Abstract
Background:
Young obese youth are generally stronger than lean youth. This has been linked to the loading effect of excess body mass, acting as a training stimulus comparable to strength training. Whether this triggers specific adaptations of the muscle architecture (MA) and voluntary activation (VA) that could account for the higher strength of obese subjects remains unknown.
Methods:
MA characteristics (that is, pennation angle (PA), fascicle length (FL) and muscle thickness (MT)) and muscle size (that is, anatomical cross-sectional area (ACSA)) of the knee extensor (KE) and plantar flexor (PF) muscles were evaluated in 12 obese and 12 non-obese adolescent girls (12–15 years). Maximal isometric torque and VA of the KE and PF muscles were also assessed.
Results:
Results revealed higher PA (P<0.05), greater MT (P<0.001), ACSA (P<0.01), segmental lean mass (P<0.001) and VA (P<0.001) for KE and PF muscles in obese girls. Moreover, obese individuals produced a higher absolute torque than their lean counterparts on the KE (224.6±39.5 vs 135.7±32.7 N m, respectively; P<0.001) and PF muscles (73.3±16.5 vs 44.5±6.2 N m; P<0.001). Maximal voluntary contraction (MVC) was correlated to PA for the KE (r=0.46–0.57, P<0.05–0.01) and PF muscles (r=0.45–0.55, P<0.05–0.01). MVC was also correlated with VA (KE: r=0.44, P<0.05; PF: r=0.65, P<0.001) and segmental lean mass (KE: r=0.48, P<0.05; PF: r=0.57, P<0.01).
Conclusions:
This study highlighted favorable muscular and nervous adaptations to obesity that account for the higher strength of obese youth. The excess of body mass supported during daily activities could act as a chronic training stimulus responsible for these adaptations.
Similar content being viewed by others
Introduction
One major feature of the neuromuscular system is its adaptability in response to endogenous and exogenous influences, such as changes in loading regimens.1, 2 Thus, the skeletal muscle has an important degree of plasticity that translates into adjustments of its anatomical and functional properties.2, 3 For instance, increased mitochondrial volume has been associated with endurance training,4 whereas the amount of contractile proteins may increase in response to growth5 or strength training (ST),6 a phenomenon known as muscle hypertrophy. Besides muscle mass, muscle architecture (MA) also presents a certain degree of plasticity.5 MA is defined as the geometrical arrangement of muscle fibers relative to the axis of force generation.7 The most common parameters assessed to define MA are the muscle fascicle length (FL), muscle thickness (MT) and the pennation angle (PA), which is defined as the angle between the fascicles and the deep aponeurosis. These MA parameters are important determinants of the strength capacity besides the neural and muscular factors.3, 8 Consequently, they are considered as good predictors of the contractile properties of skeletal muscles,7, 8, 9 and have been used to evaluate the force production capacities of the muscle–tendon complex.2, 10 MA can adapt to ST,3, 8 growth11 or ageing.12 Moreover, certain pathological conditions such as neuromuscular disorders (for example, inflammatory myopathies or dystrophies) can also modify the MA characteristics.13, 14 Surprisingly, less attention has been paid to the impact of obesity on MA characteristics. Yet, the important mechanical overload associated with excess body mass and the negative effect of obesity on muscle hypertrophy15 may trigger specific adaptations of the MA properties in obese individuals.
Although the excess of fat mass may limit functional abilities in obese people,16 it generates a mechanical overload that could act as a chronic training stimulus generating positive neuromuscular adaptations, especially during childhood.16 Indeed, muscle morphology and strength production capacity adapt quickly to the functional demand and increased body dimensions during growth in typically developing children.17, 18 In obese girls and boys, higher absolute knee extensor (KE) force values have been reported compared with non-obese.19, 20, 21, 22 This has been ascribed to a greater total fat-free mass in obese (for example, Tsiros et al.22), but also to a higher relative force (that is, normalized to segmental muscle mass).19
This higher specific force may relate to nervous factors, such as a higher muscle voluntary activation (VA) level, or to muscular factors, such as adaptations of the MA, in order to increase the physiological cross-sectional area. The effect of obesity on the VA is scarcely described. Given the constant mechanical loading underwent by the lower limb muscles, one would expect an increased VA in obese subjects to cope with the mechanical stress, as observed after a ST program in healthy subjects (for example, Gondin et al.23). However, only one study evaluated the VA in obese subjects and reported a lower VA of the KE muscles in the obese group.24 However, the force production capacity did not differ between lean and obese adolescents, suggesting that at equivalent VA, obese adolescents would have produced a higher force than their healthy counterparts. This could point out to a specific adaptation to obesity within the skeletal muscle.
