Abstract
Background:
Hypothalamic obesity is a devastating consequence of craniopharyngioma. Bariatric surgery could be a promising therapeutic option. However, its efficacy and safety in patients with craniopharyngioma-related hypothalamic obesity remain largely unknown.
Objectives:
We investigated the efficacy of bariatric surgery for inducing weight loss in patients with craniopharyngioma-related hypothalamic obesity. In addition, we studied the safety of bariatric surgery regarding its effects on hormone replacement therapy for pituitary insufficiency.
Methods:
In this retrospective matched case–control study, we compared weight loss after bariatric surgery (that is, Roux-en-Y gastric bypass and sleeve gastrectomy) between eight patients with craniopharyngioma-related hypothalamic obesity and 75 controls with ‘common’ obesity during 2 years of follow-up. We validated our results at 1 year of follow-up in a meta-analysis. In addition, we studied alterations in hormone replacement therapy after bariatric surgery in patients with craniopharyngioma.
Results:
Mean weight loss after bariatric surgery was 19% vs 25% (difference −6%, 95% confidence of interval (CI) −14.1 to 4.6; P=0.091) at 2 years of follow-up in patients with craniopharyngioma-related hypothalamic obesity compared with control subjects with ‘common’ obesity. Mean weight loss was 25% vs 29% (difference −4%, 95% CI −11.6 to 8.1; P=0.419) after Roux-en-Y gastric bypass and 10% vs 20% (difference −10%, 95% CI −14.1 to −6.2; P=0.003) after sleeve gastrectomy at 2 years of follow-up in patients with craniopharyngioma-related hypothalamic obesity vs control subjects with ‘common’ obesity. Our meta-analysis demonstrated significant weight loss 1 year after Roux-en-Y gastric bypass, but not after sleeve gastrectomy. Seven patients with craniopharyngioma suffered from pituitary insufficiency; three of them required minor adjustments in hormone replacement therapy after bariatric surgery.
Conclusions:
Weight loss after Roux-en-Y gastric bypass, but not sleeve gastrectomy, was comparable between patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity at 2 years of follow-up. Bariatric surgery seems safe regarding its effects on hormone replacement therapy.
Similar content being viewed by others
Introduction
Craniopharyngiomas are benign epithelial neoplasms located in the sellar and/or suprasellar region of the skull that occur in both children and adults. Their treatment generally consists of neurosurgical excision with or without postoperative radiotherapy.1 Long-term tumour- and/or treatment-related morbidities, including pituitary hormone deficiencies and morbid obesity related to hypothalamic dysfunction, occur frequently and may result in premature mortality.2 Hypothalamic obesity and its comorbidities are among the most devastating consequences of craniopharyngioma,3 and affect ~55% of the patients.4
Hypothalamic obesity is considered to be an ‘endogenous’ type of obesity, in which hypothalamic damage is postulated to result in autonomic nervous system dysfunction, as well as acquired leptin and insulin resistance, which altogether adversely affect food intake and food satisfaction, metabolism, as well as energy expenditure.5 Therefore, it seems to be a distinct entity separated from ‘exogenous’ or ‘common’ obesity, in which excessive caloric intake promotes weight gain.6 Hypothalamic dysfunction is a major contributor to the morbid obesity commonly observed in patients with craniopharyngioma. However, other factors like familial predisposition for obesity and reduced physical activity, which may be related to neurological and visual dysfunction, increased daytime sleepiness and psychological difficulties may also contribute to excessive weight gain.7, 8, 9 Patients with craniopharyngioma-related hypothalamic obesity experience continuous weight gain that evolves predominantly during the first year after craniopharyngioma treatment.10, 11 Hypothalamic obesity is, similar to ‘common’ obesity,6 largely resistant to lifestyle modification.12 In addition, pharmacological treatment strategies show only modest results coupled with significant side effects.5 As bariatric surgery has proven to be highly effective in the ‘common’ obese population,13 it has been proposed as a therapeutic option for hypothalamic obesity as well.14 However, studies on the efficacy and safety of bariatric surgery for craniopharyngioma-related hypothalamic obesity remain scarce, and do not compare achieved weight loss with matched control subjects.
