Abstract
Background/Objectives:
Vitamin K status has been linked to fat and glucose metabolism by several authors, but whether high vitamin K intake influences body weight or composition has remained unclear. Here we tested the hypothesis that increased vitamin K intake decreases body fat or fat distribution.
Subjects/Methods:
In a randomized placebo-controlled human intervention trial, 214 postmenopausal women, 55–65 years of age, received either 180 mcg/day of vitamin K2 (menaquinone-7, MK-7) or placebo for 3 years. Osteocalcin (OC) carboxylation was used as a marker for vitamin K status, and fat distribution was assessed by dual-energy X-ray absorptiometry total body scan.
Results:
In the total cohort, MK-7 supplementation increased circulating carboxylated OC (cOC) but had no effect on body composition. In those with an above-median response in OC carboxylation (‘good responders’), MK-7 treatment resulted in a significant increase in total and human molecular weight adiponectin and a decrease in abdominal fat mass and in the estimated visceral adipose tissue area compared with the placebo group and the poor responders.
Conclusions:
The fact that changes in body composition measures or markers for fat or glucose metabolism were not associated with changes in uncarboxylated OC (ucOC) does not support the assumption that ucOC stimulates fat metabolism in humans. Instead, high vitamin K2 intake may support reducing body weight, abdominal and visceral fat, notably in subjects showing a strong increase in cOC. A causal relation between the changes in cOC and body fat or distribution cannot be concluded from these data.
Similar content being viewed by others
Introduction
The osteoblast-specific protein osteocalcin (OC) has received much attention in the past owing to its proposed function as a key component in the interplay between bone homeostasis and fat metabolism in humans.1, 2, 3, 4 OC contains three residues of the amino-acid γ-carboxyglutamic acid (Gla) that are formed in a vitamin K-dependent way. Initially, it was suggested that uncarboxylated OC (ucOC) acts as a hormone-stimulating fat metabolism via the adiponectin pathway.1, 2, 3, 4 This hypothesis implies that decreasing ucOC by vitamin K supplementation would decrease fat metabolism and lead to obesity. Arguments supporting this hypothesis were almost exclusively found in mice injected with ucOC, showing a reduction in fat mass and improvement in glucose metabolism.5, 6 In contrast, long-term supplementation of phylloquinone (vitamin K1) and menaquinone-4 (MK-4, a short-chain vitamin K2) reduced total fat accumulation and serum triglycerides in rats.7 Although plasma OC status remained undetermined in this study, one could expect enhanced vitamin K-dependent OC carboxylation, contradicting the suggested beneficial effects of ucOC. In humans, the first outcomes were conflicting, and the role of OC carboxylation is not always clear because conformation-specific testing was not performed.8 During recent years, however, most human studies on the potential relation of vitamin K, vitamin K status and vitamin K-dependent OC conformations with body weight, obesity and type-2 diabetes mellitus suggest a beneficial effect of vitamin K on glucose and fat metabolism.9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24
In conclusion, most cross-sectional studies in humans suggest a link between the bone protein OC and body composition, wherein carboxylated OC (cOC) and not ucOC exhibits hormonal activity. Consistently, in a 4-week intervention study MK-4 supplementation both improved OC carboxylation and increased insulin sensitivity index in healthy young men.25 Furthermore, Shea et al.26 did not find an association between vitamin K-induced reduction of ucOC and changes in fat mass and fat-free mass in a 3-year intervention period in older men and women.
Recently, additional evidence for a link between vitamin K and body mass was found during a 3-year intervention period among postmenopausal women aged between 55 and 65 years.11 This group was selected because bone loss (the primary end point) is known to be high in the first decade after menopause. The present study is an exploratory analysis within the framework of the latter randomized clinical trial,27 in which we tested the hypothesis that 3-year vitamin K2 (in the form of menaquinone-7 (MK-7)) supplementation in postmenopausal women will also affect waist circumference, body composition (fat mass/fat free mass) and visceral fat as assessed by dual-energy X-ray absorptiometry.
