Abstract
Early studies have investigated the effect of prenatal cadmium (Cd) exposure on birth outcomes, such as preterm birth and low birth weight, although the results of these studies are inconsistent. The aim of the present study was to investigate the association between prenatal exposure to Cd and the risk of preterm low birth weight (PLBW). A total of 408 mother–infant pairs (102 PLBW cases and 306 pair matched controls) were selected from the participants enrolled in the Healthy Baby Cohort (HBC) study between 2012 and 2014 in Hubei province, China. Concentrations of Cd in maternal urine collected before delivery were measured by inductively coupled plasma mass spectrometry and adjusted by creatinine. A significant association was observed between higher maternal urinary Cd levels and risk of PLBW (adjusted odds ratio (OR)=1.75 for the medium tertile, 95% confidence interval (CI): 0.88, 3.47; adjusted OR=2.51 for the highest tertile, 95% CI: 1.24, 5.07; P trend=0.03). The association was more pronounced among female infants than male infants. Our study suggested that prenatal exposure to Cd at the current level encountered in China may potentially increase the risk of delivering PLBW infants, particularly for female infants.
Similar content being viewed by others
INTRODUCTION
Cadmium (Cd), a well-known toxic heavy metal, is used extensively in metal plating, producing dyes and pigments.1 As a result of industry and agriculture development, Cd is ubiquitously distributed in the environment.2 Chronic Cd exposure has been shown to adversely affect kidney,2, 3 cardiovascular health4 and bone,5 and to increase the risk of overall cancer mortality.6
Pregnant women and their fetuses are especially susceptible to the effects of exposure to Cd, and Cd is known to accumulate in the human placenta.7, 8 Cd-related maternal and developmental toxicities have been observed in studies of experimental animals, including reduced fetal body weight, malformations and impaired neurobehavioral development.9, 10, 11, 12 However, the findings from epidemiological studies about associations between prenatal Cd exposure and adverse birth outcomes are inconsistent. Some studies have showed a significant association between prenatal Cd exposure and an increased risk of a premature labor or decreased birth weight.1, 13, 14, 15, 16 However, some studies have observed no such association.17, 18, 19, 20
Environmental Cd exposure has become a serious public health problem in China owing to the country’s rapid economic development and urbanization.21 In recent decades, more than 1.3 × 105 km2 of agricultural soils and 1.46 × 108 kg of agricultural products are reported to be polluted by Cd in China every year,22 and the occurrence of Cd-contaminated rice has become a serious food security problem.23 In China, limited information is available on Cd levels among pregnant women, and few studies have been conducted to investigate the impact of prenatal exposure to Cd on preterm low birth weight (PLBW). Under this background, we took advantage of the prospective birth cohort in Hubei province of China, and conducted a nested case–control study to investigate the relationship between prenatal Cd exposure and the risk of PLBW.
MATERIALS AND METHODS
Study Population and Data Collection
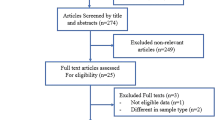
This study was conducted as a part of The Healthy Baby Cohort (HBC) study in China which is described elsewhere.24 Our cohort enrolled pregnant women at three major maternity hospitals in Wuhan, Ezhou and Macheng cities, located in Hubei province, central China. The participants were invited to finish a face-to-face interview and donate the maternal blood, urine and cord blood samples. All participants signed an informed consent form, and the study protocol was reviewed and approved by the ethical committee of School of Public Health and Tongji Medical College, Huazhong University of Science and Technology.
The PLBW cases were mothers who delivered a live singleton infant with a gestational age <37 weeks and weighing <2500 g. The controls were mothers who delivered a singleton live infant with gestational age ⩾37 weeks and weighting between ⩾2500 g and <4000 g. Women were excluded if they had multiple pregnancies, or gave birth to a stillborn infant or an infant with a birth defect. Women who had no maternal urine samples available for analysis were also excluded. For every case selected, three consecutive controls were selected randomly and matched by delivery hospital, maternal age and infant sex. A total of 102 cases and 306 controls were included in the analysis.