As many patients with craniopharyngioma require hormone replacement therapy for pituitary hormone deficiencies,2 and bariatric surgery might affect drug absorption and bioavailability,15 it is important to consider the effects of bariatric procedures on endocrine substitution regimens. This is enforced by differences in pharmacokinetics and pharmacodynamics between obese and lean subjects,16 which may reasonably change after significant weight loss. Nonetheless, the effects of bariatric surgery on hormone replacement therapy have not been addressed extensively in prior studies. Up until now, only one small study specifically investigated the absorption of hormone replacement therapy in patients with craniopharyngioma after bariatric surgery.17
The primary aim of our study was to investigate the efficacy of bariatric surgery for inducing weight loss in patients with craniopharyngioma-related hypothalamic obesity. As secondary aims, we studied the effects of bariatric surgery on hormone replacement therapy and presence of treatment for diabetes mellitus, hypertension and dyslipidaemia. Accordingly, we performed the first matched case–control study that compared bariatric surgery-induced weight loss between patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity. We validated our results on bariatric surgery-induced weight loss in patients with craniopharyngioma-related hypothalamic obesity in a meta-analysis. In addition, we investigated the safety of bariatric surgery regarding its effects on hormone replacement therapy for pituitary insufficiency. As a result, we conducted the first study addressing both the efficacy and safety of bariatric surgery in patients with craniopharyngioma-related hypothalamic obesity.
Materials and methods
Study participants
In this retrospective matched case–control study, we compared bariatric surgery-induced weight loss between patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity. Patients with craniopharyngioma who underwent bariatric surgery were identified by a computer-based search in the electronic patient files of the Erasmus University Medical Centre (Rotterdam, the Netherlands) and the Sahlgrenska University Hospital (Gothenburg, Sweden). Eight of such patients were identified (four Dutch and four Swedish patients). In the Dutch cases, all bariatric procedures had been performed at dedicated regional centres experienced in weight-loss surgery. In the Swedish patients, all but one bariatric procedure had been performed at the Sahlgrenska University Hospital. In all eight patients, diagnoses of craniopharyngioma were pathology-proven and craniopharyngioma-related hypothalamic and/or third ventricle damage was demonstrated by neuroimaging. Pituitary hormone deficiencies were diagnosed on the basis of pituitary function testing or complete neurosurgical removal of the pituitary stalk and/or gland.
Patients with craniopharyngioma were individually matched to 6–10 control subjects with ‘common’ obesity, which yielded a total of 75 control participants. Control subjects were derived from the Scandinavian Obesity Surgery Registry (SOReg), which is a Swedish nationwide registry that includes more than 40 000 individuals treated with bariatric surgery from all over the country.18 Matching was based on the type and date of bariatric procedure, age, gender, preoperative body mass index and preoperative morbidity (that is, presence of diabetes mellitus and/or hypertension). Ethical approval was obtained from the local institutional review board of the Erasmus University Medical Centre and the regional ethical review board in Gothenburg, Sweden. All patients gave their informed consent.
Outcomes of interest
We compared weight loss between patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity at 6 weeks, 1 year and 2 years of follow-up after bariatric procedure. We validated our results on weight loss at 1 year of follow-up in patients with craniopharyngioma-related hypothalamic obesity in a meta-analysis. In addition, we studied bariatric surgery-induced alterations in hormone replacement therapy for pituitary insufficiency in patients with craniopharyngioma. Furthermore, we compared presence of treatment for diabetes mellitus, hypertension and dyslipidaemia between patients with craniopharyngioma and control subjects before, as well as 1 year after bariatric procedure.
