Abstract
Eggs are rich in nutrients and a source of essential fatty- and amino acids, and the food item with highest cholesterol content. Since the 1970s dietary recommendations have advised limiting egg intake to 2–4 a week for the healthy population, and in those diagnosed with cardiovascular disease (CVD) and type 2 diabetes (T2D) an even more restricted consumption. The aim of the present paper was to assess the recommendation to lower the dietary intake of cholesterol and especially the intake of egg to reduce the risk of CVD and T2D. We performed three web-based literature searches on human studies (observational and interventional) published within the past 10 years during spring 2015. High-quality intervention studies have found nonsignificant effects of increasing the consumption of eggs on risk markers for CVD and T2D in healthy subjects and subjects with T2D. The risk associations found in the observational studies are more likely to be attributed to a dietary pattern often accompanying high egg intake and/or the cluster of other risk factors in people with high egg consumption. Dietary patterns, physical activity and genetics affect the predisposition of CVD and T2D more than a single food item as eggs. In conclusion, up to seven eggs per week can safely be consumed, but in patients with established CVD or T2D only with special emphasis on a healthy lifestyle.
Similar content being viewed by others
Introduction
The incidence of coronary heart disease (CHD), which globally still is the most frequent cause of death, has since the 1980s declined dramatically in most countries in the western Hemisphere. It is still unknown to what extent the various preventive actions including dietary guidelines have contributed to the successful prevention. It seems relevant to assess the effect of some of the recommendations in the dietary guidelines in light of information from newer studies and the use of modern statistical methods applied on the results of the studies. In the present paper we assess the recommendation to lower the dietary intake of cholesterol and especially the intake of egg.
Previous and present dietary advices regarding egg and cholesterol consumption
The most common size of chicken egg is 'Large' (greater than 2 oz. or 54.4 g) and is the size commonly referred to in food recipes. More than half of the calories found in eggs come from fat in the yolk; 56 g of chicken egg (the contents of an egg just large enough to be classified as ‘large’ in the United States, but ‘medium’ in Europe) contains approximately 5 g of fat. The energy content per 100 g is 131 kcal (547 kJ), saturated fatty acids 2.52 g, cis-monounsaturated fatty acids 3.43 g, cis-n3 fatty acids 0.13 g, cis-n6 fatty acids 1.31 g, cis-polyunsaturated fatty acids 1.44 g, trans-fatty acids 0.01 g and cholesterol 350 mg.1
Healthy people
The high cholesterol in chicken eggs has in the past been the reason for recommendations advising healthy people to eat at the most 2-4 eggs per week in prevention of cardiovascular disease (CVD). Setting an international benchmark, the Dietary Guidelines for Americans have in many years recommended people to limit cholesterol and egg consumption.2, 3 For this reason the past two generations of Americans have reduced the consumption of eggs and other animal products as they were told that fat and cholesterol were bad for their health. Globally, egg consumption has been, and still, is highest in Europe; Europeans consumes an average of approximately 3.5 eggs per person per week (Figure 1).4 The country consuming most eggs globally is Denmark, where egg consumption has increased since 1960 and is presently 4.6 eggs per person per week (Figure 2).4 This may reflect that the Nordic Nutrition Recommendations have not restricted egg consumption.
Internationally there is still no consensus on the recommendations of egg consumption for healthy people (Table 1). The preliminary report on the new Dietary Guidelines for Americans (released February 2015) stated, quite opposite to the existing Dietary Guidelines for Americans, that ‘cholesterol is not a nutrient of concern for overconsumption’.5 Thus, it was surprising that the Dietary Guidelines for Americans 2015 once again included the statement ‘individuals should eat as little cholesterol as possible’ together with the statement ‘Adequate evidence is not available for a quantitative limit for dietary cholesterol specific to the dietary guideline’.6 These opposite statements about the same dietary substance in the same guidelines have led to some concern.7, 8 The Nordic Nutrition Recommendations in 2004 and again in 2012 did not set an upper intake level for dietary cholesterol.9, 10
Patients with CVD
For patients diagnosed with CVD the Mayo Clinic11 and, as the only out of seven national Heart Associations, the German Heart Association,12 recommend limiting the consumption of eggs and dietary cholesterol (Table 2). Other national Heart Associations have in recent years loosened the restrictions on dietary cholesterol.13 In 2000, the American Heart Association (AHA) still recommended restricting dietary cholesterol.14 But the AHA's guidelines were further revised in 2014 giving the green light to enjoy eggs.15 The British Heart Foundation states that ‘it's a myth that eggs are bad for your heart. Eggs can form part of a balanced diet, despite their perceived ‘bad’ reputation due to their cholesterol content’.16 The National Heart Foundation of Australia likewise states: ‘Good news on eggs: Did you know that blood cholesterol levels are more influenced by the saturated and trans fat we eat than the cholesterol in foods? That's why it's OK to eat eggs - you can enjoy up to six eggs each week as part of a healthy balanced diet’.17 The Danish Heart Association today says that ‘eggs are a good source of protein and vitamins and can be included as part of a varied and heart-friendly diet, but be aware in that the egg yolk is high in both fat and cholesterol’.18
Atherosclerotic mechanism
