therefore, we added 10 and 15 mm Hg to measured systolic and diastolic blood pressures, respectively, for individuals reporting taking blood pressure-lowering medications as described previously.34, 35 Hypertension was defined by a systolic blood pressure of 140 mm Hg or higher, or a diastolic blood pressure of 90 mm Hg or higher, or use of antihypertensive drugs.36
Covariates and definitions
Urinary Cd levels and blood pressure have been shown to vary by age, sex, BMI and kidney function. Smoking is a source of Cd exposure and a potential confounder. All these covariates were included in models, in addition to variables to account for Cd variation in geographic regions. We also tested other variables including education (less than high school versus high school or higher degree), which was not a significant predictor in models. Kidney function was estimated using the estimated glomerular filtration rate (eGFR) derived from the equation developed by the Chronic Kidney Disease Epidemiology Collaboration. The equation is based on serum creatinine, age, sex and race/ethnicity data.37 Chronic kidney disease was defined by an eGFR <60 ml min−1 per 1.72 m2.
Statistical analyses
Urinary Cd-to-creatinine ratio was right skewed and the data were natural log-transformed (lnCd). Geometric means, medians and percentiles of urinary Cd were also estimated. We first examined the association of lnCd with prevalent systolic and diastolic blood pressure traits in SHS participants using linear regression models. Models were adjusted for age, age,2 sex, age-by-sex interactions, BMI and geographical location (Arizona, North and South Dakotas, Oklahoma) and eGFR (continuous). We adjusted for smoking quantity and intensity using a variable for never vs ever users and cumulative smoking dosage (pack-years), and also performed analysis in the strata of ever- vs never-smoking. We also examined the association of lnCd with blood pressure among never-smokers and light-smokers (<10 pack-years). To examine nonlinear effects of Cd on blood pressure, we tested the association with blood pressure and hypertension within quartiles of Cd distribution using the lower quartile as referent. In secondary analyses, we examined the associations among current-smokers, and if associations were modified by sex or changed when excluding individuals taking antihypertensive medications, given prior research suggesting confounding effects of antihypertensive medications. We also tested Cd associations with hypertension. Statistical tests were two sided with significance set at P<0.05.
Results
Among 3714 SHS participants, the mean age was 56 years, 41% were men and 67% were ever-smokers (Table 1). Thirty-eight percent of participants had hypertension, and 23% were on an antihypertensive medication. Urinary Cd ranged from 0.01 to 78.48 μg g−1 (geometric mean=0.94 μg g−1) with a higher average among ever-smokers and current-smokers than never-smokers. Urinary Cd was correlated with smoking pack-year among ever-smokers (r2=0.16, P<0.0001). On average, SHS participants were light-smokers (mean 10.8 pack-years), but Cd levels were also elevated among light- or never-smokers (Table 1 and Figure 1). Ten percent (N=370) participants had an eGFR <60 ml min−1 per 1.72 m2, but the mean urinary Cd concentration was similar among these individuals and those with an eGFR ⩾60 ml min−1 per 1.72 m2.
In cross-sectional analysis, urinary lnCd was significantly associated with higher systolic blood pressure in models adjusted for age, sex, geographic area, BMI and smoking (ever vs never, and cumulative pack-years) (β representing the mean blood pressure difference by unit of lnCd concentration=1.11, standard error (s.e.)=0.54, P=0.037, n=3714) (Table 2, Model 2). These estimates were stronger when further adjusting for kidney function (β=1.64, s.e.=0.54, P=0.002) (Table 2, Model 3) or when excluding individuals taking antihypertensive medications (β=1.57, s.e.=0.54, P=0.004) (Table 2). The interaction by sex was not significant (P=0.82). The association of urinary lnCd with blood pressure among current-smokers was not significant in fully adjusted models (Table 2).