Adjustments in the daily recombinant human growth hormone dose, necessary to maintain serum insulin-like growth factor I (IGF-I) levels within the age- and sex-adjusted reference range, represented the influence of bariatric surgery on growth hormone replacement therapy. Adjustments in the daily levothyroxine dose, necessary to maintain serum free thyroxine (fT4) levels within the reference range, were used to express bariatric surgery-induced alterations in thyroid hormone substitution. Hospital admissions for adrenal crises post- vs pre-bariatric surgery, as well as adjustments in the daily hydrocortisone dose, were used as indicators for bariatric surgery-induced alterations in hydrocortisone therapy. Switches in the oestrogen–progestin replacement therapy preparation due to signs and symptoms of oestrogen deficiency represented the influence of bariatric surgery on oestrogen–progestin replacement therapy. The influence of bariatric surgery on testosterone replacement therapy was assessed by adjustments in the testosterone dose, necessary to keep serum testosterone levels within the reference range. Adjustments in the daily desmopressin dose, required to reach an acceptable amount of fluid intake and diuresis throughout the day, were used as an indicator for bariatric surgery-induced alterations in desmopressin treatment. In addition, changes in hormone replacement therapy formulation type due to signs and symptoms of ineffective endocrine substitution were studied.
Data collection
Relevant clinical data on patient characteristics, medical status, craniopharyngioma treatment, bariatric surgery, anthropometry, use of hormone replacement therapy, antidiabetic agents, antihypertensive medication and antihyperlipidemic drugs were retrieved from the medical records of the patients with craniopharyngioma. The Scandinavian Obesity Surgery Registry provided the relevant information regarding the control subjects.
Statistics
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS 24, Chicago, IL, USA) and Review Manager (RevMan version 5.3, The Cochrane Collaboration, 2014). Continuous data were represented as mean±standard deviation (s.d.), or median and range. Categorical data were represented as observed frequencies and percentages. Baseline characteristics were compared between patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity by Mann–Whitney U-tests and Fisher’s exact tests for numerical and categorical data, respectively. Because of the matched case–control design of our study, weight loss was compared between cases and controls using a one-factor generalised randomised block design. Two-way analyses of variances were performed, in which the matched case–control units were included as blocks. Percentage weight loss at 6 weeks, 1 year and 2 years were considered dependent variables, and either being a patient with craniopharyngioma or a control subject as the independent variable. Bootstrapping with 1000 replicates was performed as assumptions of two-way analysis of variance were not met initially. Presence of treatment for diabetes mellitus, hypertension and dyslipidaemia at 1 year after bariatric procedure was compared between cases and controls using conditional logistic regression. To validate our results on bariatric surgery-induced weight loss in patients with craniopharyngioma-related hypothalamic obesity, we performed a meta-analysis in which we compared body mass index at 1 year of follow-up after bariatric surgery with body mass index at bariatric procedure. We included all patients who received a Roux-en-Y gastric bypass or sleeve gastrectomy for craniopharyngioma-related hypothalamic obesity with sufficient follow-up data at 1 year after bariatric surgery published previously,19 and added our own eight patients. This yielded a total of 20 patients. Data were pooled using the inverse variance method with a random-effects model, and mean differences and corresponding 95% confidence intervals (CI) were calculated. We estimated statistical heterogeneity between studies using the I2 statistic.20 We considered a P-value<0.05 statistically significant.
Results
Patient characteristics
Characteristics of the patients with craniopharyngioma are shown in Table 1. Six patients were treated for craniopharyngioma at an age <18 years and two at an age ⩾18 years. Subsequently, all patients developed hypothalamic obesity for which bariatric surgery was applied a median 13 years (range 2–26 years) after craniopharyngioma treatment. Five patients received a Roux-en-Y gastric bypass, and three a sleeve gastrectomy. One patient underwent a second bariatric procedure (that is, Roux-en-Y gastric bypass) ~2 years after a sleeve gastrectomy due to insufficient weight loss. In this patient, only data until the second weight-loss surgery were taken into account.