Accumulation of low-density lipoprotein (LDL)-cholesterol from plasma in the subendothelial space of the coronary arteries is an important process in the development of CHD. The transfer of LDL-cholesterol into the arterial wall increases with increasing concentration of LDL-cholesterol in plasma, but is also dependent on the resistance of the endothethelial layer to macromolecular permeation. Cholesterol cannot be metabolized in the arterial wall. It can however be removed and brought to the liver by various processes of which some may involve high-density lipoprotein (HDL). LDL-cholesterol in the arterial wall is taken up by macrophages which eventually may develop to foam cells that constitute an important part of the atherosclerotic lesion. This simple description of the development of the atherosclerotic lesion demonstrates that there are several ways that atherogenesis can be affected: (1) by changes in plasma LDL cholesterol, (2) by changes in endothelial cells and (3) by changes in reverse cholesterol transfer from artery to plasma and further on to the liver. The risk related to the intake of eggs has so far relied on the increase of LDL-cholesterol in plasma, but it is possible that intake of eggs may interfere with the other processes involved in atherogenesis. The development of atherosclerotic lesions also depends on the propensity of the macrophages in the arterial wall to take up oxidized LDL-cholesterol ending up as foam cells. This process has recently attracted some attention since trimethylamine-N oxide (TMAO) seems to promote the formation of foam cells. Trimethylamine (TMA) is formed in the intestinal microbiota from choline-rich substances like phophatidylcholine, present in relatively large amounts in egg yolks. When TMA reach the liver it is oxidized to TMAO.19 TMAO concentrations in plasma increase with increasing intake of eggs.20, 21 TMAO concentrations in plasma seem to be a powerful predictor of total mortality in patients with CHD even after adjustment for other known risk factors.22, 23 This theory makes eggs and other choline-containing food items, that is, all animal products pro-atherogenic, not because of their cholesterol content but because of their choline content being the precursor for the microbiota to form TMA. Several authors have however cautioned against letting the findings with egg ingestion and TMAO production have influence on dietary guidelines before further studies are done. This seems sensible due to phophatidylcholine is ubiquitous in our diet, thus eliminating phophatidylcholine would mean reducing the intake of many apparently healthy foods.
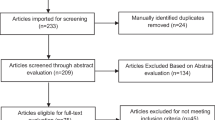
Literature search
Three literature searches on human studies within the past 10 years were performed during April–May 2015. The first search identified clinical trials with the terms: ‘egg and cholesterol’ (n=36), ‘egg and diabetes’ (n=11), ‘egg and cardiovascular’ (n=21). After removing duplicates, 33 studies were evaluated. Twelve articles were excluded for the following reasons: irrelevant outcome (n=4), multiple publications (n=6) and only abstract available in English (n=2). The second search identified observational studies with search terms: ‘egg’ and ‘cholesterol’ or ‘diabetes’ or ‘cardiovascular’ (n=18). Two studies were excluded as being irrelevant to the outcome of interest (cancer and pregnancy). Twelve studies had CVD as outcome,24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35 and four had diabetes as outcome.36, 37, 38, 39 The third search identified meta-analyses and systematic reviews with search terms: ‘egg’ and ‘cholesterol’ or ‘diabetes’ or ‘cardiovascular’; four publications were identified, one being both a meta-analysis and systematic review.40, 41, 42, 43 Subsequent initial search two observational studies,44, 45, 46 one clinical trial47 and three meta-analyses have been identified.48, 49, 50
Of the intervention studies investigating the effect of egg consumption on risk markers of CVD or diabetes among subjects not at high risk of—and without established—heart disease 12 studies were randomized controlled trial,51, 52, 53, 54, 55, 56, 57, 58, 59, 60 8 were crossover trials61, 62, 63, 64, 65 and 1 intervention was non-randomized controlled66 (Table 3). Five interventions were conducted in people with high risk of CVD or with established artery disease; two were randomized controlled trial67, 68 and three were crossover47, 69, 70 studies. All interventions were evaluated as ‘good’, ‘fair’ or ‘poor’ using the ‘Quality Assessment of Controlled Intervention Studies from National Institutes of Health’ 2014 and GRADE system (grading quality of evidence and strength of recommendations).71, 72 Only five studies, all randomized controlled trials, were evaluated as of good quality51, 52, 53, 54, 55 (Table 3), the remaining studies were either of fair or poor quality.
Observational studies
During the past decade many of the numerous investigations of ‘the diet-heart hypothesis’ have been included in systematic reviews and meta-analysis (Table 4).41, 42, 43, 48, 49, 50 They include data on the associations of egg consumption and the risk of CVD and cardiac mortality as well as the incidence of type 2 diabetes (T2D) in the general population, and also the relationship between egg consumption and CVD risk in patients with known T2D.
Only three studies have included subjects with established CVD, not included in any meta-analysis.32, 33, 34
Healthy people
Among the reviews and meta-analysis including healthy subjects, there is no consensus of an association of egg consumption and the risk of CVD and T2D (Table 4). In a meta-analysis of prospective cohort studies, Shin et al.43 found that egg consumption was not associated with the risk of CVD, cardiac mortality or total mortality in the general population. They did however, in a subanalysis, find that the highest compared with lowest egg consumption was associated with an increased hazard ratio (HR) of T2D (1.42 95% CI: 1.09–1.86). Li et al.41 included 14 studies involving 320 778 subjects and found a dose–response relationship between egg consumption and the risk of CVD and T2D. An increment of four eggs per week increased the relative risk (RR) for CVD and T2D of 1.06 (95% CI: 1.03–1.10) and 1.29 (95% CI: 1.21–1.37), respectively. Rong et al.42 performed a dose–response meta-analysis of prospective cohort studies with 17 reports including subgroups of diabetics (four reports) to quantify the association between egg consumption and risk of CVD and stroke. They found no evidence of an association between egg consumption and risk of CHD or stroke. In a meta-analysis including 17 cohorts of healthy adults, Berger et al.48 found no association between dietary cholesterol and the relative risk of ischemic stroke 1.13 (95% confidence interval (CI): 0.99–1.28) or hemorrhagic stroke 1.09 (95% CI: 0.79–1.50). In a meta-analysis including 12 cohorts, Djoussé et al.49 found increased risk of T2D with consumption of three or more eggs per week, but only in US studies. In a meta-analysis including 14 studies with healthy subjects, Alexander et al.50 found 12% decreased risk of stroke (0.88 (95% CI: 0.81–0.97)) and no association of CHD (0.97 (95% CI: 0.88–1.07)) with consumption of one egg per day compared with less than two eggs per week.