To date, the impact of obesity on the regulation of muscle mass and architecture is poorly understood. Increased total fat-free mass is frequently observed in obese preadolescent and adolescent,19, 21, 22 but this variable does not exclusively reflect the contractile tissue.19, 21, 22, 24 Only one study has studied the effect of obesity on the lower limb muscles hypertrophy and found a comparable KE anatomical cross-sectional area (ACSA) in obese compared with non-obese adolescents.24 This is consistent with the results of Sitnick et al.,15 who reported a negative effect of obesity on skeletal muscle hypertrophy on an animal model. Therefore, the only way to increase force production to cope with the mechanical overload would be the adaptation of the MA, and specifically an increase of the PA in order to increase the muscle physiological cross-sectional area. Such adaptation has already been observed in response to artificial loading, that is, ST, in healthy adults subjects (for example, Aagaard et al.25). Whether this occurs in response to obesity remains unknown.
Therefore, the purpose of this study was to assess the effect of obesity on the VA and MA. We formulated the hypothesis that the excess of body mass supported by obese people could act as a chronic training stimulus generating favorable MA (for example, increased PA) and VA adaptations but no hypertrophy (for example, comparable ACSA and MT) compared with non-obese subjects. We verified this assumption in obese adolescent girls. The rationale for this choice was that (i) puberty is a favorable period in terms of muscle plasticity;5 (ii) side effects of obesity on the skeletal muscle, such as fat infiltration, increased connective tissue and low-grade inflammation, which could bias the evaluation of MA, are generally less present during adolescence compared with adulthood;26, 27 (iii) the prevalence and incidence of obesity among adolescents are progressively increasing worldwide, and concomitantly the level of physical activity gradually decreases in adolescent girls28 and (iv) adolescent girls have a reduced potential for muscle hypertrophy,29, 30 which should favor adaptations of the VA and MA.
Materials and methods
Subjects
Twelve obese and 12 non-obese adolescent girls (12–15 years) volunteered to participate. Obese subjects were recruited in a children’s medical center, and non-obese from a secondary school. They were classified as obese and non-obese according to the International Obesity Task Force criteria.31 Body mass index data were collected from birth to the time of inclusion in the study in obese adolescent girls. According to the body mass index history, they became obese when they were 6.1±1.0 years old.
Groups were formed so that chronological age, biological age, height and maturity status were not significantly different (Table 1). All the subjects performed recreational physical activity for ⩽4 h per week and none of them was involved in any vigorous physical activity. The level of physical activity (that is, variety of physical activities, intensity and sedentary-level scores) was determined from a questionnaire validated among French children and adolescents.32 This study was approved by the local ethics committee (CPP Sud-Est VI; authorization number AU994). All the participants and their parents/guardians were informed of the experimental procedures and gave their written consent before any testing was conducted.
Design
Three experimental sessions (separated by 1 week), were organized. The first session was dedicated to the clinical examination by a pediatrician, the collection of subject characteristics and the familiarization with the experimental procedures. The second session was devoted to the measurement of MA (for the KE and plantar flexor (PF) muscles) and KE neuromuscular properties. The PF neuromuscular properties were assessed during the last visit.
Subjects characteristics
Anthropometrical measurements and body composition analysis
Body mass was measured to the nearest 0.1 kg using a calibrated scale and height and sitting height were determined to the nearest 0.01 m using a standing stadiometer. Body mass index was computed as mass divided by height squared (kg m−2). In order to normalize the positioning of the ultrasound (US) probe for MA measurements, thigh and leg lengths were used as references and measured using anatomical landmarks according to Kubo’s et al. procedures.12
Body fat and fat-free mass were determined using dual-energy X-ray absorptiometry (HOLOGIC, QDR-4500, Hologic Inc., Bedford, MA, USA). The dual-energy X-ray absorptiometry measurements were performed in supine position. Thigh and leg lean mass were measured as described by Skalsky et al.33
Maturation assessment
Tanner stages were determined from self-assessment of pubic hair and breast development.34 The children were assisted by their parents or a pediatrician while completing the questionnaire. The age from peak height velocity was used to assess somatic maturity and determined by using height, sitting height and body mass.35
Metabolic indexes
In order to discard any potential effect of metabolic disorders on MA and VA, the metabolic and inflammatory profiles were assessed. In fasting conditions, venous blood samples were withdrawn from a prominent superficial vein in the antecubital fossa. Glucose, triglycerides, total cholesterol, high-density lipoprotein cholesterol, calculated low-density lipoprotein cholesterol, and C-reactive protein were analyzed (Konelab, Vantaa, Finland). Insulin hormone was measured with enzyme-linked immunosorbent assay. Insulin sensitivity was assessed with the homeostasis model assessment–insulin resistance.36
Muscle architecture
In vivo MA characteristics of the right KE and PF muscles were achieved using B-mode real-time US scanner (Echo Blaster 128 CEXT-1Z, Telemed Ltd, Vilnius, Lithuania) with a linear array transducer (width: 59 mm; frequency range: 5–10 MHz). More specifically, rectus femoris, vastus lateralis and vastus medialis were analyzed for the KE and gastrocnemius lateralis and gastrocnemius medialis for the PF muscles. MA of the vastus intermedius and soleus muscles were difficult to determine in obese individuals, owing to the thickness of the subcutaneous adipose tissue that compromised the spatial resolution of US. They were not reported here. All measurements were performed after the subjects had laid in the supine position for at least 20 min to allow fluid shift to occur.37 Scans of the KE muscles were taken distally with the knees fully extended at 66% of the thigh length.38 For PF measurements, subjects laid in prone position with the ankles maximally plantar-flexed. Scans were taken proximally at 33% of the leg length.39 The US probe was coated with a water-soluble transmission gel (Aquasonic, Parker Laboratory, Fairfield, NJ, USA) to improve acoustic coupling. Probe alignment was considered correct when muscle fascicles and aponeurosis could be delineated without interruption across the image. All US scans were performed by the same investigator.
