Abstract
Trends in incidence and prevalence of hypertension are grave in China and identifying high-risk, non-hypertension individuals for intervention may delay hypertension onset. We aimed to investigate the incidence of hypertension in northern urban Han Chinese population and construct multivariable hypertension prediction models through the prospective cohort, which included 7537 men and 4960 women free of hypertension at baseline between 2005 and 2010. During 38 958 person-years of follow-up, 2785 participants (men, 72.57%; women, 27.43%) developed hypertension. The incidence density of hypertension was 71.48 per 1000 person-year. In multivariable backward cox analyses, age, body mass index, systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose and current drinking were retained for both men and women, while gamma-glutamyl transferase only for men, total cholesterol, neutrophil granulocyte and current smoking only for women. The area under receiver operating characteristic curve (AUC) was 0.761 (95% confidence interval (CI), 0.752–0.771) for men and 0.753 (95% CI, 0.741–0.765) for women, even after 10-fold cross-validation, the AUC was 0.760 (95% CI, 0.751–0.770) for men and 0.749 (95% CI, 0.737–0.761) for women. Through risk stratification, the absolute risk of incident hypertension in 5 years at moderate, high and very high risk level was 2.13, 3.84 and 6.14 times that of those who were at low risk in men, and 1.30, 2.56 and 6.01 times that of those who were at low risk in women. Our findings identified predictors of incident hypertension and indicated that the sex-specific multivariable prediction models would be simply used to estimate the risk of incident hypertension.
Similar content being viewed by others
Introduction
Hypertension, as the leading risk factor for cardiovascular morbidity and mortality, already affects one billion people worldwide.1 Complications of hypertension account for 9.4 million global deaths every year.2 To reduce the burden of cardiovascular disease, guidelines have stressed on the importance of preventing hypertension.3 While China, one of the world’s most populous and fastest developing countries, data reported that increased prevalence of hypertension partly attributed to increased incidence of hypertension.4, 5 A latest survey demonstrated that the prevalence rate of hypertension in China has increased to 29.6% and the awareness is just 42.6%, which is much lower than developed countries (66.5%).6 Hundreds of millions Chinese have not realized the silent, invisible killer.
Consequently, it is very necessary to establish prediction model to identify people at high risk for inclusion in clinical trials for hypertension prevention. So far many countries and regions have developed or validated risk models that predict the onset of hypertension. Among those, Framingham hypertension risk score is widely used to predict the risk for near-term incident hypertension.7 While Framingham Heart Study was based on Caucasian, its prediction models have been validated not so suitable for Chinese.8, 9, 10 With respect to Chinese, a 15-year risk of incident hypertension model was established on a cohort which set up since 1992 from 11 provinces and cities of China.11 Yet, the 15-year risk model of hypertension has not considered so many biochemical risk factors in the beginning of constructing model. Another famous Chinese hypertension risk model was established by the Chin-Shan Community Cardiovascular Cohort Study in Taiwan.12 However, lifestyle risk factors were lacking in the model of this community study.
Therefore, we aimed to investigate the incidence of hypertension in the northern urban Han Chinese health check-up population and construct a hypertension prediction model through the prospective cohort. We included many biochemical and lifestyle predictors that were confirmed by other investigations and available in the routine health check-up.
Subjects and Methods
Study population and cohort design
Subjects who participated in routine health check-up system in Center for Health Management of Shandong Provincial Qianfoshan Hospital and Shandong Provincial Hospital between 2005 and 2010 composed the longitudinal cohort representative of the northern urban Han Chinese population (n=95 908). For our research, participants were eligible for inclusion if they possessed at least three year’s health check-up records between 2005 and 2010 (n=18 665). We excluded participants at the first check-up who had hypertension with antihypertensive medication, or systolic blood pressure (SBP) ⩾140 mm Hg, or diastolic blood pressure (DBP) ⩾90 mm Hg, or cardiovascular disease (coronary heart disease, cardiomyopathy, atrial fibrillation), or stroke (ischemic stroke and hemorrhagic stroke); were younger than 18 years and had missing covariates. Finally, 7 537 men and 4 960 women remained available for analysis. The median follow-up was 4.0 years.
