Abstract
Background:
The term ‘metabolically healthy obese (MHO)’ is distinguished using body mass index (BMI), yet BMI is a poor index of adiposity. Some epidemiological data suggest that MHO carries a lower risk of cardiovascular disease (CVD) or mortality than being normal weight yet metabolically unhealthy.
Objectives:
We aimed to undertake a detailed phenotyping of individuals with MHO by using imaging techniques to examine ectopic fat (visceral and liver fat deposition) and myocardial function. We hypothesised that metabolically unhealthy individuals (irrespective of BMI) would have adverse levels of ectopic fat and myocardial dysfunction compared with MHO individuals.
Subjects:
Individuals were categorised as non-obese or obese (BMI ⩾30 kg m−2) and as metabolically healthy or unhealthy according to the presence or absence of metabolic syndrome.
Methods:
Sixty-seven individuals (mean±s.d.: age 49±11 years) underwent measurement of (i) visceral, subcutaneous and liver fat using magnetic resonance imaging and proton magnetic resonance spectroscopy, (ii) components of metabolic syndrome, (iii) cardiorespiratory fitness and (iv) indices of systolic and diastolic function using tissue Doppler echocardiography.
Results:
Cardiorespiratory fitness was similar between all groups; abdominal and visceral fat was highest in the obese groups. Compared with age- and BMI-matched metabolically healthy counterparts, the unhealthy (lean or obese) individuals had higher liver fat and decreased early diastolic strain rate, early diastolic tissue velocity and systolic strain indicative of subclinical systolic and diastolic dysfunction. The magnitude of dysfunction correlated with the number of components of metabolic syndrome but not with BMI or with the degree of ectopic (visceral or liver) fat deposition.
Conclusions:
Myocardial dysfunction appears to be related to poor metabolic health rather than simply BMI or fat mass. These data may partly explain the epidemiological evidence on CVD risk relating to the different obesity phenotypes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Obesity has been considered to confer an increased risk of cardiovascular disease (CVD) and mortality.1, 2 However, there is increasing recognition of a subgroup of obese patients with the mechanical complications of obesity but without the associated metabolic complications: ‘metabolically healthy obese’ (MHO).3
There is conflicting data in the literature regarding metabolic risk and obesity, and whether metabolic risk is determined more by the relative distribution than the absolute volume of fat. Metabolically healthy individuals have increased subcutaneous fat relative to visceral fat and lower cellular fat in liver and skeletal muscle in comparison to metabolically unhealthy individuals.4 They are also more insulin sensitive and have a better inflammatory status.5, 6 Several studies have demonstrated that the quantity of liver fat is more closely linked to the metabolic complications of obesity than that of visceral fat.7, 8, 9 However, there is conflicting evidence that suggests excess visceral fat and insulin resistance, but not general adiposity are associated with incident pre-diabetes and type 2 diabetes in obese individuals.10 A recent study of almost 30 000 individuals demonstrated that metabolically unhealthy obese individuals have a greater risk of developing diabetes than the metabolically healthy obese.11
Although this area remains contentious, a number of epidemiological studies have demonstrated that MHO individuals are also at a lower risk of CVD, and have reduced morbidity and mortality compared with the metabolically unhealthy obese, suggesting that cardiometabolic risk factors are more strongly associated with adverse cardiovascular outcomes than obesity.12, 13, 14, 15, 16 However, not all data suggest a protective effect. A recent study suggested that MHO confers increased risk of heart failure, but not acute myocardial infarction.17 Similarly, the risk of developing CVD in the San Antonio Heart Study was found to be increased in MHO.18 A recent systematic review and meta-analysis found that, after 10 years of follow-up, MHO is associated with an increased risk of total mortality and cardiovascular events.19
Several cross-sectional studies have tried to better understand the association between metabolic health and CVD by examining the impact of components of metabolic syndrome on cardiac function. Developments in echocardiographic techniques have improved the detection of relatively subtle myocardial disease.20 Strain and strain rate are sensitive measures of change of myocardial shape (that is, deformation). Strain indicates the amount of myocardial deformation (negative strain means shortening and positive strain, elongation); strain rate, is a measure of the rate of myocardial deformation. Measurement of strain and strain rate detect pre-clinical myocardial abnormalities, which can help predict risk of cardiovascular events and mortality.21 In patients with metabolic syndrome, subclinical left ventricular (LV) dysfunction has been detected (lower early diastolic and systolic tissue velocities accompanied by reduced strain and strain rates) compared with matched controls, worse in those with a greater number of components of the metabolic syndrome.22, 23 Considering the influence of liver fat on metabolic health and the association of non-alcoholic fatty liver disease (NAFLD) with features of the metabolic syndrome,24 others have looked at NAFLD patients and demonstrated subclinical myocardial systolic and diastolic dysfunction in the presence or absence of type 2 diabetes.25, 26
The main aim of this cross-sectional study was to determine whether metabolically unhealthy individuals irrespective of their BMI or normal weight, overweight or obese category, have evidence of increased ectopic fat (with higher visceral and liver fat deposition), combined with impaired myocardial function, compared with age- and BMI-matched metabolically healthy individuals. Furthermore we hypothesised that MHO individuals would have little evidence of ectopic fat and preserved myocardial function similar to normal weight (metabolically healthy) individuals despite their overall higher fat mass. This would provide a mechanistic context for the epidemiological data around CVD risk and the different obesity phenotypes. We employed a combination of whole body magnetic resonance imaging to look at ectopic fat and sensitive echocardiographic measures to measure myocardial function.