Subjects and methods
Study participants
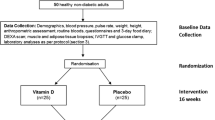
The study was performed in a previously described cohort of 244 apparently healthy women aged between 55 and 65 years, at least 2 years postmenopausal, body mass index <30 kg/m2, not using medication known to affect calcium and bone metabolism and/or vitamin K-containing supplements.27 All participants gave written informed consent for participation in this study. This study was conducted in agreement with the Declaration of Helsinki and approved by the local Medical Ethics Committee. Trial registration code: clinicaltrials.gov NCT00642551.
Study products and design
The study was double-blind, randomized, placebo controlled and had a two-armed parallel design in which participants received either placebo capsules (n=124) or capsules containing 180 μg MK-7 (MenaQ7) (n=120). The proprietary product MenaQ7 utilized in the study was provided by NattoPharma (Høvik, Norway). One capsule was taken daily either with breakfast or dinner during a period of 36 months. No side effects have been reported of long-term use of MK-7 in the study dose. There were no dietary restrictions and participants were asked to continue their regular diet and physical activities throughout the study. Participants exercising more than once weekly were considered to be physical active. From the 244 volunteers who entered the study, 21 discontinued their participation and were not available for the follow-up measurements (drop-out rate: 8.6%). Between 2008 and 2011, participants came to the research site annually for a general checkup to monitor changes in dietary pattern, physical activity, medication and/or general health. After admission and randomization, subjects entered the study between the months May and October, and care was taken that during follow-up they were monitored in the same month in subsequent years.
Waist-to-hip ratio
Waist-to-hip ratio was calculated by taking the ratio between the waist and hip circumference (both in cm), with a precision of 0.5 cm.
Whole-body composition
The distribution of fat and fat-free mass of the whole body and of the different regions was determined at baseline and after 3 years of treatment by performing a whole-body scan using dual-energy X-ray absorptiometry with the APEX software Version 4.0.2 (Hologic Discovery A, Waltham, MA, USA). The fat mass index (FMI) was calculated from the formula FMI=FM/height2 (in kg/m2) and the fat-free mass index (FFMI) from the formula: FFMI=FFM/height2 (in kg/m2). The android region of interest (ROI) is determined as 1/5 of the distance between the horizontal secants of the pelvis and neck. The lower boundary of the ROI is placed against the pelvic horizontal secant. The gynoid ROI is two times the height of the android ROI and its upper boundary is placed below the pelvic horizontal line by 1.5 times the height of the android ROI. To determine the visceral adipose tissue (VAT), the APEX software locates a region of 5 cm across the abdomen. The lower boundary of this region is located 1 cm above the iliac crest. The estimated VAT is calculated by subtracting the amount of subcutaneous fat on both sides of the region (between the skin line and outer abdominal wall) from the total amount of fat in this region. Inadequate or missing measurements of whole-body composition were excluded from subsequent statistical analyses, resulting in a total subject number of n=214.
Laboratory analyses
Blood was taken to prepare plasma and serum, in which the following biomarkers were measured: ucOC and cOC (Takara Shuzo Co., Kyoto, Japan), leptin (DIAsource ImmunoAssays, Ottignies-Louvain-la-Neuve, Belgium), insulin (DRG Instruments, Marburg, Germany), glucose (Abcam, Cambridge, MA, USA), total adiponectin (AdipoGen, Epalinges, Switzerland), human molecular weight (HMW) adiponectin (R&D Systems, Abingdon, UK), interleukin-6 (ultra-sensitive; Invitrogen, Camarillo, CA, USA), high-sensitive C-reactive protein (hsCRP; DRG International, Springfield, NJ, USA), and tumour necrosis factor-α (R&D Systems Europe, Abingdon, UK). Within- and between-assay precisions for ucOC were 4.8% and 7.7%, for cOC 2.3% and 10.6%, for glucose 2.4% and 5.1%, for leptin 9.4% and 15.8%, for insulin 9.1% and 6.8%, for total adiponectin 5.3% and 9.1% and for HMW adiponectin 6.7% and 10.9%, for interleukin-6 6.4% and 7.8%, for hsCRP 7.7% and 8.3% and for tumour necrosis factor-α 5.4% and 8.3%, respectively. We also calculated the HMW/total adiponectin ratio as an additional measure of adiponectin status. Adiponectin and leptin were used as markers for fat metabolism.
