Abstract
Background/Objectives:
Clinical heterogeneity exists in overall obesity and obesity in terms of susceptibility to type 2 diabetes, but the relationship is vulnerable to be confounded by traditional risk factors in epidemiological studies. We aimed to characterize the impact of obesity in insulin secretion and sensitivity by using Mendelian randomization (MR) approach with genetic variants.
Subjects/Methods:
We first constructed two genetic risk scores based on 38 established loci for body mass index (BMI; a surrogate of overall obesity) and 13 waist-to-hip ratio (WHR; a surrogate of central obesity) to assess the causal effects of BMI and WHR on several glycaemic-related traits in 2884 community-based Han Chinese individuals.
Results:
Both of BMI and WHR were observationally correlated with insulin secretion and sensitivity indices. The MR analysis demonstrated that a genetically determined 1 s.d. (3.35 kg m−2) higher BMI caused a unit of 178.18 pmol l−1 higher Stumvoll first-phase and 35.52 pmol l−1 higher Stumvoll second-phase insulin secretion (P=0.001 and 0.002, respectively), which were even independent of central obesity (P=0.019 and 0.039, respectively). In contrast, a genetically determined 1 s.d. higher WHR (a change of 0.002 in WHR) caused a unit of 1.21 higher homeostasis model assessment of insulin resistance and 18.40 lower Gutt index (representing the insulin sensitivity) (P=0.048 and 0.028, respectively). No substantial heterogeneity existed between the observed associations and the genetic estimated associations (P for difference >0.05).
Conclusions:
We provide new causal evidence that the impact of obesity on insulin secretion and sensitivity could vary between overall obesity and central obesity in Han Chinese populations and also identify the extent to which overall obesity affects compensatory insulin secretion and central obesity inversely links to insulin sensitivity.
Similar content being viewed by others
Introduction
Obesity is considered a major risk factor for type 2 diabetes (T2D) and the current T2D epidemic has been ascribed to a substantial increase in the incidence of obesity.1, 2 Clinical heterogeneity exists in different types of obesity leading to T2D. Some individuals with central obesity are at higher risk for the onset of diabetes than those with overall obesity.3, 4 Regarding the differences in structure and function of these two types of adiposity, it is important to discover the mechanisms underlying the development and progression of T2D in people with different types of obesity to get insight into this problem.
The declines in insulin secretion and insulin sensitivity are two major determinants in the pathogenesis of T2D. Even though it has ubiquitously been recognized that both of overall obesity and central obesity increased the T2D risk, the causal link between obesity and the pathogenesis of T2D, including insulin secretion or insulin sensitivity, remains completely understood. Previous investigations found an inverse relation of overall obesity and central obesity (that is, ectopic fat depots in liver, muscle or heart) with insulin sensitivity in the conventional epidemiological studies,3 whereas the evidence for impacts on β-cell function is not established. The mixed results may be due to study design, selection bias and other confounding factors. Novel insight into the impacts of overall obesity and central obesity on insulin secretion and sensitivity can be obtained with Mendelian randomization (MR). This is an instrumental variable approach to test for a causal link between T2D risk or related traits and a genetically influenced phenotype of obesity (that is, body mass index (BMI), waist circumference (WC) and waist-to-hip ratio (WHR)), protecting genotype–phenotype associations from the presence of potential confounding and reverse causation. So far, a number of studies have rapidly been evolving to examine the causal role of obesity as a risk factor in cardiovascular diseases,5, 6 some kinds of cancer7 and other diseases.8
Thus we conducted this population-based study in 2884 Han Chinese subjects to investigate the causal role of BMI and WHR in glycaemic-related traits and to test whether the contribution to insulin sensitivity and secretion are different between overall and central obesity susceptibility.
Materials and methods
Subjects
A total of 2960 subjects were enrolled from a community-based Han Chinese population. All subjects were given written informed consent. Subjects with cancer, severe disability or severe psychiatric disturbances were excluded. The remaining 2884 subjects completed a standard medical questionnaire, anthropometric measurements and biochemical examinations. The study complied with the Declaration of Helsinki and was approved by the Institutional Review Board of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital.
