Abstract
Background/Objectives:
Diet during pregnancy and lactation may have a role in the development of allergic diseases. There are few human studies on the topic, especially focusing on food allergies. We sought to study the associations between maternal diet during pregnancy and lactation and cow’s milk allergy (CMA) in offspring.
Subjects/Methods:
A population-based birth cohort with human leukocyte antigen-conferred susceptibility to type 1 diabetes was recruited in Finland between 1997 and 2004 (n=6288). Maternal diet during pregnancy and lactation was assessed by a validated, 181-item semi-quantitative food frequency questionnaire. Register-based information on diagnosed CMA was obtained from the Social Insurance Institution and completed with parental reports. The associations between maternal food consumption and CMA were assessed using logistic regression, comparing the highest and the lowest quarters to the middle half of consumption.
Results:
Consumption of milk products in the highest quarter during pregnancy was associated with a lower risk of CMA in offspring (odds ratio (OR) 0.56, 95% confidence interval (CI) 0.37–0.86; P<0.01). When stratified by maternal allergic rhinitis and asthma, there was evidence of an inverse association between high use of milk products and CMA in offspring of non-allergic mothers (OR 0.30, 95% CI 0.13–0.69, P<0.001). Cord blood IgA correlated positively with the consumption of milk products during pregnancy, indicating exposure to CMA and activation of antigen-specific immunity in the infant during pregnancy.
Conclusions:
High maternal consumption of milk products during pregnancy may protect children from developing CMA, especially in offspring of non-allergic mothers.
Similar content being viewed by others
Introduction
Very little is known about dietary determinants of food allergies, but there is some evidence that early nutrition has a role in the development of other allergic diseases and asthma.1 The association between maternal diet during pregnancy and food allergy in offspring has been addressed in one epidemiological Japanese study, finding no evidence of association.2 The occurrence of asthma or allergic diseases, including food allergies, seems to be unaffected by food allergen avoidance during pregnancy or lactation.3 However, diet may contain protective factors against allergic diseases. Evidence that high intake of fish during pregnancy may protect the child against the development of asthma and allergic diseases (reviewed, for example, by Sala-Vila et al.4) is as inconsistent as that afforded by high intake of nuts,5 or fruits (for example, citrus fruits and kiwi) and vegetables.6, 7, 8 Results of cohort studies addressing the possible association between maternal milk consumption and allergic diseases in offspring are equivocal.2, 9, 10, 11, 12 The association between maternal diet during lactation and long-term allergic outcomes is even less studied. The composition of breast milk, such as IgA, has been associated with the development of allergic diseases.13, 14 However, studies assessing associations between maternal diet during lactation and allergic outcomes in the child are lacking. Antigens transferred into breast milk may have immunologic effects in the infant.15
There is a clear paucity of data on associations between maternal diet during pregnancy and lactation and food allergy in offspring. Cow’s milk allergy (CMA) is the most common and the most rigorously diagnosed food allergy in infancy, affecting 2–6% of children.16, 17, 18, 19 The aim of the present study was to investigate the associations between maternal diet during pregnancy and lactation and subsequent development of CMA in children up to 2 years of age.
Subjects and methods
Study population
The Finnish Type 1 Diabetes Prediction and Prevention Study is a multidisciplinary prospective population-based cohort study.20 After parental informed consent, all newborn infants from the catchment areas of three university hospitals in Finland (Turku, Oulu and Tampere) were screened for human leukocyte antigen-conferred susceptibility to type 1 diabetes from cord blood samples. Families with infants carrying human leukocyte antigen genotypes conferring high and moderate risk (15% of those screened) were invited to participate in the study, excluding children with severe congenital abnormalities or diseases, or whose parents were of non-Caucasian origin or did not understand Finnish, Swedish or English. The Diabetes Prediction and Prevention Nutrition study is performed in the catchment areas of Oulu and Tampere University Hospitals. The present study comprised 6288 children born between October 1997 and September 2004 in these University Hospitals and whose personal identification codes were disclosed to the study. Pregnancy dietary data were available from mothers of 4921 children from 4861 pregnancies. Lactation dietary data of the mothers were gathered from August 1998 and received for 2940 children from 2915 mothers.