The average of the three consecutive scans was taken for each muscle and was used for the subsequent analysis. Images were analyzed off-line using the ImageJ software (version 1.42, National Institute of health, Bethesda, MA, USA). MT and PA were assessed by positioning the US probe parallel to the muscle fascicles while applying a minimal but constant pressure on the probe, to avoid compression of the muscles and subcutaneous fat tissue. For every muscle, MT (mm) and PA (°) (Figure 1a) were calculated and defined according to Binzoni et al.5 method. FL was calculated as follows:39

Cross-sectional images of the KE and PF muscles were also obtained by positioning the probe in the axial plane. The probe was moved manually with slow and continuous movement from the lateral to the medial side along a line marked on the skin, to generate 'panoramic' images of the muscles (InVivo ScanNT 3.6 software, Medcom, Telemed Ltd). The ACSA of each muscle was determined off-line (Figure 1b).
The intra-rater reliability of the MA characteristics was evaluated in a subsample of seven obese adolescent girls on two consecutive occasions, 7 days apart, in an additional experiment. This subsample had anthropometric characteristics and body composition similar to the experimental group. This analysis revealed a good reliability for most of the variables (Supplementary material 1).
Neuromuscular function
Isometric maximal voluntary contraction (MVC) torque was assessed with an isokinetic dynamometer (Cybex Norm, Lumex, Ronkonkoma, NY, USA). Data were acquired and digitized on-line at a rate of 2 kHz (Powerlab 8/35, ADInstruments, New South Wales, Australia). The participants performed three 5 s MVCs of the KE and PF muscles with at least 60 s of rest between efforts. Visual feedback and verbal encouragements were provided to maximize torque output. For KE MVC, subjects sat comfortably on an adjustable dynamometer chair with the hip joint set at 30° (0°=full supine position). The dynamometer lever arm was attached to the right leg by a strap positioned 1−2 cm above the lateral malleolus. For PF MVC, subjects laid prone, the right foot attached to the dynamometer. Torque was measured at a knee joint angle of 90° (0°=full extension) for KE MVC. Ankle angle was set at 90° and the knee angle at 0° for PF MVC. For each MVC procedure, the dynamometer axis of rotation was aligned with the joint axis of rotation. Absolute torque was determined as the peak force reached during maximal efforts.
MVCs were superimposed with single magnetic stimulations (Magstim 2002, MagstimCo, Whiteland, Dyfed, UK) to determine the VA of the KE and PF muscles with the twitch interpolation technique.40 The 70-mm figure-of-eight coil (peak magnetic field strength 2.04 T, stimulation duration 0.1 ms; MagstimCo) was placed in regard of the femoral nerve in the femoral triangle for the KE muscles, and in regard of the posterior tibial nerve on the posterior aspect of the knee for the PF muscles. Stimulations were delivered at supramaximal intensity, that is, 100% of the stimulator output. This intensity corresponded to 125% and 118% of the optimal intensity (that is, the intensity allowing the complete recruitment of the motor units, as assessed from the plateauing of the evoked torque) for the PF and KE muscles, respectively (for full details of the stimulation procedures, see Kluka et al.41).
Finally, the specific torque was calculated as the absolute torque divided by segmental lean mass (N m kg−1).
Statistical analysis
All the values are reported as mean±s.d. The Shapiro–Wilk test was used to verify data normality. Student's t-tests for unpaired samples were then used to compare VA, MT, PA, FL, ACSA, absolute and relative MVC and anthropometrical characteristics between obese and non-obese adolescents. The statistical power was also calculated for each comparison (Supplementary material 1). Tanner stages and the scores of physical activity were compared using a Chi-squared test. Pearson product correlation was used to determine the linear relation between MVC and each of the following variables: PA, VA and segmental lean mass (pooled data). For all statistical tests, the limit for statistical significance was set at P<0.05.
