Abstract
Background/Objectives:
Insulin resistance (IR) is the cornerstone of the obesity-associated metabolic derangements observed in obese children. Targeted metabolomics was employed to explore the pathophysiological relevance of hyperinsulinemia in childhood obesity in order to identify biomarkers of IR with potential clinical application.
Subjects/Methods:
One hundred prepubertal obese children (50 girls/50 boys, 50% IR and 50% non-IR in each group), underwent an oral glucose tolerance test for usual carbohydrate and lipid metabolism determinations. Fasting serum leptin, total and high molecular weight-adiponectin and high-sensitivity C-reactive protein (CRP) levels were measured and the metabolites showing significant differences between IR and non-IR groups in a previous metabolomics study were quantified. Enrichment of metabolic pathways (quantitative enrichment analysis) and the correlations between lipid and carbohydrate metabolism parameters, adipokines and serum metabolites were investigated, with their discriminatory capacity being evaluated by receiver operating characteristic (ROC) analysis.
Results:
Twenty-three metabolite sets were enriched in the serum metabolome of IR obese children (P<0.05, false discovery rate (FDR)<5%). The urea cycle, alanine metabolism and glucose-alanine cycle were the most significantly enriched pathways (PFDR<0.00005). The high correlation between metabolites related to fatty acid oxidation and amino acids (mainly branched chain and aromatic amino acids) pointed to the possible contribution of mitochondrial dysfunction in IR. The degree of body mass index-standard deviation score (BMI-SDS) excess did not correlate with any of the metabolomic components studied. In the ROC analysis, the combination of leptin and alanine showed a high IR discrimination value in the whole cohort (area under curve, AUCALL=0.87), as well as in boys (AUCM=0.84) and girls (AUCF=0.91) when considered separately. However, the specific metabolite/adipokine combinations with highest sensitivity were different between the sexes.
Conclusions:
Combined sets of metabolic, adipokine and metabolomic parameters can identify pathophysiological relevant IR in a single fasting sample, suggesting a potential application of metabolomic analysis in clinical practice to better identify children at risk without using invasive protocols.
Similar content being viewed by others
Introduction
Insulin resistance (IR) is the initial step in metabolic impairment in obesity and represents the cornerstone in the pathophysiological development of metabolic syndrome.1 Despite this, how to assess IR is still a matter of debate, particularly in obese children. This is in part because insulin secretion and sensitivity are affected by processes such as growth and puberty. Moreover, the proposed indexes and diagnostic criteria for IR were developed in adults and their application to children is not unanimously accepted.2 The euglycemic-hyperinsulinemic clamp is considered the ‘gold-standard’ for diagnosis of IR, but its use is mainly restricted to experimental settings. In the clinic, IR is usually estimated by using diverse indexes taking into consideration glycemia and/or insulinemia in the fasting state (that is, homoeostasis model assessment (HOMA) index) or after oral glucose ingestion in the oral glucose tolerance test (OGTT).2
The importance of determining if the hyperinsulinism in an obese child is pathophysiologically relevant, as well as the role of IR in childhood obesity-associated metabolic derangement is undisputable. In growing and developing children, tissue plasticity must be considered as tissues respond differently to the development of obesity and, consequently, in the metabolic adaptation to this disease.3 These differences are in part because developing individuals have a higher rate of preadipocyte recruitment,3 leading to more adipocytes with a lower degree of hypertrophy. This results in functional changes in the secretion of adipokines related to body fat content (for example, leptin) and more importantly, to insulin sensitivity (for example, total and high molecular weight (HMW) adiponectin), resulting in a circulating adipokine profile different from that seen in obese adults.4, 5 In contrast to obese adults, fasting glucose impairment is a late (usually absent) finding, with a rise in insulinemia being the initial identifiable step of carbohydrate metabolism impairment in obese children.4 Thus, the study of metabolic pathways influenced by insulin signaling could help to identify biomarkers that indicate the pathophysiological relevance of the hyperinsulinism in young prepubertal obese children and the potential clinical application of these biomarkers.
Targeted metabolomics allows for the accurate quantification of specific metabolites of known identity and can provide a functional readout of the upstream variations underlying a disease or disease-related condition, such as obesity,6 and its link to type 2 diabetes (T2DM) and pre-diabetic states.7 While for adults several markers of obesity, IR and T2DM have been reported (that is, carbohydrate derivatives, ketone bodies, amino acid derivatives and saturated fatty acids, among others),8, 9 few metabolomic studies have investigated the pediatric population. Albeit limited, studies aimed at investigating the progression to childhood diabetes have provided insightful information, demonstrating changes in amino acid and lipid metabolism (mainly branched chain amino acids and acylcarnitines for T2DM and methionine, kynurenine and choline-containing lipids for T1DM), as well as suggesting a role for the gut microbiota in disease progression.10, 11 Metabolomics-based studies have also investigated childhood obesity and IR, highlighting early changes in the metabolome underlying the disease pathogenesis.12, 13, 14
While some authors indicate that none of the potential metabolomic biomarkers discovered to date have made the transition to routine use in clinical practice,15 others foresee this as being a near and feasible reality.16 Thus, our objective was to determine the possible translation of our previous results14 into a novel clinical tool. The specific aims were: (1) To evaluate the suitability of metabolomic biomarkers in the diagnosis of IR in obese children as an expression of the metabolic alterations and how this associates with the traditional clinical estimation based on serum glucose and insulin levels; (2) To investigate the relationship of these biomarkers with circulating adipokine levels that act as either surrogate markers of adiposity (leptin) or as insulin sensitivity modulators (adiponectin); and (3) To explore the possible usefulness of a combination of these parameters in the discrimination of metabolically significant IR in obese hyperinsulinemic children.