Measurements
At every health check-up, participants underwent a routine questionnaire, anthropometric, clinical and laboratory tests after at least a 12-h fast. The questionnaire contained lifestyle behaviors of smoking, drinking and physical activity and history of cardiovascular disease, hypertension, contents of medicine use and other background information. The anthropometric measurement covered weight, height and blood pressure. Weight and height were measured on subjects wearing light clothes without shoes using a calibrated scale. Body mass index (BMI) was calculated as weight/height2 (kg m−2), as an estimate of obesity. Blood pressure measurement was made on the right arm with Omron HEM-907 (Omron Healthcare Co., Ltd., Matsusaka-City, Mie, Japan) by a cuff-oscillometric method. Participants had rested for 5 min in the sitting position, and the average of two measurements was recorded as the examination blood pressure. The laboratory test included fasting blood glucose (FBG), total cholesterol (CHOL), triglycerides (TG), high-density lipoprotein (HDL), gamma-glutamyl transferase (GGT), serum albumin (ALB), serum globulins (GLO), hemoglobin (Hb), hematocrit (HCT), white blood cell count (WBC), lymphocyte (LC), neutrophil granulocyte (NGC) and monocyte (MONC).
Definition of hypertension
The outcome of interest was defined as first occurrence at any follow-up medical check-up of SBP ⩾140 mm Hg or DBP ⩾90 mm Hg or of the person taking antihypertensive medication.
Statistical analysis
For baseline characteristics, continuous variables were presented as mean (s.d.), and categorical variables were presented as frequency (percentage). Difference in baseline characteristics between individuals who developed hypertension and those who did not were compared by Student's t-test or t’-test for continuous variables and by χ2 test for categorical variables. We calculated the number of person-year as the sum of the follow-up times from the baseline to the onset of hypertension or the last health check-up. Cox proportional hazard models were used to estimate the unadjusted hazard ratios. Then, a set of risk factors were selected via backward cox proportional model, and we also detected the interaction term for DBP, SBP and BMI by age. To apply the multivariable model to predict the onset of hypertension, we evaluated the area under receiver operator characteristics curve (AUC) and the AUC after 10-fold cross-validation. Finally, based on the predictive probability, we divided study sample into four risk levels. We did sex-specific analysis for all the investigations. All statistical analyses were performed using SAS 9.2 (SAS Institute, Inc., Cary, NC, USA), and a two-sided P<0.05 was set as statistically significant.
Results
The baseline characteristics of study sample were shown in Table 1.The average age at baseline was 41.73 in men and 39.49 in women. The mean or frequency of most indexes in men was higher than those women except for GLO and HDL. Most women did not smoke or drink.
During the 38 958 person-years of follow-up, 2785 participants developed hypertension between 2005 and 2010. Figure 1 demonstrated the constructed prospective cohort and the occurrence of hypertension in detail. The incidence density of hypertension in this prospective cohort was 71.48 per 1000 person-year. Diagnosis of new-onset hypertension was based on increased SBP alone in 1199 (43.05%) participants, DBP alone in 534 (19.17%), and both SBP and DBP in 498 (17.88%). Among the participants with incident hypertension, the treatment rate was 19.89% (n=554) and the blood pressure control rate was 10.99% (n=306).
Table 2 presented that the incidence of hypertension during follow-up in men (2021 cases, 26.81%) was higher than in women (764 cases, 15.40%). The statistically-significant differences between non-hypertension and hypertension for the baseline characteristics were observed apart from HDL, Hb, current smoking in men, and HDL in women. Most listed baseline variables in hypertension were higher than non-hypertension other than ALB and HDL in both men and women.
Gender differences were found in the incidence of hypertension, and the HR (95% confidence interval (CI)) of 1.857 (1.708–2.018) for men vs women. Further subgroup analyses in men and women subpopulation were structured. Table 3 illustrated the results of the association of related predictors with hypertension in unadjusted cox model. No statistically-significant differences were found in HDL, Hb, HCT and current smoking for men and HDL, LC and MONC for women.
Furthermore, multivariable cox models were constructed with all the predictors using backward elimination. We finally got seven variables in men and nine in women, shown in Table 4. These factors were independent predictors of hypertension. The interactions of BMI by age and DBP by age were statistically significant for men. Increasing levels of BMI and DBP were associated with an increased risk for incident hypertension across all ages, but the slope of the association was steeper in younger than in older. We also considered the interactions of SBP by age in men and all above interactions in women which did not enter the models.
