Abstract
Background:
In healthy subjects increasing body mass index (BMI) leads to greater mortality from a range of causes. Following onset of specific diseases, however, the reverse is often found: called the ‘obesity paradox’. But we recently observed the phenomenon called the ‘paradox within the paradox’ for stroke patients.
Objective:
The objective of our study was to examine the effect of each unit increase in BMI on renal cancer-specific survival (CSS), cancer-specific mortality, overall survival (OS) and overall mortality.
Design:
Random-effects generalized least squares models for trend estimation were used to analyze the data. Eight studies, comprising of 8699 survivals of 10 512 renal cell carcinoma (RCC) patients met the inclusion criteria, including 5 on CSS and 3 on OS.
Results:
The association of BMI with CSS and OS was non-linear (P<0.0001, P=0.004, respectively). We observed that CSS increased in relation to BMI, indicating that there was the obesity paradox in RCC. However, each unit increase in BMI over 25 was associated with decreased OS, indicating that RCC may also exhibit a paradox within the paradox.
Conclusions:
Inconsistent effects of increases in BMI on CSS and OS, as previously observed for stroke, creates a paradox (different directions of mortality for different causes) within the obesity paradox.
Similar content being viewed by others
Introduction
Obesity, defined as a body mass index (BMI) over the threshold of 30, has been identified to be associated with increased overall mortality (OM).1, 2, 3 However, following the onset of several chronic conditions the reverse has been observed,4, 5, 6 known as the ‘obesity paradox’ or ‘reverse epidemiology’.7 Particularly, it was suggested that in specific disease conditions obesity could be protective, and has been observed to be linked to higher survival in patients with kidney disease,4, 7, 8, 9, 10 coronary heart disease,11 chronic heart failure,12, 13 cardiovascular disease,14, 15 fracture16 and stroke.17, 18, 19
Although a higher BMI was observed to be a significant risk factor for the development of several diseases, following development of a disease it could serve as a protection against its complications. Such a situation has been potentially attributed to a short-term beneficial effect of obesity.20 It has been suggested that earlier diagnosis of the disease in obese patients due to earlier testing might account for the apparent higher survival among obese subjects.11 Following diagnosis with some co-morbid conditions, obese patients might change their unhealthy lifestyle contributing to a reduction in the obesity complications, which subsequently resulted in their better survival rates.17 In addition, greater sources of energy or metabolites were also suggested as the potential mechanism for the paradoxical increase in survival of obese patients:17, 18, 21, 22 the idea that fat acts as a metabolic buffer. Some reports also referred to higher skeletal muscle in patients with higher BMI as a protective factor.10, 20 Assuming these suggestions to be true, one would expect that the obesity paradox would still exist with respect to overall survival (OS) rather than exclusively to disease-specific survival. However, we recently showed using a meta-analysis, with respect to stoke mortality that patients who had undergone and survived a stroke showed a conventional ‘obesity paradox’ with respect to future risk of mortality from stroke.23 Yet when mortality from non-stroke causes was considered the reverse ‘conventional’ pattern of association to BMI was found: which we termed a ‘paradox within the paradox’.23 In fact, higher BMI was associated with lower stroke-specific but higher all-cause mortality, depicting two different patterns. These findings raise the question as to whether this is something specific to stroke or whether other causes of mortality show similar patterns when disease-specific and all-cause death are assessed.
Given the epidemic of overweight and obesity worldwide, a better understanding of this contrast, which has been systematically addressed for stroke,23 would merit further investigation. Thus, in the current paper we investigated the association between obesity and survival in patients diagnosed with renal cell carcinoma (RCC). Eligible studies on both survival and mortality among the survivors from RCC were assessed, and a dose–response meta-analysis was performed to examine the association of BMI with renal cancer-specific survival (CSS), OS, cancer-specific mortality (CSM) and OM and the likelihood of non-linear trends in these potential relationships.
