Abstract
The objective of this study was to explore the age- and sex-dependent association between sleep duration and incident hypertension in a Chinese population. The Kailuan prospective cohort study recruited 101 510 participants. Those participants were followed for an average of 3.98 years and the data obtained from 32 137 participants out of 101 510 were analyzed in this study. Sleep duration was categorized as five groups of⩽5, 6, 7, 8 and ⩾9 h. Cox proportional-hazards models were used to analyze the association of sleep duration with incident hypertension. The 3.98 years’ follow-up data showed that 12 732 out of 32 137 participants developed hypertension. Short duration of sleep (⩽5 h per night) was associated with an increased risk of hypertension in woman (hazard ratio (HR) 1.27; 95% confidence interval (CI) 1.02 to 1.58) and participants aged <60 years (HR 1.11; 95% CI 1.02–1.21), when compared with the group reported with 7 h of sleep per day. This study suggested that short sleep duration could cause an increased risk of hypertension in Chinese females and population aged <60 years.
Similar content being viewed by others
Introduction
The prevalence of hypertension has increased over the past decade despite improvements in awareness, treatment and disease prevention.1 It is well-known that hypertension in adults enhances the risk of cardiovascular events.2, 3, 4 Increasing evidence suggests that sleep plays an important role in the pathogenesis and progression of cardiovascular disease5 and hypertension.6, 7, 8, 9, 10, 11, 12 Short sleep restriction for as little as 1 night has been reported to increase blood pressure in both healthy13, 14, 15 and hypertensive16 subjects. Gangwisch et al.8 observed an increased risk of hypertension in poor sleepers (⩽5 h per night) aged from 32–59. No association between sleep duration and incident hypertension in the elderly was found in this study. Other studies17, 18, 19, 20 have also shown an increased prevalence of hypertension among children and adolescents. Cappuccio et al.21 reported a women-specific associations of short sleep duration with prevalent and incident hypertension in a cohort of 10 308 British subjects aged 35–55 at baseline.22 However, the association between short sleep duration and incident hypertension by the age and gender has not been studied in China. Thus, the aim of this study was to evaluate the associations between self-reported sleep duration and incident hypertension during an average 3.98-year follow-up period from 2006 to 2011 in the Kailuan studying group in China.
Materials and methods
Study design and participants
The Kailuan study is a prospective cohort study, which was conducted in the Kailuan community in the city of Tangshan, China. The city of Tangshan has ~7.2 million inhabitants and situated about 150 km southeast of Beijing city, and is a center of the coal mining industry in the Province of Hebei. The Kailuan community is a functional and comprehensive community owned and managed by the Kailuan Group. Eleven hospitals are responsible for the healthcare of this community. The basic medical service, such as annual physical examination including routine blood, urine and biochemical tests for all of residents in the Kailuan community is covered by medical insurance. From June 2006 to October 2007, the residents of Kailuan community receiving routine medical examination in 11 hospitals and meeting the following criteria were invited to participate in the Kailuan study: (1) aged 18 years or older; (2) provided informed consent. In total, 101 510 participants (81 110 men; age range from18 to 98 years) were enrolled in the Kailuan study during this period. The study protocol was approved by the ethics committee of the Kailuan General Hospital and an informed written consent was obtained from each participant.
All participants underwent a clinical examination and a standardized interview during enrollment. Physical activity was evaluated based on the responses to questions regarding the types and frequencies of physical activity at work and during leisure time. Physical activity was classified as ⩾4 times per week and ⩾20 min each time, <80 min per week or none. Smoking and drinking status were classified as never, former or current according to self-reported information. Salt intake amount was classified into three categories of low, medium or high, with a definition of <6 g per day, 6–10 g per day or >10 g per day. Diabetes mellitus was defined as a self-reported history, currently treated with insulin or oral hypoglycemic agents. Anthropomorphic parameters such as body height and weight and waist circumference were measured. A 10-s, 12-lead electrocardiography was used to measure the resting heart rate (RHR) after the individual had rested in the supine position for 5 min. Sleep duration was elicited by the question ‘How many hours of sleep do you have on an average night in the preceding 3 months?’. The responses of sleep duration were categorized as ⩽5, 6, 7, 8 and ⩾9 h.
