Abstract
Several studies analyzed 25-hydroxyvitamin D (25[OH]D) and blood pressure (BP) relationship with mixed results. Moreover, a relationship between the risk of hypertension and vitamin D receptor (VDR) gene polymorphisms, FokI and BsmI, was reported. This study was aimed to analyze these relationships in essential hypertensive (EH) patients. Seventy-one EH patients, 18–75 years old, were enrolled. Patients underwent clinical BP, 24-h ambulatory BP monitoring, 25[OH]D and plasma renin activity (PRA) evaluations. FokI and BsmI VDR polymorphisms were analyzed and compared with those of 72 healthy controls. In EH patients, the median 25[OH]D levels were lower than 30 ng ml−1. We found a significant negative correlation between 25[OH]D and 24-h systolic BP (r=−0.277, P=0.043). This correlation persisted in backward stepwise multivariate analyses (β=−0.337; P=0.022), after adjustment for age, gender, body mass index, glomerular filtration rate, and PRA. We did not observe statistically significant correlation between 25[OH]D and PRA. We compared the allelic frequencies and genotype distribution between patients and controls, and FokI and BsmI VDR polymorphisms were not associated either with hypertensive status or with PRA. Further wide studies are needed to clarify this relationship.
Similar content being viewed by others
Introduction
The hormone 1,25-dihydroxyvitamin D (1,25[OH]2D) is known for its important role in regulating body levels of calcium and phosphorus and in modulating bone mineralization.1
In addition to classic functions, it is implicated in endothelial function, vascular smooth muscle cell proliferation and probably blood pressure (BP) regulation.2 Experimental studies showed that 1,25[OH]2D is a negative endocrine regulator of renin–angiotensin–aldosterone system (RAAS)3 that acts by inhibiting the renin mRNA expression. This repression is independent of calcium metabolism, volume- and salt-sensing mechanisms, and angiotensin II feedback regulation.3
Actually, 1,25[OH]2D is the biologically active form of Vitamin D obtained from 25-hydroxyvitamin D (25[OH]D) hydroxylation by 1α-hydroxylase, and 25[OH]D is the best indicator of vitamin D status. Indeed, the 1,25[OH]2D concentrations are often normal or increased in patients with Vitamin D deficiency as a result of elevated levels of parathyroid hormone. In addition, the half-life of circulating 1,25[OH]2D is only 4–6 h, whereas the half-life of circulating 25[OH]D is about 2–3 weeks.4, 5
Optimal 25[OH]D levels in healthy persons have not been precisely defined. Many authors suggest that sufficient concentrations begin at 30 ng ml−1, whereas values between 29 and 21 ng ml−1 are considered as insufficient, and that levels below 20 ng ml−1 are indicative of Vitamin D deficiency.6, 7, 8, 9, 10
Biological activities of 1,25[OH]2D are mediated by high-affinity receptors, and polymorphisms in the gene-encoding vitamin D receptor (VDR) appear to predispose the onset of hypertension.11, 12, 13
The most studied VDR polymorphisms are FokI and BsmI. FokI polymorphism consists of a T to C transition that alters the start codon and modifies the length of the VDR protein. The result is a more active transcription factor. BsmI is a A to G nucleotide substitution located in intron 8 that affects the transcript stability. It is in linkage disequilibrium with other polymorphisms and his association with some diseases is likely due to this phenomenon.14
Both of these polymorphisms have been associated with the risk for essential hypertension with mixed results.11, 12, 13, 15 However, the number of studies conducted in this regard is still low.
Moreover, several clinical studies showed an inverse association between low serum 25[OH]D concentration and high BP,16, 17, 18, 19, 20, 21 whereas other investigations were in contrast with those results.22, 23, 24
The purpose of our study was to analyze the relationship between 25[OH]D serum levels and clinic and 24-h ambulatory BP values in essential hypertensive (EH) patients, and to identify any possible association between hypertension and the VDR gene polymorphisms FokI and BsmI.
Materials and methods
In accordance with the Declaration of Helsinki and institutional guidelines, the protocol was approved by the local ethical committee, and patients were aware of the investigational nature of the study and agreed to participate after informed consent.
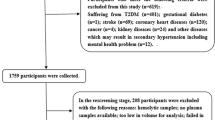
In 71 EH patients, aged 18–75 years, clinical BP, 24-h ambulatory BP monitoring, routine blood chemistry, 25[OH]D plasma level and plasma renin activity (PRA) were studied. Furthermore, FokI and BsmI VDR polymorphisms were analyzed and compared with those of 72 controls, blood donors, matched for age and sex, from the same geographical area.