Baseline characteristics of patients with craniopharyngioma-related hypothalamic obesity compared with matched control subjects with ‘common’ obesity are shown in Table 2. Baseline characteristics were comparable, although patients with craniopharyngioma who underwent sleeve gastrectomy were more likely to use antihypertensive medication before bariatric surgery (P=0.033).
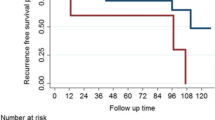
Weight loss after bariatric surgery
Weight loss after bariatric surgery in patients with craniopharyngioma-related hypothalamic obesity compared with control subjects with ‘common’ obesity is shown in Figure 1. Mean percentage weight loss after bariatric surgery was 12% vs 9% (difference 3%, 95% CI −2 to 6.2; P=0.196) at 6 weeks, 20% vs 25% (difference −5%, 95% CI −11.7 to 2.2; P=0.141) at 1 year and 19% vs 25% (difference −6%, 95% CI −14.1 to 4.6; P=0.091) at 2 years of follow-up in patients with craniopharyngioma-related hypothalamic obesity compared with control subjects with ‘common’ obesity. After Roux-en-Y gastric bypass, mean percentage weight loss was 12% vs 10% (difference 2%, 95% CI −4.2 to 8.1; P=0.443) at 6 weeks, 25% vs 30% (difference −5%, 95% CI −14.4 to 5.2; P=0.257) at 1 year and 25% vs 29% (difference −4%, 95% CI −11.6 to 8.1; P=0.419) at 2 years of follow-up in patients with craniopharyngioma-related hypothalamic obesity vs control subjects with ‘common’ obesity. Mean percentage weight loss after sleeve gastrectomy was 12% vs 8% (difference 4%, 95% CI −1.3 to 6.9; P=0.117) at 6 weeks, 12% vs 17% (difference −5%, 95% CI −15.5 to 3.2; P=0.334) at 1 year and 10% vs 20% (difference −10%, 95% CI −14.1 to −6.2; P=0.003) at 2 years of follow-up in patients with craniopharyngioma-related hypothalamic obesity vs control subjects with ‘common’ obesity. All but one patient with craniopharyngioma lost weight markedly after bariatric surgery. We have no clear explanation for the weight-loss failure in this particular patient who underwent a sleeve gastrectomy.
Mean percentage weight loss (± bootstrapped standard error) after bariatric surgery in patients with craniopharyngioma-related hypothalamic obesity compared with control subjects with ‘common’ obesity. (a) Both bariatric procedures combined. (b) Roux-en-Y gastric bypass. (c) Sleeve gastrectomy. %, percentage; Cranio, patients with craniopharyngioma; RYGB, Roux-en-Y gastric bypass.
We validated our results on bariatric surgery-induced weight loss in patients with craniopharyngioma-related hypothalamic obesity by performing a meta-analysis in which we compared body mass index at 1 year of follow-up after bariatric surgery with body mass index at bariatric procedure (Figure 2). We observed significant weight loss after bariatric surgery (mean 8.78, 95% CI 2.60 to 14.95 kg m−2). Although Roux-en-Y gastric bypass resulted in significant weight loss (mean 11.10, 95% CI 2.32 to 19.88 kg m−2), sleeve gastrectomy was less effective (mean 6.50, 95% CI −2.18 to 15.18 kg m−2).
Effects of bariatric surgery on hormone replacement therapy
Effects of bariatric surgery on hormone replacement therapy are shown in Table 3. Seven of eight patients with craniopharyngioma used hormone replacement therapy for pituitary insufficiency. In the patients using growth hormone replacement, serum IGF-I levels declined during the first year after bariatric surgery in all but one patient (data not shown). In two patients, this enforced a minor increase in the daily recombinant human growth hormone dose. The daily levothyroxine dose was reduced in three patients during the first 12 months after bariatric surgery. No patients were admitted to the hospital for adrenal crisis pre- or post-bariatric procedure. In addition, no adjustments in the daily hydrocortisone dose were necessary. One patient switched from oestradiol 2 mg/dydrogesteron 10 mg oestrogen-progestin replacement to ethinyloestradiol 30 μg/levonorgestrel 150 μg ~2 months after bariatric procedure; 5 months later she switched to ethinyloestradiol 50 μg/levonorgestrel 125 μg. No adjustments in the prescribed testosterone replacement therapy were required after bariatric surgery. In two of six patients using desmopressin, the daily dose had to be slightly increased after bariatric surgery. No patient required any change in formulation type of endocrine substitution therapy.
