Abstract
Background:
To identify loci associated with abdominal fat and replicate prior findings, we performed genome-wide association (GWA) studies of abdominal fat traits: subcutaneous adipose tissue (SAT); visceral adipose tissue (VAT); total adipose tissue (TAT) and visceral to subcutaneous adipose tissue ratio (VSR).
Subjects and Methods:
Sex-combined and sex-stratified analyses were performed on each trait with (TRAIT–BMI) or without (TRAIT) adjustment for body mass index (BMI), and cohort-specific results were combined via a fixed effects meta-analysis. A total of 2513 subjects of European descent were available for the discovery phase. For replication, 2171 European Americans and 772 African Americans were available.
Results:
A total of 52 single-nucleotide polymorphisms (SNPs) encompassing 7 loci showed suggestive evidence of association (P<1.0 × 10−6) with abdominal fat in the sex-combined analyses. The strongest evidence was found on chromosome 7p14.3 between a SNP near BBS9 gene and VAT (rs12374818; P=1.10 × 10−7), an association that was replicated (P=0.02). For the BMI-adjusted trait, the strongest evidence of association was found between a SNP near CYCSP30 and VAT–BMI (rs10506943; P=2.42 × 10−7). Our sex-specific analyses identified one genome-wide significant (P<5.0 × 10−8) locus for SAT in women with 11 SNPs encompassing the MLLT10, DNAJC1 and EBLN1 genes on chromosome 10p12.31 (P=3.97 × 10–8 to 1.13 × 10−8). The THNSL2 gene previously associated with VAT in women was also replicated (P=0.006). The six gene/loci showing the strongest evidence of association with VAT or VAT-BMI were interrogated for their functional links with obesity and inflammation using the Biograph knowledge-mining software. Genes showing the closest functional links with obesity and inflammation were ADCY8 and KCNK9, respectively.
Conclusions:
Our results provide evidence for new loci influencing abdominal visceral (BBS9, ADCY8, KCNK9) and subcutaneous (MLLT10/DNAJC1/EBLN1) fat, and confirmed a locus (THNSL2) previously reported to be associated with abdominal fat in women.
Similar content being viewed by others
Introduction
Body fat distribution, particularly truncal abdominal fat, has long been recognized as a major determinant of the metabolic complications associated with an increased risk of type 2 diabetes and cardiovascular disease in obese individuals.1, 2, 3, 4, 5, 6, 7 A large number of studies, reviewed elsewhere,8, 9, 10 have clearly established that the pattern of fat distribution is influenced by genetic factors, generally to a larger extent than overall body fatness. The first evidence for a genetic component for body fat distribution was based on data from anthropometric measures obtained in 1698 subjects from the Quebec Family Study (QFS). Truncal abdominal fat, assessed by computing the ratio of trunk skinfolds (sum of subscapular, suprailiac and abdominal skinfolds) to extremity skinfolds (sum of triceps, biceps and medial calf skinfolds), was found to be more influenced by genetic factors than total subcutaneous fat (sum of six skinfolds), with heritability estimates of 60% and 38%, respectively.11 Another study based on principal components analysis of the six skinfolds reported a heritability of 52% for a component contrasting trunk-to-extremity skinfolds.12 Waist circumference (WAIST) has also been widely used as an indicator of abdominal obesity, and a large number of twin13, 14, 15, 16 and family17, 18, 19, 20, 21, 22 studies have reported heritability estimates in the range of 40 to 75% for WAIST. It is noteworthy that in most studies, WAIST was not adjusted for body mass index (BMI) in order to obtain a heritability estimate of fat distribution independent of body mass. As observed in one study that reported a heritability estimate of 29% for BMI-adjusted WAIST, compared with 46% without adjustment for BMI,23 the heritability of WAIST is generally attenuated after adjustment for BMI.
Only a few studies have reported heritability estimates of fat distribution using imaging techniques such as dual-energy X-ray absorptiometry or computed tomography. Heritability of visceral adipose tissue (VAT) measured by computed tomography was first reported in QFS24 and the HERITAGE Family Study.25 After adjustment for total body fatness, significant genetic effects (48–56%) were found in both studies. Other family studies, which used dual-energy X-ray absorptiometry measurements to assess fat distribution, have reported heritability estimates in the range of 33–85% for the amount of fat in the trunk.26, 27, 28, 29 Two reports based on data from the HERITAGE Family Study have shown that changes in the amount and distribution of subcutaneous fat30 and changes in VAT31 in response to exercise training were influenced by genetic factors. Studies undertaken in pairs of male monozygotic twins submitted to a 100-day 1000 kcal per day caloric surplus32 or energy deficit induced by exercise33 showed significant within-pair resemblance, with intraclass coefficients reaching 0.72 and 0.84, for changes in abdominal visceral fat in response to overfeeding or negative energy balance protocol, respectively.
A large number of candidate gene studies have identified genes associated with various indices of body fat distribution34, 35, 36, 37, 38, 39 or changes in body fat distribution in response to diet.40 Multiple genome-wide association studies (GWAS) have identified several loci associated with anthropometric measures of fat distribution such as WAIST or waist-to-hip ratio (WHR),41, 42, 43, 44, 45, 46, 47 but few have been performed using direct measures of abdominal fat that can discriminate between abdominal visceral and subcutaneous fat deposition. Using measures of abdominal subcutaneous adipose tissue (SAT) and VAT obtained by computed tomography, Fox et al.48 performed a GWAS of SAT, VAT, VAT adjusted for BMI (VAT–BMI) and VAT/SAT ratio (VSR) in men and women from four population-based studies. They found genome-wide significant evidence of association for a single-nucleotide polymorphism (SNP; rs11118316) at LYPLAL1 gene for VAT/SAT ratio, in a region previously identified in a GWA study for WHR.41 A new locus for VAT was also identified on chromosome 2 in women (rs1659258 near THNSL2 gene).
In the present study, we report results from GWA analysis of several measures for fat distribution obtained by computed tomography in the coronary artery risk development in young adults (CARDIA) study, the health risk factors exercise training and genetics (HERITAGE) Family Study and the Quebec family study (QFS). We performed a GWA analysis of total abdominal (TAT), subcutaneous (SAT), visceral (VAT) adipose tissue and visceral to subcutaneous adipose tissue ratio (VSR), with and without adjustment for BMI. Given the importance of sexual dimorphism in the distribution of body fat and also as an attempt to replicate findings from the Fox et al. paper,48 we also performed sex-stratified GWA analysis of SAT, VAT, VAT–BMI and VSR.
Patients and methods
Study samples
Participants of European descent from CARDIA, HERITAGE and QFS were included in the GWA analysis. All three studies obtained informed consent from participants and approval from the appropriate institutional review boards.
The CARDIA study is a prospective multicenter study designed to investigate the development of cardiovascular disease risk factors and subclinical and clinical disease in young (18–30 years) Black and White men and women from four geographic locations in the United States. A total of 5115 subjects were recruited from the total community in Birmingham, AL, USA, from selected census tracts in Chicago, IL, USA and Minneapolis, MN, USA; and from the Kaiser Permanente health plan membership in Oakland, CA, USA. The details of the study design for the CARDIA study have been published previously.49 Eight examinations have been completed since initiation of the study in 1985–1986, respectively in the years 0, 2, 5, 7, 10, 15, 20, and 25. For the present study, abdominal adipose tissue imaging data were available at year 25 in 1335 Whites.