Patients and methods
Patients
One hundred prepubertal (Tanner stage I) obese (OB) children (BMI>+2 SDS according to Spanish standards and IOTF references for children17), were selected from a large cohort of 1300 obese children and adolescents at the Department of Endocrinology of the Hospital Infantil Universitario Niño Jesús (a monographic pediatric hospital for national referral). This study population included 50 girls and 50 boys, 50% IR and 50% non-IR in each group, showing previously validated metabolomic differences between IR and non-IR.14 The overall age was 7.83±2.70 years and 9.09±2.06 years for IR and 5.25±1.99 years for non-IR children. To be included in the study, the IR group had to demonstrate hyperinsulinism both in fasting and during the OGTT, while the non-IR group did not demonstrate hyperinsulinism at any time. The anthropometric and metabolic characteristics have been previously reported.14
All studies were approved by the scientific committee and ethics committee of the Hospital Infantil Universitario Niño Jesús. Written informed consent was obtained from all patients or their legal guardian.
Methods
Underlying pathological conditions were ruled-out prior to enrollment in the study. Body mass index (BMI) was recorded, standardized and used as an indirect estimator of body fat content (rather than waist circumference) due to its lower inter-observer variability and the possibility of more accurate standardization. An OGTT (1.75 g of glucose per kg; maximum 75 g) was performed, with blood samples drawn at 0, 30, 60 and 120 min after overnight fasting for glucose and insulin measurements. HbA1c, ALT, AST, GGT, uric acid and lipid profile were measured in the fasting sample. Samples were centrifuged and the serum stored at −80 ºC.
Patients were considered IR if their fasting insulin was above 15 μU ml−1 and they met one or more of the following criteria during the OGTT: peak insulin at 30 or 60 min>150 μU ml−1 or insulin>75 μU ml−1 at 120 min.2 The area under the curve (AUC) for glucose and insulin, HOMA-IR index and WBISI (whole body insulin sensitivity index) were calculated as previously reported.5, 14
Commercial kits (Linco, St Louis, MO, USA) were used to measure serum leptin and total and HMW adiponectin in fasting samples as previously reported.4 High-sensitivity C-reactive protein (HS-CRP) was measured by using a human high-sensitive CRP ELISA kit (Aviscera Bioscience, Inc., Santa Clara, CA, USA) according to the manufacturer’s instructions. The intra- and inter- assay variation coefficients were 5.2 and 9.8%, respectively.
Targeted metabolomics analysis
Metabolite quantification was performed by a targeted metabolomics approach by using liquid chromatography-mass spectrometry and gas chromatography-mass spectrometry (Agilent Technologies, Madrid, Spain) as described.18, 19 The metabolites included in the target analysis were the most representative metabolites that showed statistically significant differences between groups (obese children with and without IR, IR=30 and non-IR=30) in our preliminary fingerprinting study.14 See Supplementary Materials and Methods and Supplementary Table S1 for further details.
Statistical analysis
Statistical data analysis was carried out in four steps. First, the comparison of the quantitative variables between the studied groups (IR vs non-IR) was performed in SPSS version 20.0 (SPSS Inc., Armonk, NY, USA) using Student’s t-test for variables fitting a normal distribution (Kolmogorov–Smirnoff test) or by Mann–Whitney's U-test for non-normal variables. Second, the metabolite set was evaluated to highlight the metabolic pathways significantly enriched in the metabolic signature.20 For this purpose, the metabolite-set enrichment analysis was employed using the quantitative enrichment analysis feature in Metaboanalyst (http://www.metaboanalyst.ca/).21 Third, the bivariate relationship between HOMA-IR, leptin, adiponectin, triglycerides and serum metabolites was analyzed. The Spearman’s rank correlation (r) was used for comparative metabolomic correlations in SPSS, whereas the heatmap was employed to visualize all pairwise comparisons between metabolites. Fourth, the discriminatory capability of metabolites and clinical parameters, either individually or in clusters, was evaluated by the receiver operating characteristic (ROC) analysis in Metaboanalyst.21 In addition, because of the sex differences found in our previous study,14 the above statistical analyses were also performed for the male and female subgroups separately. Finally, a Benjamini–Hochberg False Discovery Rate post hoc correction (q=0.05) was applied to all data analyses performing multiple comparisons. See Supplementary Materials and Methods and Supplementary Table S2 for further details.
Results
Metabolic parameters and adipokine levels
Obese IR patients had higher indexes of IR and glycaemia, both fasting and after glucose ingestion, also higher uric acid and triglyceride levels.14 In addition, IR patients showed higher ALT (32.67±24.51 vs 21.93±7.20 IU l−1; P<0.01) and GGT levels (17.00±5.89 vs 12.12±4.15 IU l−1; P<0.001). Despite the fact that both groups were prepubertal, IR were older than non-IR patients (9.09±2.06 vs 5.25±1.99 y; P<0.001).
