Abstract
Background/Objectives:
Recent metabolomics technique reveals a plasma-free amino acid (PFAA)-based metabolite signature that is suggestive of altered PFAAs being an early manifestation of obesity-related insulin resistance. However, the PFAA profiles within non-obese, but more insulin-resistant Asians are not well researched. Compared with Caucasians, Asian populations have more central adiposity, which is generally regarded as metabolically more adverse, but the underlying mechanisms remain unclear. In the present study, we examined whether PFAA profiling was at least one important factor mediating central adiposity and insulin resistance, and aid in cardiovascular risk assessment in healthy Asians with normal body weight.
Subject/Methods:
This was a cross-sectional study. A total of 190 healthy men (n=87 with a mean±s.d. body mass index (BMI) of 23.5±3.5 kg/m2) and women (n=103 with a mean±s.d. BMI of 21.4±3.7 kg/m2) residing in Singapore took part in this study. PFAA levels were measured by using an amino acid analyzer. Basic anthropometric measurements, fasting blood glucose, fasting serum insulin and lipid profiles were obtained using standard protocols.
Results:
Seven out of 18 amino acids were significantly correlated with measures of obesity (for example, waist circumference; waist-to-hip ratio and BMI) in current participants. Among them, the plasma concentrations of five amino acids, including Phe, Tyr, Met, Ala and His were positively associated with waist-to-hip ratio. With the exception of His, which had no association with insulin resistance, Phe, Tyr, Met and Ala were significantly associated with hyperinsulinemia and insulin resistance (P<0.05). In contrast, no associations were observed between circulating BCAAs (that is, Val, Leu, Ile), measures of obesity and insulin resistance. However, significant inverse associations were observed between BCAAs and total cholesterol and high-density lipoprotein.
Conclusions:
We found that central adiposity was associated with alterations of specific amino acids. As a result, PFAAs may serve as metabolite predictors of hyperglycemia, hyperinsulinemia and dyslipidemia in healthy participants.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) is an increasingly serious public health concern globally, which is particularly alarming in Asia.1 Compared with their Western counterparts, Asian populations are found to develop type 2 diabetes (T2D) at a lower body mass index (BMI) and at younger ages.2 One plausible reason for this interethnic difference is that Asians are more insulin resistant than Caucasians and African Americans.3 However, the exact causes of the increased insulin resistance in Asians remain to be elucidated. The potential contributors may include the ‘normal-weight metabolically obese’ phenotype,4 high intake of refined carbohydrates5 and dramatically decreased physical activity levels.6
Insulin resistance has been widely accepted to precede T2D and increase the risks for cardiovascular diseases (CVD),7 its early detection and intervention, therefore, could be crucial to counteract the higher risks of T2D and CVD, especially in Asian populations. Recently, several studies have reported that the alterations of plasma-free amino acid (PFAA) profiles were significantly associated with insulin-resistant conditions.8, 9, 10, 11 For example, the levels of branched-chain amino acids (BCAAs), that is, valine (Val), leucine (Leu) and isoleucine (Ile), were elevated in obese subjects.12, 13 One possible etiology of BCAAs elevation in obesity is that insulin resistance decreases the utilization of amino acids and uptakes of BCAAs into muscles.14 Another potential cause is that insulin resistance reduces BCAA-catabolizing enzyme activity leading to suppression of BCAA catabolism.15 Other PFAAs, such as glutamate (Glu), serine (Ser), proline (Pro), glycine (Gly), alanine (Ala), tyrosine (Tyr), phenylalanine (Phe) and tryptophan (Trp), were also changed in subjects with high visceral obesity.16 The alteration of PFAA profiles is believed to be the combined results of insulin resistance-induced accelerated protein breakdown in muscle and hepatic gluconeogenesis set point changes.17
Several cohort studies have demonstrated that the alterations of PFAAs can be used as potential biomarkers to predict the future development of T2D and CVD.18, 19, 20, 21 However, only a few studies have examined the relationship between PFAA profiles, insulin resistance and risks for diabetes and CVD in Asian populations, who develop diabetes at a much lower BMI.1, 2 It is unclear whether the obesity-related PFAA alterations can be used as early markers for identifying diabetic risks in the healthy non-obese adults living in Singapore, a Southeast Asian country. A pioneer study by Tai et al.22 reported that PFAA levels, including Ala, Pro, Val, Leu/Ile, Phe, Tyr, Glu/Gln, Orn, were positively associated with HOMA-IR in non-obese Chinese and Asian-Indian men. However, only males were included in the study, and the generalizability of their findings to females is not known. Previous studies have reported that the association strength of amino acid biomarkers with insulin resistance and obesity may be gender-dependent.23 Therefore, the primary goal of this study was to characterize the PFAA profiles in both healthy males and females living in Singapore and to examine the associations between PFAA profiles and CVD risk factors including dyslipidemia, hypertension, hyperglycemia and insulin resistance. The results may have significant roles in the development of diabetes research in Singapore as well as other parts of Asia.