Results
Participant characteristics
As expected, the obese adolescent girls showed significantly higher values for body mass, body mass index, fat-free mass and body fat (P<0.001; Table 1) and also displayed higher thigh lean mass than non-obese girls (6.4±0.8 vs 4.3±0.3 kg, respectively; P<0.001) and leg lean mass (2.0±0.2 vs 1.6±0.3 kg; P<0.001).
No significant difference was observed between groups for chronological age, height, Tanner stages, age from peak height velocity, time from age from peak height velocity and physical activity scores (Table 1). All metabolic indexes fell within the normal ranges for this age and sex (Table 2).
MA parameters and muscle size
For each muscle of the KE (vastus lateralis, rectus femoris and vastus medialis) and PF (gastrocnemius lateralis and medialis), MT (P<0.001), PA (P<0.05–P<0.001) and ACSA (P<0.01–P<0.001, gastrocnemius lateralis excepted; Figure 2) were significantly higher in obese than in non-obese girls. Conversely, FL values were not significantly different between groups for the rectus femoris (86.7±12.5 vs 95.8±26.9 mm for obese and non-obese, respectively), vastus lateralis (74.4±10.8 vs 67.5±16.9 mm), vastus medialis (110.9±26.7 vs 96.3±29.8 mm), gastrocnemius medialis (39.5±7.3 vs 42.5±9.6 mm) and lateralis (50.4 ±10.6 vs 47.1±8.4 mm) muscles. US images for typical obese and non-obese individuals are presented in Supplementary material 2.
VA level
VA was significantly higher in obese compared with non-obese girls for KE and PF muscles (P<0.001; Figure 3).
Voluntary isometric torque
As expected, absolute MVC torque was significantly higher in obese than non-obese for the KE and PF muscles (P<0.001; Figure 4a). Obese subjects also displayed higher specific torque values than non-obese girls for the PF (P<0.05), but not for the KE muscles (Figure 4b).
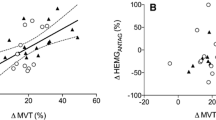
Correlations
KE MVC was correlated to PA for the rectus femoris (r=0.57, P<0.01) and vastus lateralis muscles (r=0.46, P<0.05), but not for the vastus medialis muscle (r=0.32, P=0.13). KE MVC was also correlated to VA (r=0.44, P<0.05) and segmental lean mass (r=0.48, P<0.05).
PF MVC was correlated to PA for the gastrocnemius medialis (r=0.55, P<0.01) and lateralis (r=0.45, P<0.05) muscles. PF MVC was also correlated to VA (r=0.65, P<0.001) and segmental lean mass (r=0.57, P<0.01).
Discussion
The purpose of this study was to assess the effect of obesity on VA and MA and their relation with strength production capacity in adolescent girls. We hypothesized that the excess of body mass supported by obese youth could act as a chronic training stimulus generating favorable MA adaptations (for example, higher PA) but no hypertrophy (for example, comparable ACSA or MT). The results partly support this hypothesis. Indeed, we observed higher PA on all the KE and PF muscles but a greater muscle size (represented by the MT, ACSA and the segmental lean mass) in obese compared with non-obese adolescent girls. Moreover, obese individuals had a higher VA of the KE and PF muscle groups. These muscular and nervous adaptations were associated with a higher absolute (on KE and PF muscles) and specific (only on PF muscles) isometric torque in obese compared with lean subjects.
MA differences
It has been widely reported that ST, a paradigm of chronic overloading of the skeletal muscle, results in favorable MA modifications (~ +11 to 33% for PA and +9 to 14% for MT) within the lower limb muscles of healthy subjects.6, 23, 25, 42 During the training phase, any increase of the muscle ACSA translates into an increase of MT. An increased PA further enlarges the physiological cross-sectional area. All these adaptations are aimed at increasing the force production capacity to cope with the mechanical load placed on the skeletal muscle. It is likely that the same phenomenon accounts for the PA, MT and ACSA differences between obese and non-obese adolescent girls. Although chronically loading the lower limb muscles, the excess body mass could act as a training stimulus in obese subjects. The MA differences between obese and non-obese girls reported here seem to be similar (+20% for PA) or enhanced (+30 to 50% for MT) compared with the effect of ST programs. However, the duration of exposure to mechanical overload differ greatly between ST and obesity. Healthy subjects involved in the above-mentioned ST programs trained ~2–4 times per week over short periods (8–21 weeks), whereas our obese subjects had been 'carrying' excess body mass daily for ~6–9 years. Thus, the longer exposure to overloading certainly accounts for the discrepancy between our findings and the effects of short-term ST programs in healthy subjects.