Despite similar mean body mass index-standard deviation score (BMI-SDS), IR patients exhibited higher leptin and lower total and HMW-adiponectin levels, resulting in a lower leptin/adiponectin ratio. There were no differences between groups in HS-CRP or HMW/total adiponectin ratio (Table 1). No difference between sexes was observed for adipokine levels.
Metabolite-set enrichment analysis
Twenty-three metabolite sets were enriched in the serum metabolome of IR compared to non-IR obese children (PFDR<0.05), with 13 matching more than one metabolite (Table 2). The urea cycle, alanine metabolism and glucose-alanine cycle were the most significantly enriched pathways (PFDR<0.00005), with pyruvate, alanine and ornithine being the most represented metabolites in the pathways.
Correlation study
Clinical parameters and adipokines
BMI-SDS did not correlate with adipokine levels nor with any of the metabolomic components studied, or with any of the indexes of IR. In contrast, leptin levels correlated negatively with WBISI (r=−0.59, P<0.001) and positively with HOMA index (r=+0.57, P<0.001). Adiponectin levels (both total and HMW) correlated negatively with HOMA (both r=−0.28, P<0.01) and positively with WBISI (total: r=+0.25, P<0.05, HMW: r=+0.31, P<0.01). HOMA index also correlated positively with triglyceride (r=+0.39, P<0.001), GGT (r=+0.45, P<0.001) and ALT levels (r=+0.26, P<0.05). WBISI negatively correlated with the same parameters: triglyceride (r=−0.32, P<0.01), GGT (r=−0.45, P<0.001) and ALT levels (r=−0.30, P<0.01). Neither HOMA nor WBISI correlated with AST or with HS-CRP levels.
Correlation between serum metabolites
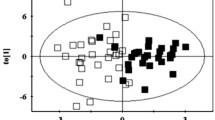
Thirty serum metabolites (13 amino acids and urea cycle intermediates, two bile acids, 12 acylcarnitines and three organic acids) were quantified (Supplementary Table S3). Correlation analysis (Supplementary Table S4) revealed several areas of highly correlated metabolites gathered in four main clusters with similar behavior across the studied population as shown in the heatmap (Figure 1). The highest correlation was among metabolites involved in fatty acid oxidation (for example, C08 and C10 acylcarnitines r=+0.93, P<0.001; C18 and C16 acylcarnitines r=+0.68, P<0.001) by indicating hot spots in the correlation matrix corresponding to metabolic pathways that might be altered in case of obesity and IR.
Correlation between metabolites and HOMA
When the whole cohort was studied, significant correlations were found between the HOMA index and several studied metabolites (Table 3). Two metabolites, C12 acylcarnitine (r=−0.35, P< 0.05) and methionine (r=+0.36, P<0.05), were found to correlate with HOMA index exclusively in the male subgroup.
Correlation between metabolites and triglycerides
In the whole cohort, significant correlations between triglyceride levels and alanine, glycodeoxycholate, 3-hydroxybutyrate, tryptophan, isoleucine, C03, C04 and C10 acylcarnitines were found (Table 3). Sex differences were observed, as methionine correlated with triglyceride levels exclusively in males (r=+0.34, P<0.05) and triglycerides correlated positively with pyruvic acid (r=+0.33, P<0.05) and valine (r=+0.29, P<0.05) and negatively with carnitines (free carnitine: r=−0.28, P<0.05 and C06: r=−0.29, P<0.05) only in females.
Leptin
In the whole cohort, leptin levels correlated with alanine, 3-hydroxybutyrate and tryptophan, as did triglycerides, but also with tyrosine and isoleucine (Table 3). In males leptin levels correlated negatively with methionine (r=+0.31, P<0.05) and in females leptin correlated positively with piperidine (r=+0.31,P<0.05).
Adiponectin
Adiponectin levels correlated with leucine, phenylalanine, valine and C03-acylcarnitine levels (Table 3). No metabolite correlated with adiponectin exclusively in males. In females, adiponectin levels correlated with tryptophan (r=−0.30, P<0.05) and several acylcarnitines (C2: r=−0.31, P<0.05; C4: r=−0.44, P<0.05; C5: r=−0.37, P<0.05 and C16: r=+0.30, P<0.05).
Receiver operator curve (ROC) analysis
In the ROC analysis, the combination of a clinically used adipokine determination (leptin) with one of the metabolites identified (alanine) showed a high AUC value for the discrimination of IR both when the cohort was studied as a whole (AUCALL=0.87), as when sexes were analyzed separately boys (AUCM=0.84), girls (AUCF=0.91) (Figures 2a–c).
Multi-metabolite biomarker ROC curves showing the best discriminatory capacity between insulin-resistant and non-insulin-resistant obese children. (a–c) ROC curves for the multi-metabolite biomarker 1 (alanine and leptin) in the overall cohort (a) and in the female (b) and male (c) subgroups. (d) ROC curve for the multi-metabolite biomarker 2 (isoleucine/pyroglutamate and leptin) in the female subgroup. (e) ROC curve for the multi-metabolite biomarker 3 (adiponectin/leptin and alanine) in the male subgroup. AUC value and its associated confidence interval together with the cutoff point (red dot) and its corresponding specificity and sensitivity values are depicted in the figure.