Subjects and methods
Subjects
Patients with hyperlipidemia and suspected NAFLD were prospectively recruited from specialist lipid and hepatology outpatient clinics at University Hospital Aintree, Liverpool. To recruit metabolically healthy, lean and obese individuals we relied on local advertisements. As the association of BMI and metabolic health with cardiac outcomes was a novel investigation, the effect size of interest was unknown. No formal sample size was calculated and recruitment of patients was based on availability with the hope that the estimates obtained will inform future studies. The study conformed to the Declaration of Helskinki and Liverpool Research Ethics Committee approved the study (Ethics Reference 09/H1005/7). All participants gave written informed consent.
Individuals aged >21 years with a BMI <40 kg m−2 who were able to walk on a treadmill and undergo magnetic resonance imaging scanning were recruited. Those with a history of CVD (including atrial fibrillation, ischaemic heart disease, heart failure or valvulopathy), type 1 or type 2 diabetes mellitus or chronic liver disease (other than NAFLD) were excluded. Individuals with a BMI >40 kg m−2 were excluded due to the technical challenges of performing high-quality echocardiographic studies on those with morbid obesity. All females and males consumed <14 and <21 units of alcohol per week, respectively. We recorded the following medications: diuretics, statins, ezetimibe, angiotensin converting enzyme inhibitors, calcium channel antagonists and beta-blockers in all participants.
Anthropometry
Age, gender, smoking status, past medical history, drug history and family history of CVD were established using a series of questionnaires. Smoking status was defined as never, former or current smoker. Physical activity levels were determined using the long format International Physical Activity Questionnaire.27 Alcohol intake was determined using the Alcohol Use Disorders Identification Test questionnaire.28 Blood pressure was measured on at least two separate occasions, with the patient sitting for at least 10 min. Body mass was measured after an overnight fast, without shoes, using a Tanita bioimpedance analyser, which also determined fat-free mass and fat percentage (Tanita BC420, Dolby Medical, Stirling, UK). Height was measured with a stadiometer to the nearest 0.5 cm (Seca, Birmingham, UK). BMI was calculated as weight in kilograms divided by height in metres (squared). Waist circumference was measured at the midpoint between the anterior superior iliac spine and the lower edge of the ribcage. The same individual undertook all anthropometric measurements.
Determinations of metabolic syndrome
Participants were classified as obese (BMI ⩾30 kg m−2) or non-obese (BMI <30 kg m−2), and with or without the metabolic syndrome (MS+ vs MS-). MS was defined by the Adult Treatment Panel III (ref. 29) as three or more of the following: waist circumference >102 cm (male) or >88 cm (female), triglycerides >1.7 mmol l−1 (or treatment for hyperlipidemia), high density lipoprotein (HDL) cholesterol <1 mmol l−1 (male) or <1.3 mmol l−1 (female), systolic blood pressure >130 mm Hg, diastolic blood pressure >85 mm Hg (or treatment for hypertension) and fasting glucose >6.1 mmol l−1. Ten-year risk of first atherosclerotic cardiovascular event was calculated using the Pooled Cohort Risk Assessment Equation.30
Magnetic resonance imaging and proton magnetic resonance spectroscopy
Participants underwent MR scanning using a 1.5 T Siemens Symphony scanner (Siemens Medical Solutions, Erlangen, Germany) at the University of Liverpool Magnetic Resonance and Image Analysis Research Centre. A single experienced radiographer performed all of the scans.
Abdominal axial T1-weighted fast spin echo scans (axial scans, 10 mm slice thickness followed by a 10 mm gap using the integrated body coil) were used to calculate abdominal visceral and subcutaneous adipose tissue.31 A blinded researcher performed all analyses of visceral and subcutaneous fat centrally.