Anthropometric and biochemical measurements
BMI was calculated as weight (kilograms) divided by height2 (metres). WC was measured at the level of the umbilicus, and hip circumference was measured around the buttocks. WHR was calculated as the ratio between the waist and hip circumferences in centimetres. Body fat percentage (%) was assessed with the TBF-410 Tanita Body Composition Analyzer (Tanita, Tokyo, Japan).
Each subject underwent a 75 g oral glucose tolerance test, and blood samples were obtained at the fasting, 30-min and 2-h time points during the oral glucose tolerance test. Glucose levels were assayed with the glucose oxidase method, and plasma insulin levels were measured by radioimmunoassay (Linco Research, St Charles, MO, USA). We also calculated the areas under the curve of glucose and insulin using the trapezoidal rule and estimated the insulinogenic index. Insulin sensitivity and secretion were estimated according to the homeostasis model assessments of insulin resistance and β-cell function (HOMA-IR and HOMA-B, respectively), as well as computations proposed by Stumvoll et al.9 and Gutt et al.,10 generating the following five indices: HOMA-IR, HOMA-B, Stumvoll first-phase and second-phase insulin secretion, and Gutt index (Supplementary Table S1).
Single-nucleotide polymorphism (SNP) selection, genotyping and quality-control analysis
We selected almost all of reported SNPs associated with BMI and WHR from large-scale genome-wide association studies, most of which were primarily identified in European populations and subsequently replicated in East Asian populations. After filtering those variants in linkage disequilibrium with each other in the same regions (r2>0.8), we focussed on 40 independent BMI-SNPs and 13 WHR-SNPs.11, 12, 13, 14 As 8 out of the 40 BMI-SNPs are monomorphic in Han Chinese populations, a total of 32 BMI-SNPs and 13 WHR-SNPs were genotyped using the MassARRAY Compact Analyzer (Sequenom, San Diego, CA, USA). The characteristics of the included SNPs are listed in Supplementary Table S2. None of the SNPs failed quality control, with call rates >95% and concordant rates >99%.
Genetic risk score (GRS) calculation
Both unweighted and weighted BMI-GRS and WHR-GRS were calculated. Specifically, the unweighted GRS was created by summing the number of BMI- or WHR-increasing alleles. Considering the varying effect size, the weighted computation of BMI and WHR was calculated by multiplying each subject’s allele score (0, 1, 2) by the SNP’s β coefficient from previous genome-wide association studies conducted in East Asian populations and then adding the scores. To facilitate comparison with the unweighted GRS, the value of the weighted computation was rescaled by dividing all values by the sum of the β coefficients and then multiplying by the total number of SNPs, thus obtaining the final weighted GRS. For missing data, only subjects for whose data were missing for >15% of total SNPs (that is, five SNPs for BMI and one SNP for WHR) were excluded. GRS of the remaining subjects with missing data was standardized to those for subjects with complete data (Supplementary Table S1).
Statistical analysis
All traits were standardized to Z-scores of a mean of 0 and an s.d. of 1 to allow comparison of effect sizes across traits. Linear regression analysis was used to test the effects of individual SNPs on quantitative traits with the additive genetic model using PLINK (http://pngu.mgh.harvard.edu/~purcell/plink/). The statistical analyses were performed using the SAS software (version 8.0; SAS Institute, Cary, NC, USA), unless otherwise specified. All analyses were adjusted for covariates, such as age, sex and other variables, if appropriate. A two-tailed P-value <0.05 was considered significant.
For observed analyses, general linear regression models were used to assess the association of BMI or WHR with other quantitative traits. The regression coefficients βObesity−Trait were calculated in units of 1-s.d. metabolic traits per 1 s.d. of BMI or WHR increment.
