Abstract
Background/Objectives:
Timing of food intake associates with body weight regulation, insulin sensitivity and glucose tolerance. However, the mechanism is unknown. The aim of this study was to investigate the effects of changes in meal timing on energy-expenditure, glucose-tolerance and circadian-related variables.
Subjects/Methods:
Thirty-two women (aged 24±4 years and body mass index 22.9±2.6 kg m−2) completed two randomized, crossover protocols: one protocol (P1) including assessment of resting-energy expenditure (indirect-calorimetry) and glucose tolerance (mixed-meal test) (n=10), the other (P2) including circadian-related measurements based on profiles in salivary cortisol and wrist temperature (Twrist) (n=22). In each protocol, participants were provided with standardized meals (breakfast, lunch and dinner) during the two meal intervention weeks and were studied under two lunch-eating conditions: Early Eating (EE; lunch at 13:00) and Late Eating (LE; lunch 16:30).
Results:
LE, as compared with EE, resulted in decreased pre-meal resting-energy expenditure (P=0.048), a lower pre-meal protein-corrected respiratory quotient (CRQ) and a changed post-meal profile of CRQ (P=0.019). These changes reflected a significantly lower pre-meal utilization of carbohydrates in LE versus EE (P=0.006). LE also increased glucose area under curve above baseline by 46%, demonstrating decreased glucose tolerance (P=0.002). Changes in the daily profile of cortisol and Twrist were also found with LE blunting the cortisol profile, with lower morning and afternoon values, and suppressing the postprandial Twrist peak (P<0.05).
Conclusions:
Eating late is associated with decreased resting-energy expenditure, decreased fasting carbohydrate oxidation, decreased glucose tolerance, blunted daily profile in free cortisol concentrations and decreased thermal effect of food on Twrist. These results may be implicated in the differential effects of meal timing on metabolic health.
Similar content being viewed by others
Introduction
The timing of food intake has recently been shown to associate with body weight regulation, insulin sensitivity and glucose tolerance.1, 2, 3, 4 However, the mechanism is unknown. Indeed, these observations appear to be independent of 24-h caloric intake and self-reported activity levels.5 Meal timing has also been shown to be able to affect the daily pattern in glucocorticoids and circadian clocks in metabolic tissues such as adipose tissue, liver and pancreas in animal studies.6, 7 Differences in the response of wrist temperature to meals have been observed between obese versus normal-weight individuals8 and between low versus high weight-loss responders.9 Thus, in the current investigation, we aimed to study the influence of meal timing on resting energy expenditure, diet-induced thermogenesis, substrate oxidation, glucose tolerance and measures related to the circadian system, including the morning-evening cortisol difference and the daily profile of wrist temperature (Twrist), as possible mechanisms underlying the differential effects of meal timing on metabolism.
Previous data have demonstrated that when experimental animals eat food at the ‘wrong time’ they become obese, although they apparently have the same energy intake.1, 3, 4 In humans, experimental data under controlled in-laboratory conditions have shown that a 12-h inversion of the fasting/fasting and sleep/wake cycle (that is, including eating during the biological night and fasting during the biological day) resulted in decreased glucose tolerance.2 Also, more subtle changes in meal timing, that is, the distribution of caloric intake across the normal wake episode, appear to influence the success of weight-loss therapy.10 Moreover, in a longitudinal study performed in a Mediterranean sample from Spain, we recently showed that the timing of the main meal (that is, lunch in this particular population) was predictive of weight-loss success during a 20-week dietary intervention conducted in 420 obese and overweight individuals, and that this effect was independent from total 24-h caloric intake.5 Another relevant result from the same study was that insulin sensitivity as estimated by HOMA-IR was lower in late eaters as compared with early eaters.5
In animal experiments, it has been demonstrated that behavioral activity and physiological changes anticipate daily rhythmic food access. Some examples are anticipatory increases in physical activity, changes in glucocorticoids and variations in body temperature.7, 11, 12
Indeed, dramatic changes in food timing, such as daytime restricted food access in nocturnal rodents, have been shown to not only lead to accelerated weight gain and impaired glucose tolerance, but also to internal desynchrony between the central and the peripheral clocks.6 In fact, peripheral oscillators located in metabolic tissues such as the liver and pancreas are synchronized by restricted food access, whereas the central circadian pacemaker, located in the suprachiasmatic nucleus, remains phase-locked to the light/dark cycle.6 This internal desynchrony has been hypothesized to underlie the adverse effects of abnormal feeding schedules. Also, in animals, the adrenal cortex has been shown to contain peripheral oscillators that are critical for the daily rhythm in glucocorticoid production.13 This raises the question whether conflicting signals derived from the suprachiasmatic nucleus—through both regulation of ACTH and the sympathetic innervations of the adrenal cortex—versus those from the peripheral oscillators themselves, blunt the daily pattern in cortisol in humans. Thus, the aim of this study was to investigate, in a randomized, crossover study, the effects of changes in lunch timing on: (i) metabolic measurements such as energy expenditure and glucose tolerance and (ii) circadian-related measures such as the daily patterns of cortisol and skin temperature.