Materials and methods
Search strategy and data extraction
We searched for papers written in English on the association of BMI with mortality from RCC in Pubmed, Scopus and Ovid databases upto 3 March 2015. Reference lists of related publications were hand-searched to identify additional studies not extracted in the database searches. The study keywords were as follows: ‘Body Composition’ OR ‘Body Size’ OR ‘fat mass’ OR ‘body fat’ OR ‘Body Mass Index’ OR ‘BMI’ OR ‘Adiposity’ OR ‘Body Weight’ OR ‘Obesity’ OR ‘Overweight’ AND ‘mortality’ OR ‘prognosis’ OR ‘death’ OR ‘survival’ OR ‘paradox’ OR ‘reverse epidemiology’ AND ‘renal cell carcinoma’ OR ‘renal cell cancer’ OR ‘RCC’ OR ‘kidney cancer’ AND ‘follow-up’ OR ‘longitudinal studies’ OR ‘cohort’ OR ‘retrospective studies’ OR ‘observational studies’ OR ‘prospective studies’. According to our full-text screening form that we designed for the current meta-analysis and PRISMA 2009 flow diagram, studies were included if they had a prospective design and included a study population aged >15 years and assessed BMI as exposure of interest and cause-specific survival/mortality or OS/OM of patients with RCC as outcome of interest. Studies were also required to have reported multivariable hazard ratios (HRs) or relative risks along with matched 95% confidence intervals (CIs) and reported number of patients suffering from RCC and number of death separately in all BMI classes. The excluded studies were among those with <3 BMI categories or they were commentaries or conference proceedings. We contacted authors in case additional data were required in 8 studies. The authors of 2 studies responded; one could not provide multivariable data as a backwards stepwise analysis was used and BMI was removed due to insignificance24 and the other one promised to calculate the information we requested but unfortunately their statistician did not do the analysis.25 The quality of studies was assessed based on the components of the Newcastle–Ottawa Scale (NOS) including selection, comparability and outcome. Information on the following variables was gathered from each study: author’s names, year of publication, location of study (country), mean age, sex of the study participants, follow-up duration, number of cases and deaths per BMI category, multivariable HRs/relative risks and CIs of cancer-specific or OS/OM per BMI category and confounding variables controlled for in multivariable analysis. Data were extracted independently by two reviewers. If consensus was not reached in data extraction, a third reviewer resolved and overcame disagreements.
Statistical analysis
GLST (Generalized least squares for trend estimation) was used to examine HRs of survival/mortality for every unit increase in BMI.26 For studies in which the lowest BMI category was not the referent, estimations of HR and CI as relative to the lowest category were calculated by suitable contrasts.27 When the BMI mean or median, considered as the dose in the dose–response meta-analysis,26, 28 was not reported, the midpoint of the boundaries in each BMI category was determined. The amplitude of open-ended categories was considered to be the same as that of the neighboring ones. If results were reported by sex, fixed-effects models were performed to calculate pooled values of HRs and CIs. The dose–response meta-analysis was administered using HRs and CIs of survival/mortality, the number of survivals/deaths and the number of cases across BMI categories reported in studies. Separate meta-analyses were performed on survival and mortality.
To assess non-linear dose–response relationships between survival/mortality and BMI, we used a two-stage hierarchical regression model in which the difference between category-specific and reference-specific doses, expressed in quadratic terms, was calculated. Spline transformations considering within- and between-study variances were used to model dose–response relationships.
To identify statistical heterogeneity between studies, we used Q-statistics. In this study, the existence of potential sources of heterogeneity was confirmed by goodness-of-fit P-values<0.05. To investigate causes of heterogeneity, subgroup analyses by mean or median duration of follow-up and the quality of studies were performed. As for the sensitivity analysis, we used a jack-knife approach, sequentially removing single studies and analyzing the remaining studies to examine the influence of each study on the overall estimates. Potential existence of publication biases were assessed using the Egger’s test.
Two-sided P<0.05 was considered statistically significant. All statistical analyses were carried out using Stata v12 software (StataCorp, College Station, TX, USA).