The HERITAGE Family Study was designed to evaluate the role of genetic and nongenetic factors in cardiovascular, metabolic, and hormonal responses to aerobic exercise training.50 Extensive data, including body composition, cardiovascular risk factors and lifestyle habits were gathered on almost 800 White and Black subjects in over 200 families, both before and after 20 weeks of supervised training. In the present study, analyses were performed using baseline data in Whites only (n=496).
The QFS was designed to investigate the contribution of genetic factors in obesity and its related metabolic complications in French–Canadian families.51 The cohort represents a mixture of random sampling and ascertainment through obese (BMI>30 kg m−2) probands. Measurements of abdominal fat by computed tomography were available on a total of 682 subjects.
Phenotype data
In all three studies, the amounts of VAT, SAT and TAT were assessed by computed tomography with a scan performed at the abdominal level (L4 and L5 vertebrae) as described elsewhere for CARDIA,52 HERITAGE25 and QFS.53 Participants were examined in the supine position with both arms stretched above head. TAT area was calculated by delineating the abdominal scan with a graph pen and then by computing the TAT with an attenuation range of −190 to −30 Hounsfield units. VAT was measured by drawing a line within the muscle wall surrounding the abdominal cavity and SAT was calculated by subtracting VAT from TAT. The VSR was also computed.
Genotype data
For the CARDIA Study, genotyping was performed using the Affymetrix Genome-Wide Human SNP Array 6.0 (Santa Clara, CA, USA). Genotyping was completed with a sample call rate ⩾98%. A total of 578 568 SNPs passed quality control (minor allele frequency ⩾2%, call rate ⩾95%, Hardy–Weinberg equilibrium (HWE)⩾10−4) and were used for imputation.
For HERITAGE, genotyping was performed using the Illumina HumanCNV370-Quad v3.0 BeadChips on Illumina BeadStation 500 GX platform (San Diego, CA, USA). The genotype calls were done with the Illumina GenomeStudio software and all samples were called in the same batch to eliminate batch-to-batch variation. Monomorphic SNPs and SNPs with only one heterozygote, as well as SNPs with more than 30% missing data were filtered out with GenomeStudio. Twelve samples were genotyped twice with 100% reproducibility across all SNPs. All GenomeStudio genotype calls with a GenTrain score less than 0.885 were checked and confirmed manually. Quality control of the GWAS SNP data confirmed all family relationships and found no evidence of DNA sample mix-ups.
For QFS, genotyping was performed using the Illumina 610-Quad chip containing 620.901 markers including 582,591 autosomal SNPs. The 610-Quad BeadChips were scanned on an Illumina BeadArray™ reader and the BeadStudio software package included with the Illumina® BeadStation 500 GX system was used to extract genotyping data from images collected from the reader. The BeadStudio Genotyping Module software was used to call SNP genotypes. After exclusion of copy number variations, SNPs called in less than 95% of the subjects, SNPs not in HWE (P<10−4) and those with a minor allele frequency <1%, a total of 543,714 SNPs were available for analysis.
For all three studies, imputation was performed using CEU reference panel consisting of 120 haplotypes from HapMap Phase II data (release 22, build 36) and the MACH software.54 A total of 2,473,256 directly typed or imputed SNPs were tested for association with the abdominal fat phenotypes.
Statistical analyses
We performed meta-analyses for a total of eight abdominal fat phenotypes: TAT, SAT, VAT, VSR, TAT–BMI, SAT–BMI, VAT–BMI and VSR–BMI. Log transformation was used to normalize the distribution of VAT and VSR. The primary analysis was performed in each cohort separately using regression models, additive genetic effects and accounting for phenotype correlation among family members when appropriate. For all phenotypes, age and sex were used as covariates. When a SNP was both genotyped and imputed, genotyped SNPs were used for analysis. These cohort-specific results were combined with fixed effects meta-analysis using the inverse-variance weighting method in METAL.55 In addition to the analyses performed in combined men and women and in an attempt to replicate the findings of Fox et al.48 sex-stratified analyses were also performed in each cohort for the following phenotypes: SAT, VAT, VAT–BMI and VSR. These cohort-specific results were then combined through meta-analysis.
Replication cohort
To replicate findings from the meta-analysis, the Pennington Center Longitudinal Study (PCLS) cohort was used. The PCLS cohort is composed of individuals who participated in various clinical studies (diet interventions, weight loss and other metabolic studies) conducted at the Pennington Biomedical Research Center since 1992.56 The total PCLS sample included 2943 adult (18–84 years of age) subjects consisting of 2171 European American men (n=897) and women (n=1,274) and 772 African American men (n=185) and women (n=587). All participants provided written, informed consent. In PCLS, abdominal fat was measured using either dual-energy X-ray absorptiometry (for 1707 subjects) or computed tomography (for 1236 subjects) as described elsewhere.57, 58
PCLS replication genotyping
A total of 23 SNPs were selected for replication in the PCLS cohort, including 10 SNPs showing evidence (P<1 × 10−6) of association with abdominal fat phenotypes in our sex-combined GWAS meta-analysis as well as 13 SNPs from the paper by Fox et al.48 showing evidence of association with abdominal fat. When multiple SNPs in strong linkage disequilibium were associated with abdominal fat traits on a given region, two SNPs were selected for genotyping to make sure that at least one SNP was available for data analysis if the other one failed the assay. DNA for the replication studies was extracted from buffy coats. The SNPs were genotyped using Illumina GoldenGate assay and Veracode technology on the BeadXpress platform (San Diego, CA, USA). Genotype calling was done using Illumina GenomeStudio software. All SNPs were in HWE (tested using the exact HWE test implemented in the PEDSTATS software package59). In addition, five CEPH DNA samples included in the HapMap Phase II CEU panel (NA10851, NA10854, NA10857, NA10860, NA10861) were genotyped in triplicate. Concordance between the replicates as well as with the SNP genotypes from the HapMap database was 100%.
In silico generation of functional hypotheses
In order to prioritize gene/loci showing evidence of association and to explore the possible functional links among these loci and obesity-related traits, we used the Biograph knowledge-mining software.60 Biograph assembles and analyzes information from 22 heterogeneous biomedical databases via unsupervised data-mining techniques and stochastic random walks to generate a map of relationships linking ‘source concepts’ (for example, phenotypes, diseases) to ‘targets’ (for example, candidate genes). This network of relationships is analyzed to score and rank the different ‘paths’ linking concepts to targets, resulting in an automated formulation of functional hypotheses. The relative strength of each hypothesis is computed to assess the ‘proximity’ of the association between a ‘concept’ and a ‘target’.61
Results
Descriptive statistics of the phenotype data for the three cohorts are presented in Table 1. A total of 2513 subjects, including 1152 men and 1361 women, were available for the discovery phase plus 2943 (2171 Whites) for the replication component. Participants were mostly middle aged, with a mean age of 35.9, 40.5 and 50.8 years in HERITAGE, QFS and CARDIA, respectively.
Sex-combined analyses
To assess population stratification, quantile–quantile (QQ) plots were examined for all phenotypes in the sex-combined (Supplementary Figure S1) and the sex-specific (Supplementary Figure S2) meta-analyses. A genomic control lambda value of 1.0 indicates no stratification and values below 1.05 are generally considered as benign.62 As shown in Supplementary Figures S1 and S2, lambda values range from 0.999 to 1.021, suggesting little evidence for unaccounted population stratification.