The total of markers for fat and glucose metabolism will be designated here as markers for energy metabolism. We tested samples obtained at baseline and at the end of the study (year 3).
Statistics
The calculated sample size of this study (n=120 per group) was based on bone strength in postmenopausal women, as described previously.27 After discontinuation of 21 subjects and inadequate measurements of 11 subjects, data sets of n=214 were available for analysis (placebo: n=107, MK-7: n=107). Normal distribution was tested by the one-sample Kolmogorov–Smirnov test. Log-transformation was performed if variables were not normally distributed (hsCRP, leptin, insulin, glucose, HMW adiponectin). One-way analysis of variance (for continuous variables) and Fisher’s Exact test (for categorical variables) were used to test between-group differences at baseline. Associations at baseline between variables of interest were assessed by Pearson correlation analysis. The response of cOC and ucOC to placebo and MK-7 was measured by calculating the differences between baseline and 3 years. To define good and poor responders in cOC and ucOC in the MK-7 group, the 50th percentile was taken. One-way analysis of variance was used to analyze the differences between the good and poor responders to MK-7 compared with placebo (3 groups). Mean values are given with s.d. or with s.e. (Figures). P<0.05 (two-sided significance level) was considered to be statistically significant. SPSS version 19.0 for Windows was used to perform statistical analyses (SPSS Inc., Chicago, IL, USA).
Results
Baseline data
Baseline measurements are given in Table 1. No significant differences were found between the placebo and the MK-7 group. Poor vitamin K status as deduced from low cOC plasma concentrations was associated with a higher fat mass at different body sites, including the android region, and with waist circumference but not with FFMI. No associations were found between baseline ucOC and markers for adiposity. On the other hand, cOC showed inverse associations with hsCRP, leptin and insulin but not with total adiponectin and HMW adiponectin (Table 2).
Effect of MK-7 supplementation on body composition
After 3 years of treatment, the ratio between fat mass in the android region and that in the gynoid region had increased 1.4% (s.e. 0.6%) in the placebo group, whereas it had not changed in the MK-7 group (−0.5% (s.e. 0.6%), P=0.021). MK-7 treatment also induced a significant increase of circulating cOC as compared with placebo (21.5% (s.e. 1.9%) and 2.6% (s.e. 1.5%), respectively; P<0.0001). UcOC had decreased significantly in the MK-7 group by 50.1% (s.e. 2.0%), whereas it had hardly changed in the placebo group (+4.3% (s.e. 4.8%); P<0.0001).
In a subsequent analysis, we have focused on the good responders in the MK-7 group, who were defined as those who had increased their circulating cOC concentration with a value above the 50th percentile (+0.92 ng/ml) of the 3-year change of this variable (Table 3). These subjects were compared with the poor responders (below the 50th percentile) in the same group and with the placebo group. Similarly, we have also subdivided the MK-7-treated group into good and poor responders based on the decrease of ucOC (−1.67 ng/ml). No significant differences were found between the baseline values of the variables of body composition in the good and poor responders in cOC and ucOC compared with the placebo (Table 3).