Three newly published observational studies are not included in any meta-analysis.33, 44, 45 In a cohort including approximately 70 000 Swedish men and women, Larsson et al.44 found no association with egg consumption and risk of myocardial infarction and stroke. They did find that consumption of more than one egg a day, but not less frequent consumption, was associated with increased risk of heart failure in men, but not in women (RR for men 1.30 (95% CI: 1.01, 1.67)). Among subjects included in the NHLBI (National Heart, Lung, and Blood Institute) Family Heart Study with no established CVD, Robbins et al.45 found no association between egg consumption and prevalence of coronary-artery calcium content. Choi et al.33 investigated the association between egg consumption and coronary artery calcium content in healthy South Korean subjects. In a multi-variable adjusted model they found higher prevalence of detectable coronary artery calcium in subjects consuming seven or more eggs per week than in subjects consuming less than one egg per week (1.80 (95% CI: 1.14–2.83)). The authors conclude that egg consumption is positively associated with coronary atherosclerosis and that this may be mediated by the cholesterol in eggs.33 The association was more pronounced in subjects with high body mass index and in those with low vegetable intake.
Diabetic subjects
Dietary cholesterol and egg intake have been associated with increased risk of CVD in people with T2D, in most studies that have assessed them (Table 4). The meta-analysis by Shin et al.43 included a database of 7549 diabetic patients in four cohorts. Patients with diabetes who ate eggs more than once per day were 1.69 times as likely to develop a CVD comorbidity than patients who never ate eggs or ate less than once per week (pooled HR: 1.69 (95% CI: 1.09–2.62)). However, egg consumption was not significantly associated with risk of overall mortality. In a review by Tran et al.40 they find no consistency in egg consumption of the risk of T2D. The authors, however, found the cohort studies significantly incomparable in study design and having limitations, not suitable for a meta-analysis. In the meta-analysis by Li et al.,41 it was found that the association between egg consumption and the risk of CVD seemed even more obvious in diabetic patients. For each increment of four eggs per week the relative risk of CVD increased by 1.40 (95% CI: 1.25, 1.57). Among diabetic patients consuming two or more eggs per day compared with less than one egg per week, Rong et al.42 found higher relative risk of CHD and lower risk of developing hemorrhagic stroke, 1.54 (95% CI: 1.14, 2.09) and 0.75 (95% CI: 0.57 to 0.99) respectively. One study included in the meta-analysis by Rong et al. found no association among diabetics,31 and the other does not describe a diabetic subgroup.27
Djoussé et al.36 found positive association between egg consumption and prevalence of T2D in African-American subjects (prevalence ratio for ⩾5 eggs/week vs <1 egg/month was 1.52 (95% CI: 1.17, 1.97). Among subjects without T2D they found no association with biomarkers of diabetes nor did they find an association between egg consumption and development of T2D after 7.3 years follow-up (HR for ⩾5 eggs/week vs <1 egg/month was 1.17 (95% CI: 0.81, 1.70)). In a subgroup analysis including subjects with T2D, Robbins et al.45 found no association between egg consumption and coronary-artery calcium content.
High CVD risk subjects
Among 1262 at risk patients Spence et al.32 found carotid plaque area to increase exponentially with egg-yolk years (P<0.0001); this remained significant after adjusting for coronary risk factors. Due to numerous confounding factors in the study, for example, recall of food ingestion, standard deviations exceeding mean in both groups, age difference between groups (for editorials following its publication please see refs 73, 74, 75), these results should however be interpreted with caution. Among 382 adults referred to undergo coronary angiography Chagas et al.34 found egg consumption inversely associated with dyslipidemia (P=0.031) and that those who ate more than one egg per week had a lower atherosclerotic burden (P=0.033). Among 1032 men, where 32.5% were carriers of the apolipoprotein E gene 4 (i.e. highly susceptible individuals), Virtanen et al.46 found no association between consumption of egg or cholesterol and the risk of coronary artery disease; HR of 1.17 (95% CI: 0.85, 1.61) in the noncarriers and an HR of 0.93 (95% CI: 0.50, 1.72) in the carriers.
Intervention studies
In total, 23 interventions have assessed the effect of egg consumption on cardiovascular risk markers; 17 including healthy subjects (i.e. subjects without T2D, not at high risk of or already established CVD), 2 including diabetics and 4 including subjects at high risk of or with already established CVD (Table 3).
Among healthy subjects two studies found egg consumption to increase LDL cholesterol; Baumgartner et al.58 found that adding an extra egg a day to the habitual diet of healthy subjects increased total and LDL cholesterol after 12 weeks. But when examining the mean results there is a higher increase of total and LDL cholesterol in the control group compared with the egg group. Further, these results should be interpreted with caution due to the quality of this study. Subjects were not equally randomized, the groups were very small, and there was no intention to treat analysis. Knopp et al.76 found increased LDL and HDL after one month’s consumption of four egg yolks a day among insulin-resistant subjects with habitual low intake of cholesterol. Including four egg yolks in the daily diet will most likely change the habitual dietary pattern, but no data on total dietary intake are presented in the paper.
