Abstract
Background/Objective:
Differences in subcutaneous abdominal adipose tissue (SAT) fat cell size and number (cellularity) are linked to insulin resistance. Men are generally more insulin resistant than women but it is unknown whether there is a gender dimorphism in SAT cellularity. The objective was to determine SAT cellularity and its relationship to insulin sensitivity in men and women.
Methods:
In a cohort study performed at an outpatient academic clinic in Sweden, 798 women and 306 men were included. Estimated SAT mass (ESAT) was derived from measures of dual-energy X-ray absorptiometry and a formula. SAT biopsies were obtained to measure mean fat cell size; SAT adipocyte number was obtained by dividing ESAT with mean fat cell weight. Fat cell size was also compared with level of insulin sensitivity in vivo.
Results:
Over the entire range of body mass index (BMI) both fat cell size and number correlated positively with ESAT in either sex. On average, fat cell size was larger in men than in women, which was driven by significantly larger fat cells in non-obese men compared with non-obese women; no gender effect on fat cell size was seen in obese subjects. For all subjects fat cell number was larger in women than men, which was driven by a gender effect among non-obese individuals (P<0.0001). The relationship between fat cell size and insulin resistance was significant in both genders (P<0.0001) but steeper in men than in women (F=19, P<0.0001).
Conclusions:
Although both fat cell size and number determine SAT mass, adipocyte number contributes more and size less in women than in men and this is most evident in non-obese subjects. Over the entire BMI range, fat cell size contributes stronger to insulin resistance in men.
Similar content being viewed by others
Introduction
White adipose tissue (WAT) mass can expand by increasing the size (hypertrophy) and/or number (hyperplasia) of fat cells. Based on studies performed in the 1970s it was for long thought that hypertrophy is the predominant factor behind WAT expansion in adults except in juvenile or excessive forms of obesity.1, 2, 3 Inter-individual differences in the degree of WAT hyperplasia/hypertrophy has strong clinical implications. Hypertrophic abdominal subcutaneous adipose tissue (SAT) is independently of body mass index (BMI) associated with insulin resistance4, 5, 6, 7 and increased risk of future development of type 2 diabetes.8, 9 It is unknown whether the relationship between fat cell size and insulin sensitivity is influenced by gender.
Determination of fat cell number in earlier studies has been based on analyses of total body fat instead of the mass of the adipose region where fat cell size was measured.1, 2, 3 This may cause erroneous estimates of hyperplasia/hypertrophy (herein defined as adipose cellularity). We recently assessed fat cell size and number in the major omentum, which was removed in connection with bariatric surgery.10 Quite surprisingly, fat cell number explained 2/3 of the variation in tissue mass compared with 1/3 for fat cell size. A previous study implicated that a moderate expansion of SAT may also increase fat cell number in women.11 These data suggest that fat cell number, in addition to its established importance in WAT expansion during infancy and adolescence,12 is also a significant determinant of WAT mass in adults. The role of gender for adipose cellularity may be relevant for type 2 diabetes as men are more insulin resistant and have a higher risk of developing type 2 diabetes than women as reviewed.13, 14 However, it is not known whether hyperplastic versus hypertrophic WAT expansion differs between men and women as this issue has only been investigated in a small groups (n=23–73) of subjects.15, 16, 17
Thanks to recent developments in dual-energy X-ray absorptiometry (DEXA), it is now possible to measure the mass of a defined (android) segment of abdominal SAT and thereby calculate the number of fat cells in this specific region.18, 19, 20 Herein, we used this method to develop a formula based on common clinical variables that allowed us to estimate SAT mass (herein termed ESAT) with very high accuracy. This formula enabled us to compare the relationship between fat mass and adipocyte size or number in the same adipose depot. The examinations were conducted in a large number of men and women displaying a wide BMI range and allowed us to determine whether gender has any impact on the relationship between abdominal subcutaneous cellularity and fat mass as well as insulin sensitivity.
Materials and methods
Subjects
The subjects were continuously included since 1986 in studies aiming to determine the genetic influence on human subcutaneous fat cell function.21 They were recruited by local advertisement in the area of Stockholm, Sweden. Exclusion criteria were severe chronic disease and diabetes treated with insulin, glitazones or glucagon like peptides. The cohort consists of 306 men and 798 women. Clinical characteristics are given in Table 1. A few subjects had type 2 diabetes, hypertension and/or dyslipidemia. The study was explained in detail to each person and informed consent was obtained. Two were<18 years of age (that is, 16 years old) and consent from the parents was also obtained for these individuals. The study was approved by the local ethical committee.