Outcomes based on response in cOC
The change in cOC in the poor responders was 0.38 ng/ml (s.e. 0.07 ng/ml) or 7.7% (s.e. 1.3%) and in the good responders it was 1.66 ng/ml (s.e. 0.087 ng/ml) or 34.9% (s.e. 2.3%) P<0.0001. Compared with the poor responders, the good responders showed a significant increase in total and in HMW adiponectin (0.71 μg/ml (s.e. 0.29 μg/ml), P=0.044 and 1.01 μg/ml (s.e. 0.29 μg/ml), P=0.002) after 3 years of MK-7 treatment. No differences between both groups were found for the other markers for fat or glucose metabolism. With respect to the body fat distribution, significant decreases of the variables of the abdominal region (waist circumference, fat mass trunk, android fat mass, estimated VAT area), as well as the android/gynoid fat mass ratio were observed in the good responders group compared with the placebo as well as to the poor responders (Figure 1).
Proportional change of body composition variables in the placebo group and in the poor and good responders (as deduced from serum cOC increase). One-way analysis of variance was performed between placebo (black bars, n=107), poor (gray bars, n=53) and good (white bars, n=54) responders to MK-7 treatment (increase of serum cOC <0.92 ng/ml and ⩾0.92 ng/ml, respectively). Bars represent mean proportional change with corresponding error bars (s.e.). *P<0.05 relate to comparison between poor and good responders with placebo. †P<0.05 and ††P<0.005 relate to comparison between poor and good responders to MK-7 treatment. WHR, waist-to-hip ratio; Ratio A/G. ratio of FM android and gynoid region; Est VAT area, estimated visceral adipose tissue area.
Outcomes based on response in ucOC
The change in ucOC in the poor responders was −0.83 ng/ml (s.e. 0.08 ng/ml) or −37.7% (s.e. 2.8%) and in the good responders it was −3.04 ng/ml (s.e. 0.14 ng/ml) or −62.7% (s.e. 1.6%) P<0.0001. No differences between good and poor responders were found except for fat mass of the trunk, which showed a small but non-significant decrease in the group of the good responders (data not shown).
Discussion
In this paper, we report that poor vitamin K status at baseline (as deduced from low serum cOC concentrations) is associated with a higher waist circumference and a higher fat mass in the android region in healthy women between 55 and 65 years of age. It is now widely accepted that obesity is associated with a chronic state of inflammation and that a number of inflammatory factors are secreted by adipose tissue. Consistently, we have found that poor vitamin K status (low cOC) is associated with higher levels of the pro-inflammatory marker hsCRP. However, we could not confirm that vitamin K supplementation leads to a decrease in inflammation markers. This is probably due to the fact that the study group was selected to be healthy, so inflammation markers were low at baseline already and did not significantly decline further during the 3-year treatment period. Additionally, we found inverse associations between cOC and insulin, and leptin, which is suggestive for an endocrine function of cOC (but not of ucOC) in metabolic pathways leading to adiposity. As compared with baseline values, MK-7 supplementation increased OC carboxylation but did not lead to any changes in body composition in the total study group. Detailed analyses revealed, however, that good responders to MK-7 treatment (as deduced from the increase of serum cOC) showed a significant increase in HMW adiponectin and a reduction of body fat in the abdominal area (waist circumference, android fat mass and estimated VAT area) compared with poor responders.
