Abstract
The T-cell immunoglobulin and mucin domain-containing protein 3 (TIM-3) is selectively expressed on terminally differentiated T helper 1 (Th1) cells and acts as a negative regulator that terminates Th1 responses. The dysregulation of TIM-3 expression on T cells is associated with several autoimmune phenotypes and with chronic viral infections; however, the mechanism of this regulation is unclear. In this study, we investigated the effect of DNA methylation on the expression of TIM-3. By analyzing the sequences of TIM-3 promoter regions in human and mouse, we identified a CpG island within the TIM-3 promoter and demonstrated that the promoter activity was controlled by DNA methylation. Furthermore, treatment with 5-aza-2′-deoxycytidine enhanced TIM-3 expression on mouse primary CD4+ T cells under Th0-, Th1- or Th2-polarizing conditions. Finally, pyrosequencing analysis revealed that the methylation level of the TIM-3 promoter gradually decreased after each round of T-cell polarization, and this decrease was inversely correlated with TIM-3 expression. These data suggest that the DNA methylation of the TIM-3 promoter cooperates with lineage-specific transcription factors in the control of Th-cell development. In conclusion, DNA methylation-based regulation of TIM-3 may provide novel insights into understanding the dysregulation of TIM-3 expression under pathogenic conditions.
Similar content being viewed by others
Introduction
The T-cell immunoglobulin and mucin domain-containing protein 3 (TIM-3) molecule is specifically expressed on terminally differentiated T helper 1 (Th1) cells and regulates Th1 cell-mediated immune responses.1 The ligand for TIM-3 was identified as galectin-9,2 a β-galactoside-binding lectin that induces T-cell apoptosis through the calcium–calpain–caspase-1 pathway.3 The roles of the galectin-9–TIM-3 pathway in the regulatory functions of T cells have been widely studied in animal models of autoimmune diseases, including autoimmune encephalomyelitis,2 autoimmune diabetes,4 rheumatoid arthritis5 and psoriasis.6 In addition, overexpression of galectin-9 has been demonstrated in several transplantation models to prolong graft survival through the downregulation of T-cell responses,7, 8, 9 which suggests that the galectin-9–TIM-3 pathway could be a therapeutic target. In addition, previous reports have demonstrated that the expression of TIM-3 is dysregulated on T cells from patients with multiple sclerosis,10 autoimmune hepatitis11, 12 or during chronic viral infections.13, 14, 15 These reports indicated that the galectin-9–TIM-3 pathway plays a pivotal role in the control of immune responses. However, the underlying mechanisms of the regulation of TIM-3 expression, especially under pathogenic conditions, are not fully understood.
Given the importance of TIM-3 in the regulation of T-cell immune responses, previous reports have focused on genetic association studies that analyze the single-nucleotide polymorphisms of the TIM-3 promoter in patients with allergic phenotypes16, 17, 18, 19 or childhood asthma20 and type 1 diabetes families.21 Although researchers have put considerable effort into the study of the genetics of TIM-3, the data from single-nucleotide polymorphism and linkage disequilibrium analysis do not provide insight into the possible mechanisms of the dysregulation of TIM-3 expression in these diseases, although it has been reported that TIM-3 is regulated by a Th1 transcription factor, T-bet.22 However, there is considerable expression of TIM-3 on T cells from T-bet–/– mice, signal transducer and activator of transcription (STAT)4–/– mice and T-bet–/– × STAT4–/– mice, which suggests that other transcription factors and different mechanisms are involved in the regulation of TIM-3 expression. Therefore, the regulation of TIM-3 expression on Th1 cells in different situations is not understood.
Recently, the role of epigenetic regulation in T-cell differentiation has attracted considerable attention. There is growing evidence that DNA methylation, histone modifications and microRNAs are involved in the control of lineage specificity and effector function of T-cell subsets (reviewed by Wilson et al.23 and Baumjohann et al.24). During Th-cell differentiation, cell division is accompanied by epigenetic changes that guide the production of lineage-specific cytokines and maintain the stability of the differentiated state.25, 26, 27 Because TIM-3 expression is restricted to selected cell types, the detailed mechanism of its regulation are unclear. We hypothesized that epigenetic regulation may be involved in the control of TIM-3 expression. In this study, we identified a CpG island within the promoter region of TIM-3 and analyzed the effect of DNA methylation on the promoter activity. Interestingly, treatment with the DNA methyltransferase (DNMT) inhibitor, 5-aza-2′-deoxycytidine (5-Aza) significantly increased TIM-3 expression on polarized Th1 and Th2 cells, but not on Th17 cells. Finally, using pyrosequencing analysis, we demonstrated that the methylation level of the TIM-3 promoter was inversely correlated with TIM-3 expression, indicating that DNA methylation was involved in the control of TIM-3 expression. These results suggest a novel regulatory mechanism for TIM-3 that can be applied to investigation of the dysregulation of TIM-3 expression under pathogenic conditions.