The Manhattan plots for the abdominal fat phenotypes with (right panel) and without (left panel) adjustment for BMI are shown in Supplementary Figure S3. The horizontal lines in the plots correspond to P-values of 1.0 × 10−6 and 5.0 × 10−8, respectively. No SNP reached genome-wide significance (P-value<5 × 10−8). However, a total of 52 SNPs showed suggestive evidence (P-values<1.0 × 10−6) of association with the various abdominal fat phenotypes (results shown in Table 2). For the phenotypes not adjusted for BMI, our most significant finding was with rs12374818 on chromosome 7p14.3 for VAT (P=1.10 × 10−7; Table 2 and Figure 1a). This SNP is located near BBS9. For the other abdominal fat phenotypes not adjusted for BMI, the top hits were with rs9328211 on chromosome 6 for TAT near the PRPF4B locus (P=7.93 × 10−7) and rs2679649 on chromosome 6 for SAT near the HMGB3P18 locus (P=4.97 × 10−7). For the BMI-adjusted phenotypes, the most significant finding was with rs10506943 on chromosome 12q21.32 for VAT–BMI near the CYCSP30 locus (P=2.42 × 10−7; Table 2 and Figure 1b). For the other BMI-adjusted traits the most significant findings were with rs6038439 on chromosome 20 for TAT–BMI near the FGFR3P3 locus (P=4.48 × 10−7) and rs6866135 on chromosome 5 for SAT–BMI near the HSPD1P15 locus (P=3.87 × 10−7). For VSR, no suggestive evidence of association was found, whether adjusted for BMI or not; the best evidence of association (results not shown) was found with two SNPs on chromosomes 4: rs2292298 for VSR (P=1.00 × 10−6) and rs11946679 (P=1.25 × 10−6) for VSR–BMI.
Regional plots for loci showing the strongest evidence of association Regional plots for loci showing the strongest evidence of association with VAT (a), VAT–BMI (b), and SAT in women (c) SNPs are plotted by position on chromosome against association (−log10 P-value) and estimated recombination rate (from HapMap-CEU). SNPs surrounding the most significant SNP (purple diamond) are color-coded to reflect their LD with this SNP. Genes and the positions of exons as well as the direction of transcription are shown below the plots. These regional plots were generated using LocusZoom (http://csg.sph.umich.edu/locuszoom/).
Sex-specific analyses
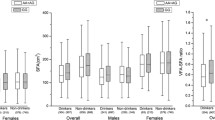
The Manhattan plots for the sex-specific analyses are presented in Supplementary Figure S4. Table 3 presents the results of the sex-specific analyses for the SNPs achieving suggestive evidence of association (P<1.0 × 10−6). Except for VAT, the top SNPs for each abdominal fat phenotype analyzed showed stronger evidence of association in women than in men. In men, the best evidence of association was found with rs170053 on chromosome 13 for SAT near the PCDH17 locus (P=5.99 × 10−7); rs10505574 on chromosome 8 for VAT near the ADCY8 locus (P=2.62 × 10−7) and rs2930176 on chromosome 3 for VSR near the CACNA1D locus (P=6.06 × 10−7). In women, 11 SNPs on chromosome 10 reached genome-wide significant evidence of association (P<5.0 × 10−8) with SAT, the strongest evidence of association being found with SNP rs7919823 on chromosome 10p12.21 near the MLLT10 locus (P=1.13 × 10−8; Table 3 and Figure 1c). Two other SNPs on chromosome 13 (rs12866352 near EFNB2, P=8.16 × 10−7) and chromosome 14 (rs4384548 near BDKRB2, P=5.27 × 10−8) reached suggestive evidence of association with SAT. The key hits for the other abdominal fat phenotypes in women were on chromosome 8 (rs16910486 near KCNK9, P=5.82 × 10−7), chromosome 11 (rs7927727 near FAR1, P=1.86 × 10−7) and chromosome 8 (rs10095849 near ADAM18, P=2.42 × 10−7) for VAT, VAT–BMI and VSR, respectively.
Replication
Table 4 presents the results of replication analyses in the PCLS cohort for the SNPs showing evidence of suggestive association in the sex-combined analyses. Among the 14 SNPs that were tested for association in European Americans and African Americans, separately, three showed evidence of replication (indicated in bold in Table 4). The association found on chromosome 6 with SAT and two SNPs in perfect linkage disequilibrium (rs2260078 and rs2679647) was replicated in African Americans (Pv0.0013), while the association found on chromosome 7 with VAT and rs4338001 was replicated in European Americans (P=0.024).
Replication results for the top SNPs of Fox et al.48 are presented in Table 5. Since the beta value was not provided in the Fox et al. paper, we cannot say for sure if we really replicated the original finding, because the direction of the association is not known. Nevertheless, the main finding of Fox et al. of an association between rs1659258 near THNSL2 gene and VAT in women was replicated in PCLS White women (P=0.0056) and was borderline significant in our meta-analysis (P=0.059). Another SNP on chromosome 6 showing evidence of association with VAT–BMI was replicated in PCLS Whites (P=0.0165). Their most significant finding of an association between rs11118316 and VSR near the LYPLAL1 gene (P=3.13 × 10−9) was not replicated in our meta-analysis nor in the PCLS cohort, but we found an association between this SNP and SAT in our sex-combined meta-analysis (P=0.048).
In an attempt to further replicate the findings from Fox et al. we also verified whether the SNPs from their Supplementary Table S2, which showed evidence of association with P-values <1.0 × 10−4, were associated (P<0.05) with abdominal fat in our sex-combined or sex-specific GWAS meta-analysis. The results presented in Supplementary Table S1 reveal that several SNPs were associated with abdominal fat in both studies, but not necessarily with the same trait. Replications (associations with the same trait) were found for seven different loci: chromosome 3 for VAT–BMI in women (rs7638389 near ADAMTS9, P=0.006); chromosome 6 for VSR (rs12204127 near BACH2, P=0.03); chromosome 7 for VAT–BMI in men (rs1299548 near C1GALT1, P=0.039); chromosome 14 for VAT in women (rs3783938 near TSHR, P=0.026); chromosome 15 for VSR in men (rs8036080 near VPS18, P=0.035); chromosome 19 for VAT–BMI in men (rs8106493 near SLC7A10, P=0.046) and chromosome 20 for VAT-BMI in men (rs13043330 near HSPA12B, P=0.011).
Exploratory analysis of functional associations
The Biograph tool was utilized to explore the possible functional links among VAT-associated loci, and obesity-related phenotypes. Six VAT-associated genes (BBS9, ROBO1, ADCY8, FAR1, KCNK9 and EFR3) were individually queried for association to target phenotypes. With the exception of CYCSP30, which is a pseudogene, these genes were those showing the strongest evidence of association in our sex-combined (Table 2) or sex-stratified (Table 3) analyses. An obvious target phenotype was ‘obesity’, as VAT mass is highly correlated with total adiposity. We also considered ‘inflammation’ as a target phenotype, because VAT is considered a proinflammatory organ having an important role in the etiology of obesity-related cardiometabolic complications,63, 64, 65 and also because of previous evidence of genetic pleiotropy between inflammation and abdominal obesity.21 It is therefore conceivable that, at least for a subset of genes, the observed association to VAT reflects association to VAT-related inflammation. For each target phenotype, the proximity of a gene to the phenotype was quantified as a relative rank of the gene compared with all other genes linking to the same phenotype in Biograph’s knowledge base. The phenotype-proximity ranks for the six genes are shown in Table 6. For each phenotype, the global rank represents the rank percent of a gene’s proximity score compared with the proximity scores for all other Biograph entities (genes, compounds, metabolites and so on) for the same phenotype, whereas for gene rank the comparison is restricted only to genes. A lower rank percentage indicates higher proximity between the gene and the phenotype. Based on the scores, ADCY8 (5.36%) and ROBO1 (11.68%) were ranked in the top 20% of all genes linked to ‘obesity’, whereas ADCY8 (9.59%), ROBO1 (8.48%) and KCNK9 (0.54%) scored in the top 20% for their global strength of connection to ‘inflammation’. The remaining genes had poorer ranks for both targets. The Biography-derived connectivity graphs between ADCY8 and obesity and KCNK9 and inflammation are shown in Figures 2a and b. Connectivity diagrams for the other genes are shown in Supplementary Figure S5 for obesity and Supplementary Figure S6 for inflammation.