Dietary assessment
Maternal diet during pregnancy (month 8) and lactation (month 3) was assessed by a validated 181-item semi-quantitative food frequency questionnaire (FFQ).21 The FFQ, specifically designed to reflect Finnish food consumption, assessed consumption frequency (not at all, number of times per day, week or month) using common serving sizes. Mothers received the FFQ concerning diet during pregnancy after delivery by mail, and it was returned at a visit to the study centre and checked by a trained study nurse when the child was 3 months old. The questionnaire concerning diet during lactation was given at the 3-month visit and returned at the 6-month visit to the study centre. All data were double-entered. If there were 10 or more missing frequencies, or the questionnaire was not filled in according to the instructions, the FFQ was rejected (n=53, 1.1% and n=25, 0.9% of FFQs concerning diet during pregnancy and lactation, respectively). Recording of the FFQ was checked by trained nutritionists. The detailed content of the FFQ and data processing with an in-house software of the National Institute for Health and Welfare are described elsewhere.21, 22 For the total milk product consumption, the use of milk, yoghurt and other sour milk products, cheese, ice cream and cream as well as milk products added to cooking was summed up; milk from chocolate, butter and margarines was not taken into account. Introduction of solids in the infant diet was recorded prospectively by the parents.
Laboratory methods
Cord blood IgA to beta-casein (Beta-Casein from Bovine Milk, Sigma C-6905, Sigma-Aldrich, St Louis, MO, USA) was measured by EIA as described earlier13 in a subgroup of 329 non-allergic mothers. The antigen-coating concentration was 100 μg/ml (beta-casein in phosphate-buffered saline; 100 μl per well), and the cord blood samples were studied at the dilution 1:20.
End points
Special diets of children were queried with open questions at the age of 6 months and 1 and 2 years and with a structured, validated questionnaire at the age of 3 years.23, 24 The structured questionnaire included questions on who instigated the special diet and how old the child was then. In addition, the Finnish Social Insurance Institution maintains a complete register of children, who have a physician diagnosis of CMA and therefore entitlement to reimbursement for the costs of special infant formulas. Pediatricians use agreed criteria for the diagnosis throughout the country (a response to an elimination diet and an open challenge; rarely, a response to an elimination diet with a positive skin prick test or specific IgE; in select cases, double-blind placebo-controlled challenge is performed). Those children who do not need a special infant formula are not included in the register; thus, to include those who are breastfed till or diagnosed with CMA after the age of 1 year, we combined these two sources of information into one end point, cumulated until 2 years of age.
For the cohort of 6288 children born between October 1997 and September 2004, 394 children were diagnosed with CMA according to information from the Social Insurance Institution by record linkage. In addition, 135 parents had reported CMA in their child; thus, there were 529 cases altogether. Information on maternal diet during pregnancy was available for 4921 children; of these, there were in all 448 cases of CMA (322 based on Social Insurance Institution register and 126 cases based on parental reports). This total was used as the end point for the analysis of the diet during pregnancy. For the analysis of the diet during lactation, the beginning of CMA was taken into account: children whose CMA had begun before completing the FFQ for the lactation diet were excluded from the analysis; thus, we ended up with 106 cases based on the registers of the Social Insurance Institution and 62 parentally reported cases, and 168 cases altogether.
Background factors
From a questionnaire at recruitment we received information on vocational education, age of both parents and place of residence. The national Medical Birth Registry provided information on pregnancy and delivery complications, gestational age, birth weight and length, earlier deliveries and maternal smoking during pregnancy. Parents reported in a questionnaire at child’s age 5 years parental asthma, allergic rhinitis and atopic eczema, as well as pet keeping and farm animal contacts during the child’s first year of life.25
Ethics
The local Ethical Committees approved the study. All families have given their written informed consent.