Materials and methods
Study design and clinical measures
This study was limited to cross-sectional analyses of data from participants attending a baseline visit between 17 June 2014 and 18 February 2016. This study was a subsection of a larger study. The participants included 190 healthy adults aged 21 to 69 years: 87 males (45.8%) and 103 females (54.2%). They were recruited from the general public in Singapore through advertisements on newspaper and posters that were placed around the National University of Singapore campus, public area and on the Clinical Nutrition Research Centre website. To be eligible, participants were required to be Singaporeans or individuals who have resided in Singapore for a minimum of 5 years, healthy males and females. Participants were excluded if they were pregnant or diagnosed with any major diseases. Before the study, no oral glucose tolerance tests were performed, but all the participants were asked to restrict alcohol and caffeine-containing drinks as well as to refrain themselves from intense physical activity. All procedures involving human subjects were approved by the National Healthcare Group Domain Specific Review Board (Reference Number: 2013/00783), Singapore.
Participants arrived at the laboratory in the morning after a 10 h overnight fast. All the participants gave written informed consent before starting. Two finger prick capillary blood samples were obtained for determining blood glucose concentration (fasting blood glucose (FBG), mmol/l) using the HemoCue 201+ RT Glucose analyser (HemoCue Ltd, Dronfield, UK). In addition, a total of 10 ml of venous blood was collected into Vacutainers (Becton Dickinson Diagnostics, Singapore). Blood samples were separated by centrifugation at 1500 r.p.m. for 10 min at 4 °C within 2 h of being drawn and aliquots were stored at −80 °C until analysis. Fasting serum insulin (FSI, μU/ml) was measured using the immunochemistry analyzer COBAS e411 (Roche, Hitachi, Indianapolis, IN, USA). Insulin resistance index HOMA-IR was calculated using FBG and FSI (HOMA-IR=FBG × FSI/22.5). Fasting lipid parameters including total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein and triglycerides were measured using chemistry analyzer COBAS c311 (Roche, Hitachi). Systolic blood pressure and diastolic blood pressure were measured with an Omron (Singapore) blood pressure monitor (model HEM-907). The measurements were done in duplicate and readings were averaged. The anthropometric measurements were achieved via the reported method.24, 25
Measurement of PFAA profiles
Eighteen amino acids from plasma samples were measured using a Hitachi high-speed amino acid analyzer L-8900 A system (Tokyo, Japan). The samples (600 μl) underwent protein precipitation by adding 1 ml of 5% of trichloroacetic acid and incubated for at least 1 h at 4 °C. After centrifuging for 30 min at 10 000 g, the supernatant was retained and filtered by a 0.45 μm membrane filter before the analysis. Plasma amino acids were identified using a reaction column system via the ninhydrin reaction method. The ratio of the area under the curves of each amino acid to its assigned internal standard was then plotted against a multiple point calibration curve, allowing for the quantification of the amino acid levels in plasma samples.