All other interventions found no adverse effects on blood lipids of a high versus low egg consumption.52, 54, 61, 69 Even up to 1 year of intervention with 1.5 egg yolk a day had no effect on blood lipids among 101 elderly subjects.53 On the contrary, consumption of 1–3 eggs daily during 8–12 weeks increased HDL in healthy adults.65, 77 In an 8-week weight loss intervention, an energy-restricted diet containing egg increased weight loss and reduced waist circumference and fat mass compared with a diet with no eggs.54
Among subjects diagnosed with T2D consumption of two eggs a day for 12 weeks increased satiety, reduced hunger and increased HDL compared with a low egg diet (less than two eggs per week).51, 56
Among subjects at high risk of heart disease (metabolic syndrome) consumption of up to three eggs a day during 12 weeks increased HDL and in one study also reduced VLDL and insulin levels.67, 68 Among subjects with hyperlipidemia or diagnosed coronary artery disease a single dose of three eggs or consumption of two eggs daily during 6 weeks had no effect on endothelial function nor on blood lipids.69, 70 Thirty-four adults with T2D had improvements in their anthropometric measurements after two eggs a day during 12 weeks; there was no effect on glycated hemoglobin or systolic blood pressure.47
A recent meta-analysis including 17 intervention studies by Berger et al.48 found dietary cholesterol until 900 mg/day to increase concentrations of total, LDL and HDL cholesterol but not triglycerides or very low-density lipoproteins. With dietary cholesterol above 900 mg/day, HDL persisted to increase but total and LDL cholesterol did not, this suggests a plateauing effect when dietary cholesterol increases,48 which is consistent with previous observations.78
Discussion
In 1971 the data on initial serum cholesterol and the risk of CHD after 14 years in The Framingham Study were published.79 The study found that elevated cholesterol was associated with an increased risk of CHD. Though not aiming at any specific cause of elevated serum cholesterol in the article, the results lead to a further establishment of the ‘diet-heart disease hypothesis’. This hypothesis proposed that elevated serum cholesterol was a direct cause of excess dietary cholesterol and saturated fat intake, and that egg consumption consequently should be limited to achieve a low intake of cholesterol.80 A later analysis of the data from The Framingham Study found however no association between egg consumption and serum cholesterol, all cause death, total CHD, myocardial infarction or angina pectoris.80 In spite of this, egg consumption has been the focus of investigation in many studies, and limited egg consumption has been recommended to minimize CHD risk, and in dietary recommendations to people with T2D.
In the observational studies including a mix of healthy persons and diabetics, the subjects have been categorized according to number of eggs consumed per month or week with the group with lowest intake set as reference.33, 36, 81 When reviewing the baseline study characteristics of anthropometry and dietary intake, subjects with the highest egg consumption (five or more or seven or more per week) share several characteristics known to influence the development of heart diseases and diabetes, different from the reference group. A greater proportion is typically males, smokers and persons with higher body mass index; a higher intake of energy, total fat/saturated fat, and of red and processed meat, and a lower intake of fruit and vegetables.25, 33, 36, 37, 81 Out of the observational studies investigating the association of egg consumption on CVD and T2D only two measured intake of trans fatty acids at baseline.36, 39 One study, a study of African American, found a positive association between egg and prevalent T2D, the subjects with high egg consumption had a daily 2 g higher intake of trans fat.36 The other, a study of Finnish men, found a 38% lower risk among those consuming more eggs than those consuming little. In this study there was no difference in intake of trans fat among groups.39 It is well recognized that dietary saturated and especially trans-fat have an adverse effect on LDL-cholesterol and the risk of CHD.82, 83, 84 Intake of trans-fat should therefore be measured and controlled for in all the observational studies.
A recent randomized controlled trial of high quality investigated the effect of a 3-month high-egg diet on blood lipids among obese subjects with T2D.51 The only differences between the groups were that the high-egg group had a 2-year longer history of T2D, and slightly higher total-, LDL- and HDL cholesterol. The diets were energy and nutrient matched. After intervention there were no differences between the groups on any risk markers of T2D or CVD, nor in body weight or fat-free mass. The high-egg group had reduced hunger and increased satiety.
As opposed to several prospective studies and meta-analyses41 high-quality intervention studies do not support that there is any adverse effect of egg consumption of up to two eggs per day on risk markers of CVD or T2D (Table 3).51, 52, 53, 55, 56, 67, 69, 70 Studies investigating the effect of increased egg consumption and restricted energy intake found either no difference in plasma lipids between groups or increased HDL after egg consumption.52, 54, 56 These studies also assessed anthropometry and found egg consumption to promote weight loss and reduce waist circumference.54, 56 This correlates well with egg consumption increasing satiety and reducing hunger as found by Fuller et al.51 The effect of egg consumption on reducing energy intake is likely to be attributed by the high content of protein that is well acknowledged to improve weight loss, weight loss maintenance and reduce obesity-related comorbidities.85, 86 Berger et al.48 concludes in their meta-analysis, including both observational and intervention trials, that there is lack of longitudinal data to support a limitation of dietary cholesterol.