Statistics
Simple associations between background factors and cumulative incidence of CMA were tested using logistic regression. The associations between maternal diet and the cumulative incidence of CMA in offspring were estimated using logistic regression, with possible dependence among outcomes in siblings accommodated in the accompanying estimates of precision through the so-called empirical or sandwich variance estimator. Consumption of each food item was divided into quarters, and highest and lowest quarters were compared with the combined middle half. In order to answer the specific question on the association between maternal diet during pregnancy and lactation, adjustments for possible confounding factors were carried out in two phases: first, adjustments were made for study area, gender and birth weight of the child, maternal age and education, maternal smoking during pregnancy, type of delivery, number of older siblings and length of breastfeeding; and second with the addition of maternal allergic rhinitis or asthma, urbanity of living environment, duration of gestation, season of birth and visits to a stable and pet keeping during the first year of life. In one last model, maternal diet during lactation was also adjusted for maternal diet during pregnancy. Confounding was handled sequentially, because data for the second adjustment from 5-year follow-up were available only for those who were still participating in the study at that age. Two-sided tests were used, and P-values below 0.05 were considered statistically significant. Multiplicity issues were taken into account in cautious interpretation of the results. Associations between maternal milk consumption during pregnancy and immunoglobulin levels in cord blood were tested using Spearman's correlation test. Analyses were conducted with the SAS statistical package (SAS Institute Inc., Cary, NC, USA, version 9.1).
Results
Diagnosis of CMA was more common among boys than girls (Table 1). The risk of CMA was higher in children born to parents with asthma and allergic rhinitis, as well as to mothers with a high level of education. On the other hand, maternal smoking during pregnancy and pet keeping during the first year of life were associated with a lower risk of CMA in offspring.
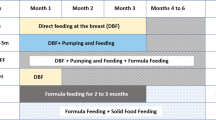
Mothers consumed an average of 810 g cow’s milk products daily during pregnancy (Table 2), which is equivalent to the national recommendation for expectant mothers, advising to drink 800 ml of milk per day. Consumption of cow’s milk products in the highest quarter during pregnancy was associated with a lower risk of CMA in offspring (Table 3). Considering simultaneously cow’s milk consumption during both pregnancy and lactation, only high intake during pregnancy was associated with a lower risk of CMA in offspring (odds ratio (OR) 0.30, confidence interval (CI) 0.13–0.68, P=0.01). Adjusting for the age at introduction of cow’s milk products in infancy did not change the result either (OR 0.59, CI 0.38–0.92; P=0.01). The association was not attributed to any specific product or fat content but to the total use (data not shown). When stratified by maternal allergic rhinitis or asthma, the association between high consumption of cow’s milk products during pregnancy and lower risk of CMA persisted only in children of non-allergic mothers (OR 0.30, 95% CI 0.13–0.69, P<0.001; Figure 1). Among offspring of allergic mothers, maternal milk consumption during pregnancy was neither a risk nor a protective factor. The outcome of the analyses on the association between maternal milk consumption and CMA in offspring remained the same when only the register-based end point was considered (data not shown).
The risk of cow’s milk allergy associated with maternal milk consumption during pregnancy (lowest and highest quarters compared with the middle half), stratified according to maternal allergic rhinitis or asthma (adjusted for energy intake, study centre, gender, birth weight of the child, maternal age and education, maternal smoking during pregnancy, type of delivery, number of older siblings, length of overall breastfeeding, maternal allergic rhinitis or asthma, duration of gestation, season of birth, urbanity of living environment and visits to a stable and pet keeping during the first year of life). *P<0.001.
Cord blood IgA levels to beta-casein correlated with the maternal consumption of the milk products; R= 0.216, P=0.003 in children who did not develop CMA and R= 0.206, P=0.05 in children who developed CMA (Spearman's test).
Low consumption of fish during pregnancy tended to associate with a higher risk of CMA (OR 1.27, 95% CI 0.99–1.61; P=0.046). Stratified according to maternal allergic rhinitis or asthma, this tendency was observable in the offspring of allergic mothers only (OR 1.47, 95% CI 0.96–2.27, P=0.04). Maternal citrus and kiwi fruit consumption during lactation was associated with a smaller risk of CMA in offspring, users vs non-users (OR 0.54; 95% CI 0.34–0.86 P=0.02).