Examinations
The subjects came to the laboratory in the morning after an overnight fast. The same three research nurses performed all clinical examinations throughout the study. Height, body weight and circumferences of waist and hip were determined. Total body fat mass was directly measured by bio-impedance (Body Stat, Quadscan 4000, Isle of Man, British Isles) and also indirectly using a formula based on age, sex and BMI.22 Thereafter a venous blood sample was obtained for measurements of plasma glucose and serum insulin, which were used to calculate HOMA-IR23 for quantification of insulin sensitivity. In 160 women and 46 men, insulin sensitivity was directly determined by the short intravenous insulin tolerance test exactly as described.24 A subset of the cohort underwent DEXA measures to determine SAT mass, exactly as described.20, 25 In brief, a GE lunar DEXA with the software enCORE18 was used (GE Healthcare, Madison, WI, USA) to EVAT (estimated visceral fat) in the android region from the formula: total android fat=EVAT+ESAT.18 The DEXA-derived EVAT measure shows an almost one-to-one relationship (r2⩾0.95) with measures obtained by computed tomography19 and has recently been approved by the US Food and Drug Administration as a valid measure of VAT. As measures of total android fat and EVAT by DEXA are valid it follows that calculation of ESAT is also valid. A SAT biopsy was obtained from the periumbilical area. Fat cell weight and volume were determined exactly as described.26 In brief, isolated fat cells were prepared and the diameters of 100 cells were measured in light microscopy. The same three technicians performed the diameter measures throughout the study, using the same microscope. These diameters were used to calculate mean fat cell weight and volume according to well-established formulas.27 It has previously been demonstrated that using >100 diameter measures does not improve the calculations.28 It has also been shown that fat cell size measures give similar results using isolated fat cells or pieces of intact adipose tissue.29 It is standard procedure to use mean diameter to determine fat cell size and number since the methods were introduced ~60 years ago, as discussed.2, 3 However, one laboratory has demonstrated that subcutaneous fat cell diameters may have a bimodal distribution.30 As far as we know there has been no independent confirmation of this bimodality in human adipose tissue. Furthermore, we recently measured 7900 fat cell diameters in 177 biopsies from the SAT region of obese, post obese and never obese subjects,25 and found a clear unimodal distribution of the diameters in this large sample. We therefore believe that the use of mean diameter is valid. Fat cell number in SAT was obtained by dividing ESAT weight with the mean fat cell weight. The relationship between fat mass and fat cell volume was determined as described in detail previously.4, 31 In brief, a curve is fit to the formula V=(a × m)/(1+b × m), where V is mean fat cell volume, m is the amount (weight) of adipose tissue, and a and b are variables that are obtained by fitting the formula to subject data using the least squares method. Separate curve fits were calculated for men and women respectively. Clinical characteristics with expected gender differences are shown in Table 1.
Statistics
Values are mean±s.d. or range in text and tables and mean±s.e. in figures. They were compared using unpaired t-test, χ2, single or multiple linear regression, analysis of variance and analysis of covariance. We prefer using linear multiple regression instead of logistic regression as it allows a better biological interpretation of results as discussed in detail.32 Coefficient of variance was determined as measure one minus measure two divided by mean of the two measures. Differences between parameter estimates for men and women in the curve fitting of fat cell volume versus ESAT mass were assessed for statistical significance using t-test.
Results
Because DEXA-based measures of SAT were only available in a subset of the cohort we developed a formula for ESAT based on clinical measures that could be used in the whole study population. DEXA was performed in 368 subjects out of which 147 were examined twice, 14 three times and 1 subject four times (before and after weight loss and subsequent weight regain). This provided a total of 546 DEXA-based ESAT measures. We constructed a multiple regression model based on waist circumference, waist-to-hip ratio, age, total body fat mass and sex to estimate SAT (Supplementary Table 1). All regressors contributed significantly to the variation in DEXA measured ESAT and together explained 85% of the variance in this measure (adjusted r2). The regression model was used to make an algorithm for abdominal subcutaneous fat mass. The equation is: ESAT (kg)=−3.317 waist-to-hip ratio × 0.889+gender (one for men and two for women) × 0.394–age (years) × 0.012+total body fat mass(kg) × 0.015+waist circumference (cm) × 0.051. It should be noted that ESAT is not the total amount of central subcutaneous WAT, just the region corresponding to that where the fat biopsy was taken. The linear relationship between algorithm- and DEXA-based measures of ESAT is demonstrated in Figure 1a. There was no gender effect. For the common regression line the slope was 1.02 and the intercept 0.01. Coefficient of variance between DEXA-determined ESAT and calculated ESAT measures from the new formula was as low as 1.1%. Similar results were obtained if only data from the first DEXA measurement were used (graph not shown). Assessments of total body fat used in the model were based on bio-impedance (n=519) or an established formula (n=27). Bio-impedance measures gave essentially the same results as when the 27 formula measures were excluded.