Methods
Subjects
Thirty-two women aged 24±4 years, with body mass index of 22.9±2.6 kg m−2, from a Mediterranean area in Spain (Murcia) were included in the study in two separate protocols (Table 1). Ten women were involved in protocol 1: age, 26±4 years; body mass index, 22.54±2.05 kg m−2; body fat percentage, 27.07±6.10. In protocol 2, 22 women participated: age, 24±4 years; body mass index, 23.19±2.99 kg m−2; body fat percentage, 25.61±6.25. No significant differences in age, body mass index and body fat were found among women from both protocols (P>0.05 in all cases). Moreover, no significant differences were found in the sleep characteristics between Late Eating (LE) and Early Eating (EE) conditions in the total population studied, that is, sleep onset (LE: 01:23±0:58 h; EE: 01:21±0:51 h; P=0.790) and sleep duration (LE: 7:22±1:01 h; EE: 7:31±1:10 h; P=0.580).
Participants fulfilled criteria previously established such as healthy women with no endocrine, renal, hepatic or psychiatric disorders and who were not using prescribed drugs or other pharmacologic treatment other than oral contraceptives. All research methods and procedures were performed in accordance with the Helsinki Declaration of Human Studies and were approved by the Ethical Committee of the University of Murcia. All participants signed an informed consent document.
Experimental design
The study was conducted in two randomized and crossover design protocols (P1 and P2). Randomization was performed by the UMU staff with block size 2 in a balanced design by a computer-executed software (http://www.randomization.com). Subjects were instructed to follow their habitual sleep patterns that were required to be the same across the 14 days for both meal timing intervention weeks within each of the Protocols P1 and P2 (two weeks per protocol). In addition, they were provided with standardized meals (breakfast, lunch and dinner) during these same weeks. In both Protocol P1 and P2, participants were studied under EE conditions (13:00 h) and LE conditions (16:30 h), in a randomized order, with a 1-week washout period between visits during which women consumed lunch at their habitual time which was at 14:45±0:33 h for P1 and 14:25±0:09 h for P2 (mean±s.d.).
General measurements in Protocol 1 and 2
Anthropometry
In both protocols (1 and 2), body weight was determined in barefooted subjects wearing light clothes using a digital scale accurate to the nearest 0.1 kg. Height was measured using a Harpenden digital stadiometer (rank, 0.7–2.05). The subject was positioned upright, relaxed and with the head in the Frankfurt plane. Height and weight measurements were obtained at the same time of day in the morning.
Total body fat was measured by bioelectrical impedance, using TANITA TBF-300 equipment (Tanita Corporation of America, Arlington Heights, IL, USA). Body fat distribution was assessed by the measurement of several circumferences and skin folds in the upright position: waist circumference at the level of the umbilicus and hip circumference at the widest circumference over the greater trochanters.