Follow-up
All participants were followed up from a baseline examination from June 2006 through December 31, 2010. The blood pressures from all of participants were re-examined every 2 years (2008–2009 and 2010–2011). At the same time, participants received interviews and clinical examinations by hospital physicians or research nurses, who were blanked to the results obtained previously.23
Assessment of hypertension
Blood pressure and RHR were assessed with the person sitting for at least 5 mins. The participants were refrained from smoking, drinking caffeine containing beverages and alcohol for at least 3 h, and any kind of exercise performed in 30 mins prior to the examination. Blood pressure was measured twice in 5-min intervals on the left arm to the nearest 2 mm Hg using a mercury sphygmomanometer. The average of two readings was used in the data analysis. If the difference between two measurements was >5 mm Hg, an additional reading was taken and the average of all three readings was used in the data analysis.
New onset hypertension was defined as systolic blood pressure of <140 mm Hg, diastolic blood pressure <90 mm Hg, no history of hypertension and no use of antihypertensive drugs at baseline of the study, and as systolic blood pressure of ⩾140 mm Hg, diastolic blood pressure ⩾90 mm Hg and/or use of antihypertensive drugs during the follow-up period.23
Statistical analysis
Statistical analysis was performed using SAS software (version 9.3; SAS Institute Inc., Cary, NC, USA). First, we defined continuous variables by their means±s.d. and categorical variables as percentages. We then compared the parameters according to the sleep duration. Analysis of variance test was used for non-paired samples of normally distributed parameters, Kruskal–Waillis test for non-parametric variables and X2-test for the comparison of categorical variables. In addition, we also performed a multivariate analysis using three models. The data in Model 1 were unadjusted. In Model 2, the data were adjusted for age, gender, body mass index, RHR, smoking status, drinking status, physical activity, salt intake status, history of diabetes, hyperlipidemia, and antidiabetic and cholesterol-lowering medication. In addition to the independent parameters analyzed in Model 2, Model 3 also included baseline systolic blood pressure, diastolic blood pressure and family history of hypertension. Cox proportional-hazards modeling was used to calculate the hazard ratio (HR) and 95% confidence interval (CI) of hypertension. Finally, we analyzed the joint effects of sleep duration and gender/age (age<60 vs age⩾60) on the risk of hypertension. The interactions of sleep duration with gender and age on their risk of hypertension were analyzed by multiplicative Cox proportional-hazards modeling. All statistical tests were two tailed, with a significance level set at P<0.05.
Results
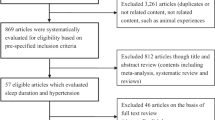
Among 101 510 participants in the Kailuan study, we excluded participants with hypertension history (44 653) and those lacking sleep duration data (2592). We also excluded 22 128 participants who did not participate in face-to-face follow-up examinations in 2008–2009 or 2010–2011. Finally, 32 137 participants meeting the criteria were eligible for the present study. The mean age of participants was 46.32±11.50 years (median: 46.63 years; range: 38.65–53.54 years).
The study participants were divided into five groups based on sleep duration ⩽5 h, 6 h, 7 h, 8 h and⩾9 h. Table 1 shows the baseline characteristics of participants according to their sleep duration. Since 7 h is conventionally considered to be the appropriate duration of sleep in Chinese adults, we appointed 7 h per night as the reference group in our study.7, 8, 21, 24 In comparison to self-reported sleep durations of 7 h, sleep durations of ⩽5 h were associated with older age, high systolic blood pressure, high diastolic blood pressure, excessive consumption of cigarettes and alcohol, past high salt intake and history of diabetes. Sleep durations of ⩾9 h were associated with younger age, low physical activity, low alcohol consumption, high salt intake and higher heart rate.
Tables 2 and 3 showed the hazard ratios of participants diagnosed with hypertension over an average 3.98 years follow-up period as computed using Cox proportional-hazards models. There were total 12 732 cases of hypertension incidence over this study period. Among them,10 774 participants were <60 years old. The correlation between age category and sleep duration was significant (P<0.001). Analysis in the unadjusted data using Model 1 (ages between 18 and 98) indicated that participants of ⩽5 h group were more likely (HR, 1.11; 95% CI, 1.03–1.20) to develop hypertension than those of 7 h group. However, these results varied with the age. The incidence of hypertension was significantly high in younger participants who slept ⩽5 h per night (HR, 1.18; 95% CI, 1.08–1.28).
The significance of the association between short sleep duration and hypertension incidence was attenuated after adjustment of age, body mass index, RHR, smoking, alcohol drinking, physical activity, salt intake, gender, history of diabetes and hyperlipidemia, and antidiabetic and cholesterol-lowering medication (HR,1.06; 95% CI, 0.98–1.14; Table 2). The Same result was seen in the Model 3 following additional adjustment of baseline blood pressure level. However, the results also revealed an age-dependent tendency. Younger participants of ⩽5 h group aged <60 were significantly more likely (HR, 1.11; 95% CI, 1.02–1.21) to develop hypertension than participants who got 7 h of sleep. The older participants (ages⩾ 60) who slept ⩽5 h were less likely (HR, 0.91; 95% CI, 0.75–1.10) to develop hypertension.