Discussion
To our knowledge, this is the first cohort study to show associations between maternal diet during pregnancy and CMA in offspring. High consumption of cow’s milk products during pregnancy associated with a lower risk for the development of CMA, suggesting antigen-specific induction of tolerance during pregnancy. Maternal lactation diet was less so associated with CMA in offspring.
Major strengths of our study are its prospective nature and the large number of mothers and children studied with reproducible and valid methods. Our end point is defined by register-based information on diagnosis, as well as by validated questionnaires for CMA, and the birth cohort is unselected regarding atopic predisposition. We were able to take into account several possible confounders, most importantly maternal allergic diseases, which could influence maternal food choices. A further strength is the use of a comprehensive, validated FFQ.21 The correlations between the FFQ and food records for the use of milk products were 0.86 and for the use of fish 0.44. Cross-classification in fifths revealed non-negligible correlations for all food items and food groups, despite the tendency of FFQs to overestimate consumption.
One limitation is that adjustment for parental asthma and allergic rhinitis could only be carried out for children who were still participating in the study at the age of 5 years. Another limitation may be that the subjects carry human leukocyte antigen-conferred susceptibility to type 1 diabetes.20 Despite the comparable frequency of diagnoses of CMA to another Finnish study,18 this could restrict the generalisability of our results. A further limitation is the uncertainty of the starting age of symptoms of CMA in the infant. Although we excluded those whose CMA diagnosis was confirmed before completing the FFQ during lactation, reverse causation cannot entirely be ruled out. In addition, maternal vitamin supplementation, a potential confounding factor, was not included in the analysis.
Previous studies on maternal diet during pregnancy and allergic diseases in offspring have focused on the development of a variety of allergic disorders, for example, eczema, asthma and sensitisation measured by IgE; aetiological factors of food allergy may differ. Comparing previous results is hampered not only by differences in end points but also by differences in methods for assessing both maternal diet and allergic diseases. We chose CMA as the end point to ensure the homogeneity of the outcome, as diagnostic practices are more varied for other food allergies. Elimination diets during pregnancy and lactation have been studied in allergy prevention, and pooled analysis of randomised, controlled trials does not support prophylactic elimination diets during pregnancy or lactation.3
Evidence from observational studies for an association between maternal milk consumption and CMA in offspring is scarce. One Japanese report found an inverse association between milk product consumption during pregnancy and atopic dermatitis in offspring but no association with food allergy.2 In another survey, Miyake et al.10 observed an inverse association between maternal milk consumption during pregnancy and wheezing but not in relation to eczema at the age of 16–24 months. However, the intake of milk products in that study was considerably lower than that in the present study. Furthermore, a Danish study observed an inverse association between maternal consumption of high-fat milk products during pregnancy and early wheezing and a direct association with maternal low-fat yoghurt intake and asthma later in childhood.12 Other recent reports have observed no evidence of association between cow’s milk consumption during pregnancy and wheeze or asthma,5 atopic eczema11 and specific IgE responses against food or inhalant allergens in offspring at the age of 5 years.8 None of the aforementioned reports have specifically studied CMA as an end point. However, a small study among lactating mothers in high-risk families did not find any associations between maternal milk protein intake and CMA in offspring.26 This result is in line with our findings of no association between maternal cow’s milk consumption and CMA in offspring of allergic mothers. Our findings are supported by those reported by Katz et al.,27 who observed that early introduction of cow’s milk was associated with a lower risk of CMA, suggesting the importance of early introduction in tolerance induction.
Fatty acids represent one potential immunomodulatory component in milk. High maternal consumption of cream,9 full-fat milk10 and high-fat milk products12 during pregnancy was inversely associated with allergic outcomes in three previous cohort studies. In our study, the overall abundant maternal use of cow’s milk products was associated with a lower risk for CMA in children, and no particular fat content of milk stood out. Thus, the inverse association seen in the present study is likely attributable to other components in the milk.