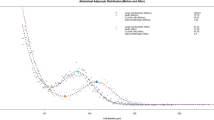
Findings with abdominal subcutaneous adipose tissue mass. (a) Comparison with determination by dual X-ray absorptiometry (DEXA) or algorithm. (b) Curve–linear relationship with fat cell volume. (c) Linearization of relationship with fat cell volume. (d) Relationship with fat cell number. Linear regression and analysis of covariance were used as statistical tests.
We next compared the curve–linear relationship between ESAT and fat cell volume to get a measure of SAT cellularity in men and women (Figure 1b). There was a significant difference between the curve for men and women (P<0.05, t-test), and men had much larger fat cells than women in the lower ESAT range. The variables a and b in the formula for subcutaneous cellularity V=(a × m)/(1+b × m) differed between men (a=1436.254 pl kg−1 and b=1.369924 per kg) and women (a=639.3137 pl kg−1 and b =0.433493 per kg). Similar results were obtained if the relationship between ESAT and fat cell volume data was linearized by plotting (10)log ESAT mass versus fat cell volume (Figure 1c) This demonstrated that although there was a strong positive correlation between ESAT and fat cell volume in either sex, the position of the lines differed markedly (P<0.0001). Visually the gender effect was most marked in the lower range of ESAT mass. We also investigated the relationship between fat cell number and (10) log ESAT mass (Figure 1d). Here a different type of gender effect was observed. Although fat cell number was positively related to increasing ESAT in either sex, the line for women was slightly but significantly above that of men (P<0.0001).
To get more insight into gender variations in adipose cellularity, multiple regression was used. In Table 2 fat cell volume was investigated. In all subjects put together gender significantly influenced the relationship between ESAT and fat cell volume. When performing a sub-analysis in non-obese (BMI<30 kg m−2) and obese, gender had an influence in non-obese but not in obese. In Table 3 fat cell number was investigated. Gender significantly influenced the relationship between ESAT and cell number in all subjects and non-obese but not in obese. These results concur with the results in Figures 1c and d. Age was included in the regression model and was a significant cofactor for the relationship between ESAT and fat cell volume or number. We also used logistic regression and the results were the same as for multiple linear regression.
Finally, the gender effect on the relationship between fat cell volume and insulin sensitivity (HOMA-IR) was compared. In both men and women there was a positive correlation between the two measures (Figure 2a). However, the association was strongly influenced by gender as men had a significantly steeper relationship than women (F=19; P<0.0001). Similar results were obtained in a subset of subjects where insulin sensitivity was determined directly by intravenous insulin tolerance (F=15; P=0.0002) (Figure 2b). We further investigated the relationship between HOMA-IR and gender by multiple regression analysis (Table 4). Independent of ESAT and age, gender had a significant influence on the relationship between fat cell volume and HOMA-IR in all subjects put together as well as in non-obese or obese investigated separately. Thus, at any given subcutaneous abdominal fat cell volume, men are more insulin-resistant than women.
Relationship between fat cell size in abdominal subcutaneous adipose tissue and insulin sensitivity measured by. (a) HOMA-IR. (b) intravenous insulin tolerance. Statistical analyses are as described in legend to Figure 1.
A few subjects were treated for type 2 diabetes, hypertension and/or dyslipidemia. However, the results were not influenced in any important way if they were excluded from the analysis.
Discussion
This study sheds new light on the influence of gender on abdominal SAT cellularity and its relationship with insulin sensitivity. It is well-established that adipose hypertrophy in this region has a strong influence on type 2 diabetes and insulin resistance. Thanks to our development of a novel formula we could accurately determine fat cell number in a defined segment of abdominal SAT in a very large cohort of men and women with marked inter-individual variations in BMI. This contrasts with prior studies in small groups of subjects where fat cell number was determined by less-accurate methods using total body fat as numerator.