The increased MT and ACSA were nevertheless unexpected. Indeed, adolescent girls have a reduced potential for hypertrophy as compared with boys.29, 30 This potential may be further reduced in obese subjects. Indeed, Sitnick et al.15 demonstrated on an animal model that obesity impairs the ability of skeletal muscle to hypertrophy in response to increased mechanical load. This has been attributed to a failure to activate the Akt/mTOR signaling pathway. Recently, Williamson et al.43 also demonstrated that obese mice had elevated REDD1 expression that coincided with aberrant Akt/mTOR signaling. Nevertheless, our obese subjects demonstrated a significant muscle hypertrophy as compared with lean girls. As our obese subjects were free from metabolic disorders, it is thus suggested that the potential inhibitory effect of obesity on muscle hypertrophy was lacking, or too weak to counteract the positive effect of mechanical loading on muscle hypertrophy. In addition, we cannot exclude the possibility that the obese girls suffered from hyperandrogenemia,44 which could have contributed to the observed muscle hypertrophy.
Interestingly, the obese subjects had increased PA and MT but comparable FL. This is quite consistent with the lack of effect of ST on FL in healthy subjects. Only few studies reported FL modifications after ST programs, such that the reality of this adaptation remains controversial.6, 42 FL has an important role in determining the force–length properties of a muscle,45 and specifically the maximum shortening velocity.46 As mentioned earlier, enhanced MT and PA increase the force production capacity of the muscle. However, any increase of PA and MT without any change of the FL reduces the effective contractile force exerted longitudinally onto the aponeurosis.25 This may translate into a reduced shortening of the aponeurosis and thus, into a reduced shortening velocity of the muscle–tendon unit. Therefore, it seems that in obese subjects, the skeletal muscle adapts principally to increase its force production capacity to cope with the mechanical overload, but this adaptation could have detrimental effects on the muscle contraction velocity. This could contribute to their poor motor performance.20
Implication for strength differences
It has been widely demonstrated that obese adolescents produce more force and power than lean adolescents.19, 20, 21, 22 This has often been related to a higher total fat-free mass.20, 21 However, the evidence for a higher muscle mass or ACSA in obese adolescents is currently lacking.19, 24 Our results show that most of the KE and PF muscles (gastrocnemius lateralis excepted) had an increased ACSA in obese adolescent girls. This was associated with a higher segmental lean mass, which may contribute to the higher force production capacity of obese subjects, as evidenced by the correlation between segmental lean mass and MVC torque. In addition, the significant correlation between PA and MVC suggests that MA could also account for the greater force production capacity of obese subjects. This is consistent with the studies that demonstrated concomitant increases in voluntary force, muscle dimensions and architecture after a ST program (for example, Aagaard et al.25).
Beyond adaptations at the muscular level, our results reveal that nervous factors also contribute to the higher force production capacity of the obese subjects, as evidenced by their increased VA, and the positive correlation between VA and MVC torque. This is consistent with studies that demonstrated an increase of the neural drive within the first weeks of a ST program.23, 47 Nevertheless, Blimkie et al.24 reported a lower activation level in obese adolescent boys. The discrepancy between our results and those of Blimkie et al.24 may be ascribed to the effect of sex. Indeed, during adolescence, boys have a higher potential for muscle hypertrophy compared with girls, thereby reducing the need to increase the VA to cope with the mechanical constraints.29, 30 Hypertrophy may then account for a larger part of the force adaptation to obesity in boys, whereas nervous adaptations may have a relatively larger contribution in girls, owing to their reduced potential for muscle hypertrophy compared with boys. Nevertheless, additional experiments are required to verify this assumption.
Validity of the MA measurements
MA measurements can be influenced by methodological conditions and/or certain pathological disorders. In this study, potential confounding factors are growth, metabolic disorders and the methodology used to assess MA variables. The latter factor can be reasonably excluded. Indeed, the MA characteristics of our lean subjects are consistent with previously published data measured on typically developing youth on the PF48, 49, 50 and KE muscles,49, 51 suggesting that our measurements are accurate. Any comparison with data from obese youth or adults is nevertheless currently impossible, as this study is the first to investigate the effect of obesity on MA characteristics. The intra-rater reliability analysis nevertheless suggests that most of the variables assessed were highly reliable. Finally, although the sample size was small, the statistical power was high for most of the comparisons between groups, except for the FL. However, this parameter is not the main outcome of this study.
One may also argue that growth may have confounded our measurements. Indeed, growth-related changes in anthropometrical parameters are strongly accompanied by MA modifications,5, 11 which are partly responsible for the increase of the maximal strength of the lower limb muscles from childhood to adulthood.45, 48, 49 However, in our study both groups were constituted so that chronological and biological age, height and maturity status were not significantly different. Therefore, any confounding effect of growth on our measurements can be reasonably discarded.
The adverse effects of obesity on the skeletal muscle, such as fat infiltration, increased connective tissue and low-grade inflammation,52, 53, 54 could also have biased the evaluation of MA. It has been shown that MT either increases in the acute phase of inflammatory myopathies14, 55 or decreases in the case of metabolic and/or mitochondrial myopathies. Yet, the effects of low-grade inflammation and intramuscular fat accumulation on MA characteristics in obese subjects are currently unknown. However, the obese subjects were young and had normal metabolic profiles,56 suggesting that they were free from disorders that could have biased MA evaluation. As a consequence, the MA differences observed between groups cannot be ascribed to methodological biases and are certainly related to the mechanical overload conferred by excess body mass in obese subjects, as discussed before.