Diabetes mellitus, hypertension and dyslipidaemia
Presence of treatment for diabetes mellitus, hypertension and dyslipidaemia before, as well as 1 year after bariatric surgery in patients with craniopharyngioma-related hypothalamic obesity compared with control subjects with ‘common’ obesity is shown in Table 4. At 1 year of follow-up after bariatric surgery, there were no significant differences in the use of antidiabetic, antihypertensive and antihyperlipidemic agents between cases and controls. Presence of treatment for diabetes mellitus, hypertension and dyslipidaemia in patients with craniopharyngioma before and 1 year after bariatric surgery was 12.5% vs 0%, 50% vs 25% and 12.5% vs 12.5%, respectively.
Discussion
This matched case–control study is the first to address two of the most important clinical questions on bariatric surgery for craniopharyngioma-related hypothalamic obesity: does bariatric surgery results in sufficient weight loss, and is bariatric surgery safe regarding its effects on hormone replacement therapy for pituitary insufficiency? We compared bariatric surgery-induced weight loss between patients with craniopharyngioma-related hypothalamic obesity and extensively matched control subjects with ‘common’ obesity. In addition, we validated our results on weight loss in patients with craniopharyngioma-related hypothalamic obesity in a meta-analysis. Moreover, we investigated the effects of bariatric surgery on hormone replacement therapy for pituitary insufficiency. At 2 years of follow-up, weight loss after Roux-en-Y gastric bypass, but not sleeve gastrectomy, was comparable between patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity. Accordingly, our meta-analysis revealed significant weight loss after Roux-en-Y gastric bypass at 1 year of follow-up after bariatric surgery in patients with craniopharyngioma-related hypothalamic obesity; sleeve gastrectomy was less effective. Minor adjustments in hormone replacement therapy were required in three of seven patients with craniopharyngioma.
One other case–control study compared weight loss after bariatric surgery between patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity. In this retrospective non-matched study, Weismann et al. included nine patients with craniopharyngioma and 143 control subjects. In their study, two patients with craniopharyngioma received a Roux-en-Y gastric bypass, and four a sleeve gastrectomy.21 In concordance with our results, weight loss after bariatric surgery was only comparable between cases and controls in the subset of patients who received a Roux-en-Y gastric bypass. In the study by Weismann et al.,21 control subjects were significantly older and presented more pronounced metabolic disturbances at baseline compared with patients with craniopharyngioma. In the present study, we validated our results on bariatric surgery-induced weight loss in patients with craniopharyngioma-related hypothalamic obesity by performing a meta-analysis. Consequently, we updated a previous meta-analysis by Bretault et al.19 This prior meta-analysis studied weight loss at 6 months and 1 year of follow-up after bariatric surgery and could not demonstrate significant weight loss after Roux-en-Y gastric bypass or sleeve gastrectomy.