We confirm the important contribution of fat cell hypertrophy for increasing fat mass.1, 2, 3 The only exception was that, in men with severe obesity, increases in fat cell size seemed to be of less importance in explaining ESAT expansion. Concerning our findings on fat cell number the results contrast with reports from the 1970s.1, 2, 3 Thus, fat cell number increased proportionally with increasing ESAT over the entire BMI range. This was true for either sex and suggests a major role for hyperplasia in explaining increases in abdominal subcutaneous fat mass. The results are supported by previous results in women but not in men.33 Thus, Tchoukalova et al.33 found that fat cell number is positively related to BMI in abdominal subcutaneous and leg adipose tissue only in women. The reason for this discrepancy is unclear but could at least in part be due to different methods used to determine regional fat mass. Furthermore, the former study did not use regression analysis of the whole study group, instead the investigators divided the sample into three BMI groups. Finally, the cohort was much smaller than the present one.
A possible explanation for SAT hyperplasia is an increase in the generation of fat cells in response to body weight gain. Previous findings support the theory. Adult human fat cells are in a highly dynamic state.31 About 10% of the total cell population is renewed each year and the rate of generation of new fat cells on the whole body level is doubled in obesity.31 Long-term weight regain after bariatric surgery is accompanied by a significant increase in SAT fat cell number.25 Also short-term weight gain increases fat cell number, at least in the lower body fat regions.11 In other words, generation of more fat cells is probably a driving force behind moderate as well as excessive expansion of fat mass in several subcutaneous and visceral adipose regions as evidenced from present and previous studies discussed above.
Why do our and previous33 results on SAT hyperplastic expansion differ from pioneer studies in the 1970s?1, 2, 3 The most likely explanation is the use of different methods to determine cellularity. In the 1970s it was not possible to measure the size of individual adipose regions in vivo.1, 2, 3 The earlier methods used mean fat cell weight from several subcutaneous regions and total fat mass estimates to calculate fat cell number.
The major objective of our study was to determine the influence of gender on SAT cellularity. As mentioned earlier previous studies on small SAT from small study groups reported similar cellularity between men and women.15, 16, 17 The results of our large study deviate from previous findings. In non-obese subjects, ESAT was found to be more hypertrophic and less hyperplastic in non-obese men than in women. On the other hand, obese subjects of either sex displayed a similar relationship between fat cell size or number and ESAT. This suggests that SAT expansion at non-obese BMI levels is driven to a relatively higher degree by hypertrophy in men and that hyperplasia is slightly more important in women. The mechanism behind these gender differences is unknown but could be linked to a greater differentiation capacity of subcutaneous adipocyte precursor cell in women.33
Our results also demonstrate a hitherto unknown impact of gender on the correlation between fat cell size and insulin sensitivity. The relationship between insulin resistance and SAT fat cell volume was much steeper in men than in women. This in combination with more pronounced SAT hypertrophy in men may underlie the well-established gender differences in insulin resistance, at least among non-obese individuals. Nevertheless, other gender differences in the metabolic and endocrine function of fat cells beyond cellularity and non-adipose factors may also be important as discussed.34, 35 Furthermore, we used an indirect (although common) measure of insulin sensitivity (HOMA-IR). It is possible that results would be different using other types of insulin sensitivity measures. However, we find this less likely, as we found similar gender differences in the relationship between fat cell size and insulin sensitivity in a subset of individuals where we had performed insulin tolerance tests. This direct measure of insulin sensitivity correlates strongly with the 'gold standard' hyperinsulinemic euglycemic clamp method.36
In summary, this study provides novel information on the impact of gender on SAT cellularity. Contrary to earlier finding, fat cell number contributes to variations in SAT mass over all BMI classes in both genders although significantly more in non-obese women. This suggests that hyperplastic expansion may be more important in women than in men. However, in the non-obese state hypertrophy is probably a stronger driving force for SAT expansion in men. Furthermore, men display a steeper relationship between abdominal subcutaneous fat cell size and insulin resistance than women. Differences in SAT cellularity may therefore at least in part explain why men are more insulin resistant than women.
References
Salans LB, Cushman SW, Weismann RE . Studies of human adipose tissue. Adipose cell size and number in nonobese and obese patients. J Clin Invest 1973; 52: 929–941.
Bjorntorp P . Sjostrom L,+SJOSTROM L: Number and size of adipose tissue fat cells in relation to metabolism in human obesity. Metabolism 1971; 20: 703–713.