Results
Identification of human and mouse TIM-3 promoter
To examine the transcriptional activity in the 5′-flanking region of TIM-3, we obtained the DNA sequence from the UCSC Genome Bioinformatics website (http://genome.ucsc.edu/) and analyzed it using the rVISTA program. We found that there are three conserved noncoding sequences near the transcription start site of human and mouse TIM-3 (Figure 1a). By using CpG Island Explorer software, we identified a CpG island within the upstream sequence of both the human (Figure 1b) and mouse (Figure 1c) TIM-3 genes. To examine the transcriptional activity of the predicted TIM-3 promoter regions and evaluate the effect of DNA methylation on the activity of the TIM-3 promoter, we cloned different fragments of the DNA sequence from human (Figure 1b) and mouse (Figure 1c) TIM-3 into the pGL4.21 luciferase reporter or a CpG-free pCpGL luciferase reporter,28 and performed reporter assays. The pCpGL vector contains no CpG site; therefore, it can be used to evaluate the effect of DNA methylation on promoter activity. The longest fragments containing the predicted CpG island displayed the strongest promoter activity for both human (Figure 1d) and mouse (Figure 1e). To test whether the CpG island-containing fragments had independent promoter activity or acted as enhancers, we first performed the reporter assay and demonstrated that the human −1702 to −899 and mouse −3393 to −3210 constructs had no promoter activity (Figure 1d; data not shown). We then investigated whether DNA methylation regulated the promoter activity. As shown in Figures 1f–h, DNA methylation greatly reduced the promoter activity in both human (Figure 1f) and mouse (Figure 1g) promoter constructs. We noticed that the reporter activity of the promoter constructs, human −1192 to +42 (Figure 1f) and mouse −3238 to +67 (Figure 1g) was reduced by DNA methylation. This phenomenon was also observed when we used the mouse minimal promoter construct for an in vitro methylation and reporter assay (Figure 1h). Thus, we propose that the CpG island-containing fragment may have enhancer activity and that the promoter activity is controlled by other CpG dinucleotides close to the transcriptional start site. Both of these activities could be inhibited by DNA methylation. To confirm this hypothesis, we took advantage of a CpG-free pCpGL-cytomegalovirus/elongation factor luciferase reporter plasmid that contains a cytomegalovirus enhancer and a human elongation factor 1 promoter (also CpG free). We replaced the cytomegalovirus enhancer with mouse −3393 to −3210, mouse −3238 to −2179 or mouse −2267 to −1541 fragments (illustrated in Figure 1c) and analyzed the enhancer activity. Our data demonstrated that mouse −3393 to −3210 had weak enhancer activity and that its activity was controlled by DNA methylation, as demonstrated by the reduced enhancer activity of the in vitro methylated construct (Me-pCpGL −3393 to −3210; Figure 1i). Interestingly, this activity was not enhanced by phorbol 12-myristate 13-acetate/ionomycin stimulation or T-bet expression (Supplementary Information 1). The mouse −3238 to −2179 and the mouse −2267 to −1541 fragments showed no promoter activity (data not shown) and were used as a control for enhancer activity (Figure 1i). In summary, we identified the promoter region of TIM-3 and demonstrated that its promoter activity is controlled by DNA methylation of the enhancer region and proximal promoter. This is analyzed further below.
Identification of the Tim-3 promoter. (a) Comparison of human Tim-3 upstream sequence to that of mouse, rat and cattle. The sequences were obtained from the UCSC database and the interspecies conservation plot was generated using the mVISTA tool on the website. Schematic illustration of the putative promoter fragments of (b) human and (c) mouse Tim-3 used for the reporter assay. The CpG islands indicated in the figure were predicted using CpGIE software. Determination of (d) human and (e) mouse promoter activity by a luciferase reporter assay. Effect of (f) human and (g and h) mouse promoter methylation on reporter assays. To investigate the effect of CpG methylation on the activity of the Tim-3 promoter, the promoter fragments were cloned into a CpG-free vector for an in vitro methylation and reporter assay. (i) Enhancer activity assay. Putative enhancer fragments were cloned into a CpG-free EF1A-promoter/enhancer cassette and the enhancer activity was evaluated. This construct was further methylated in vitro to evaluate the effect of DNA methylation on enhancer activity. Representative results from at least three independent experiments are shown. CNS, conserved nucleotide sequence. Paired t-test; **P<0.01.
Effects of DNMT inhibitor on transcription of TIM-3 and lineage-specific transcription factors in Th-cell subsets
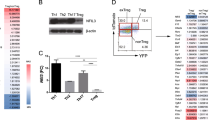
To investigate whether DNA methylation regulates TIM-3 expression and restricts TIM-3 expression on Th1 cells, we analyzed TIM-3 expression on different Th subsets. Naive CD4+ T cells were cultured under Th0-, Th1-, Th2- and Th17-polarizing conditions and in interleukin (IL)-27 condition (IL-27 promotes early induction of Th1 differentiation29) in the presence of 0.5 μm 5-Aza or 0.001% dimethyl sulfoxide (DMSO, solvent control; we confirmed that this concentration did not alter the T-cell differentiation and TIM-3 expression; see Supplementary Information 2). We found that transcription of TIM-3 was relatively higher in the cells cultured in Th1-polarizing and IL-27-stimulated conditions than in cells cultured in the other conditions, which is consistent with the previous finding that TIM-3 is preferentially expressed on Th1 cells.1 Interestingly, treatment of T cells with 5-Aza enhanced TIM-3 transcription under all stimulation conditions except Th17-polarizing conditions (Figure 2a). Although we cannot rule out that 5-Aza treatment increases TIM-3 expression through the induction of T-bet, which has been demonstrated to induce TIM-3 expression,22 the increased TIM-3 transcription in the IL-27-stimulated condition was independent of increased T-bet expression (Figure 2b), suggesting a T-bet-independent pathway in the control of TIM-3 expression. Further, the expression of GATA-3 (Figure 2c) and RORγt (Figure 2d) was not significantly changed by 5-Aza treatment of Th2 and Th17 cells, respectively. Interestingly, 5-Aza treatment preferentially promoted Th1-related gene transcription (Figures 2a and b) and inhibited RORγt expression in Th0 and Th1 cells (Figure 2d). Collectively, our data indicated that 5-Aza facilitates TIM-3 expression directly through DNA demethylation of its promoter and/or induction of the Th1-specific transcription factor, T-bet. In addition, because 5-Aza treatment did not alter the differentiation process of Th2 and Th17 cells, these two lineage-specific transcription factors may not regulate TIM-3 expression.