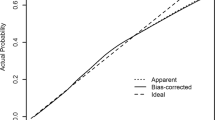
In addition, ROC curve for the multivariable models was presented in Figure 2. The AUC (95% CI) was 0.761 (0.752–0.771) for men and 0.753 (0.741–0.765) for women. While after 10-fold cross-validation, the AUC (95% CI) was 0.760 (0.751–0.770) for men and 0.749 (0.737–0.761) for women.
ROC curve for incident hypertension prediction models in men and women. (a, b) Presents the predictive power for men and women, respectively. (a) AUC (95% CI): 0.761 (0.752–0.771), z-statistic: 38.892; significance level P (area=0.5): 0.0001; cutoff point 0.3470 with sensitivity 0.724, specificity 0.672 and accuracy 68.6%; (b) AUC (95% CI): 0.753 (0.741–0.765), z-statistic: 23.741; significance level P (area=0.5): 0.0001; cutoff point 0.2262 with sensitivity 0.644, specificity 0.754 and accuracy 73.6%.
Finally, we divided study sample into four risk levels sex-specifically. As the distribution of predictive probability was not normal, we used quartiles as the dividing values. The first 25% participants were at low risk, and the following three parts were respectively at moderate, high and very high risk. The absolute risk and actual probability of incident hypertension of each risk level were shown in Table 5. The absolute risk of incident hypertension in 5 years at moderate, high and very high risk level was 2.13, 3.84 and 6.14 times of those who were at low risk in men, and 1.30, 2.56 and 6.01 times of those who were at low risk in women.
Discussion
With this prospective cohort study, we investigated the incidence of hypertension in northern urban Han Chinese population, identified the multi-marker of new-onset hypertension in this population and constructed multivariable prediction hypertension models sex-specifically resulting from 20 risk factors concerning different pathophysiological mechanisms. To our knowledge, seldom investigations examined so many risk factors to predict the onset of hypertension in northern urban Han Chinese population. The validity of our study was stressed by the prospective cohort analysis; sample size was very large; the blood pressure was obtained in a standardized manner in routine health check-up system by physician; the candidate predictors, which were available in routine health check-up were both biologically plausible and confirmed by previous works.
On the basis of previous national survey data in China, the prevalence of hypertension in adults has increased from 5.1% in 1959 to 11.3% in 1991 and 29.6% in 2009.6, 13, 14 Furthermore, an analysis of hypertension incidence trends demonstrated that high prevalence was partly owing to the increased incidence of hypertension. Results from a Chinese cohort study stated incidence of hypertension (per 1000 person-year) significantly increased from 29 in 1991–1997 to 53 in 2004–2009.4 In our study, the incidence of hypertension was 71.48 per 1 000 person-year, higher than that of previous study. This may be explained by the following reasons: first, our sample was got from the northern urban Chinese population. The northern Chinese population preferred to eat salty food and the prevalence and incidence were always higher than southern Chinese population and overall Chinese population.15 Second, our sample was based on health-check databases, which included a set of individuals who actively participated in health examination by personal expense. Therefore, our sample may be different from population who recruited from nine provinces through multistage, randomized, cluster sampling process in various aspects including health consciousness. Third, from the time point of view, the incidence may be higher in accordance with the trend of hypertension onset.4
Whether the incidence of hypertension is associated with gender is controversial. In our study, the future risk of incident hypertension was higher in men than in women, which was similar to a set of studies.16, 17 However, some investigations have suggested that women had a higher risk7 or sex was not a vital determinant.18 As expected, hypertension risk increased with aging and elevated blood pressure. The increasing future risk of hypertension with aging is due primarily to increased peripheral vascular resistance and vascular stiffness.19, 20 Previous investigations have demonstrated that baseline SBP and DBP are predominant determinants of incident hypertension, even each unit increase in the blood pressure above the optimal value of 119/79 mm Hg elevates the risk of onset hypertension.7, 12, 21 Of our study outcome, sole elevated SBP and sole elevated DBP accounted for 43.05% and 19.17%. Additionally, the interaction of DBP by age in men was statistically significant, which meant that the effect of DBP was more obvious at younger ages. These phenomena can be explained that SBP invariably rises with aging, while DBP tends to decline after fifth or sixth decade.20 Furthermore, the mechanism behind it may be resulted from large artery stiffness dominating vascular resistance and DBP falling.