We hypothesise that maternal milk consumption during pregnancy has a tolerogenic effect in utero. This idea is supported by the observation that the inverse association is not seen in children of allergic mothers, whose tolerogenic mechanisms may be deficient. Normally, antigen-specific IgG is transported from the mother to the fetus via placenta,28 and the antigens bound to IgG, such as cow’s milk antigens, are transferred thus from the mother to the fetus. Mouse models have shown that tolerance is transferred from the mother to the offspring29 and that sensitisation in offspring may be prevented by maternal immunisation.30 The fetus is exposed to dietary antigens in utero due to placental transfer,31 but the effect of maternal dietary intake on the antigen transfer to the fetus is not clear.32 A recent report found higher peanut-specific IgE levels in children with higher maternal consumption of peanut during pregnancy; however, they also reported increased levels of specific IgG and IgG4, indicating transfer of tolerance.33
The results of the present study suggest that abundant consumption of cow’s milk products during pregnancy may lower the risk of CMA in offspring likely based on the antigen-specific tolerance, as supported by our immunological studies. Because IgA is synthesised by the fetus cord blood IgA is suitable for assessing the development of the humoral immune status of the newborn infant, whereas IgG reflects maternal antibodies due to placental transfer. In the group of infants of non-allergic mothers, we found that cord blood IgA, although the levels were low, correlated positively with the consumption of CM products during pregnancy. This suggests antigen exposure and activation of humoral immune response to maternal dietary antigens in infants already during pregnancy.
The confirmatory findings on associations between sociodemographic factors and the risk of CMA also deserve some attention. The inverse association between maternal smoking during pregnancy and risk of CMA in children is likely explained by smoking being a surrogate for some other environmental exposure (Table 1). In addition, parents with higher education may be more prone to seek for a diagnosis for their children.34
This is the first study linking maternal diet during pregnancy and the risk of CMA in offspring, and the issue should be studied in other populations. Our results strengthen the notion that maternal diet during pregnancy has an impact on future disease development in offspring. Maternal diet can be modified, once risk and protective factors are identified. The results support the current recommendation of no maternal elimination diets in order to decrease the risk of food allergy. Mothers should rather consume than avoid milk during pregnancy in order to decrease the risk of CMA in their child.
References
Nurmatov U, Devereux G, Sheikh A . Nutrients and foods for the primary prevention of asthma and allergy: systematic review and meta-analysis. J Allergy Clin Immunol 2011; 127: 724–733.
Ushiyama Y, Matsumoto K, Shinohara M, Wakiguchi H, Sakai K, Komatsu T et al. Nutrition during pregnancy may be associated with allergic diseases in infants. J Nutr Sci Vitaminol (Tokyo) 2002; 48: 345–351.
Kramer MS, Kakuma R Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Cochrane Database Syst Rev 2006; (3): CD000133.
Sala-Vila A, Miles EA, Calder PC . Fatty acid composition abnormalities in atopic disease: evidence explored and role in the disease process examined. Clin Exp Allergy 2008; 38: 1432–1450.
Willers SM, Wijga AH, Brunekreef B, Kerkhof M, Gerritsen J, Hoekstra MO et al. Maternal food consumption during pregnancy and the longitudinal development of childhood asthma. Am J Respir Crit Care Med 2008; 178: 124–131.
Miyake Y, Sasaki S, Tanaka K, Hirota Y . Consumption of vegetables, fruit, and antioxidants during pregnancy and wheeze and eczema in infants. Allergy 2010; 65: 758–765.
Chatzi L, Torrent M, Romieu I, Garcia-Esteban R, Ferrer C, Vioque J et al. Mediterranean diet in pregnancy is protective for wheeze and atopy in childhood. Thorax 2008; 63: 507–513.
Nwaru BI, Ahonen S, Kaila M, Erkkola M, Haapala AM, Kronberg-Kippila C et al. Maternal diet during pregnancy and allergic sensitization in the offspring by 5 yrs of age: a prospective cohort study. Pediatr Allergy Immunol 2009; 21: 29–37.
Sausenthaler S, Koletzko S, Schaaf B, Lehmann I, Borte M, Herbarth O et al. Maternal diet during pregnancy in relation to eczema and allergic sensitization in the offspring at 2 y of age. Am J Clin Nutr 2007; 85: 530–537.