Results
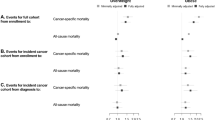
As shown in Figure 1, a total of 455 articles were identified including 437 through databases searching and 18 through other sources. After removal of duplicates (n=280), the abstracts of 178 studies were assessed to identify the records which should be given more detailed evaluation. Following further review of 58 full-text articles, 26 were excluded leaving 30 studies, of which 22 were not qualified to be included for a dose–response meta-analysis. As a result 8 studies consisting of 5 on CSS6, 29, 30, 31, 32 and 3 on OS6, 30, 33 were included for this quantitative meta-analysis. There were 4 studies on CSM34, 35, 36, 37 and 1 on OM34 (Figure 1).
Study characteristics
All studies that reported survival provided findings on either CSS or OS, except for two publications which assessed the association of BMI with both CSS and OS.6, 30 In this category three reports were from Korea,6, 30, 32 two from Germany29, 31 and one from USA.33 Regarding CSS, mean study duration of the reports ranged from 3.6 to 6.4 years. The sample size in this sub-meta-analysis was 6815 renal cancer patients, 5581 of which survived. For those studies with reported mean age across categories of BMI,29, 30, 31, 32 the mean age ranged between 54 and 62.6. Using the NOS three studies6, 31, 32 were identified to be of high and the other two were considered as moderate quality. In the studies assessing OS, however, the cancer patients were followed for a mean follow-up period of 2.75–6.4 years. The total number of patients examined was 3697, of which 579 subjects died and the rest survived. The mean age in different BMI categories reported in two studies31, 32 varied from 55.2 to 63 years. According to the components of the NOS, the publications by Choi et al.6 Jeon et al.30 and Donat et al.33 were classified as of high, moderate and low quality, respectively.
Of four studies included in our mortality analysis,34, 35, 36, 37 one recorded findings on both cancer-specific and all-cause death34 and the remaining studies provided results exclusively for RCC. Of these studies, one was conducted in Korea,34 two in USA35, 37 and one in UK.36 Mean years of follow-up in the records demonstrating data on RCC-specific mortality varied between 2 to 7 years. A total of 945 of 4848 sufferers from RCC, who were included and followed up, eventually died specifically of RCC. Of the mortality-related studies, two have provided patients’ mean age which ranged from 51.4 to 56.7 years across varied BMI categories. All of these three studies were categorized as of moderate quality with respect to the NOS.
In studies included in this meta-analysis, survival/mortality figures were reported across different BMI classifications. There were three studies29, 33, 37 in which BMI were categorized according to World Health Organization classification system. Therefore, to eliminate this detected heterogeneity in exposure among the included studies, dose–response models were fitted using the GLST method.
Cancer-specific survival
The random effect dose–response model demonstrated a non-linear trend between BMI and CSS (P<0.0001), suggesting between-study standard deviations of 0.028 and 0.034, respectively, and correlation matrix of 1. In this relationship it was found that with every increase in BMI value the risk of dying in RCC patients decreased (Figure 2). When a two-stage random-effects model was administered to compare the observed relationship with a linear trend, it was revealed that each 5-unit increase in BMI was associated with a 28% lower risk of mortality in patients suffering from RCC (HR: 0.72, 95% CI: 0.56–0.91, P=0.007). Also, the small goodness-of-fit P-value (Q=14.75, P=0.005) suggested that potential sources of heterogeneity should be taken into account. When subgroup analyses by mean/median years of follow-up and the scores gained in the NOS assessments were conducted, the shape of the dose–response relationship did not vary across the included studies, and the goodness-of-fit test revealed that the heterogeneity problem still had to be dealt with. Subsequently, as for sensitivity analyses, sequentially leaving out each study at a time and performing random effect dose–response analyses on the remaining studies did not substantially change the findings. Our overall conclusion was that no reason at all to exclude the influential study by Sung et al.32 on this topic as it was the only report to assess the largest number of patients with low BMI values.