Quantitative PCR analysis of Tim-3, T-bet, Gata-3 and Rorc expression in mouse primary T cells under different polarizing conditions in the presence of 5-Aza. (a) Tim-3, (b) T-bet, (c) Gata-3 and (d) Rorc. DMSO, solvent control (0.001%); DNA methyltransferase inhibitor, 5-Aza (0.5 μm). Data are presented as mean±s.e.m. Representative results from at least three independent experiments. Paired t-test; significance was set at P<0.05 (*).
Effect of DNMT inhibitor on TIM-3 expression and cytokine expression in Th-cell subsets
We next analyzed TIM-3 and cytokine expression under different Th-cell-polarizing conditions in the presence of DMSO or 5-Aza. Our data revealed that TIM-3 was mainly expressed on Th1 cells; however, Th0 and Th2 cells also express TIM-3 to a lesser extent after stimulation (Figure 3a). Interestingly, we found that expression of TIM-3 is significantly increased in the presence of 5-Aza under Th0-, Th1- and Th2-polarizing conditions (Figure 3a; Supplementary Information 3a). Strikingly, TIM-3 is barely expressed on Th17 cells and 5-Aza treatment (Figure 3a), even with 5 μm 5-Aza (Supplementary Information 4), does not induce TIM-3 expression on these cells. To determine the efficiency of the T-cell polarization experiment and the impact of DNA demethylation on lineage commitment, we analyzed the cytokine expression of each population. Our data showed that 5-Aza treatment enhances interferon-γ (IFN-γ; Figure 3b) and IL-4 (Figure 3c; Supplementary Information 3b) expression in Th1 and Th2 cells, respectively, and also enhances IFN-γ expression under Th0- and Th2-polarizing conditions (Figure 3b), which suggests that DNA methylation regulates the stringency of IFN-γ expression after lineage commitment. Again, 5-Aza treatment did not alter cytokine expression in Th17 cells (Figures 3b–d), suggesting that DNA methylation may not regulate IL-17 expression or that of the Th17-specific transcription factors that control the stringency of Th17 cells. In summary, we demonstrated that DNA demethylation facilities TIM-3 expression under Th0-, Th1- and Th2-polarizing conditions, which prompted us to identify the CpG sites within the TIM-3 promoter that might be involved in the control of TIM-3 expression.
Flow cytometric analysis of TIM-3 and cytokine expression in CD4+ T cells under Th0-, Th1-, Th2- and Th17-polarizing conditions in the presence of 5-Aza. Purified CD4+ T cells were stimulated in the indicated conditions for 3 days and the expression of (a) TIM-3, (b) IFN-γ, (c) IL-4 and (d) IL-17 was analyzed by flow cytometry. Data are presented as mean±s.e.m. Unpaired t-test; significance was set at P<0.05 (*).
Pyrosequencing analysis of the CpG island within the TIM-3 promoter
It is possible that nonspecific demethylation by 5-Aza treatment causes secondary effects that induce the expression of TIM-3 on Th cells under polarizing conditions, although the low dose of 5-Aza that we used should minimize the side effects of global demethylation. To analyze the correlation between DNA methylation and TIM-3 expression directly, we analyzed the methylation status of the CpG sites in the TIM-3 promoter by bisulfite pyrosequencing. Because we have identified that the enhancer region contains a CpG island and that the enhancer activity is controlled by DNA methylation, we first analyzed the 17 CpG sites within the CpG island-containing region 1 (Figure 4a) of the TIM-3 promoter in Th1-polarized cells. The methylation status of region 1 was only slightly decreased in Th1-polarized cells, even those treated with 5-Aza, compared with that in naive CD4+ T cells (Figure 4b). We also analyzed the methylation status of region 1 of Th0-, Th2- and Th17-polarized cells, and found that the methylation status was also slightly decreased in 5-Aza-treated Th0 and Th2 cells, whereas Th17 cells, which express low levels of TIM-3, showed high levels of DNA methylation (Supplementary Information 5a). To determine whether the demethylation of CpG sites in region 1 (Figure 4a) are crucial for the regulation of TIM-3 expression, we stimulated Th1 cells for several rounds in polarizing conditions to induce stable TIM-3 expression as described previously,1 and analyzed the methylation level of region 1. We found that the expression of TIM-3 on the cell surface markedly increased after the second round of stimulation (Figure 4c). Unexpectedly, the methylation status of region 1 was not significantly decreased (Supplementary Information 5b). Although we did not identify a CpG island within the mouse minimal promoter region, we have demonstrated that DNA methylation markedly reduces its activity (Figure 1h). Thus, we analyzed the methylation level of the CpG sites in region 2 of the minimal promoter (Figure 4a). CD4+ T cells after one round of stimulation showed similar methylation levels to naive CD4+ T cells, even when treated with 5-Aza (Supplementary Information 5c). Interestingly, we found that after four rounds of stimulation, Th1 cells displayed reduced methylation in region 2 and expressed high levels of TIM-3, which suggests that TIM-3 expression induced by repeated stimulation correlates with DNA demethylation (Supplementary Information 5c). Thus, we stimulated cells for four rounds in Th1-, Th2- and Th17-polarizing conditions, and analyzed TIM-3 expression and the methylation status of region 2. We found that TIM-3 expression increased after each round of stimulation (Figure 4c), and that this was inversely correlated with the methylation status of region 2 (Figures 4d–f). These data suggested that DNA demethylation in region 2 is crucial for TIM-3 expression, and that the enhancer region plays only a minor role in the promotion of TIM-3 expression. Interestingly, under certain conditions, DNA methylation may be higher in the hierarchy of control of TIM-3 expression than are lineage-specific transcription factors.