Miyake Y, Sasaki S, Tanaka K, Hirota Y . Dairy food, calcium, and vitamin D intake in pregnancy and wheeze and eczema in infants. Eur Respir J 2009; 35: 1228–1234.
Saito K, Yokoyama T, Miyake Y, Sasaki S, Tanaka K, Ohya Y et al. Maternal meat and fat consumption during pregnancy and suspected atopic eczema in Japanese infants aged 3-4 months: The Osaka Maternal and Child Health Study. Pediatr Allergy Immunol 2009; 21: 38–46.
Maslova E, Halldorsson TI, Strom M, Olsen SF . Low-fat yoghurt intake in pregnancy associated with increased child asthma and allergic rhinitis risk: a prospective cohort study. J Nutr Sci 2012; 1: e5.
Orivuori L, Loss G, Roduit C, Dalphin JC, Depner M, Genuneit J et al. Soluble immunoglobulin A in breast milk is inversely associated with atopic dermatitis at early age: the PASTURE cohort study. Clin Exp Allergy 2014; 44: 102–112.
Hoppu U, Rinne M, Salo-Väänänen P, Lampi AM, Piironen V, Isolauri E . Vitamin C in breast milk may reduce the risk of atopy in the infant. Eur J Clin Nutr 2005; 59: 123–128.
Palmer DJ, Makrides M . Diet of lactating women and allergic reactions in their infants. Curr Opin Clin Nutr Metab Care 2006; 9: 284–288.
Kajosaari M . Food allergy in Finnish children aged 1 to 6 years. Acta Paediatr Scand 1982; 71: 815–819.
Saarinen KM, Juntunen-Backman K, Järvenpää AL, Kuitunen P, Lope L, Renlund M et al. Supplementary feeding in maternity hospitals and the risk of cow's milk allergy: a prospective study of 6209 infants. J Allergy Clin Immunol 1999; 104: 457–461.
Pyrhönen K, Näyhä S, Kaila M, Hiltunen L, Läärä E . Occurrence of parent-reported food hypersensitivities and food allergies among children aged 1–4 yr. Pediatr Allergy Immunol 2009; 20: 328–338.
Pediatric Society of Finland. Food allergy among children. Duodecim 2009; 125: 1992–1993.
Kupila A, Muona P, Simell T, Arvilommi P, Savolainen H, Hamalainen AM et al. Feasibility of genetic and immunological prediction of type I diabetes in a population-based birth cohort. Diabetologia 2001; 44: 290–297.
Erkkola M, Karppinen M, Javanainen J, Räsänen L, Knip M, Virtanen SM . Validity and reproducibility of a food frequency questionnaire for pregnant Finnish women. Am J Epidemiol 2001; 154: 466–476.
Prasad M, Lumia M, Erkkola M, Tapanainen H, Kronberg-Kippila C, Tuokkola J et al. Diet composition of pregnant Finnish women: changes over time and across seasons. Public Health Nutr 2010; 13: 939–946.
Tuokkola J, Kaila M, Pietinen P, Simell O, Knip M, Virtanen SM . Agreement between parental reports and patient records in food allergies among infants and young children in Finland. J Eval Clin Pract 2008; 14: 984–989.
Tuokkola J, Luukkainen P, Kaila M, Tapanainen H, Klaukka T, Veijola R et al. Validation of a questionnaire on cow's milk allergy: parental reports and physicians diagnosis. Acta Paediatr 2010; 99: 1273–1275.
Nwaru BI, Lumia M, Kaila M, Luukkainen P, Tapanainen H, Erkkola M et al. Validation of the Finnish ISAAC questionnaire on asthma against anti-asthmatic medication reimbursement database in 5-year-old children. Clin Respir J 2011; 5: 211–218.
Hoppu U, Kalliomäki M, Isolauri E . Cow's milk allergy—a matter of fat. Allergy 2002; 57: 61–62.
Katz Y, Rajuan N, Goldberg MR, Eisenberg E, Heyman E, Cohen A et al. Early exposure to cow's milk protein is protective against IgE-mediated cow's milk protein allergy. J Allergy Clin Immunol 2010; 126: 77–82.
