Abstract
Type 1 diabetes (T1D) is a multifactorial disease that has a strong genetic component. The HLA-G is a nonclassical HLA class I locus that is associated with immunomodulatory functions, including downregulation of innate and adaptive immune responses and induction of immune tolerance. However, there is currently limited information about the involvement of HLA-G in T1D susceptibility. This case-control study aims to investigate the T1D susceptibility association of alleles and genotypes of a widely investigated 14-bp insertion/deletion polymorphism in the HLA-G and to provide further evidence of the frequency distribution of class II HLA-DR-DQ-risk genotypes in T1D children and adolescents in the Brazilian population. The deletion allele and the homozygous deletion genotype are associated with susceptibility to T1D and the insertion allele and the heterozygous deletion/insertion genotype are associated with protection from T1D. We also confirm that genetic susceptibility to T1D is associated with the DRB1*03:01-DQA1*05:01-DQB1*02:01 and DRB1*04-DQA1*03:01-DQB1*03:02 haplotypes in Brazilian northeast region. The DR3-DQ2/DR4-DQ8 genotype conferred the highest detected risk for T1D. Our results identify a novel association of the 14-bp deletion allele and the homozygous deletion genotype with T1D development and provide additional evidence of the importance of HLA class II heterozygous DR3-DQ2/DR4-DQ8 genotype in T1D susceptibility.
Similar content being viewed by others
Introduction
Type 1 diabetes (T1D) is a chronic autoimmune disorder that results from β-cell destruction, usually leading to absolute insulin deficiency.1 Numerous studies have demonstrated that the human leukocyte antigen gene (HLA) harbors genetic risk factors for T1D. The age of onset for TD1 is typically between 8 and 12 years.2 However, there has been a marked increase in T1D incidence in children under age 5 in the last decade, and there is an alarming prediction that this will double by 2020.3
The contribution of HLA appears to be the most substantial when T1D is diagnosed before age 5 years, especially if the high-risk DR3-DQ2/DR4-DQ8 genotype is present.4, 5, 6 This heterozygous genotype, which is composed of DRB1*03:01-DQA1*05:01-DQB1*02:01 and DRB1*04:01/02/05-DQA1*03:01-DQB1*03:02 haplotypes, has been linked to the formation of transdimers, which can bind and present unique sets of auto-antigen-derived peptides, that may ultimately lead to pancreas β-cell destruction and development of T1D.7, 8
HLA contains an unusually high density of genes involved in immune functions, many of which are potential candidates for T1D susceptibility. Among these, a nonclassical HLA class Ib gene, HLA-G, is quite promising.9 The HLA-G gene is composed of 8 exons, 7 introns, a 5′-promoter region (5′-URR) and a 3′-untranslated region (UTR).10 The HLA-G primary transcript generates seven alternative mRNAs that encode membrane-bound (HLA-G1, -G2, -G3, -G4) and soluble (HLA-G5, -G6, -G7) protein isoforms.11
The HLA-G proteins possess the ability to bind to inhibitory receptors that are expressed by B and T cells, natural killer cells, and dendritic cells,12, 13 which are selectively located in immunologically protected sites such as the thymus14 and pancreatic islets.15 In pancreatic islets, HLA-G proteins were detected within insulin secretory granules, and the HLA-G proteins surface expression is regulated in response to growth, inflammatory and secretory stimuli.15 As insulin granules and sites of insulin exocytosis may represent targets where a high density of potentially immunogenic ligands become exposed, local HLA-G could prevent the activation of low-affinity cytotoxic T cells, thus acting as a mediator in T1D immune tolerance.15
Compared with the classical class I loci HLA-A and HLA-B, the HLA-G gene has less polymorphism.12 Several genetic variations in the 5′-URR and 3′-UTR have been identified that could potentially affect the expression of HLA-G, as variation in these regions can alter binding affinity for transcription factors, mRNA stability and microRNA targeting.16 The 14-nucleotide deletion polymorphism, referred to as the 14-bp insertion/deletion (Ins/Del) polymorphism, in the 3′-UTR region of HLA-G has been shown to regulate alternative splicing of the mRNA isoforms, HLA-G mRNA expression levels, and HLA-G protein levels for most of the membrane-bound and soluble isoforms.17
Various HLA-G expression profiles for the 14-bp Ins/Del polymorphic site are associated with pathological conditions, including transplantation,18, 19 autoimmune and inflammatory diseases,20, 21 viral/parasite infections22, 23, 24 and malignancies,10 but there is no clear consensus about these results. Studies have suggested that the deletion allele and homozygous deletion genotype,18, 19, 20, 24, 25 the insertion allele and insertion homozygous genotype23, 26, 27 and the heterozygous genotype21, 28 are all associated with high risk of developing a pathological condition.