Several authors have reported that OC acts as a hormone-regulating adiposity and energy metabolism in mice,1, 2, 3, 4, 5, 6 whereas in wild-type rats the opposite was found.7 Most results found in human studies do not support this role for ucOC,7, 8, 9, 10, 11, 13, 19 but some papers have shown conflicting evidence.20 In humans, about 30% of the circulating OC occurs in its uncarboxylated form, and this can be readily decreased to values below the detection limit by using vitamin K supplements. In two unrelated placebo-controlled human intervention trials in which 1 mg/day of vitamin K1 (ref. 28) and 45 mg/day of MK-4 (ref. 29) were given for 3 years to postmenopausal women, we had data on body weight, body mass index and waist circumference, but in both trials we observed a tendency toward lower rather than higher indices for fat mass in the vitamin K-treated groups.11
In the present paper, we found at baseline that low serum cOC was associated with a higher fat mass at different sites. The inverse association between cOC and leptin and insulin is suggestive for a direct role of cOC in glucose homeostasis. These data are consistent with those reported by Rasekhi et al.,30 who showed that phylloquinone supplementation improves glycemic status independent of the effects of adiponectin levels in premenopausal women with prediabetes. The fact that also a weak inverse association was found between cOC and hsCRP may result from a direct anti-inflammatory effect of vitamin K. It may also be the consequence of a decreased fat mass, as chronic low-grade inflammation is a common condition in obese patients. Consequently, CRP being a biomarker indicating chronic low-grade inflammation is often increased in subjects with higher fat mass.31
Our 3-year follow-up data show that increasing cOC at the expense of ucOC by vitamin K supplements was paralleled by a decreased ratio between the android/gynoid fat mass ratio and a decreased estimated visceral fat area. In a further analysis, we have subdivided the MK-7-treated subjects in a group with a strong increase of OC carboxylation (above the median) and a group in which the response was relatively poor (below the median). As compared with the poor responders, the good responders showed a significant increase in total and HMW adiponectin and a more favorable fat mass and fat distribution, that is: significant decreases of the variables of the abdominal region (waist circumference, android fat mass, estimated VAT area), as well as the waist-to-hip circumference ratio and android/gynoid fat mass ratio. Although our data demonstrate a favorable effect of MK-7 on body fat mass and distribution, they do not prove that this is effectuated via cOC or ucOC. Alternatively, the increase of OC carboxylation and the changes in body fat composition may be epiphenomena that occur independently.
The current study must be interpreted within the context of its strengths and potential limitations. Strong points are the good compliance (95%) of participants and the long duration of the study (3 years). Our study also has a number of limitations. First, it was powered for bone strength and not for changes in body weight and fat mass. Second, no associations were found between the vitamin K-induced change in cOC and a number of biomarkers for fat and glucose metabolism, so that the mechanism underlying the observed effect of vitamin K on fat distribution remains unexplained. Finally, the data were obtained in healthy postmenopausal women aged between 55 and 65 years and may not be extrapolated to the general population (for example, men or children).
In conclusion, in this trial we demonstrate the beneficial effects of vitamin K supplementation on fat mass and body composition. Our data suggest that cOC rather than ucOC is a key component in the interplay between bone and energy metabolism, but the precise mechanism underlying this effect remains to be determined in future studies.
References
Lee NK, Karsenty G . Reciprocal regulation of bone and energy metabolism. Trends Endocrinol Metab 2008; 19: 161–166.
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C et al. Endocrine regulation of energy metabolism by the skeleton. Cell 2007; 130: 456–469.
Shiba S, Ikeda K, Azuma K, Hasegawa T, Amizuka N, Horie-Inoue K et al. γ-Glutamyl carboxylase in osteoblasts regulates glucose metabolism in mice. Biochem Biophys Res Commun 2014; 453: 350–355.
Ferron M, Lacombe J, Germain A, Oury F, Karsenty G . GGCX and VKORC1 inhibit osteocalcin endocrine functions. J Cell Biol 2015; 208: 761–776.
Ferron M, Hinoi E, Karsenty G, Ducy P . Osteocalcin differentially regulates beta cell and adipocyte gene expression and affects the development of metabolic diseases in wild-type mice. Proc Natl Acad Sci USA 2008; 105: 5266–5270.
Ferron M, McKee MD, Levine RL, Ducy P, Karsenty G . Intermittent injections of osteocalcin improve glucose metabolism and prevent type 2 diabetes in mice. Bone 2012; 50: 568–575.
Sogabe N, Maruyama R, Baba O, Hosoi T, Goseki-Sone M . Effects of long-term vitamin K(1) (phylloquinone) or vitamin K(2) (menaquinone-4) supplementation on body composition and serum parameters in rats. Bone 2011; 48: 1036–1042.