Among never-smokers, the adjusted estimates of effect for lnCd levels on blood pressure were consistent with that observed among smokers, although not significant (β=1.22, P=0.18) (Table 2, Model 3). Because never- and light-smokers (⩽10 pack-years) had similar low urinary Cd concentrations (Figure 1), we also performed a sensitivity analysis combining never- and light-smokers, for which lnCd association with systolic blood pressure showed even stronger estimates (β=2.03, P=0.002) (Table 2, Model 3). These findings suggest that a relationship exists between Cd and blood pressure even when there is minimal confounding by smoking.
The association of lnCd with diastolic blood pressure was concordant in direction as compared with systolic blood pressure, although it was not statistically significant (Table 2, Models 2 and 3). However, there was a significant association of urinary Cd concentration with diastolic blood pressure among never- and light-smokers (P=0.004, Table 2, Model 3).
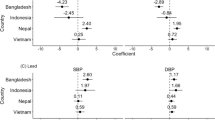
In adjusted models, systolic blood pressure increased across quartiles of Cd concentrations (P=0.029), whereas diastolic blood pressure was unchanged (Figure 2 and Supplementary Table 1). In secondary analysis, lnCd was not significantly associated with hypertension (Table 3), but there was a trend for increased odds of hypertension in the upper quartile of Cd distribution compared with the lower quartile (Figure 2 and Supplementary Table 2).
Mean systolic and diastolic blood pressure values and odds ratios of hypertension by quartile of Cd concentrations. The corresponding values of Cd for each quartiles are: Q1:<62 μg g−1; Q2: 0.62 to 0.93 μg g−1; Q3: 0.94 to 1.45 μg g−1; Q4:>1.45 μg g−1. Model 1, adjusted for age, sex, geographic region; Model 2, adjusted for age, sex, geographic region, BMI, smoking (ever vs never, and cumulative pack-years) and eGFR.
Discussion
Adolescent and young adult SHS American Indians have a high prevalence of hypertension (15%) and prehypertension (35%), which has been attributed to obesity and metabolic conditions.38 This population has above national average Cd body burden and is at risk for Cd-related health conditions. The main contribution of our study is the association findings between urinary Cd concentrations and elevated systolic blood pressure among middle-aged American Indians. These associations were present when adjusting for smoking exposure, and among individuals who were light- or never-smokers for increased systolic and diastolic blood pressures. Importantly, as tobacco smoke is a source for Cd, we did observe a correlation between urinary Cd and smoking pack-year among ever-smokers (r2=0.16, P<0.0001). A prior study has also shown a stronger association with blood pressure among never-smokers compared with ever-smokers,13 suggesting that the effect of Cd on blood pressure is unrelated to other smoking toxicants.
The potential toxic role of Cd as a risk factor for hypertension has not been highlighted in clinical guidelines for blood pressure.36, 39 Prior population studies have shown inconsistent associations between Cd and blood pressure for low-to-moderate Cd exposure.2, 4, 12, 13, 14, 15, 16, 17, 18, 19 Some of these inconsistencies can be explained by differences in populations, study design, measurements of Cd (blood vs urine) and potential sources of Cd. In NHANES III, the urinary Cd geometric mean was 0.36 μg g−1 for individuals 35 years or older27 compared with 0.88 μg g−1 among never-smokers American Indians in our study. In addition, most smokers in our study were light-smokers (mean 8.8–10.8 pack-years). These findings suggest other sources of Cd exposure in this population (e.g., food or water) and a potential role for Cd source on these outcomes, for example, by exposing to other toxins or risk factors that augment Cd toxicity. The sources of Cd and these additional risk factors will need to be further evaluated in this population.
Urinary Cd concentrations have decreased between 1988 and 2008 in the United States, in parallel with declining smoking rates and changes in exposure to tobacco smoke.27 However, it is unknown if Cd exposure is decreasing in American Indians. Urine levels of Cd correlate with increased renal cortex Cd concentration, a major site of Cd accumulation in the body,40 and thus reflect total body burden. Cd has been associated with kidney dysfunction,2 but we did not find differences in urinary Cd concentrations among individuals with and without chronic kidney disease in our study. However, adjusting for kidney function strengthened the associations between Cd and systolic blood pressure (P=0.002), highlighting the importance of adjusting for physiologic functionality.