Table 4 showed the HRs of women and men who developed hypertension during 3.98-year follow-up. Women who reported sleeping ⩽5 h per night were significantly more likely (HR, 1.27; 95% CI, 1.02–1.58; model3) to develop hypertension than the participants who reported getting 7 h of sleep per night, whereas men who slept ⩽5 h were actually slightly less likely (HR, 1.02; 95% CI, 0.94–1.12; model3) to develop hypertension.
After adjusting all the variables in the Model 3, significant interaction of sleep duration with gender/age was found in their effects on the incident hypertension (P<0.0001).
Discussion
We observed an association between short sleep duration and the incident hypertension in a large prospective cohort study in China. The participants aged <60 years at baseline who reported an average sleeping ⩽5 h per night had an increased risk for developing hypertension during the up to 3.98 years follow-up period. We failed to detect the association between sleep duration and incident hypertension in the participants aged ⩾60 years at baseline. Moreover, Sex-stratified analysis showed a marked association of sleep duration with incident hypertension in women participants. In addition, our data showed that long sleep duration of⩾9 h per night was not associated with hypertension incidence in the Chinese population.
Gangwisch et al.8 reported that sleep durations of ⩽5 h per night were associated with a significantly increased risk of hypertension in participants aged 32–59 years, but the sleep duration and incident hypertension were not related in people aged ⩾60 years. Our findings are in agreement with this result. Some factors may explain the differential association between short sleep duration and the incident hypertension in the younger and older age groups. First, participants experiencing hypertension, obesity and diabetes would be less likely to survive into their later years. Second, sleep-disordered breathing was associated with hypertension in participants below ages of 60 but not in those aged 60 or older.25 Third, advanced age is associated with changes in sleep architecture with increased difficulties in sleep initiation and maintenance.26 Elderly participants, who are often retired, also have more opportunities to take midday naps. In addition, the number of recruited older participants was smaller than that of younger participants. Therefore, lack of an association between short sleep duration and incident hypertension in the older participants could be due to a lower statistical power and resulted high probability of a type II error to detect the difference.
In contrast to our study, Miguel-Angel and co-workers27 reported an association between sleep-breathing disorders and cardiovascular diseases in elderly subjects. The discrepancy may be due to the difference of study population. Their participants were all patients diagnosed with obstructive sleep apnea syndrome (OSAS), while our data were obtained from the general population in China. Moreover, a study conducted by Gangwisch et al.24 showed that short sleep duration was associated with mortality in elderly but not in middle-aged adults. There may be two possible explanations for this discrepancy. First, our study did not observe an association between sleep duration and incident hypertension in elderly because the number of older participants was relatively smaller than that of younger participants, which resulted in a lower statistical power. Second, in Gangwisch’s study,24 the association between short sleep duration and mortality was only modestly attenuated when hypertension was included in Model 3 compared with Model 2. The slight changes in the HRs could be due to the fact that the sleep duration was not associated with incident hypertension in elderly subjects in the study by Gangwisch et al.8
The Whitehall II Study reported by Cappuccio et al.21 presented a gender-specific association of short sleep duration with prevalent and incident hypertension in a London population. Specifically, their cross-sectional analyses showed a significant association between short sleep duration (⩽5 h per night) and risk of hypertension only among women, which was attenuated in prospective analyses after multivariate adjustment. However, in our findings, this association was sustained after taking into account potential confounders. Women who sleep 6 or 8 h per night had also increased risk of incident hypertension, when compared with those who slept 7 h. In addition, Cappuccio et al.21 did not observe an association between sleep duration and incident hypertension in men, which is consistent with our finding. There may be two possible explanations for this discrepancy in men and women. First, female participants (mean age: 49 years) were around the premenopausal period. Women in premenopausal period are associated with major hormonal turmoil and psychosocial stresses that may in turn lead to hypertension.28 Second, sleep problems are particularly common in people with anxiety, depression, bipolar disorder and attention deficit. Compared with men, women are more likely to develop depression. Therefore, factors like depression may have impact on the gender-specific associations.