Biograph analysis of VAT–BMI-associated genes to ‘obesity’ and ‘inflammation’ phenotypes Biograph analysis of VAT–BMI associated genes to ‘obesity’ and ‘inflammation’ phenotypes. (a) Biograph generated connectivity graph between ADCY8 gene and obesity. (b) Biograph generated connectivity graph between KCNK9 gene and inflammation. The intermediate linking the genes to the phenotype are indicated in a gray background along with the type of interaction.
Discussion
The results of this GWA study of abdominal visceral fat measured by computed tomography in three cohort studies revealed the presence of several loci associated (P<1.0 × 10−6) with measures of abdominal fat adjusted (SPAG16, FGFR3P3, HSPD1P15, CYCSP30) or not adjusted (PRPF4B, HMGB3P18, BBS9) for BMI. Our sex-combined analysis provided no genome-wide significant loci, but the evidence of association observed for VAT at BBS9 and for SAT at HMGB3P18 was replicated in an independent cohort. Our sex-stratified analysis provided one genome-wide significant locus (P<5 × 10−8) for SAT in women with a block of 11 SNPs near the MLLT10, DNAJC1 and EBLN1 genes on chromosome 10. We also confirmed in an independent cohort a previous association observed between a SNP near the THNSL2 gene and visceral fat in women.48
In the sex-combined analyses, the strongest evidence of association was found for VAT with SNP rs12374818 near the BBS9 gene on chromosome 7p14.3. The association between VAT and BBS9 was replicated in the PCLS cohort (with SNP rs4338001, r2=1.0). BBS9 is one of the 15 genes/loci that have been associated with Bardet–Biedl syndrome (BBS), a genetically heterogeneous disorder characterized by several clinical features, including polydactyly, retinopathy, renal abnormalities, mental retardation and truncal obesity. Studies have shown that BBS proteins are involved in cilia-associated functions.66 The cilium is a specialized organelle projecting from plasma membrane of almost every vertebrate cell and has a role in the transduction of extracellular signals. Using homozygosity mapping of small consanguineous BBS families followed by comparative genomics and gene expression studies of a BBS-knockout mouse model, Nishumira et al.67 identified parathyroid hormone-responsive B1 (PTHB1) gene as the BBS9 gene. Knockdown of BBS9/PTHB1 gene in zebra fish was found to lead to developmental abnormalities in the retina and brain that were consistent with the core phenotypes observed in syndromic ciliopathies and human BBS9 mRNA rescued the bbs9 knockdown phenotype.68 The exact mechanism leading to obesity in BBS patients is not known, but a study using BBS knockout mouse models showed that Bbs2−/−, Bbs4−/−, Bbs6−/− mice were resistant to the action of leptin to reduce body weight and food intake regardless of serum leptin levels and obesity, suggesting that altered leptin receptor signaling is the major cause of obesity in BBS.69 Interestingly, variants in the BBS2, BBS4 and BBS6 genes were previously reported to be associated with obesity in non-BSS individuals.70
Suggestive evidence of association was also found for SAT near the HMGB3P18 gene (high mobility group box 3 pseudogene 18), a finding that was replicated in the PCLS cohort. This pseudogene is located on chromosome 6 near the NKAIN2 locus (also known as TCBA1 gene), which was also previously found to be associated with SAT.48 For the BMI-adjusted abdominal fat phenotypes, the strongest evidence of association was found for VAT–BMI near the CYCSP30 gene (cyctochrome c, somatic pseudogene 30; location 12q21.32), one of the numerous processed cyctochrome c pseudogenes found throughout the human genome. Several SNPs in that region of chromosome 12 showed suggestive evidence of association with VAT–BMI. In a previous large GWA study of more than 10 000 Korean subjects,44 strong evidence of association was found in that region of chromosome 12 with systolic blood pressure (rs17249754, P=1.3 × 10−7) and WHR (rs2074356, P=7.8 × 10−12).
Given the importance of sexual dimorphism in the distribution of body fat, we performed sex-stratified meta-analyses. The analyses revealed that 12 loci were associated with abdominal fat in women compared with 6 loci in men. The strongest evidence of association, and the only one reaching genome-wide significant level (P<5.0 × 10−8), was found for SAT in women with 11 SNPs encompassing three different loci on chromosome 10p12.31: MLLT10, DNAJC1 and EBLN1. No evidence of association with obesity-related traits has been reported with these loci, but a SNP located in that region of chromosome 10 (rs16923476 at OTUD1/KIAA1217 locus; P=3.69 × 10−8) was previously found to be associated with severe early-onset obesity.71 In men, the strongest evidence of association was found for VAT with SNP rs10505574 on chromosome 8 between the ADCY8 and EFR3 genes (P=2.62 × 10−7).
Recent data suggest that site-specific expression of developmental genes direct adipose tissue development, while providing a mechanistic basis to explain functional differences between upper-body and lower body adipose tissue.72, 73, 74 These developmental genes include members of the homeobox (HOX) family, HOX-domain encoding genes and T-box genes, which are transcriptional factors involved in early embryonic development, body patterning and cell specification. One such gene, TBX15, was previously reported to be associated with fat distribution in GWA studies.41 Interestingly, TBX15 was first identified by its higher expression in VAT compared with SAT in both rodents and humans.75 In our meta-analysis, a SNP located in TBX15 (rs1779437) was associated with VAT–BMI (P=0.0006) and VSR–BMI (P=0.02). A second member of the T-box family of genes showing differences in expression level between abdominal fat and lower body fat is TBX5, and results of our meta-analysis also revealed that SNPs in TBX5 were associated with VAT–BMI in women (rs2236017, P=8.7 × 10−5), TAT–BMI (rs2555025, P=0.007) and VSR–BMI (rs10850336, P=0.009).
Multiple GWA studies have identified several loci associated with anthropometric measures of fat distribution.41, 42, 43, 44, 45, 76 The most recent GWA meta-analysis of traits related to fat distribution in up to 224 450 individuals identified 49 loci associated with waist-to-hip ratio adjusted for BMI (WHRadjBMI), 33 of which were new and 16 previously described.47 The study also identified seven new loci for waist circumference adjusted for BMI and three new loci for waist-to-hip ratio. None of the loci found to be associated with abdominal fat in the present study were in the list of the 59 loci reported by Shungin et al.47 to be associated with anthropometric measures of abdominal, but two of the loci reported in the present study fall in the same genomic region as two WHRadjBMI loci. One is the FGFR3P3 locus on chromosome 20 (Table 2) associated with TAT in our sex-combined analyses (rs6038439. P=4.48 × 10−7), which is in the same genomic region as BMP2 (rs979012, P=3.3 × 10−14), and the other is CACNA1D on chromosome 3 (Table 3) associated with VSR in men (rs2930176, P=6.06 × 10−7) that is close to the PBRM1 locus (rs2276824, P=3.2 × 10−11). In total, 25 of these 59 loci associated with anthropometric measures of abdominal fat showed significant sexual dimorphism, the majority of them (21 out of 25) displaying stronger effects in women,47 which is consistent with the findings from our sex-specific analyses. Other GWA studies found significant sex differences for loci associated with anthropometric measures of fat distribution,41, 43, 76 which emphasize the need for considering sex differences in association studies when searching for genes influencing the fat-distribution profile.