Statistical analysis
Baseline characteristics of the participants were presented as arithmetic means±s.d. Linear regression models were used to examine the associations between amino acid concentrations and various clinical measures. Age, physical activity, gender, smoking status, family history of disease and ethnicity were adjusted for in all the models. All statistical analyses were performed using Stata 11.1 (StataCorp, College Station, TX, USA). Two-sided P<0.05 was considered statistically significant in all the cases.
Results
Population characteristics
A total of 190 participants (87 males and 103 females) took part in this study with a mean±s.d. age of 30.2±11.9 years. To access physical activity, about half of the study participants (91/190) wore an AM-180C activity monitor (Tanita, Japan) for seven consecutive days (with an average of 7163±2876 steps per day). Only 1.6% of participants (3/190) smoked. The participants were more insulin resistant (80/190 were HOMA-IR ⩾1.6), but they had a lower BMI (an average BMI of 22.4±3.8 as shown in Table 1). Despite these, the participants represent generally healthy metabolic status; only two of them had impaired fasting glucose (IFG⩾5.6 mmol/l). The average TC/HDL ratio was 3.2±1.0 (3.6±1.2 for males and 3.0±0.8 for females). Sixty-nine males (79.3%) and 97 females (94.2%) had TC/HDL ratio ⩽4.5. The average systolic blood pressure was 111.7±14.3 (118.6±10.0 for males and 105.8±14.7 for females) and the average diastolic blood pressure was 66.1±8.8 (68.0±8.5 for males and 64.6±8.8 for females). A total of 54 males (62.1%) and 94 females (91.3%) had systolic blood pressure <120 mm Hg, while a total of 80 males (92.0%) and 97 females (94.2%) had diastolic blood pressure <80 mm Hg.
Amino acid levels in study population
Average concentrations of 18 amino acids, including 3 of BCAAs, 2 of aromatic amino acids (AAAs), 3 of sulfur-containing amino acids, 8 of glucogenic amino acids and 2 other amino acids in healthy Singaporean adults were listed in Table 2. With the exception of taurine (Tau), aspartic acid (Asp) and Ser, males had significanlty higher concentrations of 10 amino acids, that is, Val, Ile, Leu, Phe, Tyr, methionine (Met), lysine (Lys), Ala, Gln and Pro, than females.
First, we assessed whether circulating amino acid levels were linked with measures of obesity. Table 3 shows the association magnitudes (for example, 1.40 unit increase in Val concentration was associated with 1 cm increase in waist circumference (WC)) of amino acids with central (WC and waist-to-hip ratio (WHR)) and overall obesity (BMI). When all the participants were taken together, both BCAAs and AAAs were significantly positively associated with WC, WHR and BMI in all the unadjusted models. However, the associations between BCAAs and WC, WHR, as well as BMI did not persist after adjusting for established risk factors such as age, physical activity, gender, smoking status, family history of disease and ethnicity. In contrast, AAAs and histidine (His) were positively associated with WC, WHR and BMI even after adjusting for potential confounders (Table 3). In addition, after the adjustment, both Met and Ala were positively associated with WHR, whereas Gly and Ser were negatively associated with BMI.
PFAA profiles related to CVD risk factors
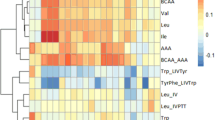
Next, we examined whether the PFAA profiles were altered in accordance with their metabolic status in the current population. Table 4 shows that BCAAs were significantly associated with lipid profiles, while AAAs and Ala were significantly associated with FBG and HOMA-IR in the unadjusted models. After adjustment for established risk factors, seven amino acids, that is, Met, Ala, Gln, Pro, Ser, Lys and Thr, were significantly associated with FBG (Figure 1a), whereas four amino acids (Phe, Tyr, Met and Ala) were significantly associated with FSI (Figure 1b) and six amino acids (Ile, Phe, Tyr, Met, Ala and Thr) were significantly associated with HOMA-IR (Figure 1c). Furthermore, Table 5 shows that BCAAs were significantly associated with TC and HDL, but Ala, Gln and His were significantly associated with triglycerides and triglycerides/HDL. It should be noted that none of the amino acids had significant association with systolic blood pressure and diastolic blood pressure after the adjustment (data not shown).