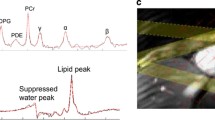
Liver lipid was measured non-invasively using proton magnetic resonance spectroscopy (1H-MRS) as previously described.31, 32, 33 NAFLD was defined as intrahepatocellular lipid content >5.5% measured by 1H-MRS. Three voxels of interest were identified in the liver avoiding ducts and vasculature and the mean value taken after data were processed independently. 1H MR spectra from liver was quantified using the AMARES algorithm in the software package jMRUI-3.0. Intrahepatocellular lipid is expressed as percentage of CH2 lipid signal amplitude relative to water signal amplitude after correcting for T1 and T2. Fat quantification by 1H-MRS has been validated against gold standard biochemical measurements.34
Biochemical markers and assays
Venous blood samples were obtained from participants after an overnight fast (minimum 8 h). Serum lipid profiles, liver function and glucose were measured using standard proprietary agents using the Olympus AU2700 analyser (Beckman Coulter Ltd, High Wycombe, UK). Plasma insulin and adiponectin were measured by radioimmunoassay using commercially available kits (Millipore Corporation, Billerica, MA; intra-assay coefficient of variation 6% and 5%, respectively). All patients with NAFLD underwent a routine liver screen (antinuclear, parietal cell, mitochondrial, smooth muscle, reticulin, liver kidney microsomal type 1 and anti-centromere antibodies, ceruloplasmin and ferritin levels and hepatitis serology).
Cardiopulmonary exercise testing
Incremental cardiopulmonary exercise testing was performed on a treadmill (Model 77OCE, RAM Medisoft Group, Sorinnes, Belgium) using a modified Bruce protocol. Breath-by-breath expiratory gases and ventilation analysis were performed (Love Medical Cardiopulmonary Diagnostics, Cheshire, UK). Following a 3-min warm-up at 2.8 km h−1 with no gradient, the initial workload was set at 2.8 km h−1 with a 5% gradient. Thereafter, stepwise increments were made in gradient and/or speed every 3 min as per the Modified Bruce Protocol. Peak patient effort was defined by any of (i) a respiratory exchange ratio >1.1, (ii) heart rate >90% of predicted maximum, (iii) a plateau in VO2, or (iv) patient exhaustion.35 Continuous electrocardiographic monitoring was used and all tests were physician-supervised.
Trans-thoracic echocardiography image acquisition and interpretation
All echocardiograms were performed using a GE Vivid 7 or E9 machine (GE, Pollards Wood, UK) with a 2.5 MHz phased array transducer and the patient in the left lateral position on a reclining couch. A combination of two-dimensional, M-mode, pulsed wave and continuous wave Doppler and tissue Doppler was used. Conventional echocardiographic views were obtained (parasternal long axis, parasternal short axis, apical 4 chamber, apical long axis, apical 2 chamber and subcostal).
LV diameter and wall thicknesses were measured in the parasternal long axis view using two-dimensional or M-mode measurements. LV mass was calculated using Devereux’s formula and was indexed to body surface area.36 Modified Simpson’s biplane method was used to determine LV ejection fraction. Mitral inflow velocities and deceleration times were measured using pulsed wave Doppler in the apical 4 chamber view. Isovolumetric relaxation time was calculated using continuous wave Doppler, with the cursor midway between left ventricular outflow and mitral inflow. For tissue Doppler imaging, colour tissue Doppler loops were recorded using a frame rate >100 frames s. Myocardial longitudinal function was assessed from three consecutive cycles of tissue Doppler imaging in the apical 4 chamber, apical 2 chamber and apical long axis views.
Echocardiographic data was analysed using Echopac V9.01 (GE, Horten, Norway). Peak systolic and early and late diastolic myocardial tissue velocities were obtained from the basal segment of all six LV walls. Myocardial deformation curves were obtained from the basal segment of all the six LV walls. Wall motion was manually tracked throughout the cardiac cycle to maintain continuity of the sampling area. Data were excluded if a smooth curve was unobtainable, or if the angle between the ventricular wall and the scan line was >20°. From these curves, peak systolic strain, systolic and early and late diastolic strain rates were obtained. Using data from each of the three cardiac cycles, the values from each wall were averaged to give a mean value.
Statistical analysis
Continuous variables are presented as mean±s.d. or median (interquartile range) if non-normally distributed; categorical variables are presented as frequencies and percentages. Univariate statistical comparisons of patient demographics between groups were conducted; for continuous variables using a one-way analysis of variance or a Kruskal–Wallis test when non-normal; for categorical variables, using a χ2 test or a Fisher’s Exact test when cell frequencies were insufficient. P-values were corrected for multiple comparisons using Sime’s procedure and declared as significant if a P-value <0.017 was achieved.