However, the specific metabolite/adipokine combination with highest sensitivity was different in girls and boys. In girls, the combination of isoleucine/pyroglutamate and leptin (AUC=0.94) had the highest sensitivity, while in boys it was the combination of adiponectin/leptin and alanine (AUC=0.86, Figures 2d–e).
Discussion
Here we investigated the relationship between anthropometrical and laboratory parameters of common clinical use to further investigate the metabolomic consequences of IR and to explore the role of metabolomic analysis in clinical practice. Our obese children were classified as IR or non-IR by using a combination of fasting and post-ingestion hyperinsulinism, with the pathophysiological relevance being reinforced by their differential metabolomic signatures. Euglycemic-hyperinsulinemic clamp and OGTT are time and resource consuming, cannot always be performed (depending on available facilities and patient conditions) and induce greater discomfort than a single fasting puncture, which is particularly relevant in children. We found that the combination of the common laboratory data, adipokine levels and metabolomic parameters from a single fasting sample could be useful in evaluating the relevance of fasting hyperinsulinism.
The relationship between BMI, adipokine levels, IR and metabolic derangement is not lineal and is only partially understood,22 especially in young children.4 Despite a similar BMI-SDS in our groups of obese children, hyperinsulinism and dyslipidaemia were only present in the IR group. The capacity for adipose tissue to expand and its functionality appear to be relevant in the development of metabolic comorbidities.23 Our findings are in agreement, as the IR group had higher leptin levels, possibly indicating a greater adipose mass despite similar BMI, and lower adiponectin levels. Together this suggests an early impairment in adipokine secretion that is not exclusively driven by the degree of BMI excess.
We previously reported correlations between parameters of carbohydrate/lipid metabolism and circulating adipokine levels in young obese prepubertal children similar to those observed here.3, 4 An important novel contribution of the present study is the demonstration that no correlations exist between BMI-SDS and any of the metabolomic markers studied. This, in addition to the metabolomic signature that differentiates IR and non-IR pre-pubertal obese children,14 indicates that something other than excess weight underlies the associated metabolic derangement.
Enrichment analysis highlighted the urea cycle, alanine metabolism and the glucose-alanine cycle as the most altered pathways in young IR obese children. Alanine, pyruvate and ornithine were consistently increased when IR was present, with alanine being the most significantly altered metabolite in IR obese children. Alanine had the highest direct correlation with HOMA, serum triglycerides and leptin, and in cluster with leptin this aa had the best discriminatory power for detecting IR in obese children. Alanine is the most abundant aa in proteins and, along with glutamine, the most abundant aa in the bloodstream. Thus, when proteolysis increases, as occurs in IR, the use of aa for gluconeogenesis is enhanced and circulating levels of alanine increase, as well as the nitrogen load on the liver, closely relating urea production to glucose synthesis and making alanine a possible hallmark indicating that key metabolic pathways have been modulated. Moreover, serum transaminases (that is, ALT and GGT) were significantly increased in IR patients. Increased transaminases have been associated to hepatic damage and fat deposition (linked to IR), with the concentration of ALT being highly correlated with the onset of cardiovascular disease and metabolic syndrome.24 There was also a correlation between ALT, alanine, pyruvate and ornithine.
The increase in serum ALT levels could contribute to the rise in alanine concentrations in the IR group. Consistent with our findings, studies in adults report an increase in alanine and pyruvate in obesity, IR and T2DM25, 26 as well as a correlation between serum alanine levels and HOMA index.27 In a longitudinal study, alanine levels, in addition to tyrosine, isoleucine, leucine and glutamine, were reported to predict the onset of diabetes up to 4.5 years in advance.28 Thus, modifications in circulating aa levels (alanine in our case) are one of the first detectable alterations in the early stages of carbohydrate metabolism impairment. An increase in circulating branched chain aa (BCAAs; that is, leucine, isoleucine and valine) and aromatic aa (ArAAs; that is, phenylalanine, tyrosine and tryptophan) was consistently found in conjunction with the rise in alanine levels in the IR state. Elevated levels of these metabolites have been associated with IR both in adults and children13, 27, 29 and BCAAs and ArAAs (phenylalanine and tyrosine) have been proposed as markers of obesity and predictors of IR and T2DM.13, 30 This is consistent with our finding that isoleucine/pyroglutamate and leptin is the best marker combination to discriminate IR in prepubertal obese females and this is supported by the positive correlation between BCAAs, ArAAs and HOMA. Interestingly, the BCAA isoleucine and the ArAAs tryptophan and tyrosine were positively correlated with leptin levels (isoleucine and tryptophan, also with triglyceride levels), possibly because leptin production by adipocytes is determined by their triglyceride content in response to insulin.31 This relationship could be bidirectional, as administration of 5-OH-tryptophan induces hyperleptinemia.32
Although leptin is reported to have insulin sensitizing effects when used therapeutically to treat leptin deficient states,33 the increased leptin levels observed in obesity are the hallmark of leptin resistance.34 Obese children are also hyperleptinemic, being even higher in our IR than in the non-IR group. Changes in the levels of ArAAs and their intermediate metabolites, together with increased leptin and decreased adiponectin levels, are reported to occur before IR is established.22 This is consistent with our finding that serum levels of the insulin sensitizing adipokine adiponectin were negatively correlated with the BCAAs (valine and leucine) and the ArAA phenylalanine. The relationship between adiponectin and the aa profile also appears to be bidirectional, as adiponectin administration corrects the altered BCAA metabolism induced by high-fat diet in mice,35 whereas leucine supplementation increases adiponectin production in cultured adipocytes.36 This effect is postulated to be mTOR mediated,37 but the underlying mechanisms remain unclear. A similar negative correlation between the circulating aa profile and adiponectin levels has been reported in adult T2DM patients, but no association with leptin levels was seen.38 This reinforces the novelty of the data reported here and stresses the postulated pathophysiological differences between children and adults.