Exclusion criteria were: secondary or malignant hypertension, diabetes or fasting glycaemia ⩾126 mg dl−1, heart failure, positive history or clinical signs of ischemic heart disease, cerebrovascular disease, chronic kidney disease and major noncardiovascular diseases.
All patients taking antihypertensive drugs underwent pharmacological washout for at least 2 weeks.
A careful clinical physical examination was carried out and anthropometric parameters (weight, height, body mass index (BMI) and waist circumference) were measured.
Clinic BP was recorded in a seated posture by a doctor. It was taken as the average of three consecutive measurements obtained using an automated sphygmomanometer, after the patient had rested for 5 min.
The 24-h ambulatory BP monitoring was performed using a non-invasive SpaceLabs 90207 recorder (Redmond, WA, USA). Only records with >80% valid data were accepted.
Subjects were instructed to ingest a diet containing 130–140 mmol per day of sodium and 40–50 mmol per day of potassium before the biochemical evaluation.
After an overnight fast of at least 10 h and after resting for 1 h in the supine position, patients underwent blood sampling for routine blood chemistry, 25[OH]D, PRA and VDR genotype determination.
Determination of routine biochemical parameters was performed with standard techniques by using an autoanalyzer (Hitachi system 911, Boehringer Mannheim, Mannheim, Germany).
Glomerular filtration rate was estimated by both Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI)25 equation and simplified Modification of Diet in Renal Disease (MDRD) Study prediction equation.26
PRA was determined as angiotensin-I generation rate and expressed as nanograms of angiotensin-I generation per milliliter of plasma per hour of incubation (ng ml−1 per h). It was measured by radioimmunoassay with commercially available kit (RENCTK for the former), purchased from Sorin Biomedica Diagnostics (Saluggia, Italy).
Serum 25[OH]D was determined by high-performance liquid chromatography (HPLC), using the 25-OH-Vitamin D2/D3 kit from Chromsystems Instruments & Chemicals GmbH (Gräfelfing, Munich, Germany) on the Waters 1525 Binary HPLC Pump, the latter equipped with UV detector and injection valve. The conditions of chromatographic separation were as follows: C18 analytical column, column temperature 25 °C, flow rate 0.7 ml min−1, wavelength 265 nm and sample injection volume 50 μl. Chromatographic separation was performed with isocratic elution. Chromatographic analysis took ~12 min with retention times, respectively, of 4.2 min for 25[OH]D3 and 4.6 min 25[OH]D2.
The FokI and BsmI VDR gene polymorphisms were analyzed by PCR–RFLP. The DNA was extracted from peripheral blood with standard methods using QIAamp DNA Blood mini kit (Qiagen GmbH, Hilden, Germany). DNA amplification was carried out on a thermal cycler. Subsequently, VDR gene polymorphisms were typed by restriction enzyme digestion. The digested samples were analyzed by electrophoresis on 2% agarose gel.
Statistics
Statistical analysis was conducted using SYSTAT DATA software package, version 13 (Systat, San Jose, CA, USA).
Normal distribution of the continuous variables was assessed using the Kolmogorov–Smirnov test.
Non-Gaussian distribution was observed for all of the examined variables. For this reason, we analyzed these data using non-parametric tests.
The continuous variables are represented as median and interquartile range.
Differences among groups were evaluated using Kruskal–Wallis test and Mann–Whitney U-test for continuous variables.
We examined univariate associations between 25[OH]D and both clinic and 24-h ambulatory BP, and between these parameters and other variables using Pearson correlation coefficients. Backward stepwise multiple linear regression analysis was used to assess the independent correlates of 24-h systolic BP (SBP), using 24-h SBP as a dependent variable, and 25[OH]D, age, sex, BMI and estimated glomerular filtration rate (eGFR) as covariates. In another multivariate analysis the covariates were 25[OH]D, PRA, BMI and eGFR(MDRD).
Any association between a specific genotype or allele and hypertension was investigated using the χ2-test.
Hardy–Weinberg equilibrium was assessed by χ2-test.
A two-tailed P<0.05 was considered statistically significant.
Results
The characteristics of the hypertensive patients are given in Table 1.
It is of note that median 25[OH]D levels were lower than 30 ng ml−1, a value to date considered as normal cutoff, notwithstanding a normal median eGFR value and a good sun exposure favored by geographical area of origin.