Hirsch J, Batchelor B . Adipose tissue cellularity in human obesity. Clin Endocrinol Metab 1976; 5: 299–311.
Arner E, Westermark PO, Spalding KL, Britton T, Ryden M, Frisen J et al. Adipocyte turnover: relevance to human adipose tissue morphology. Diabetes 2010; 59: 105–109.
Ktotkiewski M, Sjostrom L, Bjorntorp P, Smith U . Regional adipose tissue cellularity in relation to metabolism in young and middle-aged women. Metabolism 1975; 24: 703–710.
Stern JS, Batchelor BR, Hollander N, Cohn CK, Hirsch J . Adipose-cell size and immunoreactive insulin levels in obese and normal-weight adults. Lancet 1972; 2: 948–951.
Salans LB, Knittle JL, Hirsch J . The role of adipose cell size and adipose tissue insulin sensitivity in the carbohydrate intolerance of human obesity. J Clin Invest 1968; 47: 153–165.
Weyer C, Foley JE, Bogardus C, Tataranni PA, Pratley RE . Enlarged subcutaneous abdominal adipocyte size, but not obesity itself, predicts type II diabetes independent of insulin resistance. Diabetologia 2000; 43: 1498–1506.
Lonn M, Mehlig K, Bengtsson C, Lissner L . Adipocyte size predicts incidence of type 2 diabetes in women. FASEB J 2010; 24: 326–331.
Arner P, Andersson DP, Thorne A, Wiren M, Hoffstedt J, Naslund E et al. Variations in the size of the major omentum are primarily determined by fat cell number. J Clin Endocrinol Metab 2013; 98: E897–E901.
Tchoukalova YD, Votruba SB, Tchkonia T, Giorgadze N, Kirkland JL, Jensen MD . Regional differences in cellular mechanisms of adipose tissue gain with overfeeding. Proc Natl Acad Sci USA 2010; 107: 18226–18231.
Knittle JL, Timmers K, Ginsberg-Fellner F, Brown RE, Katz DP . The growth of adipose tissue in children and adolescents. Cross-sectional and longitudinal studies of adipose cell number and size. J Clin Invest 1979; 63: 239–246.
Geer EB, Shen W . Gender differences in insulin resistance, body composition, and energy balance. Gender Med 2009; 6: 60–75.
Sattar N . Gender aspects in type 2 diabetes mellitus and cardiometabolic risk. Best Pract Res Clin Endocrinol Metab 2013; 27: 501–507.
Bjorntorp P, Bengtsson C, Blohme G, Jonsson A, Sjostrom L, Tibblin E et al. Adipose tissue fat cell size and number in relation to metabolism in randomly selected middle-aged men and women. Metabolism 1971; 20: 927–935.
Sjostrom L, Smith U, Krotkiewski M, Bjorntorp P . Cellularity in different regions of adipose tissue in young men and women. Metabolism 1972; 21: 1143–1153.
Tchoukalova YD, Koutsari C, Votruba SB, Tchkonia T, Giorgadze N, Thomou T et al. Sex- and depot-dependent differences in adipogenesis in normal-weight humans. Obesity (Silver Spring) 2010; 18: 1875–1880.
Lee K, Lee S, Kim YJ . Waist circumference, dual-energy X-ray absortiometrically measured abdominal adiposity, and computed tomographically derived intra-abdominal fat area on detecting metabolic risk factors in obese women. Nutrition 2008; 24: 625–631.
Kaul S, Rothney MP, Peters DM, Wacker WK, Davis CE, Shapiro MD et al. Dual-energy X-ray absorptiometry for quantification of visceral fat. Obesity (Silver Spring) 2012; 20: 1313–1318.
Andersson DP, Eriksson Hogling D, Thorell A, Toft E, Qvisth V, Naslund E et al. Changes in subcutaneous fat cell volume and insulin sensitivity after weight loss. Diabetes Care 2014; 37: 1831–1836.
Strawbridge RJ, Laumen H, Hamsten A, Breier M, Grallert H, Hauner H et al. Effects of genetic loci associated with central obesity on adipocyte lipolysis. PLoS One 2016; 11: e0153990.
Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB . How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 1996; 143: 228–239.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Bolinder J, Ostman J, Arner P . Postreceptor defects causing insulin resistance in normoinsulinemic non-insulin-dependent diabetes mellitus. Diabetes 1982; 31: 911–916.