Associations of amino acids with (a) FBG, (b) FSI, as well as (c) HOMA-IR. Linear regression models were adjusted for age, physical activity, gender, smoking status, family history of disease and ethnicity. Association magnitudes are in standardized units of 1 unit increase in amino acid concentration per 1 unit increase in (a) FBG, (b) FSI and (c) HOMA-IR. Error bars indicate s.e. Only significant associations (P<0.05) are shown. *P<0.05; **P<0.005.
Discussion
Recent metabolomics-based technologies using targeted analyses focusing on amino acids and their metabolites have consistently revealed perturbation of normal amino acid metabolism in obesity, insulin resistance and T2D.23, 26, 27 Previous studies have shown that the levels of BCAAs and AAAs were significantly associated with the future diagnosis of DM18 and were novel biomarkers of CVD development and thus provided early links for identifying susceptibility to T2D and CVD.28 The relation of amino acid signatures with insulin resistance could even be modulated by changing the dietary protein and cereal-fiber contents in the absence of relevant weight loss.29 Although the interethnic differences of pathophysiology of insulin resistance between Asian and Caucasian populations are well known,2 few studies have examined the relationships between PFAA profiles, insulin resistance and CVD risk factors in Asian population, in particular, healthy Asians. The population-based SABRE study by Tillin et al.30 reported strong associations in South Asian men between BCAAs and AAAs and incident diabetes. Weaker (compared with European counterparts), but still significant positive associations were observed between BCAAs and measures of obesity. The study by Tillin et al. is consistent with other studies showing that elevated BCAAs in human obesity are associated with insulin resistance.23, 26, 27 The underlying mechanisms may involve the emerging role of BCAAs as potential regulators of satiety, leptin, mammalian target of rapamycin and protein kinase C signaling.31 Our data, however, indicate that there are no significant associations between BCAAs, measures of obesity and insulin resistance. Compared with the South Asian SABRE participants, the current participants were younger, had lower baseline levels of glucose, insulin and triglycerides, as well as lower central and overall obesity. The reduced adipose tissue in our participants perhaps explained the absence of associations between BCAAs, measures of obesity and HOMA-IR. Similarly, the weak correlations between BCAA levels and obesity were found in another study in Indian Asians living in India (age 35–45) with a low BMI.32 However, given that HOMA-IR was used to assess insulin resistance in ours as well as previous related studies, it cannot be excluded that the lack of associations was due to the indirect estimate of insulin resistance in the non-stimulated state. Recently, insulin resistance assessed by using HOMA-IR was found to be unaffected by dietary interventions, but the insulin resistance measured using euglycemic hyperinsulinemic clamps in the maximally stimulated state was changed with all diets.29 Therefore, a plausible conclusion from these observations is that the association between elevated BCAAs and insulin resistance depends on the ethnicity, degree of obesity of the participants and the methods used to assess insulin resistance. More research is needed to identify whether such association may exist in healthy relatively lean Southeast Asian population using an array of gold standard methods for the measurement of insulin resistance, for example, euglycemic clamps and tracer techniques.
However, we found that the elevation of five amino acids (Phe, Tyr, His, Met and Ala) were significantly associated with WHR. With the exception of His, which was minimally associated with markers of insulin resistance,30 the elevations of Phe, Tyr, Met and Ala were significantly associated with hyperinsulinemia and insulin resistance. This suggests that the alterations of specific amino acids metabolism may be the potential underlying mechanisms linking central obesity and insulin resistance. Although the relationships between BCAAs and obesity-related insulin resistance were well understood,23, 26, 27, 28, 29, 30, 31 the etiology of other amino acids in insulin-resistant states is not fully discussed yet in literature. Increased circulating concentrations of Phe and Tyr have often been reported together with BCAAs in obese, insulin-resistant and T2DM state.9, 12, 13 Phe and Tyr are metabolized to catecholamines, which could be an important factor for the development of central obesity and/or vice versa.33 Our data indicate that AAAs (Phe and Tyr) and related metabolites are associated with insulin resistance even in the absence of obesity, suggesting that dysregulation of AAAs metabolism may be an early indication of the progression to insulin resistance and T2D.