There was also a strong correlation between BCAAs, ArAAs and short-chain acylcarnitines, as depicted in the heatmap. The increase in BCAAs, which can occur via several routes, has been previously attributed to alterations in their catabolism that causes the accumulation of byproducts that can affect mitochondrial function.27, 39 Interestingly, reduced mitochondrial number, size and activity has been described in skeletal muscle and adipose tissue of patients with obesity and T2DM.40, 41, 42 Altered mitochondrial morphology has also been associated with IR43 and decreased mitochondrial oxidation occurs in peripheral tissues even before IR is established,22 supporting the hypothesis that impaired mitochondrial capacity is linked to the development of IR and diabetes. Mitochondrial dysfunction is also reported to be an early indicator of IR in obese adolescents44 and in children, but not with obesity per se.45 Mitochondria produce energy from different substrates; thus, the accumulation of energy substrates (pyruvate, BCAA, fatty acids) and their byproducts (alanine, lactic acid, and acylcarnitines and so on) observed when IR was present might indicate mitochondrial dysfunction. Consistent with this, ornithine and short- and medium-chain acylcarnitines were increased, with a subtle decrease in long-chain acylcarnitines and free carnitine in IR. Of note, medium- and long-chain acylcarnitines were clustered to acetylcarnitine and 3-hydroxybutyrate in the heatmap. Additionally, C03 and C04 acylcarnitines positively correlated with HOMA and triglyceride levels and negatively with adiponectin levels, with the latter known to be an indicator of fatty acid oxidation through AMPK stimulation.46 Mitochondrial dysfunction decreases adiponectin secretion by adipocytes, resulting in lower glucose uptake and decreased phosphorylation of Akt upon insulin stimulation in myocytes47 and adipocytes.33
Cellular acylcarnitines regulate fatty acid β-oxidation;48 thus the decrease in 3-hydroxybutyrate and the correlation between serum triglycerides and these metabolites (positive to short-chain acylcarnitines and negative to 3-hydroxybutyrate), suggest inefficient β-oxidation that could lead to increased triglyceride synthesis and reduced ketone body levels. This is consistent with the altered lipid metabolism reported in the presence of obesity and IR. Decreased lipolysis in adipose tissue has been reported to promote/maintain excess body fat mass leading to childhood onset obesity.49 Increased fat cell size, in turn, has been shown to enhance basal lipolysis50 and alter adipokine secretion,51 resulting in increased fluxes of free fatty acids to liver and skeletal muscle. This, in turn, could then cause mitochondrial dysfunction52 and contribute to dyslipidemia and ectopic lipid deposition, as suggested by the higher ALT seen in obese children with IR, while promoting IR.53 The decrease in circulating 3-hydroxybutyrate levels, previously described in children12, 54, 55 may indicate that ketone inhibition by insulin is sufficiently preserved despite IR and that catabolism of fatty acids is reduced in obese children with IR. Here, 3-hydroxybutyrate levels were negatively correlated to HOMA and leptin levels, possibly indicating leptin resistance and IR, and indicate the necessity to explore the metabolism of lipids in IR obese children.
The metabolic derangement was different between IR boys and girls despite that they were prepubertal. Although the changes in methionine levels in the whole cohort were relatively small, being increased in females and unchanged in males, methionine positively correlated with HOMA, triglycerides and leptin only in males. A link between methionine metabolism and factors associated to IR, metabolic syndrome and T2DM has been previously reported.56 While dietary methionine restriction exerts a beneficial effect on TD2M,57, 58 increased homocysteine, a by-product of methionine, is reported to be a risk factor for T2DM in a sex-dependent fashion,59 which is consistent with our findings. Although we did not measure homocysteine levels or the effect of dietary methionine restriction, the correlations observed here suggest that further investigation of the possible sex difference is important.
Adiponectin negatively correlated with short-chain acylcarnitines and positively with long-chain acylcarnitines exclusively in females. It is possible that there is a sex-dependent relationship between mitochondrial dysfunction and adiponectin production, as previously shown for other conditions.60 In the ROC curve models with the highest sensitivity for IR, leptin was present for males and females, probably because it indicates greater adiposity and possible leptin resistance closely linked to IR, whereas adiponectin was only present in the model for males. We have previously shown that the evolution of serum adiponectin levels in healthy humans from mid puberty is sexually dimorphic.3 The findings here reinforce the idea that sex differences begin even prepubertally and emphasize the pathophysiological relevance of a prepubertal modification in adiponectin secretion in males.