A multiple linear regression model was fitted to investigate the association of BMI and metabolic syndrome on cardiac function. A two-way interaction of the main effects was investigated and retained if a P-value <0.1 was obtained. Sensitivity analysis was conducted, adjusting the final model for age and gender. To explore the association between cardiac function and the number of metabolic syndrome components a univariate regression model was fitted. To investigate the relative strength of each metabolic syndrome component on cardiac function, all variables were standardised. A multivariable linear regression model was fitted including the metabolic syndrome components as main effects and then adjusted for age and gender. No interactions were investigated and results are expressed as the s.d. change in cardiac function associated with a one s.d. increment in the independent variable.
The association of liver fat with cardiac function was analysed using Spearman’s correlation coefficient.
Model fit was assessed using quantile-quantile (QQ) plots and standardised residuals against predicted means plots. Results were declared as significant if P<0.05. All statistical analyses were conducted using Stata IC 13 (Stata Statistical Software: Release 13, StataCorp LP, College Station, TX, USA).
Results
Clinical characteristics
Sixty-seven participants were recruited, of whom two were excluded (one with left bundle branch block on electrocardiography, one unable to tolerate MR scanning; Table 1). Twenty-two participants had ⩾3 components of the metabolic syndrome: 21 (96%) had the waist circumference component, 18 (82%) the triglyceride component, 16 (73%) the blood pressure component, 12 (55%) the HDL cholesterol component and 8 (36%) the glucose component. Tables 1 and 2 and Figure 1 show mean results in the four groups formed by the two classifications, obese vs non-obese and with (MS+) vs without (MS−) metabolic syndrome. There were no significant differences between the four groups in terms of age, gender, systolic blood pressure, smoking status or cardiorespiratory fitness (Table 1). Ten-year cardiovascular risk was highest in the MS+ groups.
Higher proportions of those in the MS+ groups were taking medication for hypertension or hyperlipidaemia, reflecting the higher prevalence of these conditions. In non-obese MS− one patient was taking an angiotensin converting enzyme inhibitor, two calcium channel antagonists and six statins; in non-obese MS+ two were taking calcium channel antagonists, three statins, one diuretics and one ezetimibe; in obese MS− one patient was taking a statin; in obese MS+ five were taking angiotensin converting enzyme inhibitors, one calcium channel antagonists, two beta-blockers, four statins and one ezetimibe.
Metabolic and biochemical data
There were significant differences in fasting triglyceride, HDL cholesterol and glucose concentrations between the four groups (Table 1). HbA1C was <4.5 in all individuals. Insulin concentrations were significantly different between groups (P=0.002) with higher levels observed in the obese groups. There were no significant differences in adiponectin concentrations between the groups. The liver screen was negative for all patients included in the study.
Body composition data
As expected, there was a significant difference in BMI across the four groups (P<0.001; Table 1). The obese groups had greater subcutaneous adipose tissue and visceral adipose tissue than the non-obese groups, although there was no significant difference in their relative proportion (VAT:SAT ratio). The intrahepatocellular lipid content was up to four times higher in the metabolically unhealthy patients in comparison to the metabolically healthy, however the difference across groups did not reach statistical significance (P=0.055).
Echocardiographic data
In terms of LV morphology, there were no significant differences across the groups in LV mass, posterior wall thickness, LV mass indexed to body surface area, LV septal wall thickness or LV internal diastolic diameter (Table 2).
In terms of LV systolic function, LV ejection fraction, systolic tissue velocity (S′) and peak systolic longitudinal strain rate did not differ significantly across the groups, however, there was a significant difference in peak systolic (longitudinal) strain (P=0.001; Table 2 and Figure 1a). Linear regression showed that patients with MS had significantly lower peak systolic strain than those without (Δ= −2.45: 95% confidence interval (CI) −3.74, −1.15; P<0.001), with a progressive reduction in peak systolic strain as the number of MS components increased (Figure 2a and Table 4A). Of the metabolic syndrome components, triglycerides were significantly associated with peak systolic strain (for a one s.d. increase: −0.29: 95% CI −0.53, −0.04; P=0.021; Table 4B).
A higher BMI was associated with a lower peak systolic strain (for a unit increase in BMI, Δ= −0.12: 95% CI −0.24, −0.004; P=0.043; Table 3). No significant interaction was found between BMI and metabolic health. Peak systolic strain was significantly inversely correlated with liver fat (P=−0.35; P=0.0042) but not with VAT:SAT ratio (P=−0.12; P=0.36).