Our study is limited to cross-sectional Cd–blood pressure associations, although urinary Cd is considered a biomarker of lifetime body burden as compared with blood Cd concentrations.28 We used a constant to account for blood pressure-lowering medications, but our sensitivity analysis excluding treated individuals did not show substantial changes of findings. Cd was associated with small increases in blood pressure and not with hypertension in our study. However, at the population level, these small increases in blood pressure have shown to have a large impact on CVD events1 and our ultimate goal is to focus on population prevention measures. We are currently examining these associations using prospective data. Future studies should focus on the interplay of environmental and genetic factors in the Cd–blood pressure associations. For example, genome-wide association studies have identified associations of the SLC39A8 gene with hypertension.34 This gene encodes a zinc transporter and main carrier of Cd into cells in humans. A recent study has shown the contribution of genetic variability to arsenic-associated longitudinal increases in blood pressure.41 These and our findings suggest a potential causal role of Cd and other metals in the occurrence of hypertension.

In summary, we identified significant associations between urinary Cd and increased blood pressure in American Indians, independent of smoking exposure. These findings suggest a role for low-to-moderate Cd burden in increased blood pressure. If confirmed in other studies, our findings may have implications for public health promotion and policies in relation to exposure to Cd and potentially to other toxic metals.
References
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360 (9349): 1903–1913.
Whittemore AS, DiCiccio Y, Provenzano G . Urinary cadmium and blood pressure: results from the NHANES II survey. Environ Health Perspect 1991; 91: 133–140.
Jiang J, Liu M, Parvez F, Wang B, Wu F, Eunus M et al. Association between arsenic exposure from drinking water and longitudinal change in blood pressure among HEALS cohort participants. Environ Health Perspect 2015; 123 (8): 806–812.
Telisman S, Jurasovic J, Pizent A, Cvitkovic P . Blood pressure in relation to biomarkers of lead, cadmium, copper, zinc, and selenium in men without occupational exposure to metals. Environ Res 2001; 87 (2): 57–68.
Wolf MB, Baynes JW . Cadmium and mercury cause an oxidative stress-induced endothelial dysfunction. Biometals 2007; 20 (1): 73–81.
Messner B, Knoflach M, Seubert A, Ritsch A, Pfaller K, Henderson B et al. Cadmium is a novel and independent risk factor for early atherosclerosis mechanisms and in vivo relevance. Arterioscler Thromb Vasc Biol 2009; 29 (9): 1392–1398.
Varoni MV, Palomba D, Gianorso S, Anania V . Cadmium as an environmental factor of hypertension in animals: new perspectives on mechanisms. Vet Res Commun 2003; 27 (Suppl 1): 807–810.
Schroeder HA, Vinton WH Jr . Hypertension induced in rats by small doses of cadmium. Am J Physiol 1962; 202: 515–518.
Solenkova NV, Newman JD, Berger JS, Thurston G, Hochman JS, Lamas GA . Metal pollutants and cardiovascular disease: mechanisms and consequences of exposure. Am Heart J 2014; 168 (6): 812–822.
Tellez-Plaza M, Guallar E, Howard BV, Umans JG, Francesconi KA, Goessler W et al. Cadmium exposure and incident cardiovascular disease. Epidemiology 2013; 24 (3): 421–429.
Myong JP, Kim HR, Jang TW, Lee HE, Koo JW . Association between blood cadmium levels and 10-year coronary heart disease risk in the general Korean population: the Korean National Health and Nutrition Examination Survey 2008–2010. PLoS ONE 2014; 9 (11): e111909.