At the moment, it is still largely unknown by what exact mechanisms bariatric procedures establish their effects. Alterations in eating behaviour and energy homoeostasis due to a combination of changes in gut hormone and autonomous nervous system signalling are thought to be responsible for weight loss and improved glycaemic control. Bariatric surgery-induced alterations in blood–bile acid concentrations and gut microbiota may also contribute to weight decline.22 Hypothalamic structures, like the ventromedial nucleus, arcuate nucleus, paraventricular nucleus, lateral hypothalamic area, dorsomedial nucleus, dorsal hypothalamic area, supraoptic nucleus and suprachiasmatic nucleus are key regulators in balancing feeding behaviour and energy expenditure by integrating gut hormone and autonomous nervous system signalling.5, 23 Craniopharyngiomas and/or their treatment may damage these important brain structures, thereby resulting in autonomic nervous system dysfunction and acquired leptin and insulin resistance, which subsequently adversely alter food intake and food satisfaction, metabolism, as well as energy expenditure.5 This could diminish the efficacy of bariatric procedures like Roux-en-Y gastric bypass and sleeve gastrectomy, which may rely, at least partly, on intact hypothalamic function for their beneficial effects.24 However, we observed a weight loss similar to control subjects with ‘common’ obesity in most of our patients with craniopharyngioma-related hypothalamic obesity after bariatric surgery. This may be explained by the observation that brain circuits and gut hormone receptors thought to be important in exerting beneficial effects of bariatric procedures are not only found in the hypothalamus, but in other brain regions probably not affected by the craniopharyngioma and/or its treatment as well.24 Consequently, weight-loss-promoting changes in gut hormone and autonomous nervous system signalling can probably still exert some of their beneficial effects in patients with craniopharyngioma-related hypothalamic obesity.
Bariatric procedures potentially influence drug absorption and bioavailability.15 In addition, pharmacokinetics and pharmacodynamics, which are different in obese and lean subjects,16 may reasonably change following weight loss, possibly resulting in altered drug dose requirements. Therefore, it is important to consider the effects of bariatric surgery on hormone replacement therapy for pituitary insufficiency in patients with craniopharyngioma. In our study, seven patients with craniopharyngioma used endocrine substitution regimens. Bariatric surgery did not seem to affect hormone replacement therapy significantly, although one might expect lower levothyroxine requirements due to the bariatric surgery-induced weight loss.25 Therefore, it seems likely that the absorption of some hormones might be decreased. Other studies addressing bariatric surgery-induced alterations in hormone replacement therapy are scarce. A recent study by Wolf et al. reported no significant changes in the administered daily recombinant human growth hormone, levothyroxine, hydrocortisone and desmopressin dose in four patients with craniopharyngioma at 13–65 months of follow-up after gastric bypass compared with baseline. In addition, no adrenal crises were observed. An oral thyroid/hydrocortisone absorption test, which was performed in one patient after bariatric surgery, revealed adequate drug absorption.17 Given the bariatric surgery-induced weight loss, the hydrocortisone need is expected to be reduced. Therefore, using the same hydrocortisone dose after compared with before bariatric surgery may induce steroid-related side effects like weight gain, unless the bioavailability of hydrocortisone is reduced.26 However, this has not been systematically studied.
At 1 year of follow-up after bariatric surgery, there were no significant differences in the use of antidiabetic, antihypertensive and antihyperlipidemic agents between patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity. In patients with craniopharyngioma, the presence of treatment for diabetes mellitus and hypertension declined at 1 year of follow-up after bariatric surgery compared with baseline, whereas the use of hypolipidemic medication remained equal. In the aforementioned study by Bretault et al., 31.6% of patients with craniopharyngioma-related hypothalamic obesity were diabetic at bariatric procedure. This declined to 8.3% at 1 year of follow-up. One patient required antihypertensive medication before bariatric surgery. No data on antihyperlipidemic drugs were available.19
Our study has some limitations. As craniopharyngioma is a rare disease, and only a minority of patients with craniopharyngioma is likely to have undergone bariatric surgery, it is hard to obtain a large sample size, even with international collaboration. In an attempt to overcome this issue, we performed a meta-analysis to validate our results on bariatric surgery-induced weight loss in patients with craniopharyngioma-related hypothalamic obesity. However, due to the relatively small number of patients, results of statistical analyses have to be interpreted cautiously. In addition, we were unable to report perioperative and postoperative complications of bariatric surgery in all patients with craniopharyngioma. Only data from the Swedish patients were available on this subject, in whom only one patient suffered from postoperative abdominal pain during the first six weeks after sleeve gastrectomy. In the study by Weismann et al., the occurrence of postoperative problems after bariatric surgery (that is, abdominal pain, vomiting and reflux) was similar in patients with craniopharyngioma-related hypothalamic obesity and control subjects with ‘common’ obesity.21
In conclusion, our observations suggest that bariatric surgery, in particular with Roux-en-Y gastric bypass, might be an effective therapeutic option for craniopharyngioma-related hypothalamic obesity without significant side effects on hormone replacement therapy for pituitary insufficiency. However, careful drug monitoring is still advised, especially for levothyroxine and hydrocortisone. Larger, international, well-designed studies are needed to receive more efficacy and safety data regarding the therapeutic potential of bariatric surgery for craniopharyngioma-related hypothalamic obesity. Such studies should have an adequate follow-up duration and should compare weight loss between patients and matched control subjects.