Previously, a number of groups reported the increased circulating concentrations of Met and its catabolic derivative cysteine (Cys) in obesity, insulin resistance and T2D.34, 35 The current study extends these findings to young healthy Asian population predominantly without obesity. Our results show significant associations between circulating Met, fasting hyperglycemia and hyperinsulinemia, indicating high level of Met was inversely associated with insulin sensitivity. This is consistent with previous study showing that dietary Met restriction enhances peripheral insulin sensitivity.36 The potential underlying mechanism is that Met restriction changes adiposity, releases insulin-sensitizing hormone, adiponectin, from adipose tissue, and improves the liver function. Our data support the notion that increased Met levels in plasma resulting from central adiposity may contribute to hyperinsulinemia and insulin resistance.
In addition to Met, there were positive correlations between circulating Ala and fasting hyperglycemia and hyperinsulinemia. As a NEAA, Ala is metabolized to pyruvate and is derived from BCAAs via glucose–alanine cycle.37 Therefore, Ala is involved in maintaining glucose homeostasis. Previously, Nakamura et al.38 found that Ala concentration was significantly correlated with BMI and insulin-related variables such as C-peptide, insulin, HOMA-IR and adiponectin, in T2D patients. In line with this finding, another study also reported significant associations between Ala and HOMA-IR in healthy Chinese and Asian-Indian men.22 Our data indicate that Ala is positively correlated with not only FBG, FSI and HOMA-IR but also WHR, suggesting that this Ala–insulin resistance relationship may result from protein turnover in association with increased central obesity. Another possible explanation is that the central obesity-induced increment of Ala is probably due to reduced entry of glucose into mitochondria for full oxidation, which also alters BCAAs metabolism generating insulin resistance.
Although the effect of PFAAs on obesity and insulin resistance has been extensively investigated, the effect on cholesterol metabolism, which is also associated with metabolic syndrome, has not been studied in detail. The BCAA Leu is known as a precursor of cholesterol and serves as a potent modulator of cholesterol metabolism. It was found that Leu supplement decreased TC and low-density lipoprotein levels by 27% and 53%, respectively, in mice on high-fat (60% fat calories) diet.39 Another study by Torres-Leal et al.40 reported that Leu attenuated the cholesterol levels in rats treated with high-fat diet. The reduction in cholesterol levels was found to be independent of changes in body weight. The underlying molecular mechanisms are largely related to mammalian target of rapamycin signaling activation.39 Although many studies have reported cholesterol-reducing effects of Leu in animal models, Newgard et al.13 observed that plasma Leu levels significantly increased in obese participants with hyperlipidemia compared with non-obese controls. Few studies have been undertaken to examine the cholesterol-reducing effects of Leu in non-obese populations. Although only 24 participants (12.6%) in our study cohort have a TC levels higher than 6.2 mmol/l (240 mg/dl), our data have shown that Leu is adversely correlated with TC, and suggest that dysregulation of Leu metabolism may be an early event in the progression to hypercholesterolemia. On the other hand, cholesterol-lowering effects of Val and Ile were also reported by others,41 but the underlying mechanisms remained elusive. Further elucidation of BCAAs signaling, via mammalian target of rapamycin or other potential mediators, will be required to discover the relevant mechanisms underlying the increase in BCAA levels in body cholesterol metabolism. Finally, although TC >6.2 mmol/l is recognized as a risk factor for CVD, the risk is lower if a high proportion is made up of the protective HDL than if the elevation is due primarily to increased amounts of low-density lipoprotein. Table 5 shows significant inverse associations between BCAAs, TC and HDL, suggesting that the beneficial effects of BCAAs on TC could be due to the attenuated HDL levels, which is not desirable.