Overall survival
When records exploring the association of BMI with OS were included in a single meta-analysis, a non-linear dose–response relationship between these two variables was observed (P=0.004), yielding the estimated between-studies s.ds of 0.025 and 0.044, respectively, and the correlation matrix of 1. The BMI–OS relationship showed a U-shaped curve with a nadir around BMI value of 25 kg m−2, indicating that with a unit increase in BMI, the risk of OM decreased with BMI<25 kg m−2, whereas it increased with greater values (Figure 3). Comparing the finding with a linear trend by applying a two-stage random-effect model, we observed that for each 5-unit increase in BMI, the risk of OM decreased by 29% (HR: 0.71, 95% CI: 0.50–1.03, P=0.068). The goodness-of-fit test (Q=9.19, P=0.01) detected significant heterogeneity among these studies. Subgroup analyses could not be conducted due to small number of the studies included in the OS-related meta-analysis. Also, sensitivity analyses could not be performed since spline transformations could not be created when the sample size was small.
The non-linear association between BMI and CSM is not statistically significant and therefore no estimation could be performed on this variable and we focused instead on those quantifying survival.
Discussion
The findings from the meta-analyses performed on studies assessing the association of BMI with CSS suggested that CSS was higher among overweight and obese sufferers from RCC compared with those with lower BMI values. On the other hand, the relationship between BMI and OS showed that normal-weight RCC patients had better OS compared with those who were underweight, overweight and obese. To date the only related meta-analysis by Choi et al.6 explored the association of obesity but not BMI with CSS and OS, in a method which included highest versus lowest comparison rather than the dose–response approach, and showed an increase in both CSS and OS in patients with higher BMI values. However, our meta-analysis, using the latter method, for the first time suggested how survival/mortality curves were changed with one unit increase in BMI among RCC patients and at the same time would make it possible to predict survival when the included studies did not have the same BMI classification system.
Findings on BMI–CSS indicated BMI as a prognostic variable for RCC patients’ survival. The concept of 'obesity paradox’ was strongly supported by the present data concerning the association of BMI with CSS, however, at the same time the hypothesis ‘paradox within a paradox’ might originate as an inverse association was found on BMI–OS. In agreement with our latter observation, OM was directly associated with BMI.3, 38 On the other hand, several studies reported that deaths from a specific disease were higher in individuals with BMI>25 kg m−2, compared with normal-weight patients.6, 39, 40
Increases in BMI values would be expected to influence CSS and OS in the same way, however, results from the present study, in harmony with our published findings on the association of BMI with OM and stroke-specific mortality in stroke patients,23 indicated that in RCC patients, the disease-specific survival increased, whereas OS decreased in relation to BMI. Thus, the ‘paradox within a paradox’ was also found in RCC patients is not specific to stroke.
A potential explanation for the obesity paradox effect was that by being regularly checked-up for any potential disorders, overweight and obese patients were more likely to be treated in early stage of their disease, the phenomenon called ‘Hawthorne effect’.41 As we previously suggested, improved disease-specific survival as observed in RCC patients with higher BMI values was probably not due to the ‘Hawthorne effect’, otherwise the same result would be obtained for OS in these patients and the rate of increase in survival did not differ with respect to BMI among them.23 An alternative hypothesis is that higher energy reservoirs in adipose tissue stores might mediate better prognosis linked to higher BMI categories.21, 22 Although Morgan et al.42 reported that both CSS and OS were lower in RCC patients with nutritional deficiency, they used other parameters including albumin and weight loss along with BMI to define nutritional deficiency. Hence, as a paradox was observed in the findings on CSS and OS in our study, improved nutritional status in those who are overweight and obese was not to be considered as a potential explanation for living longer than normal-weight patients. Moreover, another mechanism proposed to describe the obesity paradox might be through age-related mediating explanations including better survival in metabolically healthy obese elderly patients,21, 22 decreased insulin resistance and type 2 diabetes due to the age-related increase in subcutaneous fat mass and decline in abdominal fat21 and the ‘reverse causation’ which refers to age-linked disorders causing malnutrition and underweight and subsequently leading to worse prognosis.22, 43 Similarly, these mechanisms might lose their ability to generate the observed relationship between BMI and CSS when the inverse finding was obtained on BMI–OS and particularly when the mean age of participants in both sub-meta-analyses did not significantly differ.