BMI as general obesity index was higher in participant with hypertension than without hypertension at baseline in our study. Many investigations demonstrate that obesity is closely related to incident hypertension, and obesity is one of the most important independent risk factors of hypertension,7, 16, 22 which is consistent with our results. In addition, we discovered the interaction between BMI and age in men significantly. Just as DBP, increasing levels of BMI were associated with an increased risk for incident hypertension across all ages in men, but the slope of the association was steeper in young than in old. Unfortunately, measurements of abdominal obesity such as waist circumference and waist–hip ratio were absent in the present study, which were superior to BMI in predicting cardiovascular risk.23 Yet, a study has demonstrate that BMI was as strong as abdominal indicators in the relation of development of hypertension.22
Our prospective finding stated that current drinking was associated with the development of hypertension in both genders, and current smoking was only hazardous in women. This was determined by the baseline characteristics of our sample, which indicated no significant distribution difference of current smoking in men with or without future hypertension, so we may not get whether current smoking was harmful for men according to our results. While in many investigations, the risk of incident hypertension of current smokers has been validated much higher than non-smokers.7, 21, 24
Our study indicated that current drinking increased the risk of future hypertension, which was also suggested by other investigations.25, 26 Of note, another lifestyle factor, regular exercise was presented as a risk factor in unadjusted model, this may be caused by potential measurement misclassification in assessing exercise levels.
We can get many biomedical factors in routine health check-up whose effects are much originated from age, gender, smoking, drinking and other lifestyle factors. After backward elimination, GGT, FBG in men and FBG, CHOL, NGC in women were remained as secondary prevention biomedical factors. Quite a few investigators considered diabetes or FBG as a predictor of incident hypertension.12, 24 In our multivariable models, each unit increased in FBG, the risk of incident hypertension increased 11.6% for men and 12.3% for women. Potential relationships between glucose metabolism and hypertension seem to be multidirectional mediators involving impairing endothelium-dependent vasodilation, oxidative stress and insulin resistance.27, 28, 29 GGT has been reported to be a stronger predictor of incident hypertension, even among non-drinkers.30 Similarly, we found that GGT was significant for men in the multivariate model. Considering known functionality of GGT, this would be accounted for producing oxidative stress.30, 31 Among lipoproteins, HDL is a protective factor of incident hypertension, responsible for reversing cholesterol transport. Inversely, elevated CHOL and TG refer to atherosclerosis, endothelial dysfunction, damage of the renal microvasculature, which all infect the development of hypertension.32 With respect to our results, one unit increase in CHOL leads to 14.3% risk increment of incident hypertension for women in multivariable cox model. Our prospective finding demonstrated that leukocyte parameters were associated with incident hypertension in both men and women in unadjusted models. Only NGC was left in multivariable model for women and this was consistent with a Japanese study.33 The linkage between NGC and hypertension may be accounted for increased tendency to adhere to vascular endothelium and the release of ROS, which refers to vascular resistance and oxidative stress.34
Our final multivariable models based on northern urban Han Chinese population consisted of demographic, lifestyle and biomedical factors. Meanwhile, the performance of the final models was acceptable, whose AUC was 0.761 (95% CI, 0.752–0.771) for men and 0.753 (95% CI, 0.741–0.765) for women. Furthermore, AUC after 10-fold cross-validation was approaching to values of the original models. Despite Framingham hypertension risk score was most widely used to predict the risk for near-term incident hypertension, the source population was Caucasian. Investigators have presented that prediction models developed using certain ethnic groups tend to overestimate or underestimate the incidence in other ethnic groups.12, 24 Even in ethnic Chinese, the 15-year risk model of incident hypertension constructed by samples from 11 provinces and cities of China did not include so many biochemical predictors in the beginning.11 Conversely, the prediction model based on Chin-Shan Community Cardiovascular Cohort Study in Taiwan was lacking of lifestyle risk factors.12 As a whole, our final multivariate model was much rational. Other detailed information about our prediction model was available in the Supplementary Appendix.
According to the current health-care system in China,35 much have been invested in the treatment for non-communicable chronic diseases, especially cardiovascular disease. It was urgent to take actions on prevention of cardiovascular disease. Prevention of hypertension onset may represent primordial prevention of cardiovascular disease. Hypertension prediction models can be used to select people at high risk for personalized intervention, to estimate future burden of hypertension and to assist in projecting hypertension prevention strategies and allocation of resources in the light of hypertension risk at a population level.