No literature information was found about the involvement of the HLA-G 14-bp Ins/Del polymorphism in T1D. Thus, the objective of the present study was to evaluate, for the first time, the association of alleles and genotypes of the 14-bp Ins/Del polymorphism from HLA-G with the susceptibility to T1D. Moreover, it provides additional data concerning the frequency distribution of class II HLA-DR-DQ-risk genotypes in T1D children and adolescents in the Brazilian population. Significant differences in the frequencies of alleles and genotypes of the 14-bp Ins/Del HLA-G polymorphism were detected. The deletion allele (Del) and the homozygous deletion genotype (Del/Del) were associated with the susceptibility to T1D.
Results
Subject characteristics
Demographics and clinical data for each group are listed in Table 1. As expected, serum glucose and glycated hemoglobin values were significantly higher in the diabetic groups compared with NG controls (P<0.05).
HLA-G allele and genotype association with T1D
Allelic and genotypic frequencies of HLA-G 14-bp Ins/Del polymorphism in T1D and NG groups are presented in Table 2.
HLA-G typing was performed for 81 of 92 T1D patients and 100 NG subjects. The genotypic frequencies were in accordance with Hardy–Weinberg equilibrium in both T1D and NG groups (Hardy–Weinberg equilibrium P-value=0.585 and 0.142, respectively). The genotypic frequencies between the two groups were significantly different (P=0.0452). The 14-bp Del allele was overrepresented in the T1D group when compared with the NG group (P=0.0263, odds ratio; OR=1.68). The homozygous genotype for the 14-bp Del/Del was overrepresented in the T1D group when compared with the NG group (P<0.0220, OR=2.07). The heterozygous 14-bp Ins/Del (P=0.1366, OR=0.63) and the homozygous 14-bp insertion allele (Ins/Ins) (P=0.2091, OR=0.48) genotypes were underrepresented in the T1D group when compared with the NG group, although the latter two was not statistically significant. After Bonferroni correction none of the associations remained with significant.
HLA-DR-DQ diplotype association with T1D
DR-DQ genotypes were categorized on the basis of susceptible diplotypes: combinations of DRB1*03:01-DQA1*05:01-DQB1*02:01 (DR3-DQ2) and DRB1*04-DQA1*03:01-DQB1*03:02 (DR4-DQ8) haplotypes (Table 3).
The DR3-DQ2/DR4-DQ8 heterozygote diplotype, which represents the high-risk diplotype, was overrepresented (P<0.0001) in the T1D group (29.3%, 27/92) when compared with the NG group (1%, 1/100). In contrast, the low-risk diplotype, DRX-DQX/DRX-DQX, which was composed of haplotypes other than DR3-DQ2 or DR4-DQ8, was overrepresented (P<0.0001) in the NG group (66%, 66/100) when compared with the T1D group (16.3%, 15/92). The comparisons of frequencies for DR3-DQ2/DR4-DQ8 and DRX-DQX/DRX-DQX diplotypes remained significant even after a Bonferroni correction. The moderate-risk diplotypes, which were composed of the homozygous genotypes DR3-DQ2/DR3-DQ2 and DR4-DQ8/DR4-DQ8 and the genotypes composed of only one of susceptibility haplotypes (DR3-DQ2/ DRX-DQX, DR4-DQ8/DRX-DQX), together were also significantly more frequent (P=0.0035) in the T1D group (54.3%, 50/92) compared with the NG group (33%, 33/100), standing out, the DR3-DQ2/DR3-DQ2 and DR4-DQ8/DR4-DQ8 diplotypes. A statistically significant linkage disequilibrium between the 14pb Ins/Del HLA-G locus and HLA-DR-DQ loci was not evidenced.
Age at T1D onset and HLA-DR-DQ diplotypes
Table 4 lists the frequencies and OR values for selected HLA-DR-DQ diplotypes, which were stratified according to the age of T1D onset.
The DR3-DQ2/DR4-DQ8 diplotype was significantly increased in the T1D group with age at onset<5 years when compared with the group with age at onset >5 years (P=0.020, OR=3.05). Approximately 43% of individuals with T1D that were diagnosed before the age of 5 years carried this high-risk diplotype. In contrast, the moderate- and low-risk diplotypes were more frequent in children with age at onset >5 years. The DR3-DQ2/DRX-DQX moderate-risk diplotype frequency was underrepresented in the T1D group with age at onset <5 years when compared with the group with age at onset >5 years (P=0.046, OR=0.14).