One limitation of this study is the absence of a direct measurement of fat mass and distribution, which was instead indirectly estimated by BMI. This would have allowed a better measure of excess fat, as well as the discrimination of the eventual influence of patient age (higher in IR) and changes in fat mass/distribution on the observed differences in leptin levels, which cannot be ruled out. A second limitation of this study is that the relationship between lysophospholipids, related to inflammation and previously shown to differ between IR and non-IR prepubertal obese subjects,14 and inflammatory markers (HS-CRP) could not be explored. The lack of specificity of CRP and the high prevalence of mild infections inducing CRP and other markers in children difficult the establishment of a link between adiposity, IR and inflammation. Another limitation is the use of serum instead of tissue samples; indeed, although biofluids reflect physiological processes, it is impossible to determine the source of the metabolic alteration.
In conclusion, the results reported here reinforce the idea that the degree of BMI excess, which is routinely used in the clinical setting, is not the main predictor of metabolic impairment and that this impairment is already observed in young prepubertal children. Even though further research regarding the translation of the results obtained from metabolomics into clinical applications is still necessary, this study points to the possibility of designing sets of combined parameters (adipokines and metabolites) that could identify pathophysiological relevant IR in a single fasting sample, thus suggesting a potential application of metabolomics analysis in clinical practice.
References
Reaven GM . Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988; 37: 1595–1607.
Eyzaguirre F, Mericq V, Insulin resistance markers in children. Horm Res 71 Switzerland: 2009S. Karger AG: Basel, 2009; p 65–74.
Martos-Moreno GA, Barrios V, Chowen JA, Argente J . Adipokines in childhood obesity. Vitam Horm 2013; 91: 107–142.
Martos-Moreno GA, Barrios V, Martinez G, Hawkins F, Argente J . Effect of weight loss on high-molecular weight adiponectin in obese children. Obesity (Silver Spring) 2010; 18: 2288–2294.
Martos-Moreno GA, Kratzsch J, Korner A, Barrios V, Hawkins F, Kiess W et al. Serum visfatin and vaspin levels in prepubertal children: effect of obesity and weight loss after behavior modifications on their secretion and relationship with glucose metabolism. Int J Obes (Lond) 2011; 35: 1355–1362.
Zhang A, Sun H, Wang X . Power of metabolomics in biomarker discovery and mining mechanisms of obesity. Obes Rev 2013; 14: 344–349.
Guasch-Ferre M, Hruby A, Toledo E, Clish CB, Martinez-Gonzalez MA, Salas-Salvado J et al. Metabolomics in Prediabetes and Diabetes: A Systematic Review and Meta-analysis. Diabetes Care 2016; 39: 833–846.
Mastrangelo A, Barbas C, Chronic Diseases and Lifestyle Biomarkers Identification by Metabolomics. In: Sussulini A ed. Metabolomics: From Fundamentals to Clinical Applications Advances in Experimental Medicine and Biology 965. Springer International Publishing: New York, NY, 2017; p 235–263.
Suhre K, Meisinger C, Doring A, Altmaier E, Belcredi P, Gieger C et al. Metabolic footprint of diabetes: a multiplatform metabolomics study in an epidemiological setting. PLoS One 2010; 5: e13953.
Frohnert BI, Rewers MJ . Metabolomics in childhood diabetes. Pediatr Diabetes 2016; 17: 3–14.
Oresic M . Metabolomics in the studies of islet autoimmunity and type 1 diabetes. Rev Diabet Stud 2012; 9: 236–247.
Butte NF, Liu Y, Zakeri IF, Mohney RP, Mehta N, Voruganti VS et al. Global metabolomic profiling targeting childhood obesity in the Hispanic population. Am J Clin Nutr 2015; 102: 256–267.
McCormack SE, Shaham O, McCarthy MA, Deik AA, Wang TJ, Gerszten RE et al. Circulating branched-chain amino acid concentrations are associated with obesity and future insulin resistance in children and adolescents. Pediatr Obes 2013; 8: 52–61.
Mastrangelo A, Martos-Moreno GA, Garcia A, Barrios V, Ruperez FJ, Chowen JA et al. Insulin resistance in prepubertal obese children correlates with sex-dependent early onset metabolomic alterations. Int J Obes (Lond) 2016; 40: 1494–1502.
Mamas M, Dunn WB, Neyses L, Goodacre R . The role of metabolites and metabolomics in clinically applicable biomarkers of disease. Arch Toxicol 2011; 85: 5–17.
Klein MS, Shearer J . Metabolomics and Type 2 Diabetes: Translating Basic Research into Clinical Application. J Diabetes Res 2016; 2016: 3898502.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. Bmj 2000; 320: 1240–1243.
Naz S, Calderon AA, Garcia A, Gallafrio J, Mestre RT, Gonzalez EG et al. Unveiling differences between patients with acute coronary syndrome with and without ST elevation through fingerprinting with CE-MS and HILIC-MS targeted analysis. Electrophoresis 2015; 36: 2303–2313.