Nevertheless, several limitations of this study must be considered. First, we selected the predictors that available in routine health check-up, yet did not include many predictors such as family history, serum creatinine, uric acid, C-reactive protein, education, sodium intake, psychosocial factors and genetic markers. As a large set of predictors were associated with others, variables failed to be retained in the final model resulting from non-significant relation with the onset of hypertension. Second, most of the participants who had regular check-ups were younger than 50 years, and they may be a healthier subset of the general population.
In conclusion, we identified the multiple predictors of hypertension and established hypertension prediction models sex-specifically with a prospective cohort study. Our results were consistent with the comprehensive mechanisms of onset of hypertension. The prediction model may give a rough risk of hypertension and facilitate prevention of hypertension and other cardiovascular diseases.

References
Alwan A . Global Status Report on Noncommunicable Diseases 2010. World Health Organization: Geneva, Switzerland, 2011.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013; 380: 2224–2260.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003; 289: 2560–2571.
Liang Y, Liu R, Du S, Qiu C . Trends in incidence of hypertension in Chinese adults, 1991-2009: the China Health and Nutrition Survey. Int J Cardiol 2014; 175: 96–101.
Xi B, Liang Y, Reilly KH, Wang Q, Hu Y, Tang W . Trends in prevalence, awareness, treatment, and control of hypertension among Chinese adults 1991-2009. Int J Cardiol 2012; 158: 326–329.
Wang J, Zhang L, Wang F, Liu L, Wang H . Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens 2014; 27: 1355–1361.
Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D et al. A risk score for predicting near-term incidence of hypertension: the Framingham Heart Study. Ann Intern Med 2008; 148: 102–110.
Liu J, Hong Y, D’Agostino RB Sr, Wu Z, Wang W, Sun J et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA 2004; 291: 2591–2599.
D’Agostino RS, Grundy S, Sullivan LM, Wilson P . Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001; 286: 180–187.
Zheng L, Sun Z, Zhang X, Li J, Hu D, Chen J et al. Predictive value for the rural Chinese Population of the Framingham hypertension risk model: results from Liaoning province. Am J Hypertens 2014; 27: 409–414.
Li G, Liu J, Wang W, Wang M, Xie W, Hao Y et al. [Prediction models for the 15 years risk of new-onset hypertension in Chinese people aged from 35 to 64 years old]. Zhonghua Nei Ke Za Zhi 2014; 53: 265–268.
Chien KL, Hsu HC, Su TC, Chang WT, Sung FC, Chen MF et al. Prediction models for the risk of new-onset hypertension in ethnic Chinese in Taiwan. J Hum Hypertens 2011; 25: 294–303.
Wang LD . Nutrition and Health Status in Chinese People. Beijing CN People’s Publishing House: Beijing, China, 2005.
Wu X, Duan X, Gu D, Hao J, Tao S, Fan D . Prevalence of hypertension and its trends in Chinese populations. Int J Cardiol 1995; 52: 39–44.
Liu LS . [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi 2011; 39: 579–615.
Lee JS, Kawakubo K, Kashihara H, Mori K . Effect of long-term body weight change on the incidence of hypertension in Japanese men and women. Int J Obes Relat Metab Disord 2004; 28: 391–395.
Zhang H, Thijs L, Kuznetsova T, Fagard RH, Li X, Staessen JA . Progression to hypertension in the non-hypertensive participants in the Flemish Study on environment, genes and health outcomes. J Hypertens 2006; 24: 1719–1727.
Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D . Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 2001; 358: 1682–1686.
Benetos A, Waeber B, Izzo J, Mitchell G, Resnick L, Asmar R et al. Influence of age, risk factors, and cardiovascular and renal disease on arterial stiffness: clinical applications. Am J Hypertens 2002; 15: 1101–1108.
Franklin SS, Gustin WT, Wong ND, Larson MG, Weber MA, Kannel WB et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation 1997; 96: 308–315.
Kivimaki M, Batty GD, Singh-Manoux A, Ferrie JE, Tabak AG, Jokela M et al. Validating the Framingham Hypertension Risk Score: results from the Whitehall II study. Hypertension 2009; 54: 496–501.
Nyamdorj R, Qiao Q, Soderberg S, Pitkaniemi J, Zimmet P, Shaw J et al. Comparison of body mass index with waist circumference, waist-to-hip ratio, and waist-to-stature ratio as a predictor of hypertension incidence in Mauritius. J Hypertens 2008; 26: 866–870.