In terms of LV diastolic function, left atrial size and E/E′ ratio were not significantly different across the groups (Table 2). Early (E′) and late (A′) diastolic tissue velocity and early diastolic strain rate (EDSR) were significantly different between groups (all P<0.01) with lower levels observed for the metabolically unhealthy. Linear regression showed that patients with metabolic syndrome had significantly lower E′ (−1.89: 95% CI −2.73, −1.06; P<0.001) and EDSR (−0.28: 95% CI: −0.41, −0.15; P<0.001) with a progressive reduction occurring in both cardiac parameters as the number of metabolic syndrome components increased (Figure 2b and c; Table 4A and B). Of the metabolic syndrome components, glucose was significantly associated with early diastolic tissue velocity (for a one s.d. increase: −0.30: 95% CI −0.54, −0.07; P=0.012)(Table 4A and B) and systolic blood pressure was significantly associated with EDSR (for a one s.d. increase: −0.44: 95% CI −0.76, −0.11; P=0.01; Table 4A and B).
As to the feasibility and reproducibility of echocardiography, for tissue velocity, global peak systolic strain (%) and strain rate (s−1), the intra-observer and inter-observer variability was 0.3±0.3, 1.3±0.5%, 0.1±0.1 s−1 and 0.4±0.3, 1.2±0.8% and 0.3±0.2 s−1, respectively. Despite care taken during image acquisition, it was not possible to analyse 8% of left ventricular segments due to artefact and signal noise.
Discussion
This integration of detailed MRI and MRS analysis of body composition, echocardiographic assessment of myocardial function and evaluation of metabolic health has provided an opportunity to compare the determinants of myocardial function in four distinct phenotypes: non-obese, mean age and BMI-matched metabolically healthy and metabolically unhealthy individuals (non-obese MS− and MS+, respectively) and obese, mean age and BMI-matched metabolically healthy and metabolically unhealthy individuals (obese MS− and MS+, respectively). We find that subclinical impairment of myocardial function is more closely associated with adverse metabolic health than with either obesity or BMI. Echocardiographic measures of both diastolic and systolic myocardial function were reduced in the metabolically unhealthy vs healthy groups, irrespective of obesity. We also find that metabolic health is more closely associated with increased liver fat than visceral fat deposition suggesting fat distribution is pivotal. These observational data help provide mechanistic insight into the pathophysiology of (obesity-related) CVD and potentially support the epidemiological observations of differential cardiovascular outcomes among metabolically healthy and unhealthy, lean and obese individuals.
There is evidence from transgenic animal and human models that the capacity of SAT to expand with over-feeding determines to what extent excess lipids ‘spill over’ into ectopic sites (for example, skeletal muscle, liver and cardiac muscle), and therefore whether obesity is metabolically healthy or unhealthy.37, 38 However, there is currently no consensus on how to define metabolic health or metabolically healthy obesity except for the inclusion of obesity (BMI >30 kg m−2) as a criterion. Some studies use the number of components of the MS, although with different diagnostic criteria.39 Others have used measures of insulin resistance, with inconsistencies in definitions or diagnostic criteria (use of HOMA-IR, Matsuda index derived from an oral glucose tolerance test or from the glucose disposal rate). Several studies have used measures of inflammation including C-reactive protein measurements. Large variations in reported prevalence of MHO (that is, our obese MS− group) are a function of the varied criteria used to define this phenotype.39 Examining the impact of metabolic health on myocardial function, Seo et al.22 and Wong et al.23 have demonstrated subclinical left ventricular dysfunction in patients with an increased metabolic burden compared with control groups. However these studies provide no data on different body composition phenotypes.
Our findings are consistent with several large-scale epidemiological studies suggesting that metabolically healthy (obese and non-obese) individuals have a lower risk of CVD than metabolically unhealthy (obese and non-obese) individuals12, 13, 15 although this is not universally agreed.18, 19 Morkedal et al.17 have demonstrated disparate effects on coronary heart disease and heart failure, which may account for the contrasting conclusions.40
There are several potential mechanisms whereby metabolically unhealthy individuals may have impaired myocardial performance. The metabolically unhealthy group tended to have higher intrahepatocellular lipid content. Previous studies demonstrated that NAFLD is associated with increased levels of both intra-pericardial and extra-pericardial fat, which may adversely influence cardiac metabolism.41, 42, 43 Thus metabolically unhealthy patients may also have increased liver and intra-myocardial triglyceride, leading to lipotoxicity and apoptosis of cardiac myocytes, potentially contributing to myocardial dysfunction.44 However, in our study the difference in liver triglyceride did not reach statistical significance and we did not measure cardiac triglyceride. Metabolically unhealthy individuals have increased levels of inflammatory markers (interleukins, tumour necrosis factor-alpha and high-sensitivity CRP), which can result in cardiac fibrosis and myocardial stiffening45, 46 and increased circulating levels of the liver-secreted glycoprotein fetuin A that further induces subclinical inflammation and perturbs lipid and glucose metabolism.6, 47 Hyperinsulinaemia and/or insulin resistance may also be implicated through abnormal LV energy metabolism;41 indeed the cardiovascular benefit derived from bariatric surgery was strongly associated with reduced fasting insulin concentration.48 It has been suggested the protective effect of MHO on outcomes may be due to higher levels of cardiorespiratory fitness but we found no evidence to support this.49
These findings may have therapeutic implications. Diastolic myocardial abnormalities are associated with an increased risk of cardiovascular events and cardiac and all-cause mortality.50, 51 Early detection of myocardial dysfunction may provide an opportunity for patients to modify their lifestyles, thereby affording the opportunity for primary prevention and reducing mortality risk. In the SOS (Swedish Obese Subjects) trial, a prospective, controlled, long-term study of bariatric surgery in morbidly obese people, weight loss significantly improved cardiovascular outcomes.48 Obesity is of course associated with a variety of other medical complications besides type 2 diabetes and CVD, not related to metabolic health but caused by the mechanical consequences of obesity, for example, obstructive sleep apnoea or lower limb osteoarthritis or by so far unknown mechanisms, for example, the association with certain types of cancer. Furthermore, there are significant functional and psychological sequelae of obesity, which are again unrelated to metabolic health. However these findings would indicate that preventative strategies in obesity must be driven by disease-specific end points (metabolic, mechanical and functional end points) rather than simply driven quantitatively by weight loss.