The statistical approach to interpret the data from prospective studies is crucial to the outcome. A study including the data from 18 987 participants, including data on egg consumption, measures of adiposity and cardiovascular risk factors, examined the potential association between egg consumption and adiposity through two different statistical models.87 In the first they found egg consumers to have both higher body mass index and waist circumference than non-egg consumer. In the other they identified eight clusters among those consuming eggs, where only two patterns drove an association between egg consumption and body mass index and waist circumference before controlled against standard covariates. After adjustment one pattern remained associated with increased diastolic blood pressure and serum LDL; but after adjustment for intake of junk food and medication no associations were present. These results underscore the significance of not only assessing a single dietary component when seeking to find dietary factors enhancing the risk of development of CVD and T2D.
The suggestion of egg consumption by itself promotes the risk and development heart disease and diabetes seems improbable compared with the general complexity of the dietary pattern, physical activity and genetic predisposition. The risk of developing heart diseases is more likely to be attributed to a lifestyle and dietary pattern often accompanying high egg intake or the cluster of other risk factors that differ in people with high egg consumption compared with those with lower egg consumption. The lack of control for trans-fat intake in most studies is of concern.
Although some observational studies have found association between egg consumption and the risk of CVD, results from intervention trials have not been able to substantiate this. In high-quality intervention studies including healthy or patients with TD2 or hyperlipidemia, dietary cholesterol, primarily from eggs, does not have a clinically relevant effect on the concentration of serum cholesterol. Thereby there does not seem to be a mechanistic explanation as to why eggs should increase the risk of CVD or T2D. The lack of scientific consensus on eggs for patients at high risk for CVD or diagnosed with CVD or diabetes, has led some countries’ health organizations to refrain from a dietary recommendation on eggs to these groups. Australia and New Zealand have chosen to recommend all up to six eggs a week, but with the modification that the high-risk groups are well-treated (Table 2).88, 89 This appears for us a sensible strategy that to some extent excludes the bad reputation eggs have without the risk of putting the health at stake among patients at high risk for CVD or T2D.
In conclusion, If not for the dietary recommendations against the consumption of dietary cholesterol during the past half century, the current knowledge would most likely not be sufficient to restrict the intake of a nutrient rich basic food as eggs. Taken together up to seven eggs per week can safely be consumed, but in patients with established CVD or T2D only with special emphasis on a prudent diet and proper medical treatment.
References
Department of Health. Nutrient Analysis of Eggs—Summary Report. United Kingdom 2012.
Report of the dietary guidelines advisory committee on the dietary guidelines for Americans, 2010, to the Secretary of Agriculture and the Secretary of Health and Human Services. Secretary of Agriculture and Secretary of Health and Human Services 2010.
US Department of Health and Human Services Dietary Guidelines for Americans, 2005. US Department of Health and Human Services: USA, 2005.
GLOBAL POULTRY TRENDS 2013: European Egg Consumption Linked to Production and Population. The Poultry Site: 5m Publishing 2014.
McGuire S . Scientific report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: US Departments of Agriculture and Health and Human Services, 2015. Adv Nutr 2016; 7: 202–204.
2015-2020 Dietary Guidelines for Americans, 8th edn. US Department of Health and Human Services and US Department of Agriculture, USA 2015.
Nissen SE . US dietary guidelines: an evidence-free zone. Ann Intern Med 2016; 164: 558–559.
McNamara DJ . The fifty year rehabilitation of the egg. Nutrients 2015; 7: 8716–8722.
Nordic Nutrition Recommendations 2012: Integrating Nutrition and Physical Activity. Nordic Council of Ministers: Copenhagen, 2014.
Nordic Nutrition Recommendations 2004: Integrating Nutrition and Physical Activity. Nordic Council of Ministers: Copenhagen, 2005.
Lopez-Jimenez F, Eggs: Are they Good or Bad for My Cholesterol? Mayo Clinic 2014.
Gohlke H, Cholesterin: Wie können sich Herzpatienten schützen? Deutsche Herzstiftung 2010.
Gray J, Griffin B . Eggs and dietary cholesterol–dispelling the myth. Nutr Bull 2009; 34: 66–70.
Krauss RM, Eckel RH, Howard B, Appel LJ, Daniels SR, Deckelbaum RJ et al. AHA dietary guidelines revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation 2000 102: 2284–2299.
Eckel RH, Jakicic JM, Ard JD, De Jesus JM, Miller NH, Hubbard VS et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014; 63: 2960–2984.
British Heart Foundation. It's a Myth that Eggs are Bad for your Heart 2015.
The Australian Heart Foundation. Eggs. Australian Heart Foundation: Australia, 2015.
Det er ægge let. Hjerteforeningen 2012.
Tang WW, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 2013; 368: 1575–1584.
Miller CA, Corbin KD, da Costa K-A, Zhang S, Zhao X, Galanko JA et al. Effect of egg ingestion on trimethylamine-N-oxide production in humans: a randomized, controlled, dose-response study. Am J Clin Nutr 2014; 100: 778–786.
Hazen SL, Brown JM . Eggs as a dietary source for gut microbial production of trimethylamine-N-oxide. Am J Clin Nutr 2014; 100: 741–743.
Senthong V, Li XS, Hudec T, Coughlin J, Wu Y, Levison B et al. Plasma trimethylamine N-oxide, a gut microbe–generated phosphatidylcholine metabolite, is associated with atherosclerotic burden. J Am Coll Cardiol 2016; 67: 2620–2628.
Zheng Y, Li Y, Rimm EB, Hu FB, Albert CM, Rexrode KM et al. Dietary phosphatidylcholine and risk of all-cause and cardiovascular-specific mortality among US women and men. Am J Clin Nutr 2016; 104: 173–180.