Trained nurses conducted standardized face-to-face interviews with the women after delivery. The interview was used to obtain a variety of information, including demographic and socioeconomic data, occupation, living environments, life style, reproductive history and drug history. Information concerning the mothers (history of pregnancy outcomes and disease) and newborns (including gestational age at birth, sex, birth weight and any apparent congenital malformations) were retrieved from the medical records. The gestational age was estimated based on the onset of the last menstrual period. Trained obstetric nurses measured the birth weight of nude infants within 1 h after birth.
Urine Sample Collection and Cd Measurements
All of the maternal urine samples were collected in the third trimester (within 3 days before delivery) and stored in polypropylene tubes at −20 °C until further analysis. Before the analysis, urine samples were thawed at room temperature. Then, 1 ml supernatant of urine samples and 4 ml of 3% HNO3 were added to a Kirgen polypropylene conical centrifuge tubes for overnight nitrification, and were further digested by ultrasound at 40 °C for 1 h. The Cd concentrations in urine samples were quantified by inductively coupled plasma mass spectrometry (Agilent 7700, Agilent Technologies, Santa Clara, CA, USA). The operation conditions of inductively coupled plasma mass spectrometry have been described elsewhere.24
All measurements were performed by the laboratory personnel blind to the status of the case and the control. The standard reference material human urine SRM2670a (National Institute of Standards and Technology, Gaithersburg, MD, USA), an external quality control sample, was used in each batch to assess the instrument performance, and the concentrations measured were within the certified range (5%). A 3% HNO3 blank was applied to each batch of samples to control for possible contamination. In this study, the limit of detection (LOD) for urine Cd was 0.01 μg/l, and the recovery of the quality control standard was 99%. Cd measurements below the LOD (n=1) were assigned a value of 1/2 LOD.
The measurement of urinary creatinine concentrations were measured by a creatinine kit (Mindray CREA Kit, Shenzhen, China) and an automatic biochemical analyzer (BS-200, Mindray, Shenzhen, China). Creatinine-adjusted Cd concentration for each urine sample was calculated as the measured Cd concentration divided by creatinine concentration and expressed as μg Cd per g creatinine (μg/g creatinine).
Statistical Analyses
The Kolmogorov–Smirnov normality test was used to test the distribution of Cd concentrations, which was found to be skewed. The differences of Cd levels in maternal urine between the case and control group were compared by the Wilcoxon matched pairs signed rank test. Conditional logistic regression analyses were performed to assess the associations between the risk of PLBW and maternal Cd exposure by estimating crude and adjusted matched odds ratios (ORs) and their 95% confidence intervals (CIs). In conditional logistic regression analyses, maternal urinary Cd concentrations were analyzed as categorical variables, based on the tertile distribution of urinary Cd levels in controls, and the lowest tertile was assigned as the referent group. In the final models, we adjusted for potential confounding variables, including maternal education (more than high school, high school education, less than high school), household yearly income (<50,000, ⩾50,000 RMB), pre-pregnancy body mass index (<18.5, 18.5–23.9, ⩾24 kg/m2), parity (1, ⩾2) and passive smoking (yes or no). Additional adjustment for occupational status during pregnancy did not result in material changes in the observed associations and thus were not included in the final models. Smoking and alcohol consumption was not included in our final model, because few mothers in our study reported smoking or drinking during pregnancy. The missing values were constructed as dummy variables in the regression model.25 We further did an additional analysis excluding the samples with missing values. If a case or a control has missing values, the matched case–control was excluded. We tested for linear trends of the risk of PLBW and urinary Cd levels by modeling the median values of tertiles of Cd as a continuous variable and used the Wald test to evaluate the statistical significance of this predictor.
The risk analyses were further stratified by infant sex and maternal age (<29, ⩾29 years). The median age (29 years) of the women at delivery in our study was used as the cut-point for stratified analyses, and the Breslow–Day test was used to evaluate the heterogeneity of effects by infant gender and maternal age. We defined statistical significance as a two-sided P value<0.05. All statistical data analyses were performed using SAS (version 9.3; SAS Institute, Cary, NC, USA).