Discussion
T1D is a multifactorial disease with a strong genetic component.29 The class II HLA genes, which include DRB1, DQA1 and DQB1, are well-known susceptibility loci for T1D.30 Significant T1D associations have been reported for the classical HLA-A, -B and -C loci, which suggests that there may be additional susceptibility loci within the HLA region.31, 32 It has been proposed that class II HLA genes determine the initiation of autoimmunity, whereas class I HLA genes regulate the progression of β-cell damage.33
Unlike the classical HLA loci, the nonclassical HLA-G locus has been linked to immunomodulatory activities, including downregulation of innate and adaptive immune responses and induction of immune tolerance.17 As T1D is an autoimmune disease where the breakdown of tolerance is directly implicated in disease development, the HLA-G locus might have an important role in this process.
This study aimed to investigate, for the first time, the association of alleles and genotypes of the 14-bp Ins/Del polymorphism of the HLA-G gene with T1D susceptibility. In addition, we assessed the distribution of HLA class II-risk haplotypes and genotypes in a T1D population in the state of Rio Grande do Norte, Brazil.
To this point, the 3′-UTR of the HLA-G gene contains 16 polymorphisms that have been described in the literature and are suggested to be involved in the differential HLA-G expression profile.16 The 14-bp Ins/Del polymorphism is among the most widely studied polymorphisms within this region. It is has been implicated in the regulation of protein expression, the modulation of HLA-G mRNA stability and in microRNA targeting.34 However, the exact mechanisms and functional significance of this polymorphism are not well understood.
Insertion of the 14-bp segment between positions +2961 and +2974 in exon 8 is suggested to result in an alternative splicing variant in which 92-bp are removed from the primary mRNA, and this truncated mRNA is more stable than the mRNA fragment that is generated by the 14-bp Del.17 Despite this increase in mRNA stability, several studies have indicated that the 14-bp Ins decreases the protein levels of both soluble and membrane-bound HLA-G in blood plasma and serum; however, the 14-bp Del results in high HLA-G isoforms in blood plasma and serum.11
Cirulli et al.15 demonstrated that HLA-G is constitutively expressed in the endocrine compartment of the human pancreas, specifically in insulin secretory granules. Moreover, it may be upregulated at the cell surface of primary islet cells that have been stimulated to secrete insulin. HLA-G may prevent the activation of autoreactive T cells, potentially by regulating immunogenic ligands present at sites of insulin exocytosis.
Significant differences in the frequencies of alleles and genotypes of the 14-bp Ins/Del HLA-G polymorphism were detected within the studied groups. The Del allele and the Del/Del genotype are associated with susceptibility to T1D given their higher frequencies in the T1D group when compared with the NG group. The Ins allele and the Ins/Del genotype are associated with protection from T1D, as they are present at higher frequencies in the NG group, although not statistically significant.
The allelic frequencies and the most frequent genotypes of polymorphic sites in the HLA-G regulatory regions, including the 14-bp Ins/Del polymorphism in 3′-UTR, have been investigated for individuals from different geographic Brazilian regions.11, 35, 36 In general, a high frequency of the Del allele and the Del/Del genotype was detected in healthy subjects from the northeast, the southeast and southern Brazil. Therefore, the results here could be biased by the overrepresentation of the Del allele in the Brazilian population.
Studies involving the 14-bp Ins/Del polymorphic profile and the expressed HLA-G proteins present conflicting results. The expression of HLA-G1 (a membrane-bound isoform) was determined to be higher for the 14-bp Ins compared with the 14-bp Del in a study using human cell lines.37 Studies in autoimmune diseases such as systemic lupus erythematosus, rheumatoid arthritis and multiple sclerosis have reported a higher frequency of the 14-bp Ins allele and the homozygous 14-bp Ins/Ins genotype, which are associated with lower HLA-G plasma levels.38 In contrast, other studies have reported increased frequency of the 14-bp Del allele and homozygous Del/Del genotype that exhibit higher levels of HLA-G in blood plasma in affected patients compared with control subjects.39, 40
A report involving type 2 diabetes, which is a disease characterized by obesity, inflammation and insulin resistance, indicated that there are no significant differences in the genetic distribution of the 14-bp Ins/Del HLA-G polymorphism in the type 2 diabetes group compared with a control group.41 In contrast, a separate report provided evidence of higher expression of soluble HLA-G in type 2 diabetes patients when compared with a normal glucose tolerance group.42
Very little is known about the HLA-G gene as a risk factor for T1D development or protection. A conditional analysis using family-based haplotype estimates (T1DGC MHC data set) identified several T1D-associated SNPs in a region of HLA that is near HLA-G, but none was detected within the regulatory 3′-UTR region where the 14-bp Ins/Del polymorphism is located (rs1704).43 Therefore, to the best of our knowledge, this is the first study evaluating the association between T1D and the 14-bp Ins/Del polymorphism of HLA-G.