Bernstein AM, Pan A, Rexrode KM, Stampfer M, Hu FB, Mozaffarian D et al. Dietary protein sources and the risk of stroke in men and women. Stroke 2012; 43: 637–644.
Djoussé L, Gaziano JM . Egg consumption and risk of heart failure in the Physicians’ Health Study. Circulation 2008; 117: 512–516.
Hu FB, Stampfer MJ, Rimm EB, Manson JE, Ascherio A, Colditz GA et al. A prospective study of egg consumption and risk of cardiovascular disease in men and women. JAMA 1999; 281: 1387–1394.
Nakamura Y, Okamura T, Tamaki S, Kadowaki T, Hayakawa T, Kita Y et al. Egg consumption, serum cholesterol, and cause-specific and all-cause mortality: the National Integrated Project for Prospective Observation of Non-communicable Disease and Its Trends in the Aged, 1980 (NIPPON DATA80). Am J Clin Nutr 2004; 80: 58–63.
Nakamura Y, Iso H, Kita Y, Ueshima H, Okada K, Konishi M et al. Egg consumption, serum total cholesterol concentrations and coronary heart disease incidence: Japan Public Health Center-based prospective study. Br J Nutr 2006; 96: 921–928.
Qureshi AI, Suri MFK, Ahmed S, Nasar A, Divani AA, Kirmani JF . Regular egg consumption does not increase the risk of stroke and cardiovascular diseases. Med Sci Technol 2006; 13: CR1–CR8.
Sauvaget C, Nagano J, Allen N, Grant EJ, Beral V . Intake of animal products and stroke mortality in the Hiroshima/Nagasaki Life Span Study. Int J Epidemiol 2003; 32: 536–543.
Scrafford CG, Tran NL, Barraj LM, Mink PJ . Egg consumption and CHD and stroke mortality: a prospective study of US adults. Public Health Nutr. 2011; 14: 261–270.
Spence JD, Jenkins DJ, Davignon J . Egg yolk consumption and carotid plaque. Atherosclerosis 2012; 224: 469–473.
Choi Y, Chang Y, Lee JE, Chun S, Cho J, Sung E et al. Egg consumption and coronary artery calcification in asymptomatic men and women. Atherosclerosis 2015; 241: 305–312.
Chagas P, Caramori P, Galdino TP, de Barcellos CdS, Gomes I, Schwanke CHA . Egg consumption and coronary atherosclerotic burden. Atherosclerosis 2013; 229: 381–384.
Goldberg S, Gardener H, Tiozzo E, Kuen CY, Elkind MS, Sacco RL et al. Egg consumption and carotid atherosclerosis in the Northern Manhattan Study. Atherosclerosis 2014; 235: 273–280.
Djoussé L, Petrone AB, Hickson DA, Talegawkar SA, Dubbert PM, Taylor H et al. Egg consumption and risk of type 2 diabetes among African Americans: The Jackson Heart Study. Clin Nutr 2016; 35: 679–684.
Kurotani K, Nanri A, Goto A, Mizoue T, Noda M, Oba S et al. Cholesterol and egg intakes and the risk of type 2 diabetes: The Japan Public Health Center-based Prospective Study. Br J Nutr 2014; 112: 1636–1643.
Radzevičienė L, Ostrauskas R . Egg consumption and the risk of type 2 diabetes mellitus: a case–control study. Public Health Nutr 2012; 15: 1437–1441.
Virtanen JK, Mursu J, Tuomainen T-P, Virtanen HE, Voutilainen S . Egg consumption and risk of incident type 2 diabetes in men: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am J Clin Nutr 2015; 101: 1088–1096.
Tran NL, Barraj LM, Heilman JM, Scrafford CG . Egg consumption and cardiovascular disease among diabetic individuals: a systematic review of the literature. Diabetes Metab Syndr Obes 2014; 7: 121.
Li Y, Zhou C, Zhou X, Li L . Egg consumption and risk of cardiovascular diseases and diabetes: a meta-analysis. Atherosclerosis 2013; 229: 524–530.
Rong Y, Chen L, Zhu T, Song Y, Yu M, Shan Z et al. Egg consumption and risk of coronary heart disease and stroke: dose-response meta-analysis of prospective cohort studies. BMJ 2013; 346: e8539.
Shin JY, Xun P, Nakamura Y, He K . Egg consumption in relation to risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. Am J Clin Nutr 2013; 98: 146–159.
Larsson SC, Åkesson A, Wolk A . Egg consumption and risk of heart failure, myocardial infarction, and stroke: results from 2 prospective cohorts. Am J Clin Nutr 2015; 102: 1007–1013.
Robbins JM, Petrone AB, Ellison RC, Hunt SC, Carr JJ, Heiss G et al. Association of egg consumption and calcified atherosclerotic plaque in the coronary arteries: the NHLBI Family Heart Study. e-SPEN J 2014; 9: e131–e135.
Virtanen JK, Mursu J, Virtanen HE, Fogelholm M, Salonen JT, Koskinen TT et al. Associations of egg and cholesterol intakes with carotid intima-media thickness and risk of incident coronary artery disease according to apolipoprotein E phenotype in men: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am J Clin Nutr 2016; 103: 895–901.
Njike VY, Ayettey RG, Rajebi H, Treu JA, Katz DL . Egg ingestion in adults with type 2 diabetes: effects on glycemic control, anthropometry, and diet quality—a randomized, controlled, crossover trial. BMJ Open Diabetes Res Care 2016; 4: e000281.