Gottlieb et al.7 reported that sleep durations of ⩾9 h per night were associated with a significantly increased risk of hypertension in participants aged 40–100 years. However, our study did not observe this association, as well as in the NHANES I study.8
The biological mechanisms behind the association of short sleep duration and incident hypertension are still unclear. Sleep deprivation has been reported to cause an increase in sympathetic nervous system activity.16, 29 The sympathetic nervous system plays an important role in the regulation of arterial pressure, and increased sympathetic nervous system activity has been implicated as a contributor of hypertension in humans. Sleep restriction has also been shown to compromise insulin sensitivity29 and increase appetite by decreasing leptin and increasing ghrelin,30 which could eventually induce type 2 diabetes and obesity. Both type 2 diabetes and obesity are common risk factors for hypertension. Besides these, polymorphism of the glucocorticoid receptor gene,31 environment,32 unhealthy behavior or factors33 and depression34 were found to associate with incident hypertension through various different mechanisms.
The strengths of our study include a prospective cohort design, large sample size, Asian ethnicity of the participants and a broad spectrum of potential confounding parameters. However, potential limitations of our study should also be discussed here. One limit of this study is that all of participants in this study were from Kailuan community. Their educational and cultural background reflects a regional status in northeast China and is slightly different from the country as a whole. The second limit is that our study did not assess the OSAS, so we did not exclude participants with OSAS. OSAS was found to associate with hypertension by various different mechanisms. Apnea-induced hypoxia, hypercapnia, micro-arousals, sympathetic hyperactivity, oxidative stress and hyper-coagulability play a central role in the increase of arterial blood pressure.35 The third limit is that the information on sleep duration was collected by self-reported questionnaire without more detailed and objective measures of sleep, such as actigraphic or polysomnographic measures. In addition, data of midday nap assessment were not undertaken in our study. Thus, nocturnal sleep duration may be different from the whole day sleep duration, especially in China where napping is not unusual. Another limit is that we did not collect sufficient information on the pre- or post-menopause status of women, which appears to be an important determinant of hypertension in women.28
Conclusions
In summary, our findings from the Kailuan cohort study suggest that short sleep duration could cause an increased risk of hypertension in Chinese females and population aged <60 years. Further investigations are needed to provide reliable evidence for sleep behavioral interventions by investigating the biological mechanisms that link short sleep duration to incident hypertension.

References
Hajjar I, Kotchen TA . Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA 2003; 290 (2): 199–206.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42 (6): 1206–1252.
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ . Selected major risk factors and global and regional burden of disease. Lancet 2002; 360 (9343): 1347–1360.
Lawes CM, Vander Hoorn S, Rodgers A . Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371 (9623): 1513–1518.
Wolk R, Gami AS, Garcia-Touchard A, Somers VK . Sleep and cardiovascular disease. Curr Prob Cardiol 2005; 30 (12): 625–662.
Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 2003; 26 (2): 380–384.
Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep 2006; 29 (8): 1009–1014.
Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension 2006; 47 (5): 833–839.
Kohatsu ND, Tsai R, Young T, Vangilder R, Burmeister LF, Stromquist AM et al. Sleep duration and body mass index in a rural population. Arch Intern Med 2006; 166 (16): 1701–1705.
Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB . Association between reduced sleep and weight gain in women. Am J Epidemiol 2006; 164 (10): 947–954.
Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB . Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep 2005; 28 (10): 1289–1296.
Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE et al. A prospective study of sleep duration and mortality risk in women. Sleep 2004; 27 (3): 440–444.
Lusardi P, Mugellini A, Preti P, Zoppi A, Derosa G, Fogari R . Effects of a restricted sleep regimen on ambulatory blood pressure monitoring in normotensive subjects. Am J Hypertens 1996; 9 (5): 503–505.
Kato M, Phillips BG, Sigurdsson G, Narkiewicz K, Pesek CA, Somers VK . Effects of sleep deprivation on neural circulatory control. Hypertension 2000; 35 (5): 1173–1175.
Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol 2004; 43 (4): 678–683.
Lusardi P, Zoppi A, Preti P, Pesce RM, Piazza E, Fogari R . Effects of insufficient sleep on blood pressure in hypertensive patients: a 24- h study. Am J Hypertens 1999; 12 (1 Pt 1): 63–68.
Azadbakht L, Kelishadi R, Khodarahmi M, Qorbani M, Heshmat R, Motlagh ME et al. The association of sleep duration and cardiometabolic risk factors in a national sample of children and adolescents: the CASPIAN III study. Nutrition 2013; 29 (9): 1133–1141.