The strengths of our meta-analysis study were that we conducted three sub-meta-analyses simultaneously; on BMI–CSS, BMI–OS and BMI–CSM, using a dose–response relationship approach and thus demonstrating the feasibility of predicting the influence of each unit increase in BMI on survival/mortality, including various studies with different BMI classification systems by means of GLST rather than performing a highest versus the lowest comparison, and performing subgroup and sensitivity analysis. Furthermore, not only separate analyses were presented on CSS and OS, we conducted a single meta-analysis on CSM.
In contrast there were also several limitations. The first limitation regards the existence of potential confounders in the original studies which could bias the estimates we made. However, we tried to reduce the effect of confounders by not including publications which reported unadjusted figures. Another concern is that, based on existing literatures and our findings, we were not able to justify the paradox observed in the findings of CSS-related and OS-related meta-analyses. Therefore, the rational of the yield contrary remains to be investigated.
In conclusion, non-linear relationships were found for BMI–CSS and BMI–OS. The findings from these trends showed that increased in BMI values had a different effect on CSS and OS, indicating higher probability of disease-specific survival and lower probability of OS in RCC patients. Trends of CSM with BMI were not significant. The mechanisms explaining the opposite effect of BMI on CSS and OS is unclear and therefore further research investigating the related pathways, which support the concept of a paradox within a paradox, is needed. Although the mechanisms underpinning the association of higher BMI and better disease-specific survival are unclear, a better understanding of the effect of other factors in addition to BMI such as cardiorespiratory fitness on improved survival in obese patient is needed13 when lower OS was observed to be associated with higher BMI. The demonstrated presence of a paradox within the obesity paradox, indicates that obesity should not be regarded as uniformly advantageous following disease diagnosis. Therefore patients might be best advised to follow a healthy diet and physical activity plan to maximize survival following disease diagnosis.
References
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med 2010; 363: 2211–2219.
Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009; 373: 1083–1096.
Flegal KM, Kit BK, Orpana H, Graubard BI . Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 2013; 309: 71–82.
Kalantar-Zadeh K, Abbott KC, Salahudeen AK, Kilpatrick RD, Horwich TB . Survival advantages of obesity in dialysis patients. Am J Clin Nutr 2005; 81: 543–554.
Oreopoulos A, Padwal R, Kalantar-Zadeh K, Fonarow GC, Norris CM, McAlister FA . Body mass index and mortality in heart failure: a meta-analysis. Am Heart J 2008; 156: 13–22.
Choi Y, Park B, Jeong BC, Seo SI, Jeon SS, Choi HY et al. Body mass index and survival in patients with renal cell carcinoma: a clinical based cohort and meta analysis. Int J Cancer 2013; 132: 625–634.
Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD . Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int 2003; 63: 793–808.
Johansen KL, Young B, Kaysen GA, Chertow GM . Association of body size with outcomes among patients beginning dialysis. Am J Clin Nutr 2004; 80: 324–332.
Abbott KC . Reverse epidemiology and obesity in maintenance dialysis patients. Kidney Int 2003; 64: 1138–1138.
Park J, Ahmadi SF, Streja E, Molnar MZ, Flegal KM, Gillen D et al. Obesity paradox in end-stage kidney disease patients. Prog Cardiovasc Dis 2014; 56: 415–425.
De Schutter A, Lavie CJ, Milani RV . The impact of obesity on risk factors and prevalence and prognosis of coronary heart disease-the obesity paradox. Prog Cardiovasc Dis 2014; 56: 401–408.
Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC . Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol 2004; 43: 1439–1444.