Hoffstedt J, Andersson DP, Eriksson Hogling D, Theorell J, Naslund E, Thorell A et al. Long-term protective changes in adipose tissue after gastric bypass. Diabetes Care 2017; 40: 77–84.
Ryden M, Andersson DP, Bergstrom IB, Arner P . Adipose tissue and metabolic alterations: regional differences in fat cell size and number matter, but differently: a cross-sectional study. J Clin Endocrinol Metab 2014; 99: E1870–E1876.
Goldrick RB, McLoughlin GM . Lipolysis and lipogenesis from glucose in human fat cells of different sizes. Effects of insulin, epinephrine, and theophylline. J Clin Invest 1970; 49: 1213–1223.
Tchoukalova YD, Harteneck DA, Karwoski RA, Tarara J, Jensen MD . A quick, reliable, and automated method for fat cell sizing. J Lipid Res 2003; 44: 1795–1801.
Cushman SW, Salans LB . Determinations of adipose cell size and number in suspensions of isolated rat and human adipose cells. J Lipid Res 1978; 19: 269–273.
McLaughlin T, Sherman A, Tsao P, Gonzalez O, Yee G, Lamendola C et al. Enhanced proportion of small adipose cells in insulin-resistant vs insulin-sensitive obese individuals implicates impaired adipogenesis. Diabetologia 2007; 50: 1707–1715.
Spalding KL, Arner E, Westermark PO, Bernard S, Buchholz BA, Bergmann O et al. Dynamics of fat cell turnover in humans. Nature 2008; 453: 783–787.
Hellevik O . Linear versus logistic regression when the dependent variable is a dichotomy. Qual Quant 2009; 43: 59–74.
Tchoukalova YD, Koutsari C, Karpyak MV, Votruba SB, Wendland E, Jensen MD . Subcutaneous adipocyte size and body fat distribution. Am J Clin Nutr 2008; 87: 56–63.
Karastergiou K, Smith SR, Greenberg AS, Fried SK . Sex differences in human adipose tissues - the biology of pear shape. Biol Sex Differ 2012; 3: 13.
White UA, Tchoukalova YD . Sex dimorphism and depot differences in adipose tissue function. Biochim Biophys Acta 2014; 1842: 377–392.
Bonora E, Moghetti P, Zancanaro C, Cigolini M, Querena M, Cacciatori V et al. Estimates of in vivo insulin action in man: comparison of insulin tolerance tests with euglycemic and hyperglycemic glucose clamp studies. J Clin Endocrinol Metab 1989; 68: 374–378.
Acknowledgements
We thank Katarina Hertel, Britt-Marie Leijonhufvud and Yvonne Widlund for performing clinical examinations and technicians Elisabeth Dungner, Eva Sjölin and Kerstin Wåhlen for their measures of fat cell diameter throughout the study. This work was supported by grants from the Swedish Research Council, The Swedish Diabetes Foundation, Center for Innovative Medicine, the Diabetes Theme Center at Karolinska Institutet, the Tore Nilsson Foundation, the Stockholm County Council and the Novo Nordisk Foundation including the Tripartite Immuno-metabolism Consortium (TrIC) Grant Number NNF15CC0018486 and the MSAM consortium NNF15SA0018346.
Author contributions
PA conceived the study, collected all the data, wrote the first version of the manuscript and is the guarantor of the data. EA, MR, DEH and DPA generated data and prepared figures/tables. EA; MR, DPA and PA, analyzed data. All authors read and contributed to the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Andersson, D., Arner, E., Hogling, D. et al. Abdominal subcutaneous adipose tissue cellularity in men and women. Int J Obes 41, 1564–1569 (2017). https://doi.org/10.1038/ijo.2017.148
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.148
- Springer Nature Limited
This article is cited by
-
Adipokine secretion and lipolysis following gender-affirming treatment in transgender individuals
Journal of Endocrinological Investigation (2024)
-
Impact of blood perilipin A levels on obesity and metabolic health
BMC Research Notes (2022)
-
Subcutaneous adipose tissue expansion mechanisms are similar in early and late onset overweight/obesity
International Journal of Obesity (2022)
-
The long noncoding RNA ADIPINT regulates human adipocyte metabolism via pyruvate carboxylase
Nature Communications (2022)
-
Identification of a regulatory pathway inhibiting adipogenesis via RSPO2
Nature Metabolism (2022)