Finally, one should consider that the measurements were taken at one site of the muscle and this may be not representative of the overall muscle group.57 As the MA and hypertrophy vary within and between subjects and muscles, we cannot completely rule out the possibility that obese and non-obese muscles may adapt differently. Additional experiments are thus required to address this issue. Furthermore, ACSA measurements from US have been validated against magnetic resonance imaging in lean subjects10 but such comparison is lacking in obese subjects. Therefore, our ACSA data should be interpreted with caution until they have been validated against magnetic resonance imaging or computed tomography.
Conclusion
This study has evidenced favorable muscular and nervous adaptations to youth obesity. Results revealed that VA, PA, MT, ACSA and segmental lean mass were greater in obese adolescent girls compared with their lean counterparts. These adaptations certainly accounted for the higher force production capacity of the KE and PF muscles in the obese group. The excess of body mass supported chronically by obese adolescents girls during daily activities could act as a chronic training stimulus generating favorable VA, MA, muscle size and strength adaptations. These adaptations, aimed at coping with the mechanical overload, seem to be similar and even more pronounced that those observed after ST in healthy populations. Whether the magnitude of this training effect of obesity is related to the obesity history, that is, to the duration of exposure to overloading, remains to be determined.
References
Gelfi C, Vasso M, Cerretelli P . Diversity of human skeletal muscle in health and disease: contribution of proteomics. J Proteomics 2011; 74: 774–795.
Narici M . Human skeletal muscle architecture studied in vivo by non-invasive imaging techniques: functional significance and applications. J Electromyogr Kinesiol 1999; 9: 97–103.
Kawakami Y, Abe T, Fukunaga T . Muscle-fiber pennation angles are greater in hypertrophied than in normal muscles. J Appl Physiol 1993; 74: 2740–2744.
Irrcher I, Adhihetty PJ, Joseph AM, Ljubicic V, Hood DA . Regulation of mitochondrial biogenesis in muscle by endurance exercise. Sports Med 2003; 33: 783–793.
Binzoni T, Bianchi S, Hanquinet S, Kaelin A, Sayegh Y, Dumont M et al. Human gastrocnemius medialis pennation angle as a function of age: from newborn to the elderly. J Physiol Anthropol Appl Hum Sci 2001; 20: 293–298.
Baroni BM, Geremia JM, Rodrigues R, De Azevedo Franke R, Karamanidis K, Vaz MA . Muscle architecture adaptations to knee extensor eccentric training: rectus femoris vs vastus lateralis. Muscle Nerve 2013; 48: 498–506.
Lieber RL, Friden J . Functional and clinical significance of skeletal muscle architecture. Muscle Nerve 2000; 23: 1647–1666.
Narici MV, Roi GS, Landoni L, Minetti AE, Cerretelli P . Changes in force, cross-sectional area and neural activation during strength training and detraining of the human quadriceps. Eur J Appl Physiol Occup Physiol 1989; 59: 310–319.
Kawakami Y, Abe T, Kuno SY, Fukunaga T . Training-induced changes in muscle architecture and specific tension. Eur J Appl Physiol Occup Physiol 1995; 72: 37–43.
Ahtiainen JP, Hoffren M, Hulmi JJ, Pietikainen M, Mero AA, Avela J et al. Panoramic ultrasonography is a valid method to measure changes in skeletal muscle cross-sectional area. Eur J Appl Physiol 2010; 108: 273–279.
Jacobs J, Jansen M, Janssen H, Raijmann W, Van Alfen N, Pillen S . Quantitative muscle ultrasound and muscle force in healthy children: a 4-year follow-up study. Muscle Nerve 2013; 47: 856–863.
Kubo K, Kanehisa H, Azuma K, Ishizu M, Kuno SY, Okada M et al. Muscle architectural characteristics in women aged 20-79 years. Med Sci Sports Exerc 2003; 35: 39–44.
Heckmatt JZ, Dubowitz V, Leeman S . Detection of pathological change in dystrophic muscle with B-scan ultrasound imaging. Lancet 1980; 1: 1389–1390.
Pillen S, van Alfen N, Zwarts MJ . Muscle ultrasound: a grown-up technique for children with neuromuscular disorders. Muscle Nerve 2008; 38: 1213–1214.
Sitnick M, Bodine SC, Rutledge JC . Chronic high fat feeding attenuates load-induced hypertrophy in mice. J Physiol 2009; 587: 5753–5765.
Maffiuletti N, Ratel S, Sartorio A, Martin V . The impact of obesity on in vivo human muscle function. Curr Obes Rep 2013; 2: 251–260.