RESULTS
The general characteristics of the 102 cases and 306 controls are presented in Table 1. Most of the participants were recruited from Wuhan (84.3%), while 8.9% were from Ezhou and 6.8% were from Macheng. There were 57 sets of male infants and 45 sets of female infants. The mean age of the women at delivery was 28.9±4.9 years, and the average pre-pregnancy BMI (kg/m2) of the cases and controls was 20.6±3.7 and 20.7±3.0, respectively. The proportion of mothers who had a low educational level (⩽9 years, 45.1% vs 19.6%) and reported lower household yearly income (<50,000 yuan, 64.7% vs 45.1%) was higher among the cases than the controls. There was also a higher percentage of case mothers who were passively exposed to cigarette smoking (27.5% vs 19.3%), and had two or more parities (25.5% vs 18.9%) compared with the controls. Only one mother in the case group self-reported smoking or alcohol consumption during pregnancy.
The detection rate for Cd in maternal urine was 99.8%. The median creatinine-adjusted Cd concentration in maternal urine was 0.60 μg/g creatinine with a range of <LOD to 5.61 μg/g creatinine in the cases, and a median of 0.48 μg/g creatinine with a range of <0.04 to 18.09 μg/g creatinine in the control mothers. The mothers in the case group had significantly higher urinary Cd levels compared with the control group (P<0.05).
Table 2 shows the association between the maternal urinary Cd levels and the risk of PLBW. Compared with the lowest tertile of urinary Cd concentrations, a significant trend was found between PLBW risk and increasing levels of Cd in the unadjusted analysis (OR=1.57 (95% CI=0.85–2.91) for the medium tertile; OR=2.25 (95% CI=1.21–4.17) for the highest tertile; P trend<0.01). Similarly, after controlling for the potential confounding factors, a significant dose–response relationship was observed between Cd levels and risk of PLBW (adjusted ORs=1.75 (95% CI=0.88–3.47) and 2.51 (95% CI=1.24–5.07) for the increasing tertiles, P trend=0.03). When 32 samples with missing values and their matched cases or controls were excluded (82 case–control pairs were included), the adjusted OR for PLBW associated with Cd exposure were almost unchanged (adjusted OR=1.90 (95% CI: 0.89–4.06) for the medium tertile and adjusted OR=2.59 (95% CI: 1.20–5.59) for the highest tertile, P trend=0.03) (Supplementary Material, Supplementary Table S1).
Results for stratified analyses by maternal age (<29 and ⩾29 years) are shown in Table 3. Among younger mothers <29 years old, a significant association was apparent for higher Cd concentrations and risk of PLBW infants (adjusted ORs=3.94 (95% CI=1.32–11.72) and 3.19 (95% CI=1.02–9.23) for the increasing tertiles; P trend=0.42). Among mothers ⩾29 years old, adjusted ORs were 1.07 (95% CI=0.40–2.84) for the median tertile and 2.29 (95% CI=0.85–6.15) for the highest tertiles (P trend=0.05). But the risk estimates for PLBW associated with Cd exposure were not significantly different among the two age groups (P heterogeneity=0.19).
Table 4 shows results stratified by infant sex. Among female infants, a significant positive association was observed for higher urinary Cd concentrations and the risk of PLBW (adjusted ORs=3.65 (95% CI=1.12–11.88) and 5.90 (95% CI=1.57–22.23) for the increasing tertiles; P trend=0.02). Among male infants, adjusted ORs were 1.83 (95% CI=0.73–4.58) and 2.13 (95% CI=0.81–5.63) for increasing tertiles (P trend=0.24), but the association was not significant. There was no significant interaction between maternal age and maternal urinary Cd levels (P heterogeneity=0.44).
DISCUSSION
Preterm birth (childbirth occurring at less than 37 completed weeks of gestation) is a major social and economic public health problem in both developed and developing countries.26 The majority of preterm births are also low birth weight infants (<2500 g),26 in which case it is referred to as PLBW. PLBW represents the major cause of neonatal morbidity and long-term disability among survivors.27 In this study, we found that there was a significant positive association between PLBW risk and increasing levels of maternal urinary Cd, and mothers in the highest tertile of urinary Cd levels (⩾0.70 μg/g creatinine) had more than two times the risk of delivering PLBW infants as those in the lowest tertile (<0.35 μg/g creatinine). These findings imply that maternal exposure to the current levels of Cd in China may potentially increase the risk of delivering PLBW infants.