Booth SL, Centi A, Smith SR, Gundberg CM . The role of osteocalcin in human glucose metabolism: marker or mediator? Nat Rev Endocrinol 2013; 9: 43–55.
Juanola-Falgarona M, Salas-Salvado J, Estruch R, Portillo MP, Casas R, Miranda J et al. Association between dietary phylloquinone intake and peripheral metabolic risk markers related to insulin resistance and diabetes in elderly subjects at high cardiovascular risk. Cardiovasc Diabetol 2013; 12: 7.
Shea MK, Booth SL, Gundberg CM, Peterson JW, Waddell C, Dawson-Hughes B et al. Adulthood obesity is positively associated with adipose tissue concentrations of vitamin K and inversely associated with circulating indicators of vitamin K status in men and women. J Nutr 2010; 140: 1029–1034.
Knapen MHJ, Schurgers LJ, Shearer MJ, Newman P, Theuwissen E, Vermeer C . Association of vitamin K status with adiponectin and body composition in healthy subjects: uncarboxylated osteocalcin is not associated with fat mass and body weight. Br J Nutr 2012; 108: 1017–1024.
Tamura T, Yoneda M, Yamane K, Nakanishi S, Nakashima R, Okubo M et al. Serum leptin and adiponectin are positively associated with bone mineral density at the distal radius in patients with type 2 diabetes mellitus. Metabolism 2007; 56: 623–628.
Kanazawa I, Yamaguchi T, Yamauchi M, Yamamoto M, Kurioka S, Yano S et al. Serum undercarboxylated osteocalcin was inversely associated with plasma glucose level and fat mass in type 2 diabetes mellitus. Osteoporos Int 2011; 22: 187–194.
Pittas AG, Harris SS, Eliades M, Stark P, Dawson-Hughes B . Association between serum osteocalcin and markers of metabolic phenotype. J Clin Endocrinol Metab 2009; 94: 827–832.
Fernandez-Real JM, Izquierdo M, Ortega F, Gorostiaga E, Gómez-Ambrosi J, Moreno-Navarrete JM et al. The relationship of serum osteocalcin concentration to insulin secretion, sensitivity, and disposal with hypocaloric diet and resistance training. J Clin Endocrinol Metab 2009; 94: 237–245.
Kindblom JM, Ohlsson C, Ljunggren O, Karlsson MK, Tivesten A, Smith U et al. Plasma osteocalcin is inversely related to fat mass and plasma glucose in elderly Swedish men. J Bone Miner Res 2009; 24: 785–791.
Im JA, Yu BP, Jeon JY, Kim SH . Relationship between osteocalcin and glucose metabolism in postmenopausal women. Clin Chim Acta 2008; 396: 66–69.
Yeap BB, Chubb SA, Flicker L, McCaul KA, Ebeling PR, Beilby JP et al. Reduced serum total osteocalcin is associated with metabolic syndrome in older men via waist circumference, hyperglycemia, and triglyceride levels. Eur J Endocrinol 2010; 163: 265–272.
Centi AJ, Booth SL, Gundberg CM, Saltzman E, Nicklas B, Shea MK . Osteocalcin carboxylation is not associated with body weight or percent fat changes during weight loss in post-menopausal women. Endocrine 2015; 50: 627–632.
Hwang YC, Jeong IK, Ahn KJ, Chung HY . The uncarboxylated form of osteocalcin is associated with improved glucose tolerance and enhanced beta-cell function in middle-aged male subjects. Diabetes Metab Res Rev 2009; 25: 768–772.
Ibarrola-Jurado N, Salas-Salvado J, Martinez-Gonzalez MA, Bulló M . Dietary phylloquinone intake and risk of type 2 diabetes in elderly subjects at high risk of cardiovascular disease. Am J Clin Nutr 2012; 96: 1113–1118.