Staessen JA, Kuznetsova T, Roels HA, Emelianov D, Fagard R . Exposure to cadmium and conventional and ambulatory blood pressures in a prospective population study. Public Health and Environmental Exposure to Cadmium Study Group. Am J Hypertens 2000; 13 (2): 146–156.
Tellez-Plaza M, Navas-Acien A, Crainiceanu CM, Guallar E . Cadmium exposure and hypertension in the 1999–2004 National Health and Nutrition Examination Survey (NHANES). Environ Health Perspect 2008; 116 (1): 51–56.
Eum KD, Lee MS, Paek D . Cadmium in blood and hypertension. Sci Total Environ 2008; 407 (1): 147–153.
Vivoli G, Bergomi M, Borella P, Fantuzzi G, Caselgrandi E . Cadmium in blood, urine and hair related to human hypertension. J Trace Elem Electrolytes Health Dis 1989; 3 (3): 139–145.
Kelishadi R, Askarieh A, Motlagh ME, Tajadini M, Heshmat R, Ardalan G et al. Association of blood cadmium level with cardiometabolic risk factors and liver enzymes in a nationally representative sample of adolescents: the CASPIAN-III Study. J Environ Public Health 2013; 2013: 142856.
Caciari T, Sancini A, Tomei F, Antetomaso L, Tomei G, Scala B et al. Cadmium blood/urine levels and blood pressure in workers occupationally exposed to urban stressor. Ann Ig 2012; 24 (5): 417–428.
Lee BK, Kim Y . Association of blood cadmium with hypertension in the Korean general population: analysis of the 2008–2010 Korean National Health and Nutrition Examination Survey data. Am J Ind Med 2012; 55 (11): 1060–1067.
Gallagher CM, Meliker JR . Blood and urine cadmium, blood pressure, and hypertension: a systematic review and meta-analysis. Environ Health Perspect 2010; 118 (12): 1676–1684.
Primatesta P, Falaschetti E, Gupta S, Marmot MG, Poulter NR . Association between smoking and blood pressure: evidence from the health survey for England. Hypertension 2001; 37 (2): 187–193.
Kim SJ, Lee J, Jee SH, Nam CM, Chun K, Park IS et al. Cardiovascular risk factors for incident hypertension in the prehypertensive population. Epidemiol Health 2010; 32: e2010003.
Niskanen L, Laaksonen DE, Nyyssonen K, Punnonen K, Valkonen VP, Fuentes R et al. Inflammation, abdominal obesity, and smoking as predictors of hypertension. Hypertension 2004; 44 (6): 859–865.
Halperin RO, Gaziano JM, Sesso HD . Smoking and the risk of incident hypertension in middle-aged and older men. Am J Hypertens 2008; 21 (2): 148–152.
Bowman TS, Gaziano JM, Buring JE, Sesso HD . A prospective study of cigarette smoking and risk of incident hypertension in women. J Am Coll Cardiol 2007; 50 (21): 2085–2092.
Welty TK, Lee ET, Yeh J, Cowan LD, Go O, Fabsitz RR et al. Cardiovascular disease risk factors among American Indians. The Strong Heart Study. Am J Epidemiol 1995; 142 (3): 269–287.
Lee ET, Cowan LD, Welty TK, Sievers M, Howard WJ, Oopik A et al. All-cause mortality and cardiovascular disease mortality in three American Indian populations, aged 45–74 years, 1984–1988. The Strong Heart Study. Am J Epidemiol 1998; 147 (11): 995–1008.
Tellez-Plaza M, Navas-Acien A, Caldwell KL, Menke A, Muntner P, Guallar E . Reduction in cadmium exposure in the United States population, 1988–2008: the contribution of declining smoking rates. Environ Health Perspect 2012; 120 (2): 204–209.
Jarup L, Akesson A . Current status of cadmium as an environmental health problem. Toxicol Appl Pharmacol 2009; 238 (3): 201–208.