Only one GWA meta-analysis of abdominal adipose tissue assessed by computed tomography has been reported so far.48 In that meta-analysis of four GWA studies including 5560 women and 4997 men, the strongest association was observed between LYPLAL1 rs11118316 and VSR (P=3.1 × 10−9), a SNP in linkage disequilibrium with rs4846567 that was previously found to be associated with VSR in Japanese subjects (P=0.002)77 and with WHR adjusted for BMI (P=6.89 × 10−21).41 This result was not replicated in our study as we found only marginal evidence of association between rs11118316 and SAT in all subjects (P=0.048). For SAT, the most significant finding of Fox et al.48 was with SNP rs9922619 in the FTO gene (P=5.87 × 10−8), a SNP that we also found to be associated with SAT, but in men only (P=0.002; Supplementary Table S1). For VAT–BMI, the most significant finding of Fox et al.48 was with SNP rs1641895 in an intron of the sorting nexin 29 (SNX29) gene on chromosome 16, a variant that we found to be associated with SAT (P=0.003) and VAT (P=0.01) in women (Supplementary Table S1). Seven loci, which showed significant evidence of association with abdominal fat in the study by Fox et al.48 were replicated in our meta-analyses (Supplementary Table S1). A series of studies undertaken in overweight Japanese subjects have tested whether SNPs associated with increased susceptibility to obesity and obesity-related complications were associated with VAT and SAT measured by computed tomography. Overall, these studies tested associations between 83 SNPs in 66 genes/loci and found associations for FTO with SAT and VAT,78, 79 SH2B1 with VAT,80 CYP17A1 and NT5C2 with both SAT and VAT in women,81 LYPLAL1 with VSR, NISCH with VAT and VSR77 and NUDT3 rs206936 with SAT in women.82
As a way of exploring the potential mechanisms by which genetically associated loci may relate to biological function, we utilized the Biograph knowledge mining tool and derived exploratory functional links connecting the VAT-associated genes to the phenotypes of ‘obesity’ and ‘inflammation’. The graph linking the ADCY8 gene to ‘obesity’ displays multiple routes traversing via the GNB3 gene, an essential component of G-protein coupled receptor signaling. Notably, the GNB3 825C>T polymorphism has previously been associated with obesity in specific populations.83, 84, 85 Similarly, Biograph identified a very strong connection between the potassium channel KCNK9 gene and ‘inflammation’ (gene rank 0.7%). Among the many possible routes linking KCNK9 to inflammation, one involved local anesthetic bupivacaine. Bupivacaine is a KCNK9 inhibitor86 and is known to display complex, context-dependent pro- and anti-inflammatory effects.87, 88, 89 In addition to the hypotheses from Biograph, the KCNK9 channel activity appears to be directly enhanced by the proinflammatory cytokine TNF-alpha, eventually leading to cellular apoptosis.90 If regulation of KCNK9 activity is upstream to the generation of inflammatory signals, then one might speculate how altered KCNK9 activity could influence inflammatory signaling from VAT.
The present study has focused on the identification of genetic associations between individual loci and abdominal adipose tissue depots, with or without adjustment for total adiposity. The majority of the loci fall below the statistical threshold for genome-wide significance, suggestive of weaker effects when these loci are considered in isolation. Effect estimates of variants associated with the traits adjusted for BMI should be interpreted with caution, as suggested by a recent study which showed that estimates of variants identified in GWAS for traits adjusted for a covariate that is heritable can be biased, relative to the true direct effect on the trait.91 To illustrate this bias, the authors conducted a GWAS of WHR, BMI and WHRadjBMI and found that half of the reported associations with WHRadjBMI were likely influenced by a direct genetic association with BMI. The authors recommended avoiding such adjustment unless we know for certainty that the tested variant does not influence the covariate.91 Given the evidence of abundant pleiotropy among genes associated with complex traits,92 it is unlikely that a covariate such as BMI can fulfill that condition. In addition, it is important to remember that the genetic architecture underlying complex traits is often the result of joint interactions among multiple, weakly associated loci. Identification of these interactions can, therefore, provide additional insights into the bases of genetic susceptibilities. Among several methods, set-based techniques such as biological pathway analysis and interactome analysis93, 94, 95 have proven successful in identifying joint interactions that contribute significantly to diverse traits, including multiple sclerosis, cardiorespiratory fitness, cholesterol metabolism and lung cancer.96, 97, 98, 99 We have not examined such methods in the present study but plan on doing so in the future.
In conclusion, our study identified new loci influencing abdominal visceral (BBS9, ADCY8, KCNK9) and subcutaneous (MLLT10, DNAJC1, EBLN1) fat depots. We also confirmed in an independent cohort a previous association observed between the THNSL2 gene and visceral fat in women and replicated in our meta-analysis seven loci that were previously found to be associated with various measures of abdominal fat obtained by imaging as in the present study. Our results also highlight the importance of sex differences in the genetic architecture of body fat distribution.
References
Bouchard C, Bray GA, Hubbard VS . Basic and clinical aspects of regional fat distribution. Am J Clin Nutr 1990; 52: 946–950.
Matsuzawa Y, Shimomura I, Nakamura T, Keno Y, Tokunaga K . Pathophysiology and pathogenesis of visceral fat obesity. Ann N Y Acad Sci 1995; 748: 399–406.
Larsson B, Svardsudd K, Welin L, Wilhelmsen L, Bjorntorp P, Tibblin G . Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. Br Med J (Clin Res Ed) 1984; 288: 1401–1404.
Lapidus L, Bengtsson C, Larsson B, Pennert K, Rybo E, Sjostrom L . Distribution of adipose tissue and risk of cardiovascular disease and death: A 12 year follow up of participants in the population study of women in gothenburg, sweden. Br Med J (Clin Res Ed) 1984; 289: 1257–1261.
Kissebah AH, Vydelingum N, Murray R, Evans DJ, Hartz AJ, Kalkhoff RK et al. Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab 1982; 54: 254–260.
Vague J . The degree of masculine differentiation of obesities: A factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr 1956; 4: 20–34.
Després JP, Arsenault BJ, Côté M, Cartier A, Lemieux I . Abdominal obesity: The cholesterol of the 21st century? Can J Cardiol 2008; 24: 7D–12D.
Bouchard C . Genetic determinants of regional fat distribution. Hum Reprod 1997; 12: 1–5.
Bouchard C, Despres JP, Mauriege P . Genetic and nongenetic determinants of regional fat distribution. Endocr Rev 1993; 14: 72–93.
Pérusse L, Rice TK, Bouchard C . Evidence of a genetic component to obesity from genetic epidemiology. In: Bray GA, Bouchard C (eds). CRC Press: Boca Raton, FL, USA, 2013. pp 91–104.
Bouchard C, Pérusse L, Leblanc C, Tremblay A, Theriault G . Inheritance of the amount and distribution of human body fat. Int J Obes 1988; 12: 205–215.