Yoshida M, Booth SL, Meigs JB, Saltzman E, Jacques PF . Phylloquinone intake, insulin sensitivity, and glycemic status in men and women. Am J Clin Nutr 2008; 88: 210–215.
Kumar R, Binkley N, Vella A . Effect of phylloquinone supplementation on glucose homeostasis in humans. Am J Clin Nutr 2010; 92: 1528–1532.
Yoshida M, Jacques PF, Meigs JB, Saltzman E, Shea MK, Gundberg CM et al. Effect of vitamin K supplementation on insulin resistance in older men and women. Diabetes Care 2008; 31: 2092–2096.
Choi HJ, Yu J, Choi H, An JH, Kim SW, Park KS et al. Vitamin K2 supplementation improves insulin sensitivity via osteocalcin metabolism: a placebo-controlled trial. Diabetes Care 2011; 34: e147.
Shea MK, Dawson-Hughes B, Gundberg CM, Booth SL . Reducing undercarboxylated osteocalcin with vitamin K supplementation does not promote lean tissue loss or fat gain over 3 years in older women and men: a randomized controlled trial. J Bone Miner Res 2017; 32: 243–249.
Knapen MHJ, Drummen NE, Smit E, Vermeer C, Theuwissen E . Three-year low-dose menaquinone-7 supplementation helps decrease bone loss in healthy postmenopausal women. Osteoporos Int 2013; 24: 2499–2507.
Braam LAJLM, Knapen MHJ, Geusens P, Brouns F, Hamulyák K, Gerichhausen MJ et al. Vitamin K1 supplementation retards bone loss in postmenopausal women between 50 and 60 years of age. Calcif Tissue Int 2003; 73: 21–26.
Knapen MHJ, Schurgers LJ, Vermeer C . Vitamin K2 supplementation improves bone geometry and bone strength indices in postmenopausal women. Osteoporos Int 2007; 18: 963–972.
Rasekhi H, Karandish M, Jalali MT, Mohammad-shahi M, Zarei M, Saki A et al. The effect of vitamin K1 supplementation on sensitivity and insulin resistance via osteocalcin in prediabetic women: a double-blind randomized controlled clinical trial. Eur J Clin Nutr 2015; 69: 891–895.
Hotamisligil GS . Inflammation and metabolic disorders. Nature 2006; 444: 860–867.
Acknowledgements
This work was supported by NattoPharma (Høvik, Norway). The sponsor had no role in the design, analysis or writing of this article.
Author contributions
CV contributed to the design of the study and was involved in the interpretation of the findings and preparation of the manuscript; MHJK was involved in the conduct of the study and performed the statistical analyses. MHJK and KMJ contributed to the interpretation of the findings and to the preparation of the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Knapen, M., Jardon, K. & Vermeer, C. Vitamin K-induced effects on body fat and weight: results from a 3-year vitamin K2 intervention study. Eur J Clin Nutr 72, 136–141 (2018). https://doi.org/10.1038/ejcn.2017.146
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.146
- Springer Nature Limited
This article is cited by
-
Co-supplementation of Vitamin K2 and Selenium Synergistically Improves Metabolic Status and Reduces Cardiovascular Risk Markers in Dyslipidemic Rabbits
Biological Trace Element Research (2023)
-
Effect of vitamin K2 administration on depression status in patients with polycystic ovary syndrome: a randomized clinical trial
BMC Women's Health (2022)
-
The effect of menaquinone-7 supplementation on dp-ucMGP, PIVKAII, inflammatory markers, and body composition in type 2 diabetes patients: a randomized clinical trial
Nutrition & Diabetes (2022)
-
Vitamin K2 (menaquinone-7) increases plasma adiponectin but does not affect insulin sensitivity in postmenopausal women: a randomized controlled trial
European Journal of Clinical Nutrition (2021)
-
A critical review of the effects of vitamin K on glucose and lipid homeostasis: its potential role in the prevention and management of type 2 diabetes
Hormones (2021)