For MR analysis, we used the GRS for predisposition to higher BMI or WHR as an instrumental variable. BMI-GRS and WHR-GRS were modelled as continuous variables, and a general linear regression model was applied to test the associations with quantitative traits. The MR framework for estimating causal effects is described in Figure 1. The regression coefficients βGRS−Trait are calculated in units of 1-s.d. observed metabolic traits per 1 unit of BMI- or WHR-GRS increment. The causal effect estimates are hereby inferred to βe(Obesity−Trait), which equals to the result of βGRS−Trait divided by βGRS−Obesity, where βGRS−Obesity is the association of GRS with BMI or WHR. Difference between βo(Obesity−Trait) and βe(Obesity−Trait) is compared by using the t-statistic.
The framework of MR. The theory of MR by using obesity GRS as an instrumental variable to dissect the causal relationship between different types of obesity and glycaemic-related traits. Associations determined from observed linear regression analyses are shown in black solid line. Estimated associations are shown in black dashed line. The causal effect estimates, βe(Obesity−Trait), is the GRS association with traits (βGRS−Trait) divided by GRS association with obesity (βGRS−Obesity).
Post hoc power for each SNPs with obesity-related traits was calculated with the Quanto software (http://biostats.usc.edu/Quanto.html, version 1.2.4, May 2009) and the power for MR analyses was estimated with the G*Power software.15 Our study had 43–84% power to detect an effect size of 0.25 kg m−2 for BMI and 13–40% power to detect an effect size of 0.048 for WHR for minor allele frequencies ranging between 0.1 and 0.5. For MR analysis, we had 60–91.5% power of detecting the estimate effect sizes for BMI-GRS and WHR-GRS with a two-sided α of 0.05.
Results
General characteristics
In total, 2884 middle-aged subjects from community-based Han Chinese populations with genotype and metabolic phenotype measurements were included in our analysis. The characteristics of the subjects are shown in Table 1. As shown in Supplementary Table S2, the effects of 26 BMI-SNPs and 5 WHR-SNPs were directionally consistent with the results from previously reported studies. The association of 9 BMI-SNPs with BMI and 3 WHR-SNP with WHR reached a significant level (P range from 8.19 × 10−7 to 0.0495), which was in line with the number of SNPs according to our power calculation.
Effects of BMI and WHR with glycaemic-related traits: the observational analysis
In observational analysis, BMI was robustly correlated with a range of glycaemic-related traits (that is, insulin sensitivity and insulin secretion indices) and we also observed almost similar associations of WHR with these glycaemic-related traits (P range from 3.38 × 10−55 to 0.028; Tables 2 and 3)
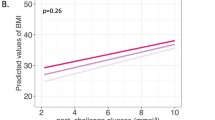
BMI and glycaemic-related traits: the MR analysis
The causal effects of BMI on glycaemic-related traits were analysed using MR using BMI-GRS as an instrumental variable. First, the weighted BMI-GRS was robustly associated with 0.036 s.d. per allele or 0.12 kg m−2 per allele higher BMI (P=4.62 × 10−13). The BMI-GRS distribution and its association with BMI are described in Figure 2. The BMI-GRS also associated with WC, WHR and body fat percentage (P range from 6.65 × 10−13 to 8.17 × 10−6).
In MR analysis, we identified that each one of s.d. (3.35 kg m−2) genetic-elevated BMI increased insulin resistance, as assessed with the HOMA-IR (β=0.379, s.e.=0.150; P=0.011), Stumvoll first-phase insulin secretion (β=0.518, s.e.=0.159; P=0.001) and higher Stumvoll second-phase insulin secretion (β=0.475, s.e.=0.155; P=0.002). In other words, a genetically determined 1 s.d. (3.35 kg m−2) higher BMI caused a unit of 1.02 higher HOMA-IR, 178.18 pmol l−1 higher Stumvoll first-phase and 35.52 pmol l−1 higher Stumvoll second-phase insulin secretion (P range from 0.001 to 0.011). However, most of the associations mentioned above disappeared after adjusting for WC and WHR, except for the Stumvoll first-phase and Stumvoll second-phase insulin secretion (P=0.013 and 0.031, respectively). When comparing the observed association of BMI with the significant glycaemic-related traits and the estimated causal association (βo(BMI−Trait) versus βe(Obesity−Trait)), we found no substantial heterogeneity (P for difference >0.05) except for the relationship between BMI and Stumvoll first-phase insulin secretion. The causal estimate of the relationship between BMI and increased Stumvoll first-phase insulin secretion analysis was larger than the observed association (0.518 versus 0.182, P for difference=0.036). However, we did not retest the difference after adjusting for central obesity in MR analysis (Table 2).