Lee ET, Welty TK, Fabsitz R, Cowan LD, Le NA, Oopik AJ et al. The Strong Heart Study. A study of cardiovascular disease in American Indians: design and methods. Am J Epidemiol 1990; 132 (6): 1141–1155.
Hayslett JA, Eichner JE, Yeh JL, Wang W, Henderson J, Devereux RB et al. Hypertension treatment patterns in American Indians: the Strong Heart Study. Am J Hypertens 2001; 14 (9, Part 1): 950–956.
North KE, Williams JT, Welty TK, Best LG, Lee ET, Fabsitz RR et al. Evidence for joint action of genes on diabetes status and CVD risk factors in American Indians: the strong heart family study. Int J Obes Relat Metab Disord 2003; 27 (4): 491–497.
Scheer J, Findenig S, Goessler W, Francesconi KA, Howard B, Umans JG et al. Arsenic species and selected metals in human urine: validation of HPLC/ICPMS and ICPMS procedures for a long-term population-based epidemiological study. Anal Methods 2012; 4 (2): 406–413.
Tobin MD, Sheehan NA, Scurrah KJ, Burton PR . Adjusting for treatment effects in studies of quantitative traits: antihypertensive therapy and systolic blood pressure. Stat Med 2005; 24 (19): 2911–2935.
Ehret GB, Munroe PB, Rice KM, Bochud M, Johnson AD, Chasman DI et al. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 2011; 478 (7367): 103–109.
Levy D, Ehret GB, Rice K, Verwoert GC, Launer LJ, Dehghan A et al. Genome-wide association study of blood pressure and hypertension. Nat Genet 2009; 41 (6): 677–687.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289 (19):2560–2572.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150 (9): 604–612.
Drukteinis JS, Roman MJ, Fabsitz RR, Lee ET, Best LG, Russell M et al. Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the Strong Heart Study. Circulation 2007; 115 (2): 221–227.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311 (5): 507–520.
Prozialeck WC, Edwards JR . Mechanisms of cadmium-induced proximal tubule injury: new insights with implications for biomonitoring and therapeutic interventions. J Pharmacol Exp Ther 2012; 343 (1): 2–12.
Farzan SF, Karagas MR, Jiang J, Wu F, Liu M, Newman JD et al. Gene-arsenic interaction in longitudinal changes of blood pressure: Findings from the Health Effects of Arsenic Longitudinal Study (HEALS) in Bangladesh. Toxicol Appl Pharmacol 2015; 288 (1): 95–105.
Acknowledgements
This research is supported by the NHLBI HL123677-02 (to NF) and the NIEHS training grant (ES007141-32) (to PB). MTP was supported by the Strategic Action for Research in Health sciences (CP12/03080), which is an initiative from Carlos III Health Institute Madrid and the Spanish Ministry of Economy and Competitiveness and are cofunded with European Funds for Regional Development (FEDER).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Journal of Human Hypertension website
Supplementary information
Rights and permissions
About this article
Cite this article
Franceschini, N., Fry, R., Balakrishnan, P. et al. Cadmium body burden and increased blood pressure in middle-aged American Indians: the Strong Heart Study. J Hum Hypertens 31, 225–230 (2017). https://doi.org/10.1038/jhh.2016.67
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2016.67
- Springer Nature Limited
This article is cited by
-
Physical activity attenuates the association between blood cadmium exposure and cardiovascular disease: findings from the National Health and Nutrition Examination Survey 2007–2018
Environmental Science and Pollution Research (2023)
-
Sex-dependent vascular effects of cadmium sub-chronic exposure on rats
BioMetals (2023)
-
Low Level of Serum Cadmium in Relation to Blood Pressures Among Japanese General Population
Biological Trace Element Research (2022)
-
The association between environmental cadmium exposure, blood pressure, and hypertension: a systematic review and meta-analysis
Environmental Science and Pollution Research (2022)
-
Co-exposure to Heavy Metals and Hypertension Among Adults in South Korea
Exposure and Health (2022)