In this study, Cd was detected in almost all of the maternal urine samples, indicating a wide exposure of Cd in our study population. A comparison of urinary Cd concentrations in pregnant women of the present study and previously published data on human exposure levels worldwide is shown in Table 5. Our population had higher concentrations of urinary Cd (median: 0.34 μg/l and 0.48 μg/g creatinine; geometrical mean (GM): 0.34 μg/l and 0.63 μg/g creatinine) than other non-occupationally exposed populations in the USA (median: 0.40 μg/g creatinine; GM: 0.38 μg/g creatinine),28 Spain (median: 0.23 μg/g creatinine; GM: 0.25 μg/g creatinine)29 and Germany (median: 0.18 μg/g creatinine; GM: 0.18 μg/g creatinine);30 whereas the levels of Cd observed in this study were lower than pregnant women from Australia (median: 0.66 μg/l),31 Bangladesh (median: 0.63 μg/l)15 and Japan (GM: 0.77 μg/g creatinine).32 The data about urinary Cd levels in Chinese pregnant women are currently limited. Only one study investigated Cd exposure in 209 pregnant women from two towns in Jiangsu province, China, and reported the GM of urinary concentrations of Cd in the third trimester was 0.13 μg/g creatinine16 that was a little lower than that observed in our present study. One possible explanation would be that the subjects in Sun’s study were residents in small towns, whereas most of our study subjects were residents in urban areas. Also, previous studies have reported a higher pollution rate of Cd in farmland soil in Hubei province, which might lead to an elevated Cd uptake through agricultural crops.33 All comparisons above suggested that the population in our study were exposed to a relatively high dose of Cd.
The associations between prenatal Cd exposure and adverse birth outcomes has been found in some of the previous studies.1, 13, 15, 16, 34 An early study by Nishijo et al.13 found that mothers with urinary Cd ⩾2 μg/g creatinine had higher rates of low birth weight or early delivery compared with mothers with urinary Cd<2 μg/g creatinine in 57 pregnant women in Japan. A mother–child cohort study in France by Menai et al.1 reported that maternal blood Cd levels were significantly associated with reduced birth weight in the offspring of women who smoked during pregnancy (β=−113.7; P=0.001) in a mother–child cohort study of 901 pregnant women in France. Similarly, a prospective cohort study of 1616 pregnant women in rural Bangladesh reported that maternal urinary Cd was significantly negatively associated with birth weight (β=–31.0; P=0.03).15 A recent study of 1027 pregnant women in North Carolina, USA, suggested that high maternal blood Cd levels (⩾0.50 μg/l) at delivery were inversely associated with birth weight percentile for gestational age and associated with increased odds of infants being born small for gestational age (OR=1.71; 95% CI, 1.10–2.64).34 Sun et al.16 conducted a cross-sectional study of 209 pregnant women living in Eastern China and reported that a significant negative correlation was found between maternal blood Cd and birth weight (r=−0.22; P=0.03). Consistent with these results, our findings also provide evidence of a positive association between maternal Cd exposure and risk of infant PLBW.
However, there were some inconsistent results of the relationship between maternal Cd exposure and birth weight from previous epidemiological studies. Lin et al.20 in a birth cohort study of 486 mother–infant pairs in Taiwan reported that there was a negative but no significant association between cord blood Cd and birth weight, probably owing to the low Cd exposure level in these population (cord blood Cd: median 0.33 μg/l). Zhang et al.19 also conducted a study with 44 mother–infant pairs in Hubei, China, but found that higher level of maternal blood Cd (>1.72 μg/l) was not associated with birth incidence rate of premature labor compared with lower maternal blood Cd level group (⩽1.72 μg/l). One possible explanation would be that their analysis of 44 subjects may have insufficient statistical power to detect a significant difference. In addition, the discrepant results of the association between prenatal Cd exposure and preterm or low birth weight may be induced by study design, differences in populations, use different biomarkers for exposure assessment or other factors.