Mastrangelo A, Ferrarini A, Rey-Stolle F, Garcia A, Barbas C . From sample treatment to biomarker discovery: A tutorial for untargeted metabolomics based on GC-(EI)-Q-MS. Anal Chim Acta 2015; 900: 21–35.
Xia J, Wishart DS . MSEA: a web-based tool to identify biologically meaningful patterns in quantitative metabolomic data. Nucleic Acids Res 2010; 38: W71–W77.
Xia J, Sinelnikov IV, Han B, Wishart DS . MetaboAnalyst 3.0—making metabolomics more meaningful. Nucleic Acids Res 2015; 43: W251–W257.
Munoz-Garach A, Cornejo-Pareja I, Tinahones FJ . Does metabolically healthy obesity exist? Nutrients 2016; 8: 6.
Giesbertz P, Daniel H . Branched-chain amino acids as biomarkers in diabetes. Curr Opin Clin Nutr Metab Care 2016; 19: 48–54.
Goessling W, Massaro JM, Vasan RS, D'Agostino RB Sr, Ellison RC, Fox CS . Aminotransferase levels and 20-year risk of metabolic syndrome, diabetes, and cardiovascular disease. Gastroenterology 2008; 135: 1935–1944 44.e1.
Wang TJ, Larson MG, Vasan RS, Cheng S, Rhee EP, McCabe E et al. Metabolite profiles and the risk of developing diabetes. Nat Med 2011; 17: 448–453.
Li LO, Hu YF, Wang L, Mitchell M, Berger A, Coleman RA . Early hepatic insulin resistance in mice: a metabolomics analysis. Mol Endocrinol 2010; 24: 657–666.
Newgard CB, An J, Bain JR, Muehlbauer MJ, Stevens RD, Lien LF et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab 2009; 9: 311–326.
Stancakova A, Civelek M, Saleem NK, Soininen P, Kangas AJ, Cederberg H et al. Hyperglycemia and a common variant of GCKR are associated with the levels of eight amino acids in 9,369 Finnish men. Diabetes 2012; 61: 1895–1902.
Lee A, Jang HB, Ra M, Choi Y, Lee HJ, Park JY et al. Prediction of future risk of insulin resistance and metabolic syndrome based on Korean boy's metabolite profiling. Obes Res Clin Pract 2014; 9: 336–345.
Hellmuth C, Uhl O, Kirchberg FF, Grote V, Weber M, Rzehak P et al. Effects of Early Nutrition on the Infant Metabolome. Nestle Nutr Inst Workshop Ser 2016; 85: 89–100.
Meier U, Gressner AM . Endocrine regulation of energy metabolism: review of pathobiochemical and clinical chemical aspects of leptin, ghrelin, adiponectin, and resistin. Clin Chem 2004; 50: 1511–1525.
Yamada J, Ujikawa M, Sugimoto Y . Serum leptin levels after central and systemic injection of a serotonin precursor, 5-hydroxytryptophan, in mice. Eur J Pharmacol 2000; 406: 159–162.
Park HK, Ahima RS . Physiology of leptin: energy homeostasis, neuroendocrine function and metabolism. Metabolism 2015; 64: 24–34.
Wang CH, Wang CC, Huang HC, Wei YH . Mitochondrial dysfunction leads to impairment of insulin sensitivity and adiponectin secretion in adipocytes. Febs j 2013; 280: 1039–1050.
Liu Y, Turdi S, Park T, Morris NJ, Deshaies Y, Xu A et al. Adiponectin corrects high-fat diet-induced disturbances in muscle metabolomic profile and whole-body glucose homeostasis. Diabetes 2013; 62: 743–752.
Blumer RM, van Roomen CP, Meijer AJ, Houben-Weerts JH, Sauerwein HP, Dubbelhuis PF . Regulation of adiponectin secretion by insulin and amino acids in 3T3-L1 adipocytes. Metabolism 2008; 57: 1655–1662.
Zhang HH, Huang J, Duvel K, Boback B, Wu S, Squillace RM et al. Insulin stimulates adipogenesis through the Akt-TSC2-mTORC1 pathway. PLoS One 2009; 4: e6189.
Nakamura H, Jinzu H, Nagao K, Noguchi Y, Shimba N, Miyano H et al. Plasma amino acid profiles are associated with insulin, C-peptide and adiponectin levels in type 2 diabetic patients. Nutr Diabetes 2014; 4: e133.
Koves TR, Ussher JR, Noland RC, Slentz D, Mosedale M, Ilkayeva O et al. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab 2008; 7: 45–56.
Kelley DE, He J, Menshikova EV, Ritov VB . Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 2002; 51: 2944–2950.
Ritov VB, Menshikova EV, He J, Ferrell RE, Goodpaster BH, Kelley DE . Deficiency of subsarcolemmal mitochondria in obesity and type 2 diabetes. Diabetes 2005; 54: 8–14.
Bogacka I, Xie H, Bray GA, Smith SR . Pioglitazone induces mitochondrial biogenesis in human subcutaneous adipose tissue in vivo. Diabetes 2005; 54: 1392–1399.
Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI . Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med 2004; 350: 664–671.