Food intake
All subjects were given a controlled diet for two 7-day periods to provide sufficient energy for body weight maintenance, based on the mean estimated energy expenditure from Harris Benedict with an activity factor of 1.375 (1–3 days of physical activity per week). The total daily energy intake was 1868±234 Kcal per day; 50% of energy was supplied by carbohydrate, 35% by fat and 15% by protein. The distribution of energy during the day was: 25.8% for breakfast, 47.0% for lunch and 27.2% for dinner. Total energy intake and macronutrient composition were determined using Grunumur (version 2.0, University of Murcia, Murcia, Spain),14 a nutritional evaluation program, in conjunction with Spanish food composition tables.
Sleep duration
Subjects were instructed to keep a sleep diary designed by the Murcia University Chronobiology Laboratory.15 The following data were obtained for every subject on a daily basis: time to bed, time of lights off, nocturnal awakenings lasting more than 10 min, sleep offset, time the subject got up. Sleep duration was calculated as the difference between lights off and sleep offset.
Specific measurements
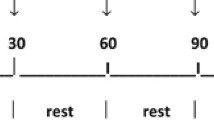
Protocol 1: Metabolic study. Protocol 1 included indirect calorimetry measures and standardized mixed meal tests (Figure 1). All participants initially selected completed Protocol 1 (n=10) (Table 1). In both EE and LE conditions, an identical test meal was provided during the indirect calorimetry/mixed meal test experiment. The test meal was the same for all subjects and consisted of typical Mediterranean food, including chickpeas Madrid-style (440 g) (Nestlé Spain SA, Esplugues de Llobregat, Barcelona, Spain) and a banana (180 g) with a total energy content of 777 kcal, 50% of energy was supplied by carbohydrate, 35% by fat and 15% by protein. Participants were required to finish the test meal within 30 min. Water was freely available during the whole experiment.
Indirect calorimetry. Subjects arrived in the indirect calorimetry room at the Catholic University of San Antonio at 11:30 h and stayed there until 20:00 h in a sedentary position, except for scheduled bathroom breaks, under the following controlled conditions: temperature 23 °C and relative humidity 52±2%. Indirect calorimetry (Oxicon Pro/Delta, VIASYS Healthcare, Germany) was performed in subjects in a calm state, in a reclining chair and after 30 min of initial rest. A facemask Triple V—highly precise (Oxycon Pro/Delta) was used to capture gas exchange. They were encouraged to keep silent and breathe normally during each measurement (20 min), and a total of four measurements were performed during the 4 h and 20 min of experiment (Figure 1). Oxygen (O2) consumption (ml min−1) and carbon dioxide (CO2) production (ml min−1) were measured. From these determinations, the Respiratory Quotient (RQ) was calculated and the derived Corrected Respiratory Quotient (CRQ) was obtained after correction for the metabolism of proteins (see below, Urine samples). Energy expenditure (kcal min−1) values were obtained according to the Weir equation.16, 17 Carbohydrate (CHO; g min−1) and fat oxidation (F; g min−1) were calculated from CRQ.
Urine samples. Urine was collected to measure urinary nitrogen by the Kjeldahl method as an estimate of protein oxidation at two different times on both calorimetry days. All urine was collected between 12:00 and 16:00 h, after having voided at 12:00 (container 1) and between 16:00 and 20:00 h (container 2). The containers of urine were kept on ice. Samples were stored at 4 °C until a Buchi solution was added (BÜCHI Labortechnik AG, Flawil, Switzerland). Protein oxidation was calculated by multiplying the urinary nitrogen excretion (g per 4 h) of urine container 1 (in the EE condition) or of urine container 2 (in the LE condition) by 6.25. No significant differences were found in urinary nitrogen excretion between the two containers (P>0.05). To obtain g min−1, the protein concentration was divided by 240 min (4 h).
Glucose tolerance (mixed meal test). Whole-blood glucose concentration was determined during the calorimetry experiment (see Figure 1). Glucose was assessed a few minutes before the test meal (LS) and every 30 min after the meal test: T30, T60, T90, T120, T150 (Figure 1). Blood glucose test strips were analyzed using Radiometer ABL 90 series (Radiometer Medical ApS, Copenhagen, Denmark). Area under the curve above baseline (AUC) for glucose for the first 150 min after the mixed meal was calculated with the trapezoid method.18
Protocol 2: Circadian-related study. Protocol 2 included assessments of the daily patterns of cortisol and Twrist. All the participants initially selected completed Protocol 2 (n=22) (Table 1).