Li Z, Rice T, Pérusse L, Bouchard C, Rao DC . Familial aggrgegation of subcutaneous fat patterning: Principal components of skinfolds in the quebec family study. Am J Hum Biol 1996; 8: 535–542.
Poulsen P, Vaag A, Kyvik K, Beck-Nielsen H . Genetic versus environmental aetiology of the metabolic syndrome among male and female twins. Diabetologia 2001; 44: 537–543.
Schousboe K, Visscher PM, Erbas B, Kyvik KO, Hopper JL, Henriksen JE et al. Twin study of genetic and environmental influences on adult body size, shape, and composition. Int J Obes Relat Metab Disord 2004; 28: 39–48.
Song Y, Lee K, Sung J, Lee D, Lee MK, Lee JY . Genetic and environmental relationships between framingham risk score and adiposity measures in koreans: The healthy twin study. Nutr Metab Cardiovasc Dis 2012; 22: 503–509.
Zhang S, Liu X, Yu Y, Hong X, Christoffel KK, Wang B et al. Genetic and environmental contributions to phenotypic components of metabolic syndrome: A population-based twin study. Obesity (Silver Spring) 2009; 17: 1581–1587.
Bayoumi RA, Al-Yahyaee SA, Albarwani SA, Rizvi SG, Al-Hadabi S, Al-Ubaidi FF et al. Heritability of determinants of the metabolic syndrome among healthy arabs of the oman family study. Obesity (Silver Spring) 2007; 15: 551–556.
Li JK, Ng MC, So WY, Chiu CK, Ozaki R, Tong PC et al. Phenotypic and genetic clustering of diabetes and metabolic syndrome in chinese families with type 2 diabetes mellitus. Diabetes Metab Res Rev 2006; 22: 46–52.
Lin HF, Boden-Albala B, Juo SH, Park N, Rundek T, Sacco RL . Heritabilities of the metabolic syndrome and its components in the northern manhattan family study. Diabetologia 2005; 48: 2006–2012.
Martin LJ, North KE, Dyer T, Blangero J, Comuzzie AG, Williams J . Phenotypic, genetic, and genome-wide structure in the metabolic syndrome. BMC Genet 2003; 4: S95.
Tang W, Hong Y, Province MA, Rich SS, Hopkins PN, Arnett DK et al. Familial clustering for features of the metabolic syndrome: The national heart, lung, and blood institute (nhlbi) family heart study. Diabetes Care 2006; 29: 631–636.
Wardle J, Carnell S, Haworth CM, Plomin R . Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am J Clin Nutr 2008; 87: 398–404.
Katzmarzyk PT, Malina RM, Perusse L, Rice T, Province MA, Rao DC et al. Familial resemblance in fatness and fat distribution. Am J Hum Biol 2000; 12: 395–404.
Pérusse L, Despres JP, Lemieux S, Rice T, Rao DC, Bouchard C . Familial aggregation of abdominal visceral fat level: Results from the quebec family study. Metabolism 1996; 45: 378–382.
Rice T, Despres JP, Daw EW, Gagnon J, Borecki IB, Perusse L et al. Familial resemblance for abdominal visceral fat: The heritage family study. Int J Obes Relat Metab Disord 1997; 21: 1024–1031.
Malis C, Rasmussen EL, Poulsen P, Petersen I, Christensen K, Beck-Nielsen H et al. Total and regional fat distribution is strongly influenced by genetic factors in young and elderly twins. Obes Res 2005; 13: 2139–2145.
Hsu FC, Lenchik L, Nicklas BJ, Lohman K, Register TC, Mychaleckyj J et al. Heritability of body composition measured by dxa in the diabetes heart study. Obes Res 2005; 13: 312–319.
Li X, Quinones MJ, Wang D, Bulnes-Enriquez I, Jimenez X, De La Rosa R et al. Genetic effects on obesity assessed by bivariate genome scan: The mexican-american coronary artery disease study. Obesity (Silver Spring) 2006; 14: 1192–1200.
Zillikens MC, Yazdanpanah M, Pardo LM, Rivadeneira F, Aulchenko YS, Oostra BA et al. Sex-specific genetic effects influence variation in body composition. Diabetologia 2008; 51: 2233–2241.
Pérusse L, Rice T, Province MA, Gagnon J, Leon AS, Skinner JS et al. Familial aggregation of amount and distribution of subcutaneous fat and their responses to exercise training in the heritage family study. Obes Res 2000; 8: 140–150.
Rice T, Hong Y, Perusse L, Despres JP, Gagnon J, Leon AS et al. Total body fat and abdominal visceral fat response to exercise training in the heritage family study: Evidence for major locus but no multifactorial effects. Metabolism 1999; 48: 1278–1286.
Bouchard C, Tremblay A, Despres JP, Nadeau A, Lupien PJ, Theriault G et al. The response to long-term overfeeding in identical twins. N Engl J Med 1990; 322: 1477–1482.
Bouchard C, Tremblay A, Despres JP, Theriault G, Nadeau A, Lupien PJ et al. The response to exercise with constant energy intake in identical twins. Obes Res 1994; 2: 400–410.
Bouchard C, Pérusse L, Rice T, Rao DC . The Genetics of Human Obesity. In: Bray GA, Bouchard C, James WPT (eds). Marcel Dekker Inc: New York, NY, USA, 1998. pp 157–190.
Bray MS, Hagberg JM, Perusse L, Rankinen T, Roth SM, Wolfarth B et al. The human gene map for performance and health-related fitness phenotypes: The 2006–2007 update. Med Sci Sports Exerc 2009; 41: 35–73.
den Hoed M, Loos RJ . Genes and the predisposition to obesity. In Bray GA, Bouchard C (eds), Hanbook of Obesity - Epidemiology, Etiology and Physiopathology. CRC Press: Boca Raton, FL, USA, 2013. pp 105–120.
Katzmarzyk PT, Perusse L, Bouchard C . Genetics of abdominal visceral fat levels. Am J Hum Biol 1999; 11: 225–235.
Lahiry P, Pollex RL, Hegele RA . Uncloaking the genetic determinants of metabolic syndrome. J Nutrigenet Nutrigenomics 2008; 1: 118–125.
Teran-Garcia M, Bouchard C . Genetics of the metabolic syndrome. Appl Physiol Nutr Metab 2007; 32: 89–114.
Rudkowska I, Pérusse L . Individualized weight management: What can be learned from nutrigenomics and nutrigenetics? Prog Mol Biol Transl Sci 2012; 108: 347–382.
Heid IM, Jackson AU, Randall JC, Winkler TW, Qi L, Steinthorsdottir V et al. Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals sexual dimorphism in the genetic basis of fat distribution. Nat Genet 2010; 42: 949–960.
Heard-Costa NL, Zillikens MC, Monda KL, Johansson A, Harris TB, Fu M et al. Nrxn3 is a novel locus for waist circumference: a genome-wide association study from the charge consortium. PLoS Genet 2009; 5: e1000539.
Lindgren CM, Heid IM, Randall JC, Lamina C, Steinthorsdottir V, Qi L et al. Genome-wide association scan meta-analysis identifies three loci influencing adiposity and fat distribution. PLoS Genet 2009; 5: e1000508.
Cho YS, Go MJ, Kim YJ, Heo JY, Oh JH, Ban HJ et al. A large-scale genome-wide association study of asian populations uncovers genetic factors influencing eight quantitative traits. Nat Genet 2009; 41: 527–534.