WHR and glycaemic-related traits: the MR analysis
We first validated that the WHR-GRS was associated with 0.039 s.d. higher WHR (equivalents to the change of 0.002 in WHR) per point score after adjusting for age, sex and BMI (P=1.00 × 10−7). The WHR-GRS distribution and its association with WHR are described in Figure 3. In addition, an elevated WHR-GRS showed a tendency to increased BMI (P=0.084).
In MR analysis, we identified each one of s.d. (equivalents to the change of 0.002 in WHR) genetic-elevated WHR increased insulin resistant as represented by the HOMA-IR (β=0.452, s.e.=0.228; P=0.048) and reduced insulin sensitivity as represented by the Gutt index (β=−0.499, s.e.=0.228; P=0.028). Namely, a genetically determined one s.d. higher WHR (equivalents to the change of 0.002 in WHR) caused a unit of 1.21 higher HOMA-IR and a unit of 18.40 lower the Gutt index. Regarding β-cell function, we observed that each additional WHR-increasing allele in the GRS was associated with higher Stumvoll first-phase insulin secretion (P=0.041) but did not retest the substantial causality between WHR and Stumvoll first-phase insulin secretion. No heterogeneity was apparent between βo(GRS−Trait) and βe(GRS−Trait) in MR analysis for WHR and glycaemic-related traits (P for difference >0.05). We did not demonstrate any causal relationship between WHR and glycaemic-related traits without adjustment of BMI (Table 3).
Sensitivity analysis
In a sensitivity analysis, similar associations were observed for the unweighted BMI-GRS (shown in Supplementary Tables S3–S5). We found that the effects of BMI-GRS and WHR-GRS on glucose and insulin metabolism were unaltered when GRS was modelled as the variable categorized into quartiles. Similar results were observed when excluding all subjects with missing genotypes (data not shown).
Discussion
We first explored the causal role of overall and central obesity in the pathogenesis of T2D by using a MR method with BMI-GRS and WHR-GRS as instrument variables in a community-based Han Chinese population comprising middle-aged adults. Our study, which first combined 13 WHR variants replicated among East Asian populations, pointed out the causal effects of overall obesity (represented by BMI) on insulin secretion but the causal link between central obesity (represented by WHR) and adverse insulin sensitivity.
Overall and central obesity were each independently associated with T2D incidence. However, there are few studies that directly addressed the difference in insulin sensitivity and insulin secretion among the two types of obesity. The recent increasing evidence has illustrated that excess visceral fat, termed with central obesity, could strongly worsen insulin sensitivity, which was consistent with the causal effects of central obesity on adverse insulin sensitivity. The ectopic fat storage, as the limited ability of fat to expand, could result in a spillover of lipid delivery to non-adipose tissue preceding insulin resistance and diabetes.16, 17, 18
In contrast, the response of β-cell function in obesity has mixed findings. The majority of obesity subjects often had higher insulin levels than lean subjects, which is known as compensatory insulin secretion in the presence of insulin resistance.19 Dietary restriction can significantly improve β-cell function in subjects with obesity and T2D.17 Yet several other studies observed the similarly impaired β-cell function between obesity and lean subjects with the same degree of glucose intolerance20 and found an association of the BMI-GRS with reduced β-cell function in non-diabetic subjects.21 The opposite findings were probably explained by the different methods of measuring β-cell function and glucose intolerance status of subjects. Thus establishing causality from observational studies is difficult. Our study first applied the framework of MR analysis to illustrate the difference in insulin secretion among two types of obesity, strongly indicating the enhanced β-cell function in overall obesity. Better understanding of the dynamic change in β-cell function followed by obesity needs to be investigated in longitudinal and experimental studies.