We also propose that the genetic susceptibility to T1D is strongly associated with the HLA-DRB1*03:01-DQA1*05:01-DQB1*02:01 (DR3-DQ2) and DRB1*04:01/02/05-DQA1*03:01-DQB1*03:02 (DR4-DQ8) class II haplotypes. In particular, both haplotypes combined into a single genotype (DR3-DQ2/DR4-DQ8) conferred the highest risk for T1D, and our results are consistent with previous studies that were conducted in Latin America44, 45 southeastern Brazil46 and northeastern Brazil.47 In addition, the presence of the HLA-DR-DQ-risk diplotypes in combination with the HLA-G 14-bp Ins/Del genotypes was assessed, and a higher frequency of individuals who carried the DR3-DQ2/DR4-DQ8 high-risk diplotype in combination with the Del/Del genotype or the Ins/Del genotype was detected in the T1D group when compared with the NG group.
Although no significant linkage disequilibrium has been evidenced between the 14pb Ins/Del HLA-G locus and HLA-DR-DQ loci in the present study, Hviid and Christiansen48 identified a significant association between HLA-DRB1*03 and the HLA-G*01:01:02 alleles, which is included in the 14-bp sequence polymorphism, in women with recurrent spontaneous abortions. In recent studies using the T1DGC MHC data set, Eike et al.9 identified SNPs and microsatellite regions49 that are located in the vicinity of HLA-G (the closest is located 3.5 kb upstream of the HLA-G coding region) as additional risk factors for T1D, which are independent of the well-established DRB1-DQA1-DQB1 loci.
The DR3-DQ2/DR4-DQ8 high-risk genotype was also significantly associated with age at T1D onset <5 years. This genotype was accompanied by a threefold increased T1D risk in the younger age group. Our results are consistent with previous studies in which differences in genetic susceptibility for T1D are related to genetic acceleration of the disease process.2, 50, 51 A decrease in the prevalence of the high-risk genotypes and an increase of moderate- and low-risk genotypes was detected in T1D patients with age at T1D onset >5 years. These results suggest that there is a greater influence of environmental factors52 as well as other HLA53 and non-HLA loci6, 54 on susceptibility to T1D in this age at onset group when compared with the younger age at onset group.
In conclusion, our results suggest, for the first time, that there is an association of the 14-bp Del allele and the homozygous 14-bp Del genotype with T1D development. Considering the high frequency of this allele and genotype in the general population and taking into account the existence of other polymorphic loci in LD with the HLA-G variant, further studies are warranted to establish a definitive relationship of this genetic variation with T1D disease development and progression. Studies investigating the HLA-G protein levels should also be conducted to better understand the effects of phenotypes from this polymorphism and others in the 3'-UTR for T1D. In addition, our results provided evidence for an important role of HLA class II genes in susceptibility to T1D, particularly through the heterozygous DR3-DQ2/DR4-DQ8 genotype and its combination with the HLA-G 14-bp Del allele.
Materials and methods
Subjects
This study was conducted with 92 unrelated T1D patients (6–20-year old) that were recruited in the period of January 2010 to December 2011, from the Pediatrics Endocrinology Unit, Pediatrics Hospital of the Federal University of Rio Grande do Norte, in Natal, Rio Grande do Norte, Brazil. One hundred NG subjects (fasting serum glucose <99 mg dl−1), with the same age and sex of the T1D patients, were recruited from local public schools, during the same study period. T1D patients were categorized into two subgroups: those with age at onset <5-year old and those with age at onset >5-year old. Exclusion criteria included history of alcohol intake, smoking, other inflammatory diseases, infections and pregnancy. All T1D patients were on insulin treatment. The University Hospital Onofre Lopes Human Research Ethics Committee, in accordance with Brazilian law, which complies with the Declaration of Helsinki, approved the study (protocol number 207/09). Written free consent was obtained from participants and/or their parents. After taking medical history and performing physical examination, fasting blood was obtained from all subjects for biochemical analysis and genotyping of peripheral blood mononuclear cells.
Biochemical measurements
Glycemic controls were assessed using glycated hemoglobin from total blood and serum glucose. Measurements were performed using Labtest kits (Lagoa Santa, Minas Gerais, Brazil). Labmax Plenno (Labtest) was used to perform serum glucose measurements, and a RA 50 spectrophotometer (Bayer Diagnostics, Dublin, Ireland) was used to measure glycated hemoglobin.
HLA genotyping
Genomic DNA was obtained from peripheral blood mononuclear cells that were isolated using a discontinuous Ficoll-Hipaque (Sigma-Aldrich, St Louis, USA) gradient with a specific density of 1.070 g ml−1, at room temperature. Extraction was performed using an Illustra Triple Prep kit (GE Healthcare, Little Chalfont, UK) according to the manufacturer instructions. DNA was stored at −20 °C until the time of analysis.