Wrist temperature. The daily rhythm in Twrist was assessed continuously for 7 days using a temperature sensor (Thermochron iButton DS1921H, Dallas, Maxim, WI, USA) with a sensitivity of 0.1 °C and a sample rate of 10 min. It was attached to a double-layered cotton sport wristband, and the sensor surface was placed over the inside of the wrist on the radial artery of the non-dominant hand, as previously described by Sarabia et al.15 The information stored in the iButton was transferred through an adapter (DS1402D-DR8; IDC, Madrid, Spain) to a personal computer using iButton Viewer v.3.22 (Dallas Semiconductor MAXIM software provided by the manufacturer (Whitewater, WI, USA)). Data were recorded during the month of March, with outdoor temperatures averaging 21.3 °C (data obtained from the Meteorology National Agency, AEMET).
From the Twrist measures, the second-harmonic power (the power of the 12-h rhythm) was calculated using an integrated package for time-series analysis, ‘Circadianware’.19
Salivary cortisol. Saliva for cortisol measurements was collected on the sixth day of both the EE and LE conditions, using the Salivette system (Sarstedt, Barcelona, Spain).20 Samples were obtained in the morning (09:00 h), before either the early or late lunch time (13:00 h), and before bedtime (23:00 h). Cortisol was measured by radioimmunoassay (IZASA, Barcelona, Spain) with a detection limit of 0.2 nmol l−1. The intra- and interassay coefficient of variances was 4.0% for levels above and 10.0% for levels below 0.4 nmol l−1. All samples were maintained refrigerated at 4 °C until assaying.
Statistical methods in protocols 1 and 2. Analyses of data. Those variables that displayed a non-normal distribution were log-transformed. Student’s t-test was used to analyze possible differences in the general characteristics of the population between P1 and P2 (Table 1). Moreover, to study statistical differences between EE and LE for sleep variables (onset, offset and duration), a paired t-test was performed. To assess statistical differences between EE and LE in glucose control and indirect calorimetry patterns and in daily patterns of cortisol and Twrist, repeated measures of analysis of variance was performed. When statistical differences were found, a paired t-test was applied to identify differences between EE and LE conditions for each time point of measures. The fasting values for glucose, glucose AUC and fasting measures from indirect calorimetry were compared between the EE and LE conditions by paired t-tests. In energy expenditure, CRQ and substrate oxidation, each timing point represents the mean value of each 20-min continuous assessment.
Results
Our results of indirect calorimetry showed that resting energy expenditure prior to the meal was affected by meal timing, with lower values in the LE than in the EE condition (LE: 1.07±0.13 kcal min−1; EE: 1.12±0.14 kcal min−1; P=0.048). However, no significant differences were found in postprandial energy expenditure (Figure 2a).
The effect of meal timing on energy expenditure (a), CRQ (b) and carbohydrate oxidation (c). Each timing point represents the mean value of a 20-min continuous measurement. Repeated measures of analysis of variance (ANOVA) were performed. Fasting measures were compared between the EE and LA conditions by paired t-tests. *, significant differences between EE and LE (P<0.05).
Interestingly, LE resulted in a significantly lower pre-meal baseline CRQ (C0; LE: (Mean±s.d.) 0.75±0.50; EE: 0.82±0.08; P=0.0002; Figure 2b). Related, LE resulted in a different profile of CRQ following the meal (analysis of variance; P=0.019), with a significant difference at the 90-min measurement (C2; LE: 0.82± 0.36; EE: 0.85±0.07; P=0.030). These changes reflect a significantly lower utilization of carbohydrates at pre-meal baseline in LE versus EE (0.038±0.38 g min−1 versus 0.089±0.49 g min−1 P=0.006; Figure 2c).
Postprandial glucose AUC was significantly increased in the LE condition compared with the EE condition (LE: 102.6±30.8 mmol l−1 × h; EE: 70.0±32.9 mmol l−1 × h; P=0.002). In fact, LE increased AUC by 46% as compared with EE. Significant differences between LE and EE were also obtained in glucose concentrations at T90 and T120 (P=0.035 and P=0.031, respectively; Figure 3).