Recio-Rodriguez JI, Gomez-Marcos MA, Patino-Alonso MC, Agudo-Conde C, Rodriguez-Sanchez E, Garcia-Ortiz L . Abdominal obesity vs general obesity for identifying arterial stiffness, subclinical atherosclerosis and wave reflection in healthy, diabetics and hypertensive. BMC Cardiovasc Disord 2012; 12: 3–11.
Kshirsagar AV, Chiu YL, Bomback AS, August PA, Viera AJ, Colindres RE et al. A hypertension risk score for middle-aged and older adults. J Clin Hypertens Greenwich 2010; 12: 800–808.
Stranges S, Wu T, Dorn JM, Freudenheim JL, Muti P, Farinaro E et al. Relationship of alcohol drinking pattern to risk of hypertension a population-based study. Hypertension 2004; 44: 813–819.
Okubo Y, Sairenchi T, Irie F, Yamagishi K, Iso H, Watanabe H et al. Association of alcohol consumption with incident hypertension among middle-aged and older Japanese Population: the Ibarakai Prefectural Health Study (IPHS). Hypertension 2014; 63: 41–47.
Title LM, Cummings PM, Giddens K, Nassar BA . Oral glucose loading acutely attenuates endothelium-dependent vasodilation in healthy adults without diabetes: an effect prevented by vitamins C and E. J Am Coll Cardiol 2000; 36: 2185–2191.
Ceriello A, Quatraro A, Giugliano D . Diabetes mellitus and hypertension: the possible role of hyperglycaemia through oxidative stress. Diabetologia 1993; 36: 265–266.
Ferrannini E, Buzzigoli G, Bonadonna R, Giorico MA, Oleggini M, Graziadei L et al. Insulin resistance in essential hypertension. N Engl J Med 1987; 317: 350–357.
Stranges S, Trevisan M, Dorn JM, Dmochowski J, Donahue RP . Body fat distribution, liver enzymes, and risk of hypertension: evidence from the Western New York Study. Hypertension 2005; 46: 1186–1193.
Lee DH, Jacobs DJ, Gross M, Kiefe CI, Roseman J, Lewis CE et al. Gamma-glutamyltransferase is a predictor of incident diabetes and hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Clin Chem 2003; 49: 1358–1366.
Rosendorff C . Hypertension: mechanisms and diagnosis. Essential Cardiology. Springer, New York, 2013, 543–559.
Tatsukawa Y, Hsu WL, Yamada M, Cologne JB, Suzuki G, Yamamoto H et al. White blood cell count, especially neutrophil count, as a predictor of hypertension in a Japanese population. Hypertens Res 2008; 31: 1391–1397.
Sela S, Mazor R, Amsalam M, Yagil C, Yagil Y, Kristal B . Primed polymorphonuclear leukocytes, oxidative stress, and inflammation antecede hypertension in the Sabra rat. Hypertension 2004; 44: 764–769.
Ling R, Liu F, Lu X, Wang W . Emerging issues in public health: a perspective on China’s healthcare system. Public Health 2011; 125: 9–14.
Acknowledgements
This work was supported by grants from the National Nature Science Foundation (No. 81273082) of China and funded by Taishan industrial expert program. The founders were not involved in study design, analysis and interpretation. We would like to thank all subjects who participated in the study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Journal of Human Hypertension website
Supplementary information
Rights and permissions
About this article
Cite this article
Chen, Y., Wang, C., Liu, Y. et al. Incident hypertension and its prediction model in a prospective northern urban Han Chinese cohort study. J Hum Hypertens 30, 794–800 (2016). https://doi.org/10.1038/jhh.2016.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2016.23
- Springer Nature Limited
This article is cited by
-
Development of hypertension models for lung cancer screening cohorts using clinical and thoracic aorta imaging factors
Scientific Reports (2024)
-
A comparison of machine learning algorithms and traditional regression-based statistical modeling for predicting hypertension incidence in a Canadian population
Scientific Reports (2023)
-
Hypertension risk prediction models for patients with diabetes based on machine learning approaches
Multimedia Tools and Applications (2023)
-
Development and validation of hypertension prediction models: The Korean Genome and Epidemiology Study_Cardiovascular Disease Association Study (KoGES_CAVAS)
Journal of Human Hypertension (2022)
-
Establishment and evaluation of a risk-prediction model for hypertension in elderly patients with NAFLD from a health management perspective
Scientific Reports (2022)