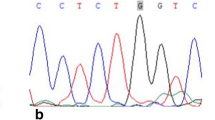
The HLA-G 14-bp Ins/Del genotypes in the 3′-UTR of exon 8 of the HLA-G locus (rs1704) were analyzed in 81 of 92 T1D patients and 100 NG subjects, according to the following protocol: 200 ng of genomic DNA was amplified in a 25 μl reaction mixture containing 0.20 mm dNTP (Ludwig, Alvorada, Rio Grande do Sul, Brazil), 0.2 mm of each primer, 0.5 U Taq DNA polymerase (Invitrogen, Carlsbad, CA, USA), 1.5 mm MgCl2 and a 1 × PCR buffer (0.2 m Tris–HCl pH8.5, 0.5 m KCl). After an initial denaturation step at 94 °C for 5 min, samples were submitted to 30 additional cycles at 95 °C for 45 s, 56 °C for 45 s and 72 °C for 30 s, with a final extension cycle at 72 °C for 10 min with 5′-TGTGAAACAGCTGCCCTGTGT-3′ as the forward primer and 5′-GTCTTCCATTTATTTTGTCTCT-3′ as the reverse primer. The amplification products were evaluated using a 3.5% agarose gel. The presence of a 345-bp fragment corresponded to the deletion allele, while a 359-bp fragment corresponded to the 14-bp insertion allele.
HLA class II genes (DRB1, DQA1 and DQB1) were genotyped using PCR sequence-specific oligonucleotides on a Luminex multianalyte system with a LABType sequence-specific oligonucleotides commercial kit (One Lambda, Inc., Canoga Park, CA, USA) as previously described.55, 56 The results were analyzed using HLA Fusion v 1.2.1. software.
Statistical analysis
Distribution of clinical and laboratory variables was analyzed using a Kolmogorov–Smirnov test. Differences between groups of normally distributed variables were calculated using the parametric test analysis of variance (one-way analysis of variance) followed by post hoc analysis with a Tukey’s test. For a non-normally distributed variables was used the nonparametric test Kruskal–Wallis followed by Dunn’s multiple comparisons test and this data were presented as median±interquartile range. The allelic and genotypic frequencies for HLA-DRB1, DQ and HLA-G 14-bp Ins/Del polymorphisms were calculated using a direct count method for all groups. A Haldane’s correction was applied where the allele frequency was zero to compute the corrected odds ratio by adding 0.5 to each cell.57 The frequencies of the most probable HLA-DRB1-DQA1-DQB1 haplotypes, adherences of genotypic proportions to Hardy–Weinberg equilibrium expectations and pairwise linkage disequilibrium were calculated using ARLEQUIN version 3.5.58 The statistical significance for the allelic, haplotypic and genotypic frequencies between the T1D group and the NG group and with the age at onset groups was calculated with a two-sided simple χ2-test or Fisher’s exact test (accurate for small sample sizes) using GraphPad Prism 5.0 software (GraphPad Software, Inc., San Diego, CA, USA). GraphPad Prism 5.0 software was used to calculate the OR and its 95% CI. Statistical significance was defined as P<0.05. For statistical haplotype and genotype association, the P-value was corrected using a Bonferroni test by dividing the previously established P-value by the number of haplotypes and genotypes tested.
References
Care M . Standards of medical care in diabetes-2013. Diabetes Care 2013; 36 (Suppl 1): S11–S66.
Emery LM, Babu S, Bugawan TL, Norris JM, Erlich HA, Eisenbarth GS et al. Newborn HLA-DR, DQ genotype screening: age- and ethnicity-specific type 1 diabetes risk estimates. Pediatr Diabetes 2005; 6: 136–144.
Patterson CC, Dahlquist GG, Gyürüs E, Green A, Soltész G, EURODIAB Study Group. Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet 2009; 373: 2027–2033.
Caillat-zucman S, Garchon H, Timsit J, Assan R, Boitard C, Djilali-saiah I et al. Age-dependent HLA genetic heterogeneity of type 1 insulin-dependent diabetes mellitus. J Clin Invest 1992; 90: 2242–2250.
Lambert A, Gillespie K, Thomson G, Cordell H, Todd J, Gale EAM et al. Absolute risk of childhood-onset type 1 diabetes defined by human leukocyte antigen class II genotype: a population-based study in the United Kingdom. J Clin Endocrinol Metab 2004; 89: 4037–4043.
Leslie RD . Predicting adult-onset autoimmune diabetes: clarity from complexity. Diabetes 2010; 59: 330–331.