Now that T2D and obesity are interplayed with each other, an unanswered question is whether glucose metabolism has the causal role in obesity. Similar MR analyses were also performed when using T2D-GRS as instrumental variables on the basis of 27 replicated T2D-related loci among 2060 subjects (as shown in Supplementary Figure S1).22 We found that the T2D risk was positively associated with BMI in conventional analyses (P<0.001). Specifically, T2D subjects had higher BMI compared with control subjects. In MR analyses, however, T2D susceptibility showed a trend to decreased BMI ((P=0.092). Even though our results did not support the hypothesis that glucose homeostasis may have a causative effect on obesity, we could not completely exclude the potential modifying role in obesity and found the opposite associations in two approaches. In support of our findings, some other researchers also have claimed an inverse associations of T2D-GRS and BMI,23, 24 reflecting biological pathways linking T2D and obesity. Moreover, observational analysis displayed the positive associations of T2D risk with obesity, which might be explained by other environmental confounding factors or reverse causality. Further large-scale prospective cohort and multi-ethnicity MR studies are warranted to elucidate the interplay between glucose metabolism and obesity.
Our study has several limitations. First, adjustments for multiple comparison tests were not performed because SNPs were selected on the basis of an a priori hypothesis and the traits analysed were highly related. Second, owing to the the differences in linkage disequilibrium patterns, the generalizability of our GRS in other ethnic groups merits further investigation. Moreover, our finding needs to be replicated in other MR analyses and large-scale prospective cohort.
Conclusions
In brief, we demonstrate that the causal role of obesity in the pathogenesis of T2D varied between overall and central obesity in Han Chinese populations. Our results suggests that overall obesity could lead to compensatory insulin secretion while central obesity resulted in worse insulin sensitivity. Those individuals in which the decrease in insulin sensitivity is not off set by increased insulin secretion owing to limited β-cell function will suffer from diabetes.
References
Kopelman P . Health risks associated with overweight and obesity. Obes Rev 2007; 8 (Suppl 1): 13–17.
Hebert JR, Allison DB, Archer E, Lavie CJ, Blair SN . Scientific decision making, policy decisions, and the obesity pandemic. Mayo Clin Proc 2013; 88: 593–604.
Goodpaster BH, Krishnaswami S, Resnick H, Kelley DE, Haggerty C, Harris TB et al. Association between regional adipose tissue distribution and both type 2 diabetes and impaired glucose tolerance in elderly men and women. Diabetes Care 2003; 26: 372–379.
Langenberg C, Sharp SJ, Schulze MB, Rolandsson O, Overvad K, Forouhi NG et al. Long-term risk of incident type 2 diabetes and measures of overall and regional obesity: the EPIC-InterAct case-cohort study. PLoS Med 2012; 9: e1001230.
Holmes MV, Lange LA, Palmer T, Lanktree MB, North KE, Almoguera B et al. Causal effects of body mass index on cardiometabolic traits and events: a Mendelian randomization analysis. Am J Hum Genet 2014; 94: 198–208.
Hagg S, Fall T, Ploner A, Magi R, Fischer K, Draisma HH et al. Adiposity as a cause of cardiovascular disease: a Mendelian randomization study. Int J Epidemiol 2015; 44: 578–586.
Zhang B, Shu XO, Delahanty RJ, Zeng C, Michailidou K, Bolla MK et al. Height and breast cancer risk: evidence from prospective studies and Mendelian randomization. J Natl Cancer Inst 2015; 107: djv219.
Adamsson Eryd S, Sjogren M, Smith JG, Nilsson PM, Melander O, Hedblad B et al. Ceruloplasmin and atrial fibrillation: evidence of causality from a population-based Mendelian randomization study. J Intern Med 2014; 275: 164–171.
Stumvoll M, Van Haeften T, Fritsche A, Gerich J . Oral glucose tolerance test indexes for insulin sensitivity and secretion based on various availabilities of sampling times. Diabetes Care 2001; 24: 796–797.
Gutt M, Davis CL, Spitzer SB, Llabre MM, Kumar M, Czarnecki EM et al. Validation of the insulin sensitivity index (ISI(0,120)): comparison with other measures. Diabetes Res Clin Pract 2000; 47: 177–184.