References
Muller HL . Craniopharyngioma. Endocr Rev 2014; 35: 513–543.
Olsson DS, Andersson E, Bryngelsson IL, Nilsson AG, Johannsson G . Excess mortality and morbidity in patients with craniopharyngioma, especially in patients with childhood onset: a population-based study in Sweden. J Clin Endocrinol Metab 2015; 100: 467–474.
Muller HL, Faldum A, Etavard-Gorris N, Gebhardt U, Oeverink R, Kolb R et al. Functional capacity, obesity and hypothalamic involvement: cross-sectional study on 212 patients with childhood craniopharyngioma. Klinische Padiatrie 2003; 215: 310–314.
Muller HL, Gebhardt U, Etavard-Gorris N, Korenke E, Warmuth-Metz M, Kolb R et al. Prognosis and sequela in patients with childhood craniopharyngioma—results of HIT-ENDO and update on KRANIOPHARYNGEOM 2000. Klinische Padiatrie 2004; 216: 343–348.
Roth CL . Hypothalamic obesity in craniopharyngioma patients: disturbed energy homeostasis related to extent of hypothalamic damage and its implication for obesity intervention. J Clin Med 2015; 4: 1774–1797.
Haslam DW, James WP . Obesity. Lancet 2005; 366: 1197–1209.
Muller HL, Bueb K, Bartels U, Roth C, Harz K, Graf N et al. Obesity after childhood craniopharyngioma—German multicenter study on pre-operative risk factors and quality of life. Klinische Padiatrie 2001; 213: 244–249.
Muller HL . Craniopharyngioma and hypothalamic injury: latest insights into consequent eating disorders and obesity. Curr Opin Endocrinol Diabetes Obes 2016; 23: 81–89.
Roemmler-Zehrer J, Geigenberger V, Stormann S, Ising M, Pfister H, Sievers C et al. Specific behaviour, mood and personality traits may contribute to obesity in patients with craniopharyngioma. Clin Endocrinol 2015; 82: 106–114.
Muller HL, Emser A, Faldum A, Bruhnken G, Etavard-Gorris N, Gebhardt U et al. Longitudinal study on growth and body mass index before and after diagnosis of childhood craniopharyngioma. J Clin Endocrinol Metab 2004; 89: 3298–3305.
Roth CL, Eslamy H, Werny D, Elfers C, Shaffer ML, Pihoker C et al. Semiquantitative analysis of hypothalamic damage on MRI predicts risk for hypothalamic obesity. Obesity 2015; 23: 1226–1233.
Rakhshani N, Jeffery AS, Schulte F, Barrera M, Atenafu EG, Hamilton JK . Evaluation of a comprehensive care clinic model for children with brain tumor and risk for hypothalamic obesity. Obesity 2010; 18: 1768–1774.
Sjostrom L . Review of the key results from the Swedish Obese Subjects (SOS) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med 2013; 273: 219–234.
Inge TH, Pfluger P, Zeller M, Rose SR, Burget L, Sundararajan S et al. Gastric bypass surgery for treatment of hypothalamic obesity after craniopharyngioma therapy. Nat Clin Pract 2007; 3: 606–609.