De Ste Croix M, Deighan M, Armstrong N . Assessment and interpretation of isokinetic muscle strength during growth and maturation. Sports Med 2003; 33: 727–743.
Kanehisa H, Ikegawa S, Tsunoda N, Fukunaga T . Strength and cross-sectional area of knee extensor muscles in children. Eur J Appl Physiol Occup Physiol 1994; 68: 402–405.
Abdelmoula A, Martin V, Bouchant A, Walrand S, Lavet C, Taillardat M et al. Knee extension strength in obese and nonobese male adolescents. Appl Physiol Nutr Metab 2012; 37: 269–275.
Duche P, Ducher G, Lazzer S, Dore E, Tailhardat M, Bedu M . Peak power in obese and nonobese adolescents: effects of gender and braking force. Med Sci Sports Exerc 2002; 34: 2072–2078.
Maffiuletti NA, Jubeau M, Agosti F, De Col A, Sartorio A . Quadriceps muscle function characteristics in severely obese and nonobese adolescents. Eur J Appl Physiol 2008; 103: 481–484.
Tsiros MD, Coates AM, Howe PR, Grimshaw PN, Walkley J, Shield A et al. Knee extensor strength differences in obese and healthy-weight 10-to 13-year-olds. Eur J Appl Physiol 2013; 113: 1415–1422.
Gondin J, Guette M, Ballay Y, Martin A . Electromyostimulation training effects on neural drive and muscle architecture. Med Sci Sports Exerc 2005; 37: 1291–1299.
Blimkie CJ, Sale DG, Bar-Or O . Voluntary strength, evoked twitch contractile properties and motor unit activation of knee extensors in obese and non-obese adolescent males. Eur J Appl Physiol Occup Physiol 1990; 61: 313–318.
Aagaard P, Andersen JL, Dyhre-Poulsen P, Leffers AM, Wagner A, Magnusson SP et al. A mechanism for increased contractile strength of human pennate muscle in response to strength training: changes in muscle architecture. J Physiol 2001; 534: 613–623.
Kalofoutis C, Piperi C, Zisaki A, Singh J, Harris F, Phoenix D et al. Differences in expression of cardiovascular risk factors among type 2 diabetes mellitus patients of different age. Ann N Y Acad Sci 2006; 1084: 166–177.
Xinfei Wen SP, Wang Renwei, Wiklund Petri, Feng Guoshaung, Cheng Shu Mei, XT, Liu Yang et al. Does systemic low-grade inflammation associate with fat accumulation and distribution? A 7-year follow-up study with peripubertal girls. J Clin Endocrinol Metab 2014; 99: 1411–1419.
Yan AF, Voorhees CC, Beck KH, Wang MQ . A social ecological assessment of physical activity among urban adolescents. Am J Health Behav 2014; 38: 379–391.
Tipton KD . Gender differences in protein metabolism. Curr Opin Clin Nutr Metab Care 2001; 4: 493–498.
Ramos E, Frontera WR, Llopart A, Feliciano D . Muscle strength and hormonal levels in adolescents: gender related differences. Int J Sports Med 1998; 19: 526–531.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Tessier S, Vuillemin A, Briançon S . Propriétés psychométriques d'un questionnaire de mesure de l'activité physique chez l'enfant scolarisé âgé de six à dix ans: QAPE-semaine. Sci Sports 2007; 22: 224–231.
Skalsky AJ, Han JJ, Abresch RT, Shin CS, McDonald CM . Assessment of regional body composition with dual-energy X-ray absorptiometry in Duchenne muscular dystrophy: correlation of regional lean mass and quantitative strength. Muscle Nerve 2009; 39: 647–651.
Tanner JM, Whitehouse RH, Hughes PC, Carter BS . Relative importance of growth hormone and sex steroids for the growth at puberty of trunk length, limb length, and muscle width in growth hormone-deficient children. J Pediatr 1976; 89: 1000–1008.
Mirwald RL, Baxter-Jones AD, Bailey DA, Beunen GP . An assessment of maturity from anthropometric measurements. Med Sci Sports Exerc 2002; 34: 689–694.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Berg HE, Tedner B, Tesch PA . Changes in lower limb muscle cross-sectional area and tissue fluid volume after transition from standing to supine. Acta Physiol Scand 1993; 148: 379–385.
Noorkoiv M, Nosaka K, Blazevich AJ . Assessment of quadriceps muscle cross-sectional area by ultrasound extended-field-of-view imaging. Eur J Appl Physiol 2010; 109: 631–639.
Narici MV, Binzoni T, Hiltbrand E, Fasel J, Terrier F, Cerretelli P . In vivo human gastrocnemius architecture with changing joint angle at rest and during graded isometric contraction. J Physiol 1996; 496, Pt 1 287–297.
Merton PA . Voluntary strength and fatigue. J Physiol 1954; 123: 553–564.