Moustakas AK, Papadopoulos GK . Molecular properties of HLA-DQ alleles conferring susceptibility to or protection from insulin-dependent diabetes mellitus: keys to the fate of islet beta-cells. Am J Med Genet 2002; 115: 37–47.
Van Lummel M, van Veelen PA, Zaldumbide A, de Ru A, Janssen GMC, Moustakas AK et al. Type 1 diabetes-associated HLA-DQ8 transdimer accommodates a unique peptide repertoire. J Biol Chem 2012; 287: 9514–9524.
Eike MC, Becker T, Humphreys K, Olsson M, Lie BA . Conditional analyses on the T1DGC MHC dataset: novel associations with type 1 diabetes around HLA-G and confirmation of HLA-B. Genes Immun 2009; 10: 56–67.
Teixeira AC, Souza FF, Marano LA, Deghaide NHS, Ferreira SC . The 14 bp-deletion allele in the HLA-G gene confers susceptibility to the development of hepatocellular carcinoma in the Brazilian population. Tissue Antigens 2013; 81: 408–413.
Martelli-palomino G, Pancotto JA, Muniz YC, Mendes-junior CT, Erick C, Massaro JD et al. Polymorphic sites at the 3’ untranslated region of the HLA-G gene are associated with differential HLA-G soluble levels in the Brazilian and French population. PLoS One 2013; 8: e71742.
Carosella ED, Favier B, Rouas-freiss N, Moreau P, Lemaoult J, Bm I . Beyond the increasing complexity of the immunomodulatory HLA-G molecule. Blood 2008; 111: 4862–4870.
Abediankenari S, Eslami MB, Sarrafnejad A, Mohseni M . Dendritic cells bearing HLA-G inhibit T-cell activation in type 1 diabetes. Iran J Allergy Asthma Immunol 2007; 6: 1–7.
Blaschitz A, Crisa L, Schmitt C, Fournel S, King A, Loke YW et al. HLA-G in the human thymus: a subpopulation of medullary epithelial but not CD83 (+) dendritic cells expresses HLA-G as a membrane-bound and soluble protein. Int Immunol 1999; 11: 889–898.
Cirulli V, Zalatan J, Mcmaster M, Prinsen R, Salomon DR, Ricordi C et al. The class I HLA repertoire of pancreatic islets comprises the nonclassical class Ib antigen HLA-G. Diabetes 2006; 55: 1214–1222.
Castelli EC, Veiga-castelli LC, Yaghi L, Moreau P, Donadi EA . Transcriptional and posttranscriptional regulations of the HLA-G Gene. J Immunol Res 2014; 2014: 734068.
Amodio G, De Albuquerque RS, Gregori S . New insights into HLA-G mediated tolerance. Tissue Antigens 2014; 84: 255–263.
Twito T, Joseph J, Mociornita A, Rao V, Ross H, Delgado DH . The 14-bp deletion in the HLA-G gene indicates a low risk for acute cellular rejection in heart transplant recipients. J Heart Lung Transplant 2011; 30: 778–782.
Misra MK, Prakash S, Kapoor R, Pandey SK, Sharma RK, Agrawal S . Association of HLA-G promoter and 14-bp insertion – deletion variants with acute allograft rejection and end-stage renal. Tissue Antigens 2013; 82: 317–326.
Borghi A, Rizzo R, Corazza M, Bertoldi AM, Bortolotti D, Sturabotti G et al. HLA-G 14-bp polymorphism: a possible marker of systemic treatment response in psoriasis vulgaris? Preliminary results of a retrospective study. Dermatol Ther 2014; 27: 284–289.
Lee YH, Bae SC, Song SG . Meta-analysis of associations between functional HLA-G polymorphisms and susceptibility to systemic lupus erythematosus and rheumatoid arthritis. Rheumatol Int 2015; 35: 953–961.
Courtin D, Milet J, Sabbagh A, Massaro JD, Castelli EC, Jamonneau V et al. Infection, genetics and evolution HLA-G 3 0 UTR-2 haplotype is associated with human African trypanosomiasis susceptibility. Infect Genet Evol 2013; 17: 1–7.
Xu H, Shi W, Lin A, Yan W . HLA-G 3′ untranslated region polymorphisms influence the susceptibility for human papillomavirus infection. Tissue Antigens 2014; 84: 216–222.
Haddad R, Cilião Alves DC, Rocha-Junior MC, Azevedo R, Pombo-de-Oliveira MS, Takayanagui OM et al. HLA-G 14-bp Insertion/Deletion Polymorphism Is a Risk Factor for HTLV-1 Infection. AIDS Res Hum Retroviruses 2011; 27: 283–288.