Effect of meal timing on glucose control. Glucose was assessed a few minutes before the test meal (BG0) and every half hour after the meal test (see Figure 1). Area under the curve above baseline (AUCs) for glucose for the first 150 min after the mixed meal was calculated with the trapezoid method.18 Decimal logarithms were used for AUC and paired t-test was used to evaluate AUC. *, significant differences between EE and LE (P<0.05).
The daily patterns of cortisol were also affected by meal timing (P=0.041; Figure 4), with a blunted daily cortisol profile in the LE condition compared with the EE condition because of significantly lower morning (LE: 22.11±10.50 nmol l−1; EE: 33.39±17.42 nmol l−1; P=0.001), and afternoon values (LE: 13.32±5.39 nmol l−1; EE: 17.97±6.92 nmol l−1; P=0.012), whereas values were similar at night (LE: 8.42±5.63 nmol l−1; EE: 8.87±9.68 nmol l−1; P=0.85).
Effect of meal timing on cortisol profiles. Salivary free cortisol values during the day (at 9:00, 13:00 and 23:00 h) in the two conditions: EE and LE; significant differences between EE (grey line) and LE (black line) were calculated by two-way ANOVA with repeated measurements (ANOVArm).When statistical differences were found by repeated measurements analysis, a paired t-test was applied at each timing point (*P<0.05). B, breakfast; L, lunch; D, dinner.
Figure 5 represents the average daily pattern of wrist temperature derived from 7 days of continuous recordings. Data indicated that LE resulted in changes in the Twrist pattern with a significant lower second-harmonic power (LE: 1.17±0.72 °C; EE: 1.78±1.23 °C; P=0.041). Further detailed analysis confirmed these results, with significant differences between both meal timing conditions in the postprandial timing period towards an attenuation of the postprandial increase of Twrist in LE as compared with EE (Figure 5 and Supplementary Figure 1).
Discussion
The results of this interventional study show that delaying the timing of an identical meal for a week resulted in decreased resting energy expenditure prior to the meal, unchanged postprandial energy expenditure, decreased fasting carbohydrate oxidation, decreased glucose tolerance, blunted daily profile of free cortisol concentrations and decreased thermal effect of food on Twrist.
Previous results of our group demonstrated that eating late was predictive of decreased weight-loss success during a 20-week intervention, although no significant differences were found in energy intake and estimated energy expenditure between the late and early eaters. Two potential limitations could be implicated in these results; one that this was an observational study and second that we estimated energy expenditure using the Harris–Benedict formula and self-reported physical activity (MET scores). We could not exclude the possibility that the groups had differences in resting energy expenditure not predicted by their weight, height, gender and age or in postprandial energy expenditure.
To address these aspects, we performed the current interventional study and we measured resting and postprandial energy expenditure by indirect calorimetry in two meal-timing conditions, LE and EE, with identical meals within the same subjects in a crossover design. Our results show that a delay of three and a half hours in lunch timing (from 13:00 to 16:30 h) resulted in decreased resting energy expenditure prior to the meal. However, no significant differences were found in postprandial energy expenditure. These slight changes in pre-meal energy expenditure do not seem sufficient to explain the previously described differences in weight loss between early eaters and late eaters. Further studies are required to measure the effect of early and late eating on energy expenditure across 24 h to assess whether meal timing affects energy expenditure at other times of day.
Nevertheless, fasting protein-corrected RQ and fasting carbohydrate oxidation were decreased in the LE as compared with the EE conditions. Previous studies have found that lower RQ values are significantly correlated with higher age, percent body fat, plasma glucose, free fatty acids and waist-hip ratio.21
In the current study, postprandial glucose tolerance was affected by meal timing. After the test meal, glucose levels were significantly higher in the LE than in the EE condition. In fact, LE increased AUC by 46% as compared with EE. These data point to a decreased glucose tolerance in LE. These results could be related to: (i) the Staub-Traugott effect, which states that plasma glucose concentrations after ingestion of an oral glucose load are higher if administered in the fasting state compared with the postprandial state.22 Indeed, one of the characteristics of the LE condition is the significantly longer fasting state which was 3.5 h longer than in EE; and (ii) the influence of the circadian system on glucose regulation, independent of the sleep/wake and fasting/feeding cycle.23 These combined effects may help explain why consuming the main meal later in the day results in decreased glucose tolerance.