In the present study, we found a possible sex difference in the association between maternal Cd exposure and risk of delivering a PLBW infant, which was more apparent in females. Consistent with our observations, Kippler et al.15 also found maternal urinary Cd was significantly negatively associated with birth size in girls, but not in boys in a prospective cohort study of 1616 pregnant women in rural Bangladesh. Cd has estrogen-like effects that may affect reproduction and fetal development.35, 36 Because a larger number of estrogen receptor-positive cells were observed in females than in males, the expression of estrogen receptor is strikingly different among females and males.37, 38 It is plausible that the risk of PLBW would have been more apparent in females. The other possible reason may be that Cd also interfere with the insulin-like growth factor (IGF) axis and thereby reduce fetal growth in a sex-specific manner.15 Rats treated with Cd through drinking water had significantly lower levels of IGF-1 and IGF-binding protein 3 (IGFBP-3) than did controls.39 Numerous studies have found that both IGF-1 and IGFBP-3 levels in pregnant women are usually positively associated with infant birth weight.40 Furthermore, previous epidemiologic studies have reported that IGF-I and IGFBP-3 concentrations in cord blood or cord plasma were higher in female neonates than males.41, 42 This reason may partly explain why a significant association between maternal Cd exposure and PLBW was more apparent in female infants than males. Further evaluation of potential differences in the effect of maternal Cd exposure on PLBW according to infant sex should be conducted in larger studies. In addition, we also found that the significant association between maternal urinary Cd levels and the risk of delivering a PLBW infant was more pronounced in younger mothers (<29 years old) compared with older mothers (⩾29 years old). A plausible explanation would be that younger mothers have a lower proportion of adequate prenatal care, and there was a significant association of adequate prenatal care with maternal age.43
There are several possible mechanisms that might explain the association between higher levels of Cd and increased risk of PLBW. Cd accumulates in human placenta,44 and infant birth weight can be impaired by the indirect toxic effects of Cd on the placenta or direct effects of Cd on the fetus.14 Other possible mechanisms of Cd impairing fetal growth may include downregulating the expression and activity of placental 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2) gene,45 interfering with the IGF axis39 and the epigenetic machinery, such as DNA methylation.46, 47
Our study has several strengths. The nested case–control design provided the opportunity to include all the PLBW infants in the study. Interviews conducted with all participants allowed us to adjust for other potential risk factors for PLBW, such as maternal body mass index, household income and passive smoking during pregnancy. Smoking has been recognized as a risk factor for LBW,48 and one of the main sources of Cd exposure in the general population.5 However, smoking was not included in our final adjusted logistic model, because only one mother in our study population reported smoking during pregnancy.
The present study has some limitations. First, maternal urinary samples in our study were only collected at a single time point, which may not accurately reflect Cd exposure in the whole pregnancy. However, previous studies have reported that there is no significant changes in urinary Cd concentrations before pregnancy, during gestation and after birth.49 Urinary Cd concentrations were also considered to be a well-recognized biomarker of chronic Cd exposure.2
CONCLUSIONS
In conclusion, our nested case–control study found that there is a positive association between higher levels of maternal urinary Cd concentrations and an increased risk of PLBW in Chinese pregnant women. These findings suggest that prenatal Cd exposure may be an important risk factor in the etiology of PLBW. Future research is needed to identify the sources of Cd exposure among pregnant women, and design appropriate strategies to reduce Cd exposure in pregnant women.
References
Menai M, Heude B, Slama R, Forhan A, Sahuquillo J, Charles MA et al. Association between maternal blood cadmium during pregnancy and birth weight and the risk of fetal growth restriction: the EDEN mother-child cohort study. Reprod Toxicol 2012; 34: 622–627.
Jarup L, Akesson A . Current status of cadmium as an environmental health problem. Toxicol Appl Pharm 2009; 238: 201–208.
Suwazono Y, Sand S, Vahter M, Filipsson AF, Skerfving S, Lidfeldt J et al. Benchmark dose for cadmium-induced renal effects in humans. Environ Health Perspect 2006; 114: 1072–1076.
Peters JL, Perlstein TS, Perry MJ, McNeely E, Weuve J . Cadmium exposure in association with history of stroke and heart failure. Environ Res 2010; 110: 199–206.