Padwal R, Brocks D, Sharma AM . A systematic review of drug absorption following bariatric surgery and its theoretical implications. Obes Rev 2010; 11: 41–50.
Knibbe CA, Brill MJ, van Rongen A, Diepstraten J, van der Graaf PH, Danhof M . Drug disposition in obesity: toward evidence-based dosing. Ann Rev Pharmacol Toxicol 2015; 55: 149–167.
Wolf P, Winhofer Y, Smajis S, Kruschitz R, Schindler K, Gessl A et al. Hormone substitution after gastric bypass surgery in patients with hypopituitarism secondary to craniopharyngioma. Endocr Pract 2016; 22: 595–601.
Hedenbro JL, Naslund E, Boman L, Lundegardh G, Bylund A, Ekelund M et al. Formation of the Scandinavian Obesity Surgery Registry, SOReg. Obesity Surgery 2015; 25: 1893–1900.
Bretault M, Boillot A, Muzard L, Poitou C, Oppert JM, Barsamian C et al. Clinical review: bariatric surgery following treatment for craniopharyngioma: a systematic review and individual-level data meta-analysis. J Clin Endocrinol Metab 2013; 98: 2239–2246.
Higgins JP, Thompson SG, Deeks JJ, Altman DG . Measuring inconsistency in meta-analyses. Brit Med J 2003; 327: 557–560.
Weismann D, Pelka T, Bender G, Jurowich C, Fassnacht M, Thalheimer A et al. Bariatric surgery for morbid obesity in craniopharyngioma. Clin Endocrinol 2013; 78: 385–390.
Madsbad S, Dirksen C, Holst JJ . Mechanisms of changes in glucose metabolism and bodyweight after bariatric surgery. Lancet 2014; 2: 152–164.
Coomans CP, van den Berg SA, Lucassen EA, Houben T, Pronk AC, van der Spek RD et al. The suprachiasmatic nucleus controls circadian energy metabolism and hepatic insulin sensitivity. Diabetes 2013; 62: 1102–1108.
Rao RS . Bariatric surgery and the central nervous system. Obesity Surgery 2012; 22: 967–978.
Fierabracci P, Martinelli S, Tamberi A, Piaggi P, Basolo A, Pelosini C et al. Weight loss and variation of levothyroxine requirements in hypothyroid obese patients after bariatric surgery. Thyroid 2016; 26: 499–503.
Mah PM, Jenkins RC, Rostami-Hodjegan A, Newell-Price J, Doane A, Ibbotson V et al. Weight-related dosing, timing and monitoring hydrocortisone replacement therapy in patients with adrenal insufficiency. Clin Endocrinol 2004; 61: 367–375.
Acknowledgements
We would like to thank the bariatric surgical teams of the Maasstad Ziekenhuis and Sint Franciscus Gasthuis (Rotterdam, the Netherlands), as well as the bariatric surgical teams of the Carlanderska Sjukhuset and Sahlgrenska University Hospital (Gothenburg, Sweden).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wijnen, M., Olsson, D., van den Heuvel-Eibrink, M. et al. Efficacy and safety of bariatric surgery for craniopharyngioma-related hypothalamic obesity: a matched case–control study with 2 years of follow-up. Int J Obes 41, 210–216 (2017). https://doi.org/10.1038/ijo.2016.195
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.195
- Springer Nature Limited
This article is cited by
-
Update on management of craniopharyngiomas
Journal of Neuro-Oncology (2022)
-
Five-Year Changes in Weight and Diabetes Status After Bariatric Surgery for Craniopharyngioma-Related Hypothalamic Obesity: a Case–Control Study
Obesity Surgery (2022)
-
Obesità post-neurochirurgia ipotalamica
L'Endocrinologo (2021)
-
Bariatric Surgery for Treatment of Hypothalamic Obesity After Craniopharyngioma Therapy: a Matched Case–Control Study
Obesity Surgery (2020)
-
Craniopharyngioma
Nature Reviews Disease Primers (2019)