Slattery MJ, Bredella MA, Thakur H, Torriani M, Misra M . Insulin resistance and impaired mitochondrial function in obese adolescent girls. Metab Syndr Relat Disord 2014; 12: 56–61.
Fleischman A, Kron M, Systrom DM, Hrovat M, Grinspoon SK . Mitochondrial function and insulin resistance in overweight and normal-weight children. J Clin Endocrinol Metab 2009; 94: 4923–4930.
Chen H, Zhang L, Li X, Sun G, Yuan X, Lei L et al. Adiponectin activates the AMPK signaling pathway to regulate lipid metabolism in bovine hepatocytes. J Steroid Biochem Mol Biol 2013; 138: 445–454.
Wang CH, Wang CC, Wei YH . Mitochondrial dysfunction in insulin insensitivity: implication of mitochondrial role in type 2 diabetes. Ann N Y Acad Steroid 2010; 1201: 157–165.
Kerner J, Hoppel C . Fatty acid import into mitochondria. Biochim Biophys Acta 2000; 1486: 1–17.
Bougneres P, Stunff CL, Pecqueur C, Pinglier E, Adnot P, Ricquier D . In vivo resistance of lipolysis to epinephrine. A new feature of childhood onset obesity. J Clin Invest 1997; 99: 2568–2573.
Jacobsson B, Smith U . Effect of cell size on lipolysis and antilipolytic action of insulin in human fat cells. J Lipid Res 1972; 13: 651–656.
Skurk T, Alberti-Huber C, Herder C, Hauner H . Relationship between adipocyte size and adipokine expression and secretion. J Clin Endocrinol Metab 2007; 92: 1023–1033.
Yang C, Aye CC, Li X, Diaz Ramos A, Zorzano A, Mora S . Mitochondrial dysfunction in insulin resistance: differential contributions of chronic insulin and saturated fatty acid exposure in muscle cells. Biosci Rep 2012; 32: 465–478.
Jung UJ, Choi MS . Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int J Mol Sci 2014; 15: 6184–6223.
Newbern D, Gumus Balikcioglu P, Balikcioglu M, Bain J, Muehlbauer M, Stevens R et al. Sex differences in biomarkers associated with insulin resistance in obese adolescents: metabolomic profiling and principal components analysis. J Clin Endocrinol Metab 2014; 99: 4730–4739.
Wurtz P, Makinen VP, Soininen P, Kangas AJ, Tukiainen T, Kettunen J et al. Metabolic signatures of insulin resistance in 7,098 young adults. Diabetes 2012; 61: 1372–1380.
Adams SH . Emerging perspectives on essential amino acid metabolism in obesity and the insulin-resistant state. Adv Nutr 2011; 2: 445–456.
Plaisance EP, Greenway FL, Boudreau A, Hill KL, Johnson WD, Krajcik RA et al. Dietary methionine restriction increases fat oxidation in obese adults with metabolic syndrome. J Clin Endocrinol Metab 2011; 96: E836–E840.
Stone KP, Wanders D, Orgeron M, Cortez CC, Gettys TW . Mechanisms of increased in vivo insulin sensitivity by dietary methionine restriction in mice. Diabetes 2014; 63: 3721–3733.
Masuda Y, Kubo A, Kokaze A, Yoshida M, Fukuhara N, Takashima Y . Factors associated with serum total homocysteine level in type 2 diabetes. Environ Health Prev Med 2008; 13: 148–155.
Demarest TG, Schuh RA, Waite EL, Waddell J, McKenna MC, Fiskum G . Sex dependent alterations in mitochondrial electron transport chain proteins following neonatal rat cerebral hypoxic-ischemia. J Bioenerg Biomembr 2016; 48: 591–598.
Acknowledgements
AM received a PhD grant from the Spanish Ministry of Economy and Competitiveness (AP-2012-1385). We express our gratitude to the financial support received from the Spanish Ministry of Economy and Competitiveness MINECO CTQ2014-55279-R (CB) and BFU2014-51836-C2-2R (JAC); Fondo de Investigación Sanitaria with Fondos FEDER [FIS: PI13/01295 and PI16/00485 (JA)] and CIBER Fisiopatología de la Obesidad y Nutrición (CIBEROBN) (JA and JAC). Instituto de Salud Carlos III. Madrid, Spain and Fundación Endocrinología y Nutrición.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Martos-Moreno, G., Mastrangelo, A., Barrios, V. et al. Metabolomics allows the discrimination of the pathophysiological relevance of hyperinsulinism in obese prepubertal children. Int J Obes 41, 1473–1480 (2017). https://doi.org/10.1038/ijo.2017.137
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.137
- Springer Nature Limited
This article is cited by
-
Probing erythrocytes as sensitive and reliable sensors of metabolic disturbances in the crosstalk between childhood obesity and insulin resistance: findings from an observational study, in vivo challenge tests, and ex vivo incubation assays
Cardiovascular Diabetology (2024)
-
NMR-based metabolic profiling of children with premature adrenarche
Metabolomics (2022)
-
Paediatric obesity: a systematic review and pathway mapping of metabolic alterations underlying early disease processes
Molecular Medicine (2021)
-
Metabolomics approach by 1H NMR spectroscopy of serum reveals progression axes for asymptomatic hyperuricemia and gout
Arthritis Research & Therapy (2018)