Satarug S, Moore MR . Adverse health effects of chronic exposure to low-level cadmium in foodstuffs and cigarette smoke. Environ Health Perspect 2004; 112: 1099–1103.
Adams SV, Passarelli MN, Newcomb PA . Cadmium exposure and cancer mortality in the Third National Health and Nutrition Examination Survey cohort. Occup Environ Med 2012; 69: 153–156.
Korpela H, Loueniva R, Yrjanheikki E, Kauppila A . Lead and cadmium concentrations in maternal and umbilical cord blood, amniotic fluid, placenta, and amniotic membranes. Am J Obstet Gynecol 1986; 155: 1086–1089.
Osman K, Akesson A, Berglund M, Bremme K, Schutz A, Ask K et al. Toxic and essential elements in placentas of Swedish women. Clin Biochem 2000; 33: 131–138.
Christensen MM, Keith I, Rhodes PR, Graziano FM, Madsen PO, Bruskewitz RC et al. A guinea pig model for study of bladder mast cell function: histamine release and smooth muscle contraction. J Urol 1990; 144: 1293–1300.
Sorell TL, Graziano JH . Effect of oral cadmium exposure during pregnancy on maternal and fetal zinc metabolism in the rat. Toxicol Appl Pharmacol 1990; 102: 537–545.
Nagymajtenyi L, Schulz H, Desi I . Behavioural and functional neurotoxicological changes caused by cadmium in a three-generational study in rats. Hum Exp Toxicol 1997; 16: 691–699.
Shen HM, Dong SY, Ong CN . Critical role of calcium overloading in cadmium-induced apoptosis in mouse thymocytes. Toxicol Appl Pharm 2001; 171: 12–19.
Nishijo M, Nakagawa H, Honda R, Tanebe K, Saito S, Teranishi H et al. Effects of maternal exposure to cadmium on pregnancy outcome and breast milk. Occup Environ Med 2002; 59: 394–396.
Salpietro CD, Gangemi S, Minciuollo PL, Briuglia S, Merlino MV, Stelitano A et al. Cadmium concentration in maternal and cord blood and infant birth weight: a study on healthy non-smoking women. J Perinat Med 2002; 30: 395–399.
Kippler M, Tofail F, Gardner R, Rahman A, Hamadani JD, Bottai M et al. Maternal cadmium exposure during pregnancy and size at birth: a prospective cohort study. Environ Health Perspect 2012; 120: 284–289.
Sun H, Chen W, Wang D, Jin Y, Chen X, Xu Y . The effects of prenatal exposure to low-level cadmium, lead and selenium on birth outcomes. Chemosphere 2014; 108: 33–39.
Odland JO, Nieboer E, Romanova N, Thomassen Y, Lund E . Blood lead and cadmium and birth weight among sub-arctic and arctic populations of Norway and Russia. Acta Obstet Gyn Scan 1999; 78: 852–860.
Nishijo M, Tawara K, Honda R, Nakagawa H, Tanebe K, Saito S . Relationship between newborn size and mother’s blood cadmium levels, Toyama, Japan. Arch Environ Health 2004; 59: 22–25.
Zhang YL, Zhao YC, Wang JX, Zhu HD, Liu QF, Fan YG et al. Effect of environmental exposure to cadmium on pregnancy outcome and fetal growth: A study on healthy pregnant women in China. J Environ Sci Heal A 2004; 39: 2507–2515.
Lin CM, Doyle P, Wang D, Hwang YH, Chen PC . Does prenatal cadmium exposure affect fetal and child growth? Occup Environ Med 2011; 68: 641–646.
Jin TY, Wu XW, Tang YQ, Nordberg M, Bernard A, Ye TT et al. Environmental epidemiological study and estimation of benchmark dose for renal dysfunction in a cadmium-polluted area in China. Biometals 2004; 17: 525–530.
Yu H, Wang J, Fang W, Yuan J, Yang Z . Cadmium accumulation in different rice cultivars and screening for pollution-safe cultivars of rice. Sci Total Environ 2006; 370: 302–309.