Pyrosequencing analysis of the methylation level of CpG motifs within the Tim-3 promoter. (a) CpG sites within the enhancer (region 1) and minimal promoter (region 2). (b) Methylation level of 17 CpG sites within region 1 of the Tim-3 promoter. DNA from naive CD4+ T cells and DMSO-treated or 5-Aza-treated Th1 cells was extracted for determination of the methylation level. (c) Expression of Tim-3 in Th cells after repetitive stimulation. Naive CD4+ T cells were subjected to four rounds of polarization in the indicated condition, and the expression of Tim-3 was determined after each round of stimulation. Methylation levels of the four CpG sites within the Tim-3 minimal promoter under (d) Th1-, (e) Th2- and (f) Th17-polarizing conditions were determined by pyrosequencing. Viable cells were collected from each round of stimulation and DNA was extracted for pyrosequencing analysis.
Discussion
Epigenetic mechanisms for regulation of gene expression have been widely studied in many fields, including embryogenesis, stem cell biology, oncology and immunology. There is growing evidence that histone modification, DNA methylation and microRNAs control the lineage stringency and plasticity of Th cells.30 TIM-3 plays a crucial role in the control of T-cell responses in autoimmunity,31 transplant acceptance,7, 8, 32 chronic viral infections13, 14, 33 and immune surveillance of tumors.34 In this study, we identified a CpG island within the TIM-3 enhancer region and demonstrated that the enhancer activity was controlled by DNA methylation. More importantly, methylation level of the four CpG sites within the minimal promoter region was highly correlated with the level of TIM-3 expression on T cells. In addition to the role of cytokine signaling and lineage-specific transcription factors in the control of the stringency of TIM-3 expression on Th1 cells, it is noteworthy that the DNA methylation status controls the stable levels of TIM-3 expression in terminally differentiated cells. These findings may help to clarify the mechanism of the dysregulation of TIM-3 expression in autoimmune disorders and chronic infections. These findings also provide a new perspective by indicating that epigenetic mechanisms regulate not only T-cell differentiation and effector function (expression of transcription factors and effector cytokines), but also T-cell homeostasis (TIM-3-expressing T cells are susceptible to galectin-9-mediated apoptosis).
Although it is well documented that TIM-3 is specifically expressed on Th1 cells1 and dendritic cells,35 Th17 cells also express low levels of TIM-3 in a T-bet-dependent manner after immunization and restimulation.36 Thus, 5-Aza-induced TIM-3 expression under Th0-, Th1- and Th2-polarizing conditions may be partially the result of slightly increased T-bet expression. However, we did not detect a significant level of TIM-3 expression on one round-polarized Th17 cells even when treated with 5-Aza, which suggests that IL-6 and/or transforming growth factor-β may suppress the induction of TIM-3 at an early stage. It was unexpected that Th2 and Th17 cells expressed TIM-3 after several rounds of polarization (Figure 4c). In this situation, it is possible that T-cell receptor/CD28-induced signal transduction and/or T-cell proliferation accompanied by passive DNA demethylation induce TIM-3 expression. Previous studies have demonstrated that TIM-3 is expressed on Th1 cells after the third round of polarization in in vitro cultures, even in the absence of the Th1-specific transcription factors T-bet and STAT4.1, 22 Besides, previous reports also indicated that TIM-3 is not exclusively expressed on Th1 cells under certain stimulation conditions. Sanchez-Fueyo et al.31 have demonstrated that Th2 cells also express TIM-3 after repeated stimulation, albeit the expression level is lower than Th1 cells. Besides, Th17 cells also express low levels of TIM-3 in a T-bet-dependent manner after immunization and restimulation.36 The discrepancy of these results may be due to different experimental settings (for example, stimulation condition, mouse strains and antibody clones used for staining). Altogether, these results suggested that there may be methylation-dependent regulatory mechanisms that are more efficient than, or synergistic with, Th1-specific transcription factors for the control of TIM-3 expression. Moreover, a decreased methylation status of the four CpG sites within the minimal promoter may facilitate T-bet-mediated transcription of TIM-3, even with the low level of T-bet expression in Th0, Th2 and Th17 cells.