Table 2 shows the univariate correlations between 25[OH]D and both clinic and 24-h ambulatory BP. We observed a significant negative correlation between 25[OH]D and 24-h SBP (r=−0.277, P=0.043; Figure 1).
This correlation persisted in backward stepwise multivariate analysis considering 24-h SBP as a dependent variable (β=−0.337; P=0.022) and including in the statistical model 25[OH]D, age, gender, BMI and eGFR(MDRD). BMI (β=0.290; P=0.037) and eGFR(MDRD; β=−0.301; P=0.038) were independently correlated to 24-h SBP, as well.
The inverse correlation between 25[OH]D and 24-h SBP persisted also when the covariates considered in multiple regression analysis were 25[OH]D, PRA, BMI and eGFR(MDRD).
We did not observe statistically significant correlation between 25[OH]D and PRA (r=0.192, P=0.173).
Successively, EH patients were grouped on the basis of VDR genotypes (Table 3), and the anthropometric, clinical and biohumoral parameters were compared.
There were no differences in age, gender, BMI, eGFR(MDRD), eGFR(CKD-EPI), calcium, phosphorus, 25[OH]D, parathormone, PRA, 24-h SBP, diastolic BP (DBP), mean and pulse BP and clinic SBP among patients with different FokI genotype.
We observed a significant difference in clinic DBP among the three FokI genotypes (P=0.018). The Mann–Whitney U-test disclosed significantly higher DBP values in patients with ff FokI genotype compared with those with Ff FokI genotype (P=0.002; Figure 2).
Box plots showing clinic diastolic blood pressure in hypertensive patients, grouped in the FokI genotypes. In the box-and-whisker plots, the central boxes represent the values from the lower to upper quartile (25–75 percentile). The middle lines represent the medians. Lower and upper whiskers extend to 5th and 95th percentiles.
No difference was found regarding age, gender, BMI, eGFR(MDRD), eGFR(CKD-EPI), calcium, phosphorus, 25[OH]D, parathormone, PRA, clinic and 24-h ambulatory BP among patients with different BsmI genotypes.
When the correlation analysis was applied in the subgroups with different FokI and BsmI genotype, we observed significant negative correlations between 25[OH]D and 24-h pulse BP in patients with Ff FokI genotype (r=−0.474, P=0.035) and between 25[OH]D and 24-h SBP in patients with Bb BsmI genotypes (r=−0.397, P=0.020).
We compared allelic frequencies and genotype distribution between 71 patients and 72 controls (Table 3). FokI and BsmI genotypes were in Hardy–Weinberg equilibrium.
We did not find any association between a specific genotype or allele and hypertension. Moreover, no association between polymorphisms and PRA was pointed out.
Discussion
The results of our study show that in EH patients VDR FokI and BmsI polymorphisms are not associated either with hypertensive status or with PRA, notwithstanding low 25[OH]D levels, correlating inversely with 24-h SBP.
Indeed, in 71 EH patients we observed a significant negative correlation between 25[OH]D and 24-h SBP, independently of age, gender, BMI and eGFR(MDRD), and PRA.
Our results are in part in line with wider observational studies that evaluated 25[OH]D and BP relationship.
In 12 644 NHANHES III subjects, Scragg et al.19 found SBP values 3 mm Hg lower in the highest quintile of 25[OH]D (>85.7 nmol l−1) compared with the lowest quintile.
Moreover, Forman et al.20 examined the relationship between 25[OH]D concentrations and incidence of hypertension in 1198 women from the Nurses' Health Study and 613 men from the Health Professionals' Follow-Up Study without history of hypertension. The relative risk of incident hypertension was, respectively, 6.13 and 2.67 among men and women with 25[OH]D levels <15 ng ml−1 compared with those having levels ⩾30 ng ml−1.
In addition, the same author performed a case–control study in 1484 women and he observed that plasma levels of 25[OH]D were inversely and independently associated with the risk of developing high BP.21
In contrast to these data, in other studies the relationship between 25[OH]D concentrations and BP values was not observed.22, 23, 24 However, most of them were characterized by a limited number of population samples. Furthermore, it is noteworthy that only a poor percentage of patients of the study populations had vitamin D deficiency.22
Several mechanisms have been postulated to explain the relationship between Vitamin D and BP, including regulatory action on proinflammatory cytokines, direct effect on vascular wall and upregulation of RAAS, the latter reported in studies in knockout mice for VDR.3
It has been hypothesized that Vitamin D is a negative regulator of renin expression in vivo in humans.27 In the hypertensive patients group we found low PRA and 25[OH]D levels, and we did not observe any relationship between 25[OH]D and PRA.