Conclusions
Early intervention against conventional T2D and CVD risk factors, such as hyperglycemia, hyperinsulinemia, hypertension and dyslipidemia, is crucial to prevent the overt diseases onset. Our results suggest that the information generated from PFAA profiles is useful in identifying healthy, relatively non-obese individuals who are at high risk of developing insulin resistance and/or dyslipidemia. Our data also support the hypothesis that either central obesity is a risk factor for altered four plasma amino acid levels, including Phe, Tyr, Ala and Met, or PFAAs alteration is a risk factor for central obesity. Regardless of the outcomes, the current study has shown that the combinations of four amino acids are significantly associated with increased insulin resistance in healthy Singaporean adults. The intriguing result of the present study is that there is no relationship between BCAAs and insulin resistance that warrants further investigation. Our study, however, indicates that BCAAs could help to improve cholesterol metabolism.
Our study has several limitations. First, this is a cross-sectional study and thus causal inferences cannot be drawn. Second, the sample size of this study is not large enough. Future studies should be conducted with larger sample sizes. Third, although HOMA-IR has become a widely used clinical and epidemiological tool, it is not a direct measurement of insulin resistance. Therefore, the use of HOMA-IR to assess insulin resistance may have potential problems and fails to show a close relationship with whole-body insulin resistance assessed by euglycemic clamp techniques.29 Finally, dietary effects on amino acid profiles and insulin resistance were observed in some previous reports,29, 42 but other studies yielded contrary results showing that increased protein intake was not observed as evidence for higher BCAA levels.18, 22 Moreover, the pool size of free BCAAs is quite small and constant because of the continuous supply from muscle.43 Although we did not evaluate dietary nutrient intake, the circulating BCAAs and other EAAs are unlikely dominantly regulated by dietary intake, at least in the steady state of the present study. Despite these limitations, the results of our study provide evidence of the linkage between alterations of PFAAs, central adiposity and increased insulin resistance in Asian populations.
References
Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH et al. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006; 368: 1681–1688.
Ma RCW, Chan JCN . Type 2 diabetes in East Asians: Similarities and differences with populations in Europe and the United States. Ann N Y Acad Sci 2013; 1281: 64–91.
Chiu KC, Cohan P, Lee NP, Chuang LM . Insulin sensitivity differs among ethnic groups with a compensatory response in beta-cell function. Diabetes Care 2000; 23: 1353–1358.
Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL . Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr 2007; 86: 353–359.
Choi H, Song S, Kim J, Chung J, Yoon J, Paik HY et al. High carbohydrate intake was inversely associated with high-density lipoprotein cholesterol among Korean adults. Nutr Res 2012; 32: 100–106.
Amati F, Dube JJ, Coen PM, Stefanovic-Racic M, Toledo FGS, Goodpaster BH . Physical inactivity and obesity underlie the insulin resistance of aging. Diabetes Care 2009; 32: 1547–1549.
Ruige JB, Assendelft WJJ, Dekker JM, Kostense PJ, Heine RJ, Bouter LM . Insulin and risk of cardiovascular disease: a meta-analysis. Circulation 1998; 97: 996–1001.
Seibert R, Abbasi F, Hantash FM, Caulfield MP, Reaven G, Kim SH . Relationship between insulin resistance and amino acids in women and men. Physiol Rep 2015; 3: e12392.
Wurtz P, Soininen P, Kangas AJ, Rönnemaa T, Lehtimäki T, Kähönen M et al. Branched-chain and aromatic amino acids are predictors of insulin resistance in young adults. Diabetes Care 2013; 36: 648–655.
Wurtz P, Makinen VP, Soininen P, Kangas AJ, Tukiainen T, Kettunen J et al. Metabolic signatures of insulin resistance in 7098 young adults. Diabetes 2012; 61: 1372–1380.