DNA methylation has been implicated in the regulation of the expression in T cells of cytokines, including IFN-γ,37 IL-2(ref. 38) and IL-3,39 and of T-cell lineage markers including perforin, CD4 and CD8, suggesting that DNA methylation may help to establish and/or maintain the different effector responses exhibited by CD4+ and CD8+ T cells.40, 41 Moreover, genetic ablation of DNMT in T cells has demonstrated that DNMT1 is crucial for the development, function and survival of T cells,42, 43 whereas DNMT3a controls lineage stability after differentiation.44 The expression of Foxp3 in naturally occurring regulatory T cells is also controlled by DNA methylation. Analysis of the promoter region of the Foxp3 gene showed that this noncoding region contains CpG motifs, which are completely demethylated in thymic regulatory T cells, but heavily methylated in conventional T cells and peripheral-induced regulatory T cells.45, 46 These results suggested that, in coordination with lineage-specific transcription factors, DNA methylation controls accessibility to the promoter or gene in the regulation of gene expression in Th cells.
It has been demonstrated that under pathogenic conditions, such as during chronic viral infections in mice, demethylation of the promoter region of the pdcd-1 gene results in a high level of expression of the inhibitory molecule PD-1 on T cells, which is associated with clonal exhaustion.47 In clinical studies, aberrant signal transduction leads to hypomethylation of the promoter region of methylation-sensitive genes (LFA-1, CD70, CD40L and perforin) in T cells, which causes T-cell overactivation and leads to autoimmune diseases such as lupus erythematosus.48, 49, 50 Thus, it is possible that the dysregulation of TIM-3 expression in chronic viral infections13 and autoimmune diseases10 may be the result of abnormal regulation of DNA methylation of the TIM-3 promoter. We are now studying the regulation of TIM-3 in an autoimmune diabetes mouse model. In our preliminary results, we found that CD4+ T cells from the inflammatory pancreas expressed predominant IFN-γ but less TIM-3. Besides, by pyrosequencing analysis, these CD4+ T cells maintained high methylation level on the TIM-3 promoter. Our data suggested that in autoimmune diabetes, dysregulated demethylation of TIM-3 promoter reduced TIM-3 expression and eventually caused uncontrolled Th1 responses (our unpublished data). However, the detailed mechanisms of, for example, the regulation of DNMT expression in T cells under T-cell receptor and/or cytokine stimulation, or the process of active DNA demethylation by Tet proteins51 during T-cell activation, need to be further investigated.
Materials and methods
Prediction of promoters and CpG island analysis
The upstream sequences of TIM-3 were obtained from the UCSC Genome database (4000 base pairs) and were subjected to comparative analysis using the rVISTA program.52 The putative promoter region and CpG islands within these sequences were analyzed using website software and the CpGIE program, respectively.
Construction of luciferase reporter plasmids and in vitro DNA methylation
The promoter fragments were cloned into a pGL4.21 luciferase vector (Promega, Mannheim, Germany) and CpG-free pCpGL or pCpGL-cytomegalovirus/elongation factor 1 luciferase vectors,28 depending on the experiment. Primer sets for cloning the promoter fragment are listed in Table 1. To determine the effects of DNA methylation on promoter/enhancer activity, the constructed pCpGL and pCpGL-elongation factor vectors were subjected to in vitro methylation with SssI methylase in the presence of S-adenosylmethionine (New England Biolabs, Ipswich, MA, USA). The efficiency of methylation was evaluated using restriction enzymes HpaII (methylation sensitive) and MspI (methylation insensitive), respectively.
Electroporation of T cells and reporter assay
Human and mouse promoter constructs were transfected into Jurkat and EL4 cell lines, respectively, by electroporation. A total of 107 cells were cotransfected with 20 μg of promoter constructs and 0.4 μg of phRL-TK Renilla plasmid (Promega, Mannheim, Germany) using an ECM830 electroporation system (BTX Harvard Apparatus, Holliston, MA, USA; Jurkat cells: 290 V, 20 ms; EL4 cells: 225 V, 35 ms). For the in vitro methylation of plasmids, 2.5 × 106 cells were prepared in Ingenio Electroporation Solution (Mirus Bio LLC, Madison, WI, USA) and cotransfected with 2 μg of promoter constructs and 0.04 μg of phRL-TK Renilla plasmid. After 24 h, cell lysates were assayed for firefly and Renilla luciferase activity using the Dual-Luciferase Reporter Assay System (Promega) on a Packard TopCount Microplate Scintillation Counter (PerkinElmer, Shelton, CT, USA). The firefly luciferase activity of individual transfections was normalized against their Renilla luciferase activity. Data are presented as relative luciferase units (luciferase/Renilla).