The study has several limitations. Due to the small group sizes for the metabolic analysis, it was not possible to calculate robust estimates. Furthermore, the small sample size also led to large variability within the measurements. However the sample size is large enough to observe clinically and statistically significant differences between the groups. It must be noted that our cohort sampling strategy may have led to a bias in the metabolically unhealthy cohort towards an abnormal phenotype that is predisposed to myocardial functional abnormalities as these patients required specialist care. Likewise, recruitment of ‘healthy participants’ from the community may have exaggerated the bias away from the null with ‘healthy volunteer’ bias. A further limitation is the possibility that a proportion of our participants may have undiagnosed atherosclerotic disease, contributing to the apparent myocardial abnormalities. However, it was not feasible to undertake coronary angiography or myocardial functional imaging in our participants to completely exclude silent coronary artery disease but all patients were screened with clinical assessment, echocardiography and exercise electrocardiography for evidence of coronary artery disease. We were also unable to measure serum fetuin A concentrations or markers of inflammation due to sample volume limitations.
Conclusion
The metabolic sequelae associated with unhealthy obesity appear to underlie the functional abnormalities in myocardial systolic and diastolic function, so metabolically healthy obese subjects have normal myocardial performance. This finding may help explain the epidemiological associations of metabolically healthy obesity with lower cardiovascular morbidity and mortality.
References
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med 2010; 363: 2211–2219.
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet 2005; 366: 1640–1649.
Stefan N, Häring H-U, Hu FB, Schulze MB . Metabolically healthy obesity: epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol 2013; 1: 152–162.
Arsenault BJ, Beaumont EP, Despres JP, Larose E . Mapping body fat distribution: a key step towards the identification of the vulnerable patient? Ann Med 2012; 44: 758–772.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med 2008; 168: 1617–1624.
Phillips CM, Perry IJ . Does inflammation determine metabolic health status in obese and nonobese adults? J Clin Endocrinol Metab 2013; 98: E1610–E1619.
Kantartzis K, Machann J, Schick F, Fritsche A, Haring HU, Stefan N . The impact of liver fat vs visceral fat in determining categories of prediabetes. Diabetologia 2010; 53: 882–889.
Fabbrini E, Magkos F, Mohammed BS, Pietka T, Abumrad NA, Patterson BW et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc Natl Acad Sci USA 2009; 106: 15430–15435.
Klein S . Is visceral fat responsible for the metabolic abnormalities associated with obesity?: implications of omentectomy. Diabetes Care 2010; 33: 1693–1694.
Neeland IJ, Turer AT, Ayers CR, Powell-Wiley TM, Vega GL, Farzaneh-Far R et al. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA 2012; 308: 1150–1159.
Heianza Y, Kato K, Kodama S, Ohara N, Suzuki A, Tanaka S et al. Risk of the development of type 2 diabetes in relation to overall obesity, abdominal obesity and the clustering of metabolic abnormalities in Japanese individuals: does metabolically healthy overweight really exist? The Niigata Wellness Study. Diabet Med 2015; 32: 665–672.
Appleton SL, Seaborn CJ, Visvanathan R, Hill CL, Gill TK, Taylor AW et al. Diabetes and cardiovascular disease outcomes in the metabolically healthy obese phenotype: a cohort study. Diabetes Care 2013; 36: 2388–2394.
Hamer M, Stamatakis E . Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab 2012; 97: 2482–2488.
Voulgari C, Tentolouris N, Dilaveris P, Tousoulis D, Katsilambros N, Stefanadis C . Increased heart failure risk in normal-weight people with metabolic syndrome compared with metabolically healthy obese individuals. J Am Coll Cardiol 2011; 58: 1343–1350.