Yamada C, Kondo M, Kishimoto N, Shibata T, Nagai Y, Imanishi T et al. Association between insulin resistance and plasma amino acid profile in non-diabetic Japanese subjects. J Diabetes Invest 2015; 6: 408–415.
Felig P, Marliss E, Cahill GF Jr . Plasma amino acid levels and insulin secretion in obesity. N Engl J Med 1969; 281: 811–816.
Newgard CB, An J, Bain JR, Muehlbauer MJ, Stevens RD, Lien LF et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab 2009; 9: 311–326.
Lynch CJ, Adams S . Branched-chain amino acids in metabolic signalling and insulin resistance. Nat Rev Endocrinol 2014; 10: 723–736.
Lackey DE, Lynch CJ, Olson KC, Mostaedi R, Ali M, Smith WH et al. Regulation of adipose branched-chain amino acid catabolism enzyme expression and cross-adipose amino acid flux in human obesity. Am J Physiol Endocrinol Metab 2013; 304: E1175–E1187.
Yamakado M, Tanaka T, Nagao K, Ishizaka Y, Mitushima T, Tani M et al. Plasma amino acid profile is associated with visceral fat accumulation in obese Japanese subjects. Clin Obes 2012; 2: 29–40.
Tochikubo O, Nakamura H, Jinzu H, Nagao K, Yoshida H, Kageyama N et al. Weight loss is associated with plasma free amino acid alterations in subjects with metabolic syndrome. Nutr Diabetes 2016; 6: e197.
Wang TJ, Larson MG, Vasan RS, Cheng S, Phee EP, McCabe E et al. Metabolite profiles and the risk of developing diabetes. Nat Med 2011; 17: 448–454.
Floegel A, Stefan N, Yu Z, Muhlenbruch K, Drogan D, Joost HG et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes 2013; 62: 639–648.
Kume S, Araki S, Ono N, Shinhara A, Muramatsu T, Araki H et al. Predictive properties of plasma amino acid profile for cardiovascular disease in patients with type 2 diabetes. PLoS ONE 2015; 9: e101219.
Yamakado M, Nagao K, Imaizumi A, Tani M, Toda A, Tanaka T et al. Plasma free amino acid profiles predict four-year risk of developing diabetes, metabolic syndrome, dyslipidemia, and hypertension in Japanese population. Sci Rep 2015; 5: 11918.
Tai ES, Tan MLS, Stevens RD, Low YL, Muehlbauer MJ, Goh DLM et al. Insulin resistance is associated with a metabolic profile of altered protein metabolism in Chinese and Asian-Indian men. Diabetologia 2010; 53: 757–767.
Huffman KM, Shah SH, Stevens RD . Relationships between circulating metabolic intermediates and insulin action in overweight to obese, inactive men and women. Diabetes Care 2009; 32: 1678–1683.
Bi X, Tey SL, Leong C, Quek R, Loo YT, Henry CJ . Correlation of adiposity indices with cardiovascular disease risk factors in healthy adults of Singapore: a cross-sectional study. BMC Obesity 2016; 3: 33.
Bi X, Tey SL, Leong C, Quek R, Henry CJ . Prevalence of vitamin D deficiency in Singapore: its implications to cardiovascular risk factors. PLoS ONE 2016; 11: e0147616.
Shah SH, Crosslin DR, Haynes CS . Branched-chain amino acid levels are associated with improvement in insulin resistance with weight loss. Diabetologia 2012; 55: 321–330.
McCormack SE, Shaham O, McCarthy MA . Circulating branched-chain amino acid concentrations are associated with obesity and future insulin resistance in children and adolescents. Pediatr Obes 2013; 8: 52–61.
Magnusson M . A diabetes-predictive amino acid score and future cardiovascular disease. Eur Heart J 2013; 34: 1982–1989.
Hattersley JG, Pfeiffer AFH, Roden M, Petzke KJ, Hoffmann D, Rudovich NN et al. Modulation of amino acid metabolic signatures by supplemented isoenergetic diets differing in protein and cereal fiber content. J Clin Endocrinol Metab 2014; 99: E2599–E2609.