Clark AL, Fonarow GC, Horwich TB . Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis 2014; 56: 409–414.
Uretsky S, Messerli FH, Bangalore S, Champion A, Cooper-Dehoff RM, Zhou Q et al. Obesity paradox in patients with hypertension and coronary artery disease. Am J Med 2007; 120: 863–870.
Jahangir E, De Schutter A, Lavie CJ . Low weight and overweightness in older adults: risk and clinical management. Prog Cardiovasc Dis 2014; 57: 127–133.
Prieto-Alhambra D, Premaor MO, Avilés FF, Castro AS, Javaid MK, Nogués X et al. Relationship between mortality and BMI after fracture: a population based study of men and women aged ≥40 years. J Bone Miner Res 2014; 29: 1737–1744.
Andersen KK, Olsen TS . The obesity paradox in stroke: lower mortality and lower risk of readmission for recurrent stroke in obese stroke patients. Int J Stroke 2015; 10: 99–104.
Kim BJ, Lee S-H, Ryu W-S, Kim CK, Lee J, Yoon B-W . Paradoxical longevity in obese patients with intracerebral hemorrhage. Neurology 2011; 76: 567–573.
Vemmos K, Ntaios G, Spengos K, Savvari P, Vemmou A, Pappa T et al. Association between obesity and mortality after acute first-ever stroke the obesity–stroke paradox. Stroke 2011; 42: 30–36.
Kalantar-Zadeh K, Rhee CM, Amin AN . To legitimize the contentious obesity paradox. Mayo Clinic Proc 2014; 89: 1033–1035.
Hainer V, Aldhoon-Hainerová I . Obesity paradox does exist. Diabetes Care 2013; 36 (Supplement 2): S276–S281.
Oreopoulos A, Kalantar-Zadeh K, Sharma AM, Fonarow GC . The obesity paradox in the elderly: potential mechanisms and clinical implications. Clin Geriatr Med 2009; 25: 643–659.
Bagheri M, Speakman JR, Shabbidar S, Kazemi F, Djafarian K . A dose-response meta-analysis of the impact of body mass index on stroke and all cause mortality in stroke patients: a paradox within a paradox. Obes Rev 2015; 16: 416–423.
Brookman-May S, Kendel F, Hoschke B, Wieland WF, Burger M, Rößler W et al. Impact of body mass index and weight loss on cancer-specific and overall survival in patients with surgically resected renal cell carcinoma. Scand J Urol Nephrol 2011; 45: 5–14.
Sunela KL, Kataja MJ, Kellokumpu-Lehtinen PI . Influence of body mass index and smoking on the long-term survival of patients with renal cell cancer. Clin Genitourin Cancer 2013; 11: 458–464.
Orsini N, Bellocco R, Greenland S . Generalized least squares for trend estimation of summarized dose-response data. Stata J 2006; 6: 40.
Hamling J, Lee P, Weitkunat R, Ambühl M . Facilitating meta analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med 2008; 27: 954–970.
Greenland S, Longnecker MP . Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 1992; 135: 1301–1309.
Haferkamp A, Pritsch M, Bedke J, Wagener N, Pfitzenmaier J, Buse S et al. The influence of body mass index on the long-term survival of patients with renal cell carcinoma after tumour nephrectomy. BJU Int 2008; 101: 1243–1246.
Jeon HG, Jeong IG, Lee JH, Lee CJ, Kwak C, Kim HH et al. Prognostic value of body mass index in Korean patients with renal cell carcinoma. J Urol 2010; 183: 448–454.
Steffens S, Ringe KI, Schroeer K, Lehmann R, Rustemeier J, Wegener G et al. Does overweight influence the prognosis of renal cell carcinoma? Results of a multicenter study. Int J Urol 2013; 20: 585–592.
Sung HH, Jeon SS, Park SY, Jeong BC, Seo SI, Lee HM et al. Impact of body mass index in Korean patients with renal cell carcinoma. Cancer Causes Control 2012; 23: 505–511.