Berger S, Raman G, Vishwanathan R, Jacques PF, Johnson EJ . Dietary cholesterol and cardiovascular disease: a systematic review and meta-analysis. Am J Clin Nutr 2015; 102: 276–294. ajcn100305.
Djoussé L, Khawaja OA, Gaziano JM . Egg consumption and risk of type 2 diabetes: a meta-analysis of prospective studies. Am J Clin Nutr 2016; 103: 474–480.
Alexander DD, Miller PE, Vargas AJ, Weed DL, Cohen SS . Meta-analysis of egg consumption and risk of coronary heart disease and stroke. J Am Coll Nutr 2016; 35: 1–13.
Fuller NR, Caterson ID, Sainsbury A, Denyer G, Fong M, Gerofi J et al. The effect of a high-egg diet on cardiovascular risk factors in people with type 2 diabetes: the Diabetes and Egg (DIABEGG) study—a 3-mo randomized controlled trial. Am J Clin Nutr 2015; 101: 705–713.
Harman NL, Leeds AR, Griffin BA . Increased dietary cholesterol does not increase plasma low density lipoprotein when accompanied by an energy-restricted diet and weight loss. Eur J Nutr 2008; 47: 287–293.
van der Made SM, Kelly ER, Berendschot TT, Kijlstra A, Lütjohann D, Plat J . Consuming a buttermilk drink containing lutein-enriched egg yolk daily for 1 year increased plasma lutein but did not affect serum lipid or lipoprotein concentrations in adults with early signs of age-related macular degeneration. J Nutr 2014; 144: 1370–1377.
Vander Wal J, Gupta A, Khosla P, Dhurandhar N . Egg breakfast enhances weight loss. Int J Obes 2008; 32: 1545–1551.
Vislocky LM, Pikosky MA, Rubin KH, Vega-López S, Gaine PC, Martin WF et al. Habitual consumption of eggs does not alter the beneficial effects of endurance training on plasma lipids and lipoprotein metabolism in untrained men and women. J Nutr Biochem 2009; 20: 26–34.
Pearce KL, Clifton PM, Noakes M . Egg consumption as part of an energy-restricted high-protein diet improves blood lipid and blood glucose profiles in individuals with type 2 diabetes. Br J Nutr 2011; 105: 584–592.
Bunger M, Quataert M, Kamps L, Versloot P, Hulshof PJ, Togtema A et al. Bioavailability of lutein from a lutein-enriched egg-yolk beverage and its dried re-suspended versions. Int J Food Sci Nutr 2014; 65: 903–909.
Baumgartner S, Kelly ER, van der Made S, Berendschot TT, Husche C, Lütjohann D et al. The influence of consuming an egg or an egg-yolk buttermilk drink for 12 wk on serum lipids, inflammation, and liver function markers in human volunteers. Nutrition 2013; 29: 1237–1244.
Iglay H, Apolzan J, Gerrard D, Eash J, Anderson J, Campbell W . Moderately increased protein intake predominately from egg sources does not influence whole body, regional, or muscle composition responses to resistance training in older people. J Nutr Health Aging 2009; 13: 108–114.
Wenzel AJ, Gerweck C, Barbato D, Nicolosi RJ, Handelman GJ, Curran-Celentano J . A 12-wk egg intervention increases serum zeaxanthin and macular pigment optical density in women. J. Nutr. 2006; 136: 2568–2573.
Greene CM, Zern TL, Wood RJ, Shrestha S, Aggarwal D, Sharman MJ et al. Maintenance of the LDL cholesterol: HDL cholesterol ratio in an elderly population given a dietary cholesterol challenge. J Nutr 2005; 135: 2793–2798.
Nissinen MJ, Gylling H, Miettinen TA . Responses of surrogate markers of cholesterol absorption and synthesis to changes in cholesterol metabolism during various amounts of fat and cholesterol feeding among healthy men. Br J Nutr 2008; 99: 370–378.
Burns-Whitmore B, Haddad E, Sabaté J, Rajaram S . Effects of supplementing n-3 fatty acid enriched eggs and walnuts on cardiovascular disease risk markers in healthy free-living lacto-ovo-vegetarians: a randomized, crossover, free-living intervention study. Nutr J 2014; 13: 29.
Goodrow EF, Wilson TA, Houde SC, Vishwanathan R, Scollin PA, Handelman G et al. Consumption of one egg per day increases serum lutein and zeaxanthin concentrations in older adults without altering serum lipid and lipoprotein cholesterol concentrations. J Nutr 2006; 136: 2519–2524.
Vishwanathan R, Goodrow-Kotyla EF, Wooten BR, Wilson TA, Nicolosi RJ . Consumption of 2 and 4 egg yolks/d for 5 wk increases macular pigment concentrations in older adults with low macular pigment taking cholesterol-lowering statins. Am J Clin Nutr 2009; 90: 1272–1279.
Rueda JM, Khosla P . Impact of breakfasts (with or without eggs) on body weight regulation and blood lipids in university students over a 14-week semester. Nutrients 2013; 5: 5097–5113.
Mutungi G, Ratliff J, Puglisi M, Torres-Gonzalez M, Vaishnav U, Leite JO et al. Dietary cholesterol from eggs increases plasma HDL cholesterol in overweight men consuming a carbohydrate-restricted diet. J Nutr 2008; 138: 272–276.