Berndt SI, Gustafsson S, Magi R, Ganna A, Wheeler E, Feitosa MF et al. Genome-wide meta-analysis identifies 11 new loci for anthropometric traits and provides insights into genetic architecture. Nat Genet 2013; 45: 501–512.
Liu CT, Monda KL, Taylor KC, Lange L, Demerath EW, Palmas W et al. Genome-wide association of body fat distribution in african ancestry populations suggests new loci. PLoS Genet 2013; 9: e1003681.
Shungin D, Winkler TW, Croteau-Chonka DC, Ferreira T, Locke AE, Magi R et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature 2015; 518: 187–196.
Fox CS, Liu Y, White CC, Feitosa M, Smith AV, Heard-Costa N et al. Genome-wide association for abdominal subcutaneous and visceral adipose reveals a novel locus for visceral fat in women. PLoS Genet 2012; 8: e1002695.
Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR Jr et al. Cardia: Study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988; 41: 1105–1116.
Borecki IB, Rice T, Pérusse L, Bouchard C, Rao DC . Major gene influence on the propensity to store fat in trunk versus extremity depots: Evidence from the quebec family study. Obes Res 1995; 3: 1–8.
Bouchard C . Bray GA, Ryan DH . Genetic Epidemiologu, Association, and Sib-pair Linkage: Results from the Quebec Family Study. 5th edn. Louisiana State University Press: Baton Rouge, LA, USA, 1996, pp 470–481.
Hill JO, Sidney S, Lewis CE, Tolan K, Scherzinger AL, Stamm ER . Racial differences in amounts of visceral adipose tissue in young adults: The cardia (coronary artery risk development in young adults) study. Am J Clin Nutr 1999; 69: 381–387.
Ferland M, Despres JP, Tremblay A, Pinault S, Nadeau A, Moorjani S et al. Assessment of adipose tissue distribution by computed axial tomography in obese women: Association with body density and anthropometric measurements. Br J Nutr 1989; 61: 139–148.
Li Y, Willer CJ, Ding J, Scheet P, Abecasis GR . Mach: Using sequence and genotype data to estimate haplotypes and unobserved genotypes. Genet Epidemiol 2010; 34: 816–834.
Willer CJ, Li Y, Abecasis GR . Metal: Fast and efficient meta-analysis of genomewide association scans. Bioinformatics 2010; 26: 2190–2191.
Katzmarzyk PT, Bray GA, Greenway FL, Johnson WD, Newton RL Jr., Ravussin E et al. Racial differences in abdominal depot-specific adiposity in white and african american adults. Am J Clin Nutr 2010; 91: 7–15.
Katzmarzyk PT, Greenway FL, Heymsfield SB, Bouchard C . Clinical utility and reproducibility of visceral adipose tissue measurements derived from dual-energy x-ray absorptiometry in white and african american adults. Obesity (Silver Spring) 2013; 21: 2221–2224.
Katzmarzyk PT, Heymsfield SB, Bouchard C . Clinical utility of visceral adipose tissue for the identification of cardiometabolic risk in white and african american adults. Am J Clin Nutr 2013; 97: 480–486.
Wigginton JE, Abecasis GR . Pedstats: Descriptive statistics, graphics and quality assessment for gene mapping data. Bioinformatics 2005; 21: 3445–3447.
Liekens AM, De Knijf J, Daelemans W, Goethals B, De Rijk P, Del-Favero J . Biograph: Unsupervised biomedical knowledge discovery via automated hypothesis generation. Genome Biol 2011; 12: R57.
Bornigen D, Tranchevent LC, Bonachela-Capdevila F, Devriendt K, De Moor B, De Causmaecker P et al. An unbiased evaluation of gene prioritization tools. Bioinformatics 2012; 28: 3081–3088.
Price AL, Zaitlen NA, Reich D, Patterson N . New approaches to population stratification in genome-wide association studies. Nat Rev Genet 2010; 11: 459–463.
Alexopoulos N, Katritsis D, Raggi P . Visceral adipose tissue as a source of inflammation and promoter of atherosclerosis. Atherosclerosis 2014; 233: 104–112.
Mathieu P, Boulanger MC, Despres JP . Ectopic visceral fat: A clinical and molecular perspective on the cardiometabolic risk. Rev Endocr Metab Disord 2014; 15: 289–298.
Kloting N, Bluher M . Adipocyte dysfunction, inflammation and metabolic syndrome. Rev Endocr Metab Disord 2014; 15: 277–287.
Nachury MV, Loktev AV, Zhang Q, Westlake CJ, Peranen J, Merdes A et al. A core complex of bbs proteins cooperates with the gtpase rab8 to promote ciliary membrane biogenesis. Cell 2007; 129: 1201–1213.
Nishimura DY, Swiderski RE, Searby CC, Berg EM, Ferguson AL, Hennekam R et al. Comparative genomics and gene expression analysis identifies bbs9, a new bardet-biedl syndrome gene. Am J Hum Genet 2005; 77: 1021–1033.
Veleri S, Bishop K, Dalle Nogare DE, English MA, Foskett TJ, Chitnis A et al. Knockdown of bardet-biedl syndrome gene bbs9/pthb1 leads to cilia defects. PLoS One 2012; 7: e34389.
Seo S, Guo DF, Bugge K, Morgan DA, Rahmouni K, Sheffield VC . Requirement of bardet-biedl syndrome proteins for leptin receptor signaling. Hum Mol Genet 2009; 18: 1323–1331.
Benzinou M, Walley A, Lobbens S, Charles MA, Jouret B, Fumeron F et al. Bardet-biedl syndrome gene variants are associated with both childhood and adult common obesity in french caucasians. Diabetes 2006; 55: 2876–2882.
Wheeler E, Huang N, Bochukova EG, Keogh JM, Lindsay S, Garg S et al. Genome-wide snp and cnv analysis identifies common and low-frequency variants associated with severe early-onset obesity. Nat Genet 2013; 45: 513–517.
Pinnick KE, Nicholson G, Manolopoulos KN, McQuaid SE, Valet P, Frayn KN et al. Distinct developmental profile of lower-body adipose tissue defines resistance against obesity-associated metabolic complications. Diabetes 2014; 63: 3785–3797.
Tchkonia T, Thomou T, Zhu Y, Karagiannides I, Pothoulakis C, Jensen MD et al. Mechanisms and metabolic implications of regional differences among fat depots. Cell Metab 2013; 17: 644–656.
Karpe F, Pinnick KE . Biology of upper-body and lower-body adipose tissue-link to whole-body phenotypes. Nat Rev Endocrinol 2014; 11: 90–100.
Gesta S, Bluher M, Yamamoto Y, Norris AW, Berndt J, Kralisch S et al. Evidence for a role of developmental genes in the origin of obesity and body fat distribution. Proc Natl Acad Sci USA 2006; 103: 6676–6681.
Randall JC, Winkler TW, Kutalik Z, Berndt SI, Jackson AU, Monda KL et al. Sex-stratified genome-wide association studies including 270,000 individuals show sexual dimorphism in genetic loci for anthropometric traits. PLoS Genet 2013; 9: e1003500.
Hotta K, Kitamoto A, Kitamoto T, Mizusawa S, Teranishi H, So R et al. Replication study of 15 recently published loci for body fat distribution in the japanese population. J Atheroscler Thromb 2013; 20: 336–350.
Hotta K, Nakamura M, Nakamura T, Matsuo T, Nakata Y, Kamohara S et al. Polymorphisms in nrxn3, tfap2b, msra, lyplal1, fto and mc4r and their effect on visceral fat area in the japanese population. J Hum Genet 2010; 55: 738–742.