T-cell polarization and flow cytometry
CD4+CD25– T cells and CD4+CD62L+ T cells (naive CD4 T cells) were isolated from BALB/c mice using the BD IMag Cell Separation System (BD Pharmingen, San Jose, CA, USA). A total of 2 × 106 cells were stimulated with IL-2 (5 ng ml−1), and plate-bound anti-CD3 (1 μg per well) and anti-CD28 (1 μg ml−1) monoclonal antibodies for 3 days in 24-well plates under conditions for polarizing Th0 (anti-IFN-γ, 5 μg ml−1; anti-IL-4, 5 μg ml−1), Th1 (IL-12, 10 μg ml−1; anti-IL-4, 5 μg ml−1 or IL-27, 10 μg ml−1; anti-IL-4, 5 μg ml−1), Th2 (IL-4, 10 μg ml−1; anti-IFN-γ, 5 μg ml−1) and Th17 (transforming growth factor-β, 5 ng ml−1; IL-6, 10 ng ml−1; anti-IFN-γ, 5 μg ml−1; anti-IL-4, 5 μg ml−1). 5-Aza-2′-deoxycytidine (0.5 μm) was added at the beginning of culture. For intracellular cytokine staining, the T cells were stimulated for 4 h with phorbol 12-myristate 13-acetate and ionomycin in the presence of monensin. All chemicals were from Sigma-Aldrich (St Louis, MO, USA). Cells were stained with anti-CD4 (RM4-5), anti-IFN-γ (XMG1.2), anti-IL-4, anti-IL-17 (TC11-18H10.1), anti-TIM-3 (B8.2C12) and isotype antibodies (BioLegend, San Diego, CA, USA). Cells were analyzed using a FACSCalibur flow cytometer and CellQuest software (BD Pharmingen). For the analysis of the DNA methylation level of the TIM-3 promoter after each round of polarization, cells were polarized for 3 days and rested for 2 days in the presence of IL-2 (5 ng ml−1) before the next round of polarization. Viable cells from each round of polarization were isolated using Histopaque-1077 (Sigma-Aldrich) density gradient sedimentation.
Quantitative reverse transcription PCR analysis
After Th cells were polarized for 3 days, RNA was extracted using a NucleoSpin RNA kit (Macherey-Nagel GmbH, Duren, Germany) and converted to cDNA using a SuperScript III synthesis kit (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. The primers used for quantitative reverse transcription PCR using the SYBR Green method are listed in Table 2.
DNA extraction, bisulfite conversion and pyrosequencing analysis
Genomic DNA was extracted using a QIAamp DNA Mini kit (Qiagen, Hilden, Germany). One microgram of genomic DNA was subjected to sodium bisulfite treatment using an EZ DNA Methylation kit (Zymo Research, Orange, CA, USA) and the treated genomic DNA was used for pyrosequencing. The CpG sites within the CpG island or the minimal promoter region were first amplified by PCR using various primer sets and the PCR product was used for pyrosequencing analysis. PCR was performed in a 20-μl reaction mixture containing 1-μl-bisulfite-converted DNA, 2 × RBC SensiZyme HotStart Taq Mastermix (RBC Bioscience Corp., Taipei, Taiwan) and primers, using the following program: 95 °C for 15 min, then 49 cycles of 95 °C for 30 s, followed by 62 °C for 30 s and 72 °C for 30 s, with a final extension at 72 °C for 10 min. The primer sequences for pyrosequencing are listed in Table 3.
References
Monney L, Sabatos CA, Gaglia JL, Ryu A, Waldner H, Chernova T et al. Th1-specific cell surface protein TIM-3 regulates macrophage activation and severity of an autoimmune disease. Nature 2002; 415: 536–541.
Zhu C, Anderson AC, Schubart A, Xiong H, Imitola J, Khoury SJ et al. The TIM-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat Immunol 2005; 6: 1245–1252.
Kashio Y, Nakamura K, Abedin MJ, Seki M, Nishi N, Yoshida N et al. Galectin-9 induces apoptosis through the calcium-calpain-caspase-1 pathway. J Immunol 2003; 170: 3631–3636.
Chou FC, Shieh SJ, Sytwu HK . Attenuation of Th1 response through galectin-9 and T-cell Ig mucin 3 interaction inhibits autoimmune diabetes in NOD mice. Eur J Immunol 2009; 39: 2403–2411.
Seki M, Oomizu S, Sakata KM, Sakata A, Arikawa T, Watanabe K et al. Galectin-9 suppresses the generation of Th17, promotes the induction of regulatory T cells, and regulates experimental autoimmune arthritis. Clin Immunol 2008; 127: 78–88.
Niwa H, Satoh T, Matsushima Y, Hosoya K, Saeki K, Niki T et al. Stable form of galectin-9, a TIM-3 ligand, inhibits contact hypersensitivity and psoriatic reactions: a potent therapeutic tool for Th1- and/or Th17-mediated skin inflammation. Clin Immunol 2009; 132: 184–194.
Chou FC, Kuo CC, Wang YL, Lin MH, Linju Yen B, Chang DM et al. Overexpression of galectin-9 in islets prolongs grafts survival via downregulation of Th1 responses. Cell Transplant 2013; 22: 2135–2145.
He W, Fang Z, Wang F, Wu K, Xu Y, Zhou H et al. Galectin-9 significantly prolongs the survival of fully mismatched cardiac allografts in mice. Transplantation 2009; 88: 782–790.
Wang F, He W, Yuan J, Wu K, Zhou H, Zhang W et al. Activation of TIM-3-galectin-9 pathway improves survival of fully allogeneic skin grafts. Transpl Immunol 2008; 19: 12–19.
Koguchi K, Anderson DE, Yang L, O'Connor KC, Kuchroo VK, Hafler DA . Dysregulated T cell expression of TIM3 in multiple sclerosis. J Exp Med 2006; 203: 1413–1418.
Li H, Wu K, Tao K, Chen L, Zheng Q, Lu X et al. TIM-3/galectin-9 signaling pathway mediates T-cell dysfunction and predicts poor prognosis in patients with hepatitis B virus-associated hepatocellular carcinoma. Hepatology 2012; 56: 1342–1351.
Liberal R, Grant CR, Holder BS, Ma Y, Mieli-Vergani G, Vergani D et al. The impaired immune regulation of autoimmune hepatitis is linked to a defective galectin-9/tim-3 pathway. Hepatology 2012; 56: 677–686.