Okada Y, Kubo M, Ohmiya H, Takahashi A, Kumasaka N, Hosono N et al. Common variants at CDKAL1 and KLF9 are associated with body mass index in east Asian populations. Nat Genet 2012; 44: 302–306.
Wen W, Cho YS, Zheng W, Dorajoo R, Kato N, Qi L et al. Meta-analysis identifies common variants associated with body mass index in east Asians. Nat Genet 2012; 44: 307–311.
Wen W, Zheng W, Okada Y, Takeuchi F, Tabara Y, Hwang JY et al. Meta-analysis of genome-wide association studies in East Asian-ancestry populations identifies four new loci for body mass index. Hum Mol Genet 2014; 23: 5492–5504.
Wen W, Kato N, Hwang JY, Guo X, Tabara Y, Li H et al. Genome-wide association studies in East Asians identify new loci for waist-hip ratio and waist circumference. Sci Rep 2016; 6: 17958.
Faul F, Erdfelder E, Buchner A, Lang AG . Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 2009; 41: 1149–1160.
Samuel VT, Shulman GI . Mechanisms for insulin resistance: common threads and missing links. Cell 2012; 148: 852–871.
Hajer GR, van Haeften TW, Visseren FL . Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur Heart J 2008; 29: 2959–2971.
Tchernof A, Despres JP . Pathophysiology of human visceral obesity: an update. Physiol Rev 2013; 93: 359–404.
Prentki M, Nolan CJ . Islet beta cell failure in type 2 diabetes. J Clin Invest 2006; 116: 1802–1812.
Takahara M, Katakami N, Kaneto H, Noguchi M, Shimomura I . Pancreatic beta cell function in lean and obese Japanese with various degrees of glucose tolerance. Endocr J 2013; 60: 923–930.
Zhu J, Zong G, Lu L, Gan W, Ji L, Hu R et al. Association of genetic predisposition to obesity with type 2 diabetes risk in Han Chinese individuals. Diabetologia 2014; 57: 1830–1833.
Yan J, Peng D, Jiang F, Zhang R, Chen M, Wang T et al. Impaired pancreatic beta cell compensatory function is the main cause of type 2 diabetes in individuals with high genetic risk: a 9 year prospective cohort study in the Chinese population. Diabetologia 2016; 59: 1458–1462.
Peter I, McCaffery JM, Kelley-Hedgepeth A, Hakonarson H, Reis S, Wagenknecht LE et al. Association of type 2 diabetes susceptibility loci with one-year weight loss in the look AHEAD clinical trial. Obesity (Silver Spring) 2012; 20: 1675–1682.
Langenberg C, Sharp SJ, Franks PW, Scott RA, Deloukas P, Forouhi NG et al. Gene-lifestyle interaction and type 2 diabetes: the EPIC interact case-cohort study. PLoS Med 2014; 11: e1001647.
Acknowledgements
This work is supported by 973 Program of China (2013CB530606), program from National Natural Science Foundation of China grants (81322010, 81300619 and 81570713), The Shanghai Jiaotong Medical/Engineering Foundation (YG2014MS18), National Program for Support of Top-notch Young Professionals and grants from the State Key Laboratory of Medical Genomics, Youth research project of Shanghai Municipal Health Bureau (20134Y048). We thank all the research volunteers and cooperative workers for their participation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Rights and permissions
About this article
Cite this article
Wang, T., Ma, X., Tang, T. et al. Overall and central obesity with insulin sensitivity and secretion in a Han Chinese population: a Mendelian randomization analysis. Int J Obes 40, 1736–1741 (2016). https://doi.org/10.1038/ijo.2016.155
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.155
- Springer Nature Limited
This article is cited by
-
Alcohol consumption and its interaction with genetic variants are strongly associated with the risk of type 2 diabetes: a prospective cohort study
Nutrition & Metabolism (2019)
-
Thyroid function and ischemic heart disease: a Mendelian randomization study
Scientific Reports (2017)