From animal experimental studies, it is known that abnormal meal timing can disturb the phase relationship between the central circadian pacemaker and peripheral oscillators located in virtually all cells of the body, including metabolic tissues such as liver and pancreas, and lead to adverse metabolic effects such as glucose intolerance. In humans, misalignment between the central circadian pacemaker and the fasting/feeding and sleep/wake cycle has been shown to result in decreased glucose tolerance.2 Interestingly, our results are similar to those obtained by Gonnissen et al.,25 who studied the effect of circadian misalignment, by either advancing or delaying the fasting/feeding and sleep/wake cycle, on energy expenditure and glucose metabolism. The authors found a disturbance of the glucose metabolism and substrate oxidation, whereas energy balance was less affected by circadian misalignment, results that concur with our current study on meal timing.
The daily profile in free cortisol concentrations was also affected by meal timing in the current study. LE caused a blunted profile with lower morning and afternoon values as compared with EE, whereas night values were similar in both food timing conditions. A high daily variability of cortisol is a sign of the typical normal diurnal rhythm, with a peak in the morning, shortly after awakening, and low values in the evening close to bedtime. Lower variability or flattened cortisol rhythmicity has been related to chronic emotional or physical stress;26, 27 moreover, it has been related to obesity.28 Indeed, a similar blunting of the daily cortisol rhythm as that observed during our LE conditions has also been described in subjects suffering from metabolic syndrome as compared with healthy subjects.29 This blunted daily variability in cortisol may result in a reduction of the circadian signaling to peripheral clocks as has been previously proposed with a mathematical semimechanistic model: the authors suggested that as cortisol's amplitude decreases, cells gradually fall out of synchrony.30 The model also predicted a dynamic regime of entrainment when cortisol has a slightly decreased amplitude rhythm, where individual clock genes remain relatively synchronized among themselves but are phase shifted in relation to the entrainer.30 Previous work performed in twin studies shows that, although the nighttime nadir in cortisol values has a high genetic influence, the morning acrophase is mainly associated with environmental factors.31 Our results, based on within-subject comparisons, are consistent with this observation, with lunch timing influencing morning cortisol without an effect on evening cortisol. Further studies are required to determine the underlying mechanisms, and to resolve whether the endogenous circadian rhythm of cortisol is influenced by meal timing. Of note, the change in morning and afternoon cortisol cannot be explained by acute effects of the test meals, because times at which cortisol was assessed (09:00 and 13:00 h) occurred before the test meals in both conditions (13:00 and 16:30 h, for early and late, respectively). This suggests that there is a long-term effect of meal timing on the daily control of cortisol.
The current data show that delayed timing of an identical meal resulted in changes in the daily pattern of wrist temperature caused primarily by a decreased thermal effect of food (postprandial peak) in LE condition as compared with EE. We have previously shown that decreases of the second-harmonic power, reflecting in part a blunting of the postprandial peak, could be a marker of metabolic alterations32 and has been related to obesity and impaired weight loss.8, 9 In fact, in individuals undergoing a weight-loss program, low responders displayed a less marked postprandial peak in Twrist than high responders.9 Differences in this postprandial peak in Twrist are also the most notable findings in the currently observed daily patterns of temperature between EE and LE conditions. These differences in Twrist with meal timing may underlie the already demonstrated difficulties in losing weight of LE subjects.5
In summary, late timing of the main meal of the day (lunch in Spain) affects resting energy expenditure, glucose tolerance and oxidation, the daily variability of free cortisol concentrations, and the thermal effect of food on Twrist. Even though these effects seem to be of a small magnitude, this may be due to the fact that the meal timing intervention comprised only 1 week. Chronically eating at a later time of day may create metabolic disturbances of a larger magnitude and may be implicated in the metabolic alterations that characterize late eaters.