Jones RB, Ndhlovu LC, Barbour JD, Sheth PM, Jha AR, Long BR et al. TIM-3 expression defines a novel population of dysfunctional T cells with highly elevated frequencies in progressive HIV-1 infection. J Exp Med 2008; 205: 2763–2779.
McMahan RH, Golden-Mason L, Nishimura MI, McMahon BJ, Kemper M, Allen TM et al. TIM-3 expression on PD-1+ HCV-specific human CTLs is associated with viral persistence, and its blockade restores hepatocyte-directed in vitro cytotoxicity. J Clin Invest 2010; 120: 4546–4557.
Golden-Mason L, Palmer BE, Kassam N, Townshend-Bulson L, Livingston S, McMahon BJ et al. Negative immune regulator TIM-3 is overexpressed on T cells in hepatitis C virus infection and its blockade rescues dysfunctional CD4+ and CD8+ T cells. J Virol 2009; 83: 9122–9130.
Zhang J, Daley D, Akhabir L, Stefanowicz D, Chan-Yeung M, Becker AB et al. Lack of association of TIM3 polymorphisms and allergic phenotypes. BMC Med Genet 2009; 10: 62.
Chae SC, Park YR, Lee YC, Lee JH, Chung HT . The association of TIM-3 gene polymorphism with atopic disease in Korean population. Hum Immunol 2004; 65: 1427–1431.
Chae SC, Park YR, Shim SC, Yoon KS, Chung HT . The polymorphisms of Th1 cell surface gene TIM-3 are associated in a Korean population with rheumatoid arthritis. Immunol Lett 2004; 95: 91–95.
Gao PS, Mathias RA, Plunkett B, Togias A, Barnes KC, Beaty TH et al. Genetic variants of the T-cell immunoglobulin mucin 1 but not the T-cell immunoglobulin mucin 3 gene are associated with asthma in an African American population. J Allergy Clin Immunol 2005; 115: 982–988.
Zhang CC, Wu JM, Cui TP, Wang P, Pan SX . [Study on relationship between polymorphism sites of TIM-3 and allergic asthma in a population of adult Hans from Hubei province of China]. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2006; 23: 74–77.
Bruck P, Ramos-Lopez E, Bartsch W, Bohme A, Badenhoop K . TIM-3 polymorphisms in type 1 diabetes families. J Hum Genet 2008; 53: 559–564.
Anderson AC, Lord GM, Dardalhon V, Lee DH, Sabatos-Peyton CA, Glimcher LH et al. T-bet, a Th1 transcription factor regulates the expression of TIM-3. Eur J Immunol 2010; 40: 859–866.
Wilson CB, Rowell E, Sekimata M . Epigenetic control of T-helper-cell differentiation. Nat Rev Immunol 2009; 9: 91–105.
Baumjohann D, Ansel KM . MicroRNA-mediated regulation of T helper cell differentiation and plasticity. Nat Rev Immunol 2013; 13: 666–678.
Bird JJ, Brown DR, Mullen AC, Moskowitz NH, Mahowald MA, Sider JR et al. Helper T cell differentiation is controlled by the cell cycle. Immunity 1998; 9: 229–237.
Young HA, Ghosh P, Ye J, Lederer J, Lichtman A, Gerard JR et al. Differentiation of the T helper phenotypes by analysis of the methylation state of the IFN-gamma gene. J Immunol 1994; 153: 3603–3610.
Valapour M, Guo J, Schroeder JT, Keen J, Cianferoni A, Casolaro V et al. Histone deacetylation inhibits IL4 gene expression in T cells. J Allergy Clin Immunol 2002; 109: 238–245.
Klug M, Rehli M . Functional analysis of promoter CpG methylation using a CpG-free luciferase reporter vector. Epigenetics 2006; 1: 127–130.
Owaki T, Asakawa M, Morishima N, Hata K, Fukai F, Matsui M et al. A role for IL-27 in early regulation of Th1 differentiation. J Immunol 2005; 175: 2191–2200.
Kanno Y, Vahedi G, Hirahara K, Singleton K, O'Shea JJ . Transcriptional and epigenetic control of T helper cell specification: molecular mechanisms underlying commitment and plasticity. Annu Rev Immunol 2012; 30: 707–731.
Sanchez-Fueyo A, Tian J, Picarella D, Domenig C, Zheng XX, Sabatos CA et al. TIM-3 inhibits T helper type 1-mediated auto- and alloimmune responses and promotes immunological tolerance. Nat Immunol 2003; 4: 1093–1101.
Sabatos CA, Chakravarti S, Cha E, Schubart A, Sanchez-Fueyo A, Zheng XX et al. Interaction of TIM-3 and TIM-3 ligand regulates T helper type 1 responses and induction of peripheral tolerance. Nat Immunol 2003; 4: 1102–1110.
Vali B, Jones RB, Sakhdari A, Sheth PM, Clayton K, Yue FY et al. HCV-specific T cells in HCV/HIV co-infection show elevated frequencies of dual TIM-3/PD-1 expression that correlate with liver disease progression. Eur J Immunol 2010; 40: 2493–2505.
Klibi J, Niki T, Riedel A, Pioche-Durieu C, Souquere S, Rubinstein E et al. Blood diffusion and Th1-suppressive effects of galectin-9-containing exosomes released by Epstein-Barr virus-infected nasopharyngeal carcinoma cells. Blood 2009; 113: 1957–1966.