Loibichler C, Pichler J, Gerstmayr M, Bohle B, Kisst H, Urbanek R et al. Materno-fetal passage of nutritive and inhalant allergens across placentas of term and pre-term deliveries perfused in vitro. Clin Exp Allergy 2002; 32: 1546–1551.
Polte T, Hennig C, Hansen G . Allergy prevention starts before conception: maternofetal transfer of tolerance protects against the development of asthma. J Allergy Clin Immunol 2008; 122: 1022–1030.
Fusaro AE, Brito CA, Victor JR, Rigato PO, Goldoni AL, Duarte AJ et al. Maternal-fetal interaction: preconception immunization in mice prevents neonatal sensitization induced by allergen exposure during pregnancy and breastfeeding. Immunology 2007; 122: 107–115.
Edelbauer M, Loibichler C, Nentwich I, Gerstmayr M, Urbanek R, Szepfalusi Z . Maternally delivered nutritive allergens in cord blood and in placental tissue of term and preterm neonates. Clin Exp Allergy 2004; 34: 189–193.
Vance GH, Lewis SA, Grimshaw KE, Wood PJ, Briggs RA, Thornton CA et al. Exposure of the fetus and infant to hens' egg ovalbumin via the placenta and breast milk in relation to maternal intake of dietary egg. Clin Exp Allergy 2005; 35: 1318–1326.
Sicherer SH, Wood RA, Stablein D, Lindblad R, Burks AW, Liu AH et al. Maternal consumption of peanut during pregnancy is associated with peanut sensitization in atopic infants. J Allergy Clin Immunol 2010; 126: 1191–1197.
Metsala J, Lundqvist A, Kaila M, Gissler M, Klaukka T, Virtanen SM . Maternal and perinatal characteristics and the risk of cow's milk allergy in infants up to 2 years of age: a case-control study nested in the Finnish population. Am J Epidemiol 2010; 171: 1310–1316.
Acknowledgements
We are extremely grateful to all the families who took part in this study. We also acknowledge the excellent collaboration of the Diabetes Prediction and Prevention research nurses, doctors, nutritionists and laboratory staff over the years. We especially thank Mirka Puputti for her work in the laboratory. The study was supported by the Academy of Finland (grants 63672, 79685, 79686, 80846, 201988, 210632, 129492 and 126813), the Finnish Paediatric Research Foundation, the Juho Vainio Foundation, the Yrjö Jahnsson Foundation, the Competitive Research Funding of the Tampere University Hospital, Medical Research Funds of Turku and Oulu University Hospitals, the Juvenile Diabetes Research Foundation (grants 197032, 4-1998-274, 4-1999-731 and 4-2001-435), the Novo Nordisk Foundation and EU Biomed 2 (BMH4-CT98-3314), Doctoral Programs for Public Health, Foundation for Allergy Research, Research Foundation of Orion Corporation, Tampere Tuberculosis Foundation and the Jalmari and Rauha Ahokas Foundation.
Author contributions
SMV, JT, MKa and OV were responsible for the current study concept and design; JI, MKn and OS designed the DIPP study; SMV designed the nutrition study within DIPP; JT, SMV and OV conducted research; LV provided registry data from the Social Insurance Institute; OV was responsible for laboratory analyses of β-casein-specific IgA antibodies; MGK designed and HT carried out the statistical analysis; RV was responsible for the clinical work in Oulu; JT wrote the first version of the manuscript; PL, MKa, SMV and OV participated in the writing process; SMV had primary responsibility for the final content; all the authors contributed to the critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tuokkola, J., Luukkainen, P., Tapanainen, H. et al. Maternal diet during pregnancy and lactation and cow’s milk allergy in offspring. Eur J Clin Nutr 70, 554–559 (2016). https://doi.org/10.1038/ejcn.2015.223
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.223
- Springer Nature Limited
This article is cited by
-
Maternal dietary patterns during pregnancy and the risk of infantile eczema during the first year of life: a cohort study in northeast China
BMC Public Health (2023)
-
Allergieprävention in Schwangerschaft und Stillzeit
gynäkologie + geburtshilfe (2018)