References
Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW . Circadian timing of food intake contributes to weight gain. Obesity (Silver Spring) 2009; 17: 2100–2102.
Scheer FAJL, Hilton MF, Mantzoros CS, Shea SA . Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci 2009; 106: 4453–4458.
Fonken LK, Workman JL, Walton JC, Weil ZM, Morris JS, Haim A et al. Light at night increases body mass by shifting the time of food intake. Proc Natl Acad Sci USA 2010; 107: 18664–18669.
Salgado-Delgado R, Angeles-Castellanos M, Saderi N, Buijs RM, Escobar C . Food intake during the normal activity phase prevents obesity and circadian desynchrony in a rat model of night work. Endocrinology 2010; 151: 1019–1029.
Garaulet M, Gomez-Abellan P, Alburquerque-Bejar JJ, Lee YC, Ordovas JM, Scheer FA . Timing of food intake predicts weight loss effectiveness. Int J Obes (Lond) 2013; 37: 604–611.
Stokkan KA, Yamazaki S, Tei H, Sakaki Y, Menaker M . Entrainment of the circadian clock in the liver by feeding. Science (New York, NY) 2001; 291: 490–493.
Patton DF, Mistlberger RE . Circadian adaptations to meal timing: neuroendocrine mechanisms. Front Neurosci 2013; 7: 185.
Corbalan-Tutau MD, Madrid JA, Ordovas JM, Smith CE, Nicolas F, Garaulet M . Differences in daily rhythms of wrist temperature between obese and normal-weight women: associations with metabolic syndrome features. Chronobiol Int 2011; 28: 425–433.
Bandin C, Martinez-Nicolas A, Ordovas JM, Madrid JA, Garaulet M . Circadian rhythmicity as a predictor of weight-loss effectiveness. Int J Obes (Lond) 2013; 38: 1083–1088.
Jakubowicz D, Barnea M, Wainstein J, Froy O . High caloric intake at breakfast vs dinner differentially influences weight loss of overweight and obese women. Obesity (Silver Spring) 2013; 21: 2504–2512.
Boulos Z, Terman M . Food availability and daily biological rhythms. Neurosci Biobehav Rev 1979; 4: 119–131.
Angeles-Castellanos M, Salgado-Delgado R, Rodriguez K, Buijs RM, Escobar C . The suprachiasmatic nucleus participates in food entrainment: a lesion study. Neuroscience 2010; 165: 1115–1126.
Son GH, Chung S, Choe HK, Kim HD, Baik SM, Lee H et al. Adrenal peripheral clock controls the autonomous circadian rhythm of glucocorticoid by causing rhythmic steroid production. Proc Natl Acad Sci U S A. 2008; 105: 20970–20975.
Perez-Llamas F, Garaulet M, Torralba C, Zamora S . [Development of a current version of a software application for research and practice in human nutrition (GRUNUMUR 2.0)]. Nutr Hosp 2012; 27: 1576–1582.
Sarabia JA, Rol MA, Mendiola P, Madrid JA . Circadian rhythm of wrist temperature in normal-living subjects A candidate of new index of the circadian system. Physiol Behav 2008; 95: 570–580.
da Rocha EE, Alves VG, da Fonseca RB . Indirect calorimetry: methodology, instruments and clinical application. Curr Opin Clin Nutr Metabol Care 2006; 9: 247–256.
Weir JB . New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 1949; 109: 1–9.
Allison DB, Paultre F, Maggio C, Mezzitis N, Pi-Sunyer FX . The use of areas under curves in diabetes research. Diabetes Care 1995; 18: 245–250.
Ortiz-Tudela E, Martinez-Nicolas A, Campos M, Rol MA, Madrid JA . A new integrated variable based on thermometry, actimetry and body position (TAP) to evaluate circadian system status in humans. PLoS Comput Biol 2010; 6: e1000996.
Kirschbaum C, Hellhammer DH . Salivary cortisol in psychoneuroendocrine research: recent developments and applications. Psychoneuroendocrinology 1994; 19: 313–333.