Calori G, Lattuada G, Piemonti L, Garancini MP, Ragogna F, Villa M et al. Prevalence, metabolic features, and prognosis of metabolically healthy obese Italian individuals: the Cremona Study. Diabetes Care 2011; 34: 210–215.
Choi KM, Cho HJ, Choi HY, Yang SJ, Yoo HJ, Seo JA et al. Higher mortality in metabolically obese normal-weight people than in metabolically healthy obese subjects in elderly Koreans. Clin Endocrinol (Oxf) 2013; 79: 364–370.
Morkedal B, Vatten LJ, Romundstad PR, Laugsand LE, Janszky I . Risk of myocardial infarction and heart failure among metabolically healthy but obese individuals. The HUNT Study, Norway. J Am Coll Cardiol 2013; 63: 1071–1078.
Aung K, Lorenzo C, Hinojosa MA, Haffner SM . Risk of developing diabetes and cardiovascular disease in metabolically unhealthy normal-weight and metabolically healthy obese individuals. J Clin Endocrinol Metab 2014; 99: 462–468.
Kramer CK, Zinman B, Retnakaran R . Are metabolically healthy overweight and obesity benign conditions?: A systematic review and meta-analysis. Ann Intern Med 2013; 159: 758–769.
Hoit BD . Strain and strain rate echocardiography and coronary artery disease. Circ Cardiovasc Imaging 2011; 4: 179–190.
Ersboll M, Valeur N, Mogensen UM, Andersen MJ, Moller JE, Velazquez EJ et al. Prediction of all-cause mortality and heart failure admissions from global left ventricular longitudinal strain in patients with acute myocardial infarction and preserved left ventricular ejection fraction. J Am Coll Cardiol 2013; 61: 2365–2373.
Seo JM, Park TH, Lee DY, Cho YR, Baek HK, Park JS et al. Subclinical myocardial dysfunction in metabolic syndrome patients without hypertension. J Cardiovasc Ultrasound 2011; 19: 134–139.
Wong CY, O'Moore-Sullivan T, Fang ZY, Haluska B, Leano R, Marwick TH . Myocardial and vascular dysfunction and exercise capacity in the metabolic syndrome. Am J Cardiol 2005; 96: 1686–1691.
Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 2001; 50: 1844–1850.
Goland S, Shimoni S, Zornitzki T, Knobler H, Azoulai O, Lutaty G et al. Cardiac abnormalities as a new manifestation of nonalcoholic fatty liver disease: echocardiographic and tissue Doppler imaging assessment. J Clin Gastroenterol 2006; 40: 949–955.
Bonapace S, Perseghin G, Molon G, Canali G, Bertolini L, Zoppini G et al. Nonalcoholic fatty liver disease is associated with left ventricular diastolic dysfunction in patients with type 2 diabetes. Diabetes Care 2011; 35: 389–395.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA . The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 1998; 158: 1789–1795.
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2013; 129: S49–S73.
Thomas EL . Hepatic triglyceride content and its relation to body adiposity: a magnetic resonance imaging and proton magnetic resonance spectroscopy study. Gut 2005; 54: 122–127.
Gardner CJ, Irwin AJ, Daousi C, McFarlane IA, Joseph F, Bell JD et al. Hepatic steatosis, GH deficiency and the effects of GH replacement: a Liverpool magnetic resonance spectroscopy study. Eur J Endocrinol 2012; 166: 993–1002.
Cuthbertson DJ, Irwin A, Gardner CJ, Daousi C, Purewal T, Furlong N et al. Improved glycaemia correlates with liver fat reduction in obese, type 2 diabetes, patients given glucagon-like peptide-1 (GLP-1) receptor agonists. PloS One 2012; 7: e50117.
Szczepaniak LS, Babcock EE, Schick F, Dobbins RL, Garg A, Burns DK et al. Measurement of intracellular triglyceride stores by H spectroscopy: validation in vivo. Am J Physiol 1999; 276: E977–E989.
Stickland MK, Butcher SJ, Marciniuk DD, Bhutani M . Assessing exercise limitation using cardiopulmonary exercise testing. Pulm Med 2012; 2012: 824091.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986; 57: 450–458.
Kim JY, van de Wall E, Laplante M, Azzara A, Trujillo ME, Hofmann SM et al. Obesity-associated improvements in metabolic profile through expansion of adipose tissue. J Clin Invest 2007; 117: 2621–2637.
Alligier M, Gabert L, Meugnier E, Lambert-Porcheron S, Chanseaume E, Pilleul F et al. Visceral fat accumulation during lipid overfeeding is related to subcutaneous adipose tissue characteristics in healthy men. J Clin Endocrinol Metab 2013; 98: 802–810.