Du Y, Hu XF, Wu XH, Shu Y, Jiang Y, Yan XJ . Affects of mining activities on Cd pollution to the paddy soils and rice grain in Hunan province, Central South China. Environ Monit Assess 2013; 185: 9843–9856.
Xia W, Du X, Zhang B, Li Y, Bassig BA, Zhou A et al. A case-control study of prenatal thallium exposure and low birth weight in China. Environ Health Perspect 2015; 124: 164–169.
Janevic T, Petrovic O, Bjelic I, Kubera A . Risk factors for childhood malnutrition in Roma settlements in Serbia. BMC Public Health 2010; 10: 509.
Williams CE, Davenport ES, Sterne JA, Sivapathasundaram V, Fearne JM, Curtis MA . Mechanisms of risk in preterm low-birthweight infants. Periodontol 2000 2000; 23: 142–150.
Offenbacher S, Lieff S, Boggess KA, Murtha AP, Madianos PN, Champagne CM et al. Maternal periodontitis and prematurity. Part I: Obstetric outcome of prematurity and growth restriction. Ann Periodontol 2001; 6: 164–174.
Gunier RB, Horn-Ross PL, Canchola AJ, Duffy CN, Reynolds P, Hertz A et al. Determinants and within-person variability of urinary cadmium concentrations among women in northern California. Environ Health Perspect 2013; 121: 643–649.
Castano A, Sanchez-Rodriguez JE, Canas A, Esteban M, Navarro C, Rodriguez-Garcia AC et al. Mercury, lead and cadmium levels in the urine of 170 Spanish adults: a pilot human biomonitoring study. Int J Hyg Environ Health 2012; 215: 191–195.
Becker K, Schulz C, Kaus S, Seiwert M, Seifert B . German Environmental Survey 1998 (GerES III): environmental pollutants in the urine of the German population. Int J Hyg Environ Health 2003; 206: 15–24.
Hinwood AL, Callan AC, Ramalingam M, Boyce M, Heyworth J, McCafferty P et al. Cadmium, lead and mercury exposure in non smoking pregnant women. Environ Res 2013; 126: 118–124.
Shirai S, Suzuki Y, Yoshinaga J, Mizumoto Y . Maternal exposure to low-level heavy metals during pregnancy and birth size. J Environ Sci Health A Tox Hazard Subst Environ Eng 2010; 45: 1468–1474.
Zhang X, Zhong T, Liu L, Ouyang X . Impact of soil heavy metal pollution on food safety in China. PloS One 2015; 10: e0135182.
Johnston JE, Valentiner E, Maxson P, Miranda ML, Fry RC . Maternal cadmium levels during pregnancy associated with lower birth weight in infants in a North Carolina cohort. PloS One 2014; 9: e109661.
Johnson MD, Kenney N, Stoica A, Hilakivi-Clarke L, Singh B, Chepko G et al. Cadmium mimics the in vivo effects of estrogen in the uterus and mammary gland. Nat Med 2003; 9: 1081–1084.
Henson MC, Chedrese PJ . Endocrine disruption by cadmium, a common environmental toxicant with paradoxical effects on reproduction. Exp Biol Med 2004; 229: 383–392.
Orikasa C, Kondo Y, Hayashi S, McEwen BS, Sakuma Y . Sexually dimorphic expression of estrogen receptor beta in the anteroventral periventricular nucleus of the rat preoptic area: implication in luteinizing hormone surge. Proc Natl Acad Sci USA 2002; 99: 3306–3311.
Davis LK, Pierce AL, Hiramatsu N, Sullivan CV, Hirano T, Grau EG . Gender-specific expression of multiple estrogen receptors, growth hormone receptors, insulin-like growth factors and vitellogenins, and effects of 17 beta-estradiol in the male tilapia (Oreochromis mossambicus). Gen Comp Endocrinol 2008; 156: 544–551.
Turgut S, Kaptanoglu B, Turgut G, Emmungil G, Genc O . Effects of cadmium and zinc on plasma levels of growth hormone, insulin-like growth factor I, and insulin-like growth factor-binding protein 3. Biol Trace Elem Res 2005; 108: 197–204.