Hotta K, Kitamoto A, Kitamoto T, Mizusawa S, Teranishi H, So R et al. Association between type 2 diabetes genetic susceptibility loci and visceral and subcutaneous fat area as determined by computed tomography. J Hum Genet 2012; 57: 305–310.
Hotta K, Kitamoto T, Kitamoto A, Mizusawa S, Matsuo T, Nakata Y et al. Computed tomography analysis of the association between the sh2b1 rs7498665 single-nucleotide polymorphism and visceral fat area. J Hum Genet 2011; 56: 716–719.
Hotta K, Kitamoto A, Kitamoto T, Mizusawa S, Teranishi H, Matsuo T et al. Genetic variations in the cyp17a1 and nt5c2 genes are associated with a reduction in visceral and subcutaneous fat areas in japanese women. J Hum Genet 2012; 57: 46–51.
Kitamoto A, Kitamoto T, Mizusawa S, Teranishi H, So R, Matsuo T et al. Nudt3 rs206936 is associated with body mass index in obese japanese women. Endocr J 2013; 60: 991–1000.
Hsiao TJ, Hwang Y, Liu CH, Chang HM, Lin E . Association of the c825t polymorphism in the gnb3 gene with obesity and metabolic phenotypes in a taiwanese population. Genes Nutr 2013; 8: 137–144.
Goldlust IS, Hermetz KE, Catalano LM, Barfield RT, Cozad R, Wynn G et al. Mouse model implicates gnb3 duplication in a childhood obesity syndrome. Proc Natl Acad Sci USA 2013; 110: 14990–14994.
Ko KD, Kim KK, Suh HS, Hwang IC . Associations between the gnb3 c825t polymorphism and obesity-related metabolic risk factors in korean obese women. J Endocrinol Invest 2014; 37: 1117–1120.
Meadows HJ, Randall AD . Functional characterisation of human task-3, an acid-sensitive two-pore domain potassium channel. Neuropharmacology 2001; 40: 551–559.
Beloeil H, Ababneh Z, Chung R, Zurakowski D, Mulkern RV, Berde CB . Effects of bupivacaine and tetrodotoxin on carrageenan-induced hind paw inflammation in rats (part 1): Hyperalgesia, edema, and systemic cytokines. Anesthesiology 2006; 105: 128–138.
Block L, Jorneberg P, Bjorklund U, Westerlund A, Biber B, Hansson E . Ultralow concentrations of bupivacaine exert anti-inflammatory effects on inflammation-reactive astrocytes. Eur J Neurosci 2013; 38: 3669–3678.
Gordon SM, Chuang BP, Wang XM, Hamza MA, Rowan JS, Brahim JS et al. The differential effects of bupivacaine and lidocaine on prostaglandin e2 release, cyclooxygenase gene expression and pain in a clinical pain model. Anesth Analg 2008; 106: 321–327, table of contents.
El Hachmane MF, Rees KA, Veale EL, Sumbayev VV, Mathie A . Enhancement of twik-related acid-sensitive potassium channel 3 (task3) two-pore domain potassium channel activity by tumor necrosis factor alpha. J Biol Chem 2014; 289: 1388–1401.
Aschard H, Vilhjalmsson BJ, Joshi AD, Price AL, Kraft P . Adjusting for heritable covariates can bias effect estimates in genome-wide association studies. Am J Hum Genet 2015; 96: 329–339.
Sivakumaran S, Agakov F, Theodoratou E, Prendergast JG, Zgaga L, Manolio T et al. Abundant pleiotropy in human complex diseases and traits. Am J Hum Genet 2011; 89: 607–618.
Zhang K, Chang S, Cui S, Guo L, Zhang L, Wang J . Icsnpathway: Identify candidate causal snps and pathways from genome-wide association study by one analytical framework. Nucleic Acids Res 2011; 39: W437–W443.
Cantor RM, Lange K, Sinsheimer JS . Prioritizing gwas results: A review of statistical methods and recommendations for their application. Am J Hum Genet 2010; 86: 6–22.
Wang K, Li M, Hakonarson H . Analysing biological pathways in genome-wide association studies. Nat Rev Genet 2010; 11: 843–854.
Ghosh S, Vivar JC, Sarzynski MA, Sung YJ, Timmons JA, Bouchard C et al. Integrative pathway analysis of a genome-wide association study of vo2max response to exercise training. J Appl Physiol (1985) 2013; 115: 1343–1359.
Fehringer G, Liu G, Briollais L, Brennan P, Amos CI, Spitz MR et al. Comparison of pathway analysis approaches using lung cancer gwas data sets. PLoS One 2012; 7: e31816.
International Multiple Sclerosis Genetics C. Network-based multiple sclerosis pathway analysis with gwas data from 15,000 cases and 30,000 controls. Am J Hum Genet 2013; 92: 854–865.
Wang K, Edmondson AC, Li M, Gao F, Qasim AN, Devaney JM et al. Pathway-wide association study implicates multiple sterol transport and metabolism genes in hdl cholesterol regulation. Front Genet 2011; 2: 41.
Acknowledgements
We thank Mrs Allison Templet and Mrs Robin Post for their support in the development and submission of this manuscript. The Quebec Family Study (QFS) was supported for three decades by multiple grants from the Medical Research Council of Canada and the Canadian Institutes for Health Research. This project was supported by a team grant from the Canadian Institute for Health Research (FRCN-CCT-83028). We thank all PIs who contributed to the HERITAGE Family Study in the past via support from the National Heart, Lung, and Blood Institute (NHLBI) through the following grants: C Bouchard (HL-45670); AS Leon (HL-47323); DC Rao (HL-47317); JS Skinner (HL-47327); JH Wilmore (HL-47321). We also acknowledge grant 8P20 GM-1033528 (COBRE center grant to Pennington Biomedical Research Center, PI: Thomas Gettys, supporting M.A. Sarzynski). The Pennington Center Longitudinal Study is partially supported by a Nutrition Obesity Research Center (NIH 2P30DK072476) grant from the National Institutes of Health and by 1 U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health which funds the Louisiana Clinical and Translational Science Center. The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the NHLBI in collaboration with the University of Alabama at Birmingham (HHSN268201300025C and HHSN268201300026C), Northwestern University (HHSN268201300027C), University of Minnesota (HHSN268201300028C), Kaiser Foundation Research Institute (HHSN268201300029C), and Johns Hopkins University School of Medicine (HHSN268200900041C). CARDIA is also partially supported by the Intramural Research Program of the National Institute on Aging (NIA) and an intra-agency agreement between NIA and NHLBI (AG0005). This manuscript has been reviewed by CARDIA for scientific content. The CARDIA CT Scan year 25 data were obtained with the support of NHLBI (R01-HL-098445). C. Bouchard is partially funded by the John W. Barton Sr. Chair in Genetics and Nutrition.
Disclaimer
The funders had no role in the study design, data collection, decision to publish, or preparation of the manuscript. The funding agencies had no role in the design of the present study, collection and analysis of the data and the decision to publish. None of the authors are employed by institutions that stand to gain or lose financially as a result of this publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Sung, Y., Pérusse, L., Sarzynski, M. et al. Genome-wide association studies suggest sex-specific loci associated with abdominal and visceral fat. Int J Obes 40, 662–674 (2016). https://doi.org/10.1038/ijo.2015.217
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.217
- Springer Nature Limited
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.