Rizzo MR, Mari D, Barbieri M, Ragno E, Grella R, Provenzano R et al. Resting metabolic rate and respiratory quotient in human longevity. J Clin Endocrinol Metabol 2005; 90: 409–413.
Lewis GF, McNally C, Blackman JD, Polonsky KS, Barron WM . Prior feeding alters the response to the 50-g glucose challenge test in pregnancy. The Staub-Traugott effect revisited. Diabetes Care 1993; 16: 1551–1556.
Van Cauter E, Blackman JD, Roland D, Spire JP, Refetoff S, Polonsky KS . Modulation of glucose regulation and insulin secretion by circadian rhythmicity and sleep. J Clin Invest 1991; 88: 934–942.
Leproult R, Holmback U, Van Cauter E . Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes 2014; 63: 1860–1869.
Gonnissen HK, Rutters F, Mazuy C, Martens EA, Adam TC, Westerterp-Plantenga MS . Effect of a phase advance and phase delay of the 24-h cycle on energy metabolism, appetite, and related hormones. Am J Clin Nutr 2012; 96: 689–697.
Chrousos GP, Gold PW . A healthy body in a healthy mind—and vice versa—the damaging power of ‘uncontrollable’ stress. J Clin Endocrinol Metabol 1998; 83: 1842–1845.
Lipiner-Friedman D, Sprung CL, Laterre PF, Weiss Y, Goodman SV, Vogeser M et al. Adrenal function in sepsis: the retrospective Corticus cohort study. Crit Care Med 2007; 35: 1012–1018.
Garcia-Prieto MD, Tebar FJ, Nicolas F, Larque E, Zamora S, Garaulet M . Cortisol secretary pattern and glucocorticoid feedback sensitivity in women from a Mediterranean area: relationship with anthropometric characteristics, dietary intake and plasma fatty acid profile. Clin Endocrinol 2007; 66: 185–191.
Corbalan-Tutau D, Madrid JA, Nicolas F, Garaulet M . Daily profile in two circadian markers ‘melatonin and cortisol’ and associations with metabolic syndrome components. Physiol Behav 2014; 123: 231–235.
Mavroudis PD, Scheff JD, Calvano SE, Lowry SF, Androulakis IP . Entrainment of peripheral clock genes by cortisol. Physiol Genomics 2012; 44: 607–621.
Linkowski P, Onderbergen AV, Kerkhofs M, Bosson D, Mendlewicz J, Cauter EV . Twin study of the 24-h cortisol profile evidence for genetic control of the human circadian clock. Am J Physiol 1993; 264 (2 Pt 1): WI 53190 USA E173–E181.
Corbalán-Tutau MD, Gómez-Abellán P, Madrid JA, Canteras M, Ordovás JM, Garaulet M . Toward a chronobiological characterization of obesity and metabolic syndrome in clinical practice. Clin Nutr 2014. In Press.
Acknowledgements
This work was supported by The Spanish Government of Science and Innovation (Project No. BFU2011-24720 and BFU2010-21945-C02-01) and Seneca Foundation (Project No. 15123/PI/10). Frank A.J.L. Scheer was supported in part by grants NHLBI R01 HL094806 and NIDDK R01 DK099512.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Bandín, C., Scheer, F., Luque, A. et al. Meal timing affects glucose tolerance, substrate oxidation and circadian-related variables: A randomized, crossover trial. Int J Obes 39, 828–833 (2015). https://doi.org/10.1038/ijo.2014.182
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.182
- Springer Nature Limited
This article is cited by
-
Maternal melatonin levels and temporal dietary intake: results from MY-CARE cohort study
BMC Pregnancy and Childbirth (2023)
-
Isocaloric diet is as effective as the hypocaloric diet in ameliorating symptoms in PCOS patients
International Journal of Diabetes in Developing Countries (2023)
-
Integration of Time-Based Recommendations with Current Pediatric Health Behavior Guidelines: Implications for Obesity Prevention and Treatment in Youth
Current Obesity Reports (2022)
-
Behavioral circadian phenotypes are associated with the risk of elevated body mass index
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2022)
-
Der Genotyp diktiert die Glukosetoleranz bei Spätessern mit
Info Diabetologie (2022)