Anderson AC, Anderson DE, Bregoli L, Hastings WD, Kassam N, Lei C et al. Promotion of tissue inflammation by the immune receptor TIM-3 expressed on innate immune cells. Science 2007; 318: 1141–1143.
Chen Y, Langrish CL, McKenzie B, Joyce-Shaikh B, Stumhofer JS, McClanahan T et al. Anti-IL-23 therapy inhibits multiple inflammatory pathways and ameliorates autoimmune encephalomyelitis. J Clin Invest 2006; 116: 1317–1326.
Penix LA, Sweetser MT, Weaver WM, Hoeffler JP, Kerppola TK, Wilson CB . The proximal regulatory element of the interferon-gamma promoter mediates selective expression in T cells. J Biol Chem 1996; 271: 31964–31972.
Bruniquel D, Schwartz RH . Selective, stable demethylation of the interleukin-2 gene enhances transcription by an active process. Nat Immunol 2003; 4: 235–240.
Fitzpatrick DR, Shirley KM, McDonald LE, Bielefeldt-Ohmann H, Kay GF, Kelso A . Distinct methylation of the interferon gamma (IFN-gamma) and interleukin 3 (IL-3) genes in newly activated primary CD8+ T lymphocytes: regional IFN-gamma promoter demethylation and mRNA expression are heritable in CD44(high)CD8+ T cells. J Exp Med 1998; 188: 103–117.
Makar KW, Wilson CB . DNA methylation is a nonredundant repressor of the Th2 effector program. J Immunol 2004; 173: 4402–4406.
Sellars M, Huh JR, Day K, Issuree PD, Galan C, Gobeil S et al. Regulation of DNA methylation dictates Cd4 expression during the development of helper and cytotoxic T cell lineages. Nat Immunol 2015; 16: 746–754.
Lee PP, Fitzpatrick DR, Beard C, Jessup HK, Lehar S, Makar KW et al. A critical role for Dnmt1 and DNA methylation in T cell development, function, and survival. Immunity 2001; 15: 763–774.
Makar KW, Perez-Melgosa M, Shnyreva M, Weaver WM, Fitzpatrick DR, Wilson CB . Active recruitment of DNA methyltransferases regulates interleukin 4 in thymocytes and T cells. Nat Immunol 2003; 4: 1183–1190.
Gamper CJ, Agoston AT, Nelson WG, Powell JD . Identification of DNA methyltransferase 3a as a T cell receptor-induced regulator of Th1 and Th2 differentiation. J Immunol 2009; 183: 2267–2276.
Baron U, Floess S, Wieczorek G, Baumann K, Grutzkau A, Dong J et al. DNA demethylation in the human FOXP3 locus discriminates regulatory T cells from activated FOXP3(+) conventional T cells. Eur J Immunol 2007; 37: 2378–2389.
Ohkura N, Hamaguchi M, Morikawa H, Sugimura K, Tanaka A, Ito Y et al. T cell receptor stimulation-induced epigenetic changes and Foxp3 expression are independent and complementary events required for Treg cell development. Immunity 2012; 37: 785–799.
Youngblood B, Oestreich KJ, Ha SJ, Duraiswamy J, Akondy RS, West EE et al. Chronic virus infection enforces demethylation of the locus that encodes PD-1 in antigen-specific CD8(+) T cells. Immunity 2011; 35: 400–412.
Gorelik G, Richardson B . Aberrant T cell ERK pathway signaling and chromatin structure in lupus. Autoimmun Rev 2009; 8: 196–198.
Gorelik G, Fang JY, Wu A, Sawalha AH, Richardson B . Impaired T cell protein kinase C delta activation decreases ERK pathway signaling in idiopathic and hydralazine-induced lupus. J Immunol 2007; 179: 5553–5563.
Deng C, Kaplan MJ, Yang J, Ray D, Zhang Z, McCune WJ et al. Decreased Ras-mitogen-activated protein kinase signaling may cause DNA hypomethylation in T lymphocytes from lupus patients. Arthritis Rheum 2001; 44: 397–407.
Ichiyama K, Chen T, Wang X, Yan X, Kim BS, Tanaka S et al. The methylcytosine dioxygenase tet2 promotes DNA demethylation and activation of cytokine gene expression in T cells. Immunity 2015; 42: 613–626.
Loots GG, Ovcharenko I, Pachter L, Dubchak I, Rubin EM . rVista for comparative sequence-based discovery of functional transcription factor binding sites. Genome Res 2002; 12: 832–839.
Acknowledgements
This work was supported by the Ministry of Science and Technology, Taiwan, ROC (MOST 103-2320-B-016-017-MY3 and MOST 104-2320-B-016-014-MY3 to H-KS; NSC 102-2321-B-016-005-MY3 to F-CC), and Tri-service General Hospital foundation (TSGH-C103-005-007-009-S01 and TSGH-C104-008-S02 to H-KS). We thank Drs Maja Klug and Michael Rehli for kindly providing us the CpG-free plasmids.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Genes and Immunity website
Supplementary information
Rights and permissions
About this article
Cite this article
Chou, FC., Kuo, CC., Chen, HY. et al. DNA demethylation of the TIM-3 promoter is critical for its stable expression on T cells. Genes Immun 17, 179–186 (2016). https://doi.org/10.1038/gene.2016.6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gene.2016.6
- Springer Nature Limited