Tillin T, Hughes AD, Wang Q . Diabetes risk and amino acid profiles: cross-sectional and prospective analyses of ethnicity, amino acids and diabetes in a South Asian and European cohort from the SABRE (Southall and brent revisited) study. Diabetologia 2015; 58: 968–979.
She P, VanHorn CG, Reid T, Hutson SM . Obesity-related elevations in plasma leucine are associated with defective branched chain amino acid (BCAA) metabolism. FASEB J 2007; 21: 830.3.
Gogna N, Krishna M, Oommen AM, Dorai K . Investigating correlations in the altered metabolic profiles of obese and diabetic subjects in a South Indian Asian population using an NMR-based metabolomic approach. Mol Biosyst 2015; 11: 595–606.
Arner P . Catecholamine-induced lipolysis in obesity. Int J Obes 1999; 23: 10–13.
Fiehn O, Garvey WT, Newman JW, Lok KH, Hoppel CL, Adams SH . Plasma metabolomic profiles reflective of glucose homeostasis in non-diabetic and type 2 diabetic obese African-American women. PLoS One 2010; 5: e15234.
Elshorbagy AK, Nurk E, Gjesdal CG, Tell GS, Ueland PM, Nygard O et al. Homocysteine, cysteine, and body composition in the Hordaland Homocysteine Study: does cysteine link amino acid and lipid metabolism? Am J Clin Nutr 2008; 88: 738–746.
Stone KP, Wanders D, Orgeron M, Cortez CC, Gettys TW . Mechanisms of increased in vivo insulin sensitivity by dietary methionine restriction in mice. Diabetes 2014; 63: 3721–3733.
Holecek M . Relation between glutamine, branched-chain amino acids, and protein metabolism. Nutrition 2002; 18: 130–133.
Nakamura H, Jinzu H, Nagao K, Noguchi Y, Shimba N, Miyano H et al. Plasma amino acid profiles are associated with insulin, C-peptide and adiponectin levels in type 2 diabetic patients. Nutr Diabetes 2014; 4: e133.
Zhang Y, Guo K, LeBlanc RE, Loh D, Schwartz GJ, Yu YH . Increasing dietary leucine intake reduces diet-induced obesity and improves glucose and cholesterol metabolism in mice via multimechanisms. Diabetes 2007; 56: 1647–1654.
Torres-Leal FL, Fonseca-Alaniz MH, Teodoro GFR, Capitani MD, Vianna D, Pantaleao LC et al. Leucine supplementation improves adiponectin and total cholesterol concentrations despite the lack of changes in adiposity or glucose homeostasis in rats previously exposed to a high-fat diet. Nutr Metab 2011; 8: 62.
Ohara M, Doi H, Hayasi M, Satomi S . Administration of L-valine lowered plasma cholesterol by accelerating the conversion of cholesterol into bile acid. Clin Nutr 2003; 22: S57.
Weickert MO, Roden M, Isken F, Hoffmann D, Nowotny P, Osterhoff M et al. Effects of supplemented isoenergetic diets differing in cereal fiber and protein content on insulin sensitivity in overweight humans. Am J Clin Nutr 2011; 94: 459–471.
Shimomura Y, Honda T, Shiraki M, Murakami T, Sato J, Kobayashi H et al. Branched-chain amino acid catabolism in exercise and liver disease. J Nutr 2006; 136: 250S–253S.
Acknowledgements
We greatly acknowledge the financial support from Singapore Institute for Clinical Sciences, Agency for Science, Technology, and Research (A*Star), Singapore. Clinical Trial No: ACTRN12614000643673.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bi, X., Tey, S., Loo, Y. et al. Central adiposity-induced plasma-free amino acid alterations are associated with increased insulin resistance in healthy Singaporean adults. Eur J Clin Nutr 71, 1080–1087 (2017). https://doi.org/10.1038/ejcn.2017.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.34
- Springer Nature Limited