Although RAAS regulation by 1,25[OH]2D has been demonstrated in vitro and in mice,3 humans data are few and contradictory.
Several years ago, in 51 EH patients Resnick et al.28 observed a continuous relationship between calcitriol levels and PRA.
In 184 normotensive individuals, Forman et al.27 found higher PRA levels among those with 25[OH]D deficiency and insufficiency; however, the association was not statistically significant.
This is in line with our results, and it could be owing to the fact that the mechanisms of cell or tissue renin–angiotensin–aldosterone regulation by Vitamin D do not mirror sharply the systemic phenomena.
In recent years, several VDR polymorphisms have been identified and it has shown the existence of the possible relationships between these genetic variants and the risk for developing arterial hypertension.
The study by Muray et al.11 was one of the first to highlight an association of BsmI genotype and BP, observing SBP values higher in apparently healthy men with bb genotype, than in the other genotypes. Neverthless, in healthy female genotypes were not associated with BP.
Another VDR polymorphism called into question is FokI, analyzed by Swapna et al.12 who compared 280 hypertensive patients and 200 healthy controls and observed an association between the FF genotype and the risk for developing EH.12
The existence of a relationship between the development of hypertension and FokI and BsmI VDR polymorphisms was also shown in a prospective study conducted by Wang et al.13 in 1211 men free from hypertension at baseline, followed up for 15.3 years. Subjects with BB or Bb genotype had a hazard ratio for hypertension of 1.25 compared with bb genotype; with regard to FokI, men with ff genotype had a hazard ratio of 1.32 compared with FF and Ff carriers. In the same cohort an inverse association between 25[OH]D and risk of hypertension was also observed.
Further, an association between FokI and PRA in combination with 25[OH]D levels was demonstrated in hypertensive and normotensive individuals from the HyperPath cohort.29
Our results do not confirm neither the existence of an association between VDR polymorphisms and hypertension, nor between these polymorphisms and PRA.
Indeed, very recently, a comprehensive genetic association study in a very wide population of men and women did not replicate the previously reported association between vitamin D-related single nucleotide polymorphisms and BP.15
To the best of our knowledge, this is one of the few studies that comprehensively analyzes the relationship between BP, PRA, 25[OH]D and the polymorphisms of the VDR, FokI and BsmI, in EH patients.
According to recent hypotheses, low 25[OH]D levels lead to an upregulation of the RAAS, thus favoring the increase in BP.
In our study, although we found low 25[OH]D values in EH patients and a statistically significant relationship between 25[OH]D and 24-h SBP, we did not observe any correlation between 25[OH]D and PRA.
However, our study has some limitations, such as the small size sample, the observational nature and the unavailability of the PRA and 25[OH]D values in the polymorphism control group.
In conclusion, although some studies have confirmed the existence of an association between VDR polymorphisms and the risk of hypertension, the comprehensive results do not seem to be conclusive and further wide studies are needed to clarify this relationship.

References
Dusso AS, Brown AJ, Slatopolsky E . Vitamin D. Am J Physiol Renal Physiol 2005; 289: F8–F28.
Almirall J, Vaqueiro M, Baré ML, Anton E . Association of low serum 25-hydroxyvitamin D levels and high arterial blood pressure in the elderly. Nephrol Dial Transplant 2010; 25: 503–509.
Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP . 1,25-Dihydroxyvitamin D3 is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest 2002; 110: 229–238.
Hollis BW, Wagner CL, Drezner MK, Binkley NC . Circulating Vitamin D3 and 25-hydroxyvitamin D in Humans: An Important Tool to Define Adequate Nutritional Vitamin D Status. J Steroid Biochem Mol Biol 2007; 103 (3–5): 631–634.
Holick MF . Vitamin D status: measurement, interpretation and clinical application. Ann Epidemiol 2009; 19 (2): 73–78.
Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B . Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr 2006; 84 (1): 18–28.
Holick MF . Vitamin D deficiency. N Engl J Med 2007; 357: 266–281.
Holick MF . High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc 2006; 81: 353–373.
Malabanan A, Veronikis IE, Holick MF . Redefining vitamin D insufficiency. Lancet 1998; 351: 805–806.
Thomas MK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska DJ, Kitch BT et al. Hypovitaminosis D in medical inpatients. N Engl J Med 1998; 338: 777–783.