Blesso CN, Andersen CJ, Barona J, Volek JS, Fernandez ML . Whole egg consumption improves lipoprotein profiles and insulin sensitivity to a greater extent than yolk-free egg substitute in individuals with metabolic syndrome. Metabolism 2013; 62: 400–410.
Katz DL, Gnanaraj J, Treu JA, Ma Y, Kavak Y, Njike VY . Effects of egg ingestion on endothelial function in adults with coronary artery disease: a randomized, controlled, crossover trial. Am Heart J 2015; 169: 162–169.
Njike V, Faridi Z, Dutta S, Gonzalez-Simon AL, Katz DL . Daily egg consumption in hyperlipidemic adults—effects on endothelial function and cardiovascular risk. Nutr J 2010; 9: 28.
Quality Assessent of Controlled Intervention Sstudies. National Institut of Health 2014.
GRADEWorkingGroup. Grading quality of evidence and strength of recommendations. Br Med J 2004; 328: 1490.
Olver TD, Thomas GW, Hamilton CD, Spence N . Putting eggs and cigarettes in the same basket; are you yolking? Atherosclerosis 2013; 227: 184–185.
Zampelas A . Still questioning the association between egg consumption and the risk of cardiovascular diseases. Atherosclerosis 2012; 224: 318–319.
Lucan SC . Egg on their faces (probably not in their necks); the yolk of the tenuous cholesterol-to-plaque conclusion. Atherosclerosis 2013; 227: 182–183.
Knopp RH, Retzlaff B, Fish B, Walden C, Wallick S, Anderson M et al. Effects of insulin resistance and obesity on lipoproteins and sensitivity to egg feeding. Arterioscler Thromb Vasc Biol 2003; 23: 1437–1443.
Mayurasakorn K, Srisura W, Sitphahul P, Hongto P . High-density lipoprotein cholesterol changes after continuous egg consumption in healthy adults. J Med Assoc Thai 2008; 91: 400–407.
Hegsted D . Serum-cholesterol response to dietary cholesterol: a re-evaluation. Am J Clin Nutr 1986; 44: 299–305.
Kannel WB, Castelli WP, Gordon T, McNamara PM . Serum cholesterol, lipoproteins, and the risk of coronary heart disease: the Framingham Study. Ann Intern Med 1971; 74: 1–12.
Dawber TR, Nickerson RJ, Brand FN, Pool J . Eggs, serum cholesterol, and coronary heart disease. Am J Clin Nutr 1982; 36: 617–625.
Shi Z, Yuan B, Zhang C, Zhou M, Holmboe-Ottesen G . Egg consumption and the risk of diabetes in adults, Jiangsu, China. Nutrition 2011; 27: 194–198.
Stender S, Dyerberg J . Influence of trans fatty acids on health. Ann Nutr Metab 2004; 48: 61–66.
Dyerberg J, Eskesen D, Andersen P, Astrup A, Buemann B, Christensen J et al. Effects of trans-and n-3 unsaturated fatty acids on cardiovascular risk markers in healthy males. An 8 weeks dietary intervention study. Eur J Clin Nutr 2004; 58: 1062–1070.
Bendsen NT, Christensen R, Bartels EM, Astrup A . Consumption of industrial and ruminant trans fatty acids and risk of coronary heart disease: a systematic review and meta-analysis of cohort studies. Eur J Clin Nutr 2011; 65: 773–783.
Astrup A, Raben A, Geiker N . The role of higher protein diets in weight control and obesity-related comorbidities. Int J Obes 2015; 39: 721–726.
Paddon-Jones D, Westman E, Mattes RD, Wolfe RR, Astrup A, Westerterp-Plantenga M . Protein, weight management, and satiety. Am J Clin Nutr 2008; 87: 1558S–1561S.
Nicklas TA, O’Neil CE, Fulgoni VL . Differing statistical approaches affect the relation between egg consumption, adiposity, and cardiovascular risk factors in adults. J Nutr 2015; 145: 170S–176S.
The Australian Heart Foundation. Cholesterol in Food. Australian Heart Foundation: Australia, 2016.
The New Zealand Heart Foundation. Eggs Healthier than Cracked Up to be. New Zealand Heart Foundation: New Zealand, 2016.
Acknowledgements
NRWG and AA initiated the review. The literature search was performed by NRWG, reviewed and discussed by all authors. All authors contributed to the content and NRWG collected the individual contributions and drafted the manuscript; all authors critically reviewed and endorsed the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The work of NRWG has been funded by the Danish Egg Association. The funders had no influence on design, execution, data handling of the investigation, on interpretation or dissemination. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Geiker, N., Larsen, M., Dyerberg, J. et al. Egg consumption, cardiovascular diseases and type 2 diabetes. Eur J Clin Nutr 72, 44–56 (2018). https://doi.org/10.1038/ejcn.2017.153
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.153
- Springer Nature Limited
This article is cited by
-
The effect of whole egg consumption on weight and body composition in adults: a systematic review and meta-analysis of clinical trials
Systematic Reviews (2023)
-
Eggs and Cardiovascular Disease Risk: An Update of Recent Evidence
Current Atherosclerosis Reports (2023)
-
The association of egg consumption with blood pressure levels and glycated hemoglobin in Spanish adults according to body mass index
Scientific Reports (2022)
-
Associations between exploratory dietary patterns and incident type 2 diabetes: a federated meta-analysis of individual participant data from 25 cohort studies
European Journal of Nutrition (2022)
-
Effects of Quality and Quantity of Protein Intake for Type 2 Diabetes Mellitus Prevention and Metabolic Control
Current Nutrition Reports (2020)