Hinnouho GM, Czernichow S, Dugravot A, Batty GD, Kivimaki M, Singh-Manoux A . Metabolically healthy obesity and risk of mortality: does the definition of metabolic health matter? Diabetes Care 2013; 36: 2294–2300.
Lavie CJ, Milani RV, Ventura HO . Disparate effects of metabolically healthy obesity in coronary heart disease and heart failure. J Am Coll Cardiol 2014; 63: 1079–1081.
Perseghin G, Ntali G, De Cobelli F, Lattuada G, Esposito A, Belloni E et al. Abnormal left ventricular energy metabolism in obese men with preserved systolic and diastolic functions is associated with insulin resistance. Diabetes Care 2007; 30: 1520–1526.
Perseghin G, Lattuada G, De Cobelli F, Esposito A, Belloni E, Ntali G et al. Increased mediastinal fat and impaired left ventricular energy metabolism in young men with newly found fatty liver. Hepatology 2008; 47: 51–58.
Hallsworth K, Hollingsworth KG, Thoma C, Jakovljevic D, MacGowan GA, Anstee QM et al. Cardiac structure and function are altered in adults with non-alcoholic fatty liver disease. J Hepatol 2013; 58: 757–762.
Szczepaniak LS, Victor RG, Orci L, Unger RH . Forgotten but not gone: the rediscovery of fatty heart, the most common unrecognized disease in America. Circ Res 2007; 101: 759–767.
Edgley AJ, Krum H, Kelly DJ . Targeting fibrosis for the treatment of heart failure: a role for transforming growth factor-beta. Cardiovasc Ther 2012; 30: e30–e40.
Tamaki S, Mano T, Sakata Y, Ohtani T, Takeda Y, Kamimura D et al. Interleukin-16 promotes cardiac fibrosis and myocardial stiffening in heart failure with preserved ejection fraction. PLoS One 2013; 8: e68893.
Stefan N, Häring HU . The role of hepatokines in metabolism. Nat Rev Endocrinol 2013; 9: 144–152.
Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012; 307: 56–65.
Ortega FB, Lee DC, Katzmarzyk PT, Ruiz JR, Sui X, Church TS et al. The intriguing metabolically healthy but obese phenotype: cardiovascular prognosis and role of fitness. Eur Heart J 2013; 34: 389–397.
Bella JN, Palmieri V, Roman MJ, Liu JE, Welty TK, Lee ET et al. Mitral ratio of peak early to late diastolic filling velocity as a predictor of mortality in middle-aged and elderly adults: the Strong Heart Study. Circulation 2002; 105: 1928–1933.
Schillaci G, Pasqualini L, Verdecchia P, Vaudo G, Marchesi S, Porcellati C et al. Prognostic significance of left ventricular diastolic dysfunction in essential hypertension. J Am Coll Cardiol 2002; 39: 2005–2011.
Acknowledgements
The European Foundation for the Study of Diabetes (EFSD) funded this work. We are grateful to the volunteers for participating in the study and to Ms Rebecca Asher, Liverpool Clinical Trials Unit, University of Liverpool, for her significant statistical input. Funding was provided by the European Foundation for the Study of Diabetes, Rheindorfer Weg 3, 40591 Dusseldorf, Germany.
Author contributions
All authors assisted in the writing of the manuscript. In addition, RD collected and analysed the demographic, echocardiographic and cardiorespiratory exercise data. JJ cross-checked the echocardiographic data acquisition and analysis. VSS assisted with demographic and biochemical data collection and analysis. AI performed the anthropometric measurements and assisted with the biochemical data collection. VA collected the magnetic resonance imaging data. GJK analysed the magnetic resonance imaging data. MH and CD assisted in the characterisation of the patient groups. FS-M and MU processed and analysed all of the biochemical samples. MB and DJC devised the protocol for the study, and oversaw all aspects of data acquisition and analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dobson, R., Burgess, M., Sprung, V. et al. Metabolically healthy and unhealthy obesity: differential effects on myocardial function according to metabolic syndrome, rather than obesity. Int J Obes 40, 153–161 (2016). https://doi.org/10.1038/ijo.2015.151
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.151
- Springer Nature Limited
This article is cited by
-
Association of metabolically healthy obesity in young adulthood with myocardial structure and function
International Journal of Obesity (2023)
-
Clinical evaluation of patients living with obesity
Internal and Emergency Medicine (2023)
-
Illness perceptions and health-related quality of life in individuals with overweight and obesity
International Journal of Obesity (2022)
-
Metabolically healthy obesity and physical fitness in military males in the CHIEF study
Scientific Reports (2021)
-
Metabolically healthy obesity: time for a change of heart?
Nature Reviews Endocrinology (2021)