Veit TD, Vianna P, Xavier RM, Delgado-can A, Gutierrez JE, Carneiro AP et al. Association of the HLA-G 14-bp insertion/deletion polymorphism with juvenile idiopathic arthritis and rheumatoid arthritis. Tissue Antigens 2008; 71: 440–446.
Fabris A, Segat L, Catamo E, Morgutti M, Vendramin A, Crovella S . HLA-G 14 bp deletion/insertion polymorphism in celiac disease. Am J Gastroenterol 2010; 106: 139–144.
Jeong KH, Kim SK, Kang BK, Chung JH, Shin MK, Lee MH . Association between an HLA-G 14 bp insertion/deletion polymorphism and non-segmental vitiligo in the Korean population. Arch Dermatol Res 2014; 306: 577–582.
Xue S, Yang J, Yao F, Xu L, Fan L, Fan L . Recurrent spontaneous abortions patients have more 1 14 bp heterozygotes in the 3 # UT region of the HLA-G gene in a Chinese Han population. Tissue Antigens 2007; 69: 153–155.
Steck AK, Rewers MJ . Genetics of type 1 diabetes. Clin Chem 2011; 57: 176–185.
Thomson G, Valdes AM, Noble JA, Kockum I, Grote MN, Najman J et al. Relative predispositional effects of HLA class II DRB1-DQB1 haplotypes and genotypes on type 1 diabetes: a meta-analysis. Tissue Antigens 2007; 70: 110–127.
Valdes AM, Erlich HA, Carlson J, Varney M, Moonsamy PV, Noble JA . Use of class I and class II HLA loci for predicting age at onset of type 1 diabetes in multiple populations. Diabetologia 2012; 55: 2394–2401.
Nejentsev S, Howson JMM, Walker NM, Szeszko J, Sarah F, Stevens HE et al. Localization of type 1 diabetes susceptibility to the MHC class I genes HLA-B and HLA-A. Nature 2007; 450: 887–892.
With C, Ii RC, Lipponen K, Gombos Z, Kiviniemi M, Siljander H et al. Effect of HLA class I and class II alleles on progression from autoantibody positivity to overt type 1 diabetes in children with risk-associated class II genotypes. Diabetes 2010; 59: 3253–3256.
Castelli EC, Moreau P, Oya A, Mendes-junior CT, Antonio E . In silico analysis of microRNAS targeting the HLA-G 3=untranslated region alleles and haplotypes. Hum Immunol 2009; 70: 1020–1025.
Lucena-Silva N, de Souza VS, Gomes RG, Fantinatti A, Muniz YC, de Albuquerque RS et al. HLA-G 3′ untranslated region polymorphisms are associated with systemic lupus erythematosus in 2 Brazilian populations. J Rheumatol 2013; 40: 1104–1113.
Tureck LV, Santos LC, Wowk PF, Mattar SB, Silva JS, Roxo VMMS et al. HLA-G 5 ′ URR SNPs and 3 ′ UTR 14-bp insertion/deletion polymorphism in an Afro-Brazilian population from Parana State. Int J Immunogenet 2014; 41: 29–33.
Goul S, Hantash BM, Zhao L, Faber C, Bzorek M, Holst M et al. The expression and functional activity of membrane-bound human leukocyte antigen-G1 are influenced by the 3 0 -untranslated region. Hum Immunol 2013; 74: 818–827.
Rizzo R, Hviid TVF, Govoni M, Padovan M, Rubini M, Melchiorri L et al. HLA-G genotype and HLA-G expression in systemic lupus erythematosus: HLA-G as a putative susceptibility gene in systemic lupus erythematosus. Tissue Antigens 2008; 71: 520–529.
Rizzo R, Rubini M, Govoni M, Padovan M, Melchiorri L, Stignani M et al. HLA-G 14-bp polymorphism regulates the methotrexate response in rheumatoid arthritis. Pharmacogenet Genomics 2006; 16: 615–623.
Rizzo R, Bortolotti D, Ben N, Rotola A, Cura F, Castellazzi M et al. Role of HLA-G 14 bp deletion/insertion and+3142C>G polymorphisms in the production of sHLA-G molecules in relapsing-remitting multiple sclerosis. Hum Immunol 2012; 73: 1140–1146.
García-gonzález IJ, Valle Y, Rivas F, Figuera-villanueva LE, Muñoz-valle JF, Flores-salinas HE et al. The 14 bp Del/Ins HLA-G polymorphism is related with high blood pressure in acute coronary syndrome and type 2 diabetes mellitus. Biomed Res Int 2014; 2014: 898159.
Solini A, Muscelli E, Stignani M, Melchiorri L, Santini E, Rossi C et al. Soluble human leukocyte antigen-G expression and glucose tolerance in subjects with different degrees of adiposity. J Clin Endocrinol Metab 2010; 95: 3342–3346.