Murphy VE, Smith R, Giles WB, Clifton VL . Endocrine regulation of human fetal growth: the role of the mother, placenta, and fetus. Endocr Rev 2006; 27: 141–169.
Vatten LJ, Nilsen ST, Odegard RA, Romundstad PR, Austgulen R . Insulin-like growth factor I and leptin in umbilical cord plasma and infant birth size at term. Pediatrics 2002; 109: 1131–1135.
Geary MP, Pringle PJ, Rodeck CH, Kingdom JC, Hindmarsh PC . Sexual dimorphism in the growth hormone and insulin-like growth factor axis at birth. J Clin Endocrinol Metab 2003; 88: 3708–3714.
Vieira CL, Coeli CM, Pinheiro RS, Brandao ER, Camargo KR, Jr., Aguiar FP . Modifying effect of prenatal care on the association between young maternal age and adverse birth outcomes. J Pediatr Adolesc Gynecol 2012; 25: 185–189.
Iyengar GV, Rapp A . Human placenta as a “dual” biomarker for monitoring fetal and maternal environment with special reference to potentially toxic trace elements. Part 3: toxic trace elements in placenta and placenta as a biomarker for these elements. Sci Total Environ 2001; 280: 221–238.
McTernan CL, Draper N, Nicholson H, Chalder SM, Driver P, Hewison M et al. Reduced placental 11 beta-hydroxysteroid dehydrogenase type 2 mRNA levels in human pregnancies complicated by intrauterine growth restriction: an analysis of possible mechanisms. J Clin Endocr Metab 2001; 86: 4979–4983.
Doi T, Puri P, McCann A, Bannigan J, Thompson J . Epigenetic effect of cadmium on global de novo DNA hypomethylation in the cadmium-induced ventral body wall defect (VBWD) in the chick model. Toxicol Sci 2011; 120: 475–480.
Smith ZD, Chan MM, Mikkelsen TS, Gu HC, Gnirke A, Regev A et al. A unique regulatory phase of DNA methylation in the early mammalian embryo. Nature 2012; 484: 339–U74.
Ko TJ, Tsai LY, Chu LC, Yeh SJ, Leung C, Chen CY et al. Parental smoking during pregnancy and its association with low birth weight, small for gestational age, and preterm birth offspring: a birth cohort study. Pediatr Neonatol 2014; 55: 20–27.
Hernandez M, Schuhmacher M, Fernandez JD, Domingo JL, Llobet JM . Urinary cadmium levels during pregnancy and postpartum. A longitudinal study. Biol Trace Elem Res 1996; 53: 205–212.
Acknowledgements
This work was supported by the National Basic Research Program of China (973 Program) (2012CB722401), the National Natural Science Foundation of China (21437002, 81030051, 81372959, 81402649) and the R&D Special Fund for Public Welfare Industry (Environment) (201309048). Also, this work was partly supported by Fogarty training grants D43TW 008323 and D43TW 007864-01 from the US National Institutes of Health.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Exposure Science and Environmental Epidemiology website
Supplementary information
Rights and permissions
About this article
Cite this article
Huang, K., Li, H., Zhang, B. et al. Prenatal cadmium exposure and preterm low birth weight in China. J Expo Sci Environ Epidemiol 27, 491–496 (2017). https://doi.org/10.1038/jes.2016.41
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2016.41
- Springer Nature America, Inc.
Keywords
This article is cited by
-
Effects of heavy metal exposure during pregnancy on birth outcomes
Scientific Reports (2023)
-
Cadmium exposure and risk of adverse pregnancy and birth outcomes: a systematic review and dose–response meta-analysis of cohort and cohort-based case–control studies
Journal of Exposure Science & Environmental Epidemiology (2021)
-
Evidence of selected nephrotoxic elements in Sri Lankan human autopsy bone samples of patients with CKDu and controls
BMC Nephrology (2020)
-
Maternal Exposure to Cadmium and Fetal Growth: a Systematic Review and Meta-Analysis
Biological Trace Element Research (2020)
-
A quantitative analysis of chronic exposure of selected heavy metals in a model diet in a CKD hotspot in Sri Lanka
BMC Nephrology (2019)