Muray S, Parisi E, Cardús A, Craver L, Fernández E . Influence of vitamin D receptor gene polymorphisms and 25-hydroxyvitamin D on blood pressure in apparently healthy subjects. J Hypertens 2003; 21 (11): 2069–2075.
Swapna N, Vamsi UM, Usha G, Padma T . Risk conferred by FokI polymorphism of vitamin D receptor (VDR) gene for essential hypertension. Indian J Hum Genet 2011; 17 (3): 201–206.
Wang L, Ma J, Manson JE, Buring JE, Gaziano JM, Sesso HD . A prospective study of plasma vitamin D metabolites, vitamin D receptor gene polymorphisms, and risk of hypertension in men. Eur J Nutr 2013; 52 (7): 1771–1779.
Lins LR, Nogueira LR, Lima RM, Gentil P, Oliveira RJ, Pereira RW . A multiplex single-base extension protocol for genotyping Cdx2, FokI, BsmI, ApaI, and TaqI polymorphisms of the vitamin D receptor gene. Genet Mol Res 2007; 6 (2): 316–324.
Wang L, Chu A, Buring JE, Ridker PM, Chasman DI, Sesso HD . Common genetic variations in the vitamin D pathway in relation to Blood Pressure. Am J Hypertens 2014; 27 (11): 1387–1395.
Feneis JF, Arora RR . Role of vitamin D in blood pressure homeostasis. Am J Ther 2010; 17 (6): e221–e229.
Demir M, Günay T, Özmen G, Melek M . Relationship between vitamin d deficiency and nondipper hypertension. Clin Exp Hypertens 2013; 35 (1): 45–49.
Moyano Peregrín C, López Rodríguez F, Castilla Castellano Mdel M . Vitamin D and hypertension. Med Clin (Barc) 2012; 138 (9): 397–401.
Scragg R, Sowers M, Bell C . Serum 25-hydroxyvitamin D, ethnicity, and blood pressure in the Third National Health and Examination Survey. Amer J Hypertens 2007; 20: 713–719.
Forman JP, Giovannucci E, Holmes MD, Bischoff-Ferrari HA, Tworoger SS, Willett WC et al. Plasma 25-hydroxyvitamin D levels and risk of incident hypertension. Hypertension 2007; 49 (5): 1063–1069.
Forman JP, Curhan GC, Taylor EN . Plasma 25-hydroxyvitamin D levels and risk of incident hypertension among young women. Hypertension 2008; 52 (5): 828–832.
Snijder MB, Lips P, Seidell JC, Visser M, Deeg DJ, Dekker JM et al. Vitamin D status and parathyroid hormone levels in relation to blood pressure: a population-based study in older men and women. J Intern Med 2007; 261 (6): 558–565.
Scragg R, Holdaway I, Singh V, Metcalf P, Baker J, Dryson E . Serum 25-hydroxycolecalciferol concentration in newly detected hypertension. Am J Hypertens 1995; 8: 429–432.
Rueda S, Fernández-Fernández C, Romero F, Martínez de Osaba J, Vidal J . Vitamin D, PTH, and the metabolic syndrome in severely obese subjects. Obes Surg 2008; 18: 151–154.
Levey A, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150: 604–612.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D . A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999; 130: 461–470.
Forman JP, Williams JS, Fisher ND . Plasma 25-Hydroxyvitamin D and regulation of the renin-angiotensin system in humans. Hypertension 2010; 55: 1283–1288.
Resnick LM, Müller FB, Laragh JH . Calcium-regulating hormones in essential hypertension. Relation to plasma renin activity and sodium metabolism. Ann Intern Med 1986; 105 (5): 649–654.
Vaidya A, Sun B, Forman JP, Hopkins PN, Brown NJ, Kolatkar NS et al. The FOK1 Vitamin D receptor gene polymorphism is associated with plasma renin activity in caucasians. Clin Endocrinol (Oxf) 2011; 74 (6): 783–790.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cottone, S., Guarino, L., Arsena, R. et al. Vitamin D receptor gene polymorphisms and plasma renin activity in essential hypertensive individuals. J Hum Hypertens 29, 483–487 (2015). https://doi.org/10.1038/jhh.2014.113
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2014.113
- Springer Nature Limited
This article is cited by
-
Fok I and Bsm I gene polymorphism of vitamin D receptor and essential hypertension: a mechanistic link
Clinical Hypertension (2023)
-
Low serum 25-hydroxyvitamin D levels may increase the detrimental effect of VDR variants on the risk of essential hypertension
European Journal of Clinical Nutrition (2020)