Cheung YH, Watkinson J, Anastassiou D . Conditional meta-analysis stratifying on detailed HLA genotypes identifies a novel type 1 diabetes locus around TCF19 in the MHC. Hum Genet 2011; 129: 161–176.
Cifuentes RA, Rojas-Villarraga A, Anaya J-M . Human leukocyte antigen class II and type 1 diabetes in Latin America: a combined meta-analysis of association and family-based studies. Hum Immunol 2011; 72: 581–586.
Rojas-Villarraga A, Botello-Corzo D, Anaya J-M . HLA-Class II in Latin American patients with type 1 diabetes. Autoimmun Rev 2010; 9: 666–673.
Alves C, Meyer I, Vieira N, Toralles MBP, LeMaire D . [Distribution and frequency of HLA alleles and haplotypes in Brazilians with type 1 diabetes mellitus]. Arq Bras Endocrinol Metabol 2006; 50: 436–444.
Brandao LC, Vatta S, Guimaraes R, Segat L, Araujo J, De Lima Filho JL et al. Rapid genetic screening for major human leukocyte antigen risk haplotypes in patients with type 1 diabetes from Northeastern Brazil. Hum Immunol 2010; 71: 277–280.
Hviid TVF, Christiansen OB . Linkage disequilibrium between human leukocyte antigen (HLA) class II and HLA-G —possible implications for human reproduction and autoimmune disease. Hum Immunol 2005; 66: 688–699.
Eike MC, Humphreys K, Becker T, Olsson M, Lie BA . Three microsatellites from the T1DGC MHC data set show highly significant association with type 1 diabetes, independent of the HLA-DRB1, -DQA1 and -DQB1 genes. Diabetes Obes Metab 2009; 11: 17–24.
Komulainen J, Kulmala P, Savola K, Lounamaa R, Ilonen J, Reijonen H et al. Clinical, autoimmune, and genetic characteristics of very young children with type 1 diabetes. Diabetes Care 1999; 22: 1950–1955.
Hathout EH, Hartwick N, Fagoaga OR, Colacino AR, Racine M, Nelsen-cannarella S et al. Clinical, autoimmune, and HLA characteristics of children diagnosed with type 1 diabetes before 5 years of age. Pediatrics 2003; 111: 860–863.
Dang MN, Mary Q . Epigenetics in autoimmune diseases with focus on type 1 diabetes. Diabetes Metab Res Rev 2013; 29: 8–18.
Varney MD, Valdes AM, Carlson JA, Noble JA, Tait BD, Bonella P et al. HLA DPA1, DPB1 alleles and haplotypes contribute to the risk associated with type 1 diabetes. Diabetes 2010; 59: 2055–2062.
Borchers A, Uibo R, Gershwin M . The geoepidemiology of type 1 diabetes. Autoimmun Rev 2010; 9: A355–A365.
Silveira A, Gomes M, Gomes J, Rosa A, Regina S, Neumann J et al. HLA-A, -B, and -DRB1 allelic and haplotypic diversity in a sample of bone marrow volunteer donors from Rio Grande do Sul State, Brazil. Hum Immunol 2012; 73: 180–185.
Trajanoski D, Fidler SJ . HLA typing using bead-based methods. Methods Mol Biol 2012; 882: 47–65.
Haldane J . The estimation and significance of the logarithm of a ratio of frequencies. Ann Hum Genet 1956; 20: 309–311.
Excoffier L, Lischer HEL . Arlequin suite ver 3.5: a new series of programs to perform population genetics analyses under Linux and Windows. Mol Ecol Resour 2010; 10: 564–567.
Acknowledgements
This study was supported by CNPq research project (Grant number 620099/2008-9) and CAPES scholarship. We thank all of the volunteers who participated in this study. We are grateful for the technical support provided by students and technicians from LABMULT/UFRN/RN, LABIOMOL/UFRN/RN and FUNDHERP/SP in special to Neifi Hassan Saloum Deghaide. We also thank all of the physicians, nurses and hospital staff at HOSPED/UFRN who were involved in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Silva, H., Ururahy, M., Souza, K. et al. The association between the HLA-G 14-bp insertion/deletion polymorphism and type 1 diabetes. Genes Immun 17, 13–18 (2016). https://doi.org/10.1038/gene.2015.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gene.2015.45
- Springer Nature Limited
This article is cited by
-
Single-nucleotide polymorphisms as important risk factors of diabetes among Middle East population
Human Genomics (2022)
-
“HLA-G 3′UTR gene polymorphisms and rheumatic heart disease: a familial study among South Indian population”
Pediatric Rheumatology (2017)