Donat SM, Salzhauer EW, Mitra N, Yanke BV, Snyder ME, Russo P . Impact of body mass index on survival of patients with surgically treated renal cell carcinoma. J Urol 2006; 175: 46–52.
Park B, Jeong BC, Seo SI, Jeon SS, Choi HY, Lee HM . Influence of body mass index, smoking, and blood pressure on survival of patients with surgically-treated, low stage renal cell carcinoma: a 14-year retrospective cohort study. J Korean Med Sci 2013; 28: 227–236.
Parker AS, Lohse CM, Cheville JC, Thiel DD, Leibovich BC, Blute ML . Greater body mass index is associated with better pathologic features and improved outcome among patients treated surgically for clear cell renal cell carcinoma. Urology 2006; 68: 741–746.
Reeves GK, Pirie K, Beral V, Green J, Spencer E, Bull D et al. Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ 2007; 335: 1134.
Hakimi AA, Furberg H, Zabor EC, Jacobsen A, Schultz N, Ciriello G et al. An epidemiologic and genomic investigation into the obesity paradox in renal cell carcinoma. J Natl Cancer Inst 2013; 105: 1862–1870.
McGee, Daniel L . Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol 2005; 15: 87–97.
Padwal R, McAlister FA, McMurray JJ, Cowie MR, Rich M, Pocock S et al. The obesity paradox in heart failure patients with preserved versus reduced ejection fraction: a meta-analysis of individual patient data. Int J Obes 2013; 38: 1110–1114.
Sharma A, Vallakati A, Einstein AJ, Lavie CJ, Arbab-Zadeh A, Lopez-Jimenez F et al. Relationship of body mass index with total mortality, cardiovascular mortality and myocardial infarction after coronary revascularization: evidence from a meta-analysis. J Am Coll Cardiol 2014; 63: 1080–1100.
Tajer CD, . RAC director’s letter. The obesity paradox. intention of making a reasonable suggestion for secondary prevention. Revista Argentina de Cardiologia 2012; 80: 195–204.
Morgan TM, Tang D, Stratton KL, Barocas DA, Anderson CB, Gregg JR et al. Preoperative nutritional status is an important predictor of survival in patients undergoing surgery for renal cell carcinoma. Eur Urol 2011; 59: 923–928.
Löser C, Lübbers H, Mahlke R, Lankisch PG . cme: involuntary weight loss in elderly people. Dtsch Arztebl 2007; 104: 3411–3420.
Acknowledgements
The study was supported by Tehran University of Medical Sciences. We gratefully thank Dr Peter Lee for providing us with technical assistance.
Author contributions
MB designed research, analyzed data, wrote paper and had primary responsibility for final content. JRS has developed overall research plan, wrote paper and had responsibility for critical revision. FS had hands-on data collection. KD was responsible for interpretation of data, drafting of manuscript and critical revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bagheri, M., Speakman, J., Shemirani, F. et al. Renal cell carcinoma survival and body mass index: a dose–response meta-analysis reveals another potential paradox within a paradox. Int J Obes 40, 1817–1822 (2016). https://doi.org/10.1038/ijo.2016.171
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.171
- Springer Nature Limited
This article is cited by
-
The m6A modification-mediated OGDHL exerts a tumor suppressor role in ccRCC by downregulating FASN to inhibit lipid synthesis and ERK signaling
Cell Death & Disease (2023)
-
A hint for the obesity paradox and the link between obesity, perirenal adipose tissue and Renal Cell Carcinoma progression
Scientific Reports (2022)
-
Associating the risk of three urinary cancers with obesity and overweight: an overview with evidence mapping of systematic reviews
Systematic Reviews (2021)
-
Body mass index as an independent risk factor for inferior vena cava resection during thrombectomy for venous tumor thrombus of renal cell carcinoma
World Journal of Surgical Oncology (2019)
-
Increasing the rigor of obesity research publications
International Journal of Obesity (2017)