Javaheri S, Storfer-Isser A, Rosen CL, Redline S . Sleep quality and elevated blood pressure in adolescents. Circulation 2008; 118 (10): 1034–1040.
Paciencia I, Barros H, Araujo J, Ramos E . Association between sleep duration and blood pressure in adolescents. Hypertens Res 2013; 36 (8): 747–752.
Guo X, Zheng L, Li Y, Yu S, Liu S, Zhou X et al. Association between sleep duration and hypertension among Chinese children and adolescents. Clin Cardiol 2011; 34 (12): 774–781.
Cappuccio FP, Stranges S, Kandala NB, Miller MA, Taggart FM, Kumari M et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension 2007; 50 (4): 693–700.
Kim SJ, Lee SK, Kim SH, Yun CH, Kim JH, Thomas RJ et al. Genetic association of short sleep duration with hypertension incidence—a 6-year follow-up in the Korean genome and epidemiology study. Circulation J 2012; 76 (4): 907–913.
Wang A, Liu X, Guo X, Dong Y, Wu Y, Huang Z et al. Resting heart rate and risk of hypertension: results of the Kailuan cohort study. J Hypertens 2014; 32 (8): 1600–1605 Discussion 5.
Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Opler MG et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep 2008; 31 (8): 1087–1096.
Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation 2005; 111 (5): 614–621.
Prinz PN . Age impairments in sleep, metabolic and immune functions. Exp Gerontol 2004; 39 (11-12): 1739–1743.
Martinez-Garcia MA, Campos-Rodriguez F, Catalan-Serra P, Soler-Cataluna JJ, Almeida-Gonzalez C, De la Cruz Moron I et al. Cardiovascular mortality in obstructive sleep apnea in the elderly: role of long-term continuous positive airway pressure treatment: a prospective observational study. Am J Respir Crit Care Med 2012; 186 (9): 909–916.
Stranges S, Dorn JM, Cappuccio FP, Donahue RP, Rafalson LB, Hovey KM et al. A population-based study of reduced sleep duration and hypertension: the strongest association may be in premenopausal women. J Hypertens 2010; 28 (5): 896–902.
Spiegel K, Leproult R, Van Cauter E . Impact of sleep debt on metabolic and endocrine function. Lancet 1999; 354 (9188): 1435–1439.
Spiegel K, Tasali E, Penev P, Van Cauter E . Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004; 141 (11): 846–850.
Yan YX, Dong J, Wu LJ, Shao S, Zhang J, Zhang L et al. Associations between polymorphisms in the glucocorticoid-receptor gene and cardiovascular risk factors in a Chinese population. J Epidemiol 2013; 23 (5): 389–395.
Yan YX, Dong J, Liu YQ, Zhang J, Song MS, He Y et al. Association of suboptimal health status with psychosocial stress, plasma cortisol and mRNA expression of glucocorticoid receptor alpha/beta in lymphocyte. Stress 2015; 18 (1): 29–34.
Gao J, Sun H, Liang X, Gao M, Zhao H, Qi Y et al. Ideal cardiovascular health behaviors and factors prevent the development of hypertension in prehypertensive subjects. Clin Exp Hypertens 2015; 37: 1–6.
Li Z, Yang X, Wang A, Qiu J, Wang W, Song Q et al. Association between ideal cardiovascular health metrics and depression in Chinese population: a cross-sectional study. Sci Rep 2015; 5: 11564.
Kario K . Obstructive sleep apnea syndrome and hypertension: mechanism of the linkage and 24- h blood pressure control. Hypertens Res 2009; 32 (7): 537–541.
Acknowledgements
We thank all study participants, their relatives, the members of the survey teams at the 11 regional hospitals of the Kailuan Medical Group, and the project development and management teams at the Beijing Tiantan hospital and the Kailuan Group.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Song, Q., Liu, X., Wang, X. et al. Age- and gender-specific associations between sleep duration and incident hypertension in a Chinese population: the Kailuan study. J Hum Hypertens 30, 503–507 (2016). https://doi.org/10.1038/jhh.2015.118
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2015.118
- Springer Nature Limited
This article is cited by
-
Sleep duration, hypnotic drug use, and risk factors: cross- sectional study
Scientific Reports (2023)
-
The association between sleep duration and hypertension: a meta and study sequential analysis
Journal of Human Hypertension (2021)
-
Effects of sleep deprivation on endothelial function in adult humans: a systematic review
GeroScience (2021)
-
Sleep and hypertension
Sleep and Breathing (2020)
-
Correlation between sleep duration and hypertension: a dose-response meta-analysis
Journal of Human Hypertension (2019)