Kluka V, Martin V, Vicencio SG, Jegu AG, Cardenoux C, Morio C et al. Effect of muscle length on voluntary activation level in children and adults. Med Sci Sports Exerc 2015; 47: 718–724.
Alegre LM, Ferri-Morales A, Rodriguez-Casares R, Aguado X . Effects of isometric training on the knee extensor moment-angle relationship and vastus lateralis muscle architecture. Eur J Appl Physiol 2014; 114: 2437–2446.
Williamson DL, Li Z, Tuder RM, Feinstein E, Kimball SR, Dungan CM . Altered nutrient response of mTORC1 as a result of changes in REDD1 expression: effect of obesity vs REDD1 deficiency. J Appl Physiol 2014; 117: 246–256.
Anderson AD, Solorzano CM, McCartney CR . Childhood obesity and its impact on the development of adolescent PCOS. Sem Reprod Med 2014; 32: 202–213.
O'Brien TD, Reeves ND, Baltzopoulos V, Jones DA, Maganaris CN . In vivo measurements of muscle specific tension in adults and children. Exp Physiol 2010; 95: 202–210.
Abe T, Fukashiro S, Harada Y, Kawamoto K . Relationship between sprint performance and muscle fascicle length in female sprinters. J Physiol Anthropol Appl Hum Sci 2001; 20: 141–147.
Maffiuletti NA, Pensini M, Martin A . Activation of human plantar flexor muscles increases after electromyostimulation training. J Appl Physiol 2002; 92: 1383–1392.
Kannas T, Kellis E, Arampatzi F, de Villarreal ES . Medial gastrocnemius architectural properties during isometric contractions in boys and men. Pediatr Excer Sci 2010; 22: 152–164.
Kubo K, Teshima T, Ikebukuro T, Hirose N, Tsunoda N . Tendon properties and muscle architecture for knee extensors and plantar flexors in boys and men. Clin Biomech 2014; 29: 506–511.
Shortland AP, Harris CA, Gough M, Robinson RO . Architecture of the medial gastrocnemius in children with spastic diplegia. Dev Med Child Neurol 2001; 43: 796–801.
Moreau NG, Teefey SA, Damiano DL . In vivo muscle architecture and size of the rectus femoris and vastus lateralis in children and adolescents with cerebral palsy. Dev Med Child Neurol 2009; 51: 800–806.
Bastard JP, Maachi M, Lagathu C, Kim MJ, Caron M, Vidal H et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw 2006; 17: 4–12.
Carolan E, Hogan AE, Corrigan M, Gaotswe G, O'Connell J, Foley N et al. The impact of childhood obesity on inflammation, innate immune cell frequency, and metabolic microRNA expression. J Clin Endocrinol Metab 2014; 99: E474–E478.
Reyes M, Quintanilla C, Burrows R, Blanco E, Cifuentes M, Gahagan S . Obesity is associated with acute inflammation in a sample of adolescents. Pediatr Diabetes 2014; 16: 109–116.
Pillen S, Scholten RR, Zwarts MJ, Verrips A . Quantitative skeletal muscle ultrasonography in children with suspected neuromuscular disease. Muscle Nerve 2003; 27: 699–705.
Vukovic R, Mitrovic K, Milenkovic T, Todorovic S, Soldatovic I, Sipetic-Grujicic S et al. Insulin-sensitive obese children display a favorable metabolic profile. Eur J Pediatr 2013; 172: 201–206.
Blazevich AJ, Gill ND, Zhou S . Intra- and intermuscular variation in human quadriceps femoris architecture assessed in vivo. J Anat 2006; 209: 289–310.
Acknowledgements
This project was funded by a grant from the Auvergne Regional Council (New Researcher Program 2012—V Martin).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Supplementary information
Rights and permissions
About this article
Cite this article
Garcia-Vicencio, S., Coudeyre, E., Kluka, V. et al. The bigger, the stronger? Insights from muscle architecture and nervous characteristics in obese adolescent girls. Int J Obes 40, 245–251 (2016). https://doi.org/10.1038/ijo.2015.158
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.158
- Springer Nature Limited
This article is cited by
-
Examining the mediating role of muscle quantity in adolescents: associations with adiposity, cardiorespiratory fitness, muscular fitness, and cardiometabolic risk factors
Scientific Reports (2024)
-
Comparison of gluteus medius strength between individuals with obesity and normal-weight individuals: a cross-sectional study
BMC Musculoskeletal Disorders (2021)
-
Assessment of peripheral muscle thickness and architecture in healthy volunteers using hand-held ultrasound devices; a comparison study with standard ultrasound
BMC Medical Imaging (2019)
-
Obesity-induced decreases in muscle performance are not reversed by weight loss
International Journal of Obesity (2017)
-
Factors associated with active commuting to school by bicycle from Bogotá, Colombia: The FUPRECOL study
Italian Journal of Pediatrics (2016)