Abstract
Background/Objectives:
Despite considerable research on the association between physical activity (PA) and body composition, there remains limited information on the directionality of the relationship. The present study examined the prospective associations among objectively measured PA, energy intake (EI) and body composition.
Subjects/Methods:
A convenience sample of 430 adults (49% male) between 21 and 35 years of age was followed over 1 year with repeated measurements taken every 3 months. BMI (kg/m2) and percent body fat (%BF) were calculated based on anthropometric measurements and dual energy X-ray absorptiometry. A multi-sensor device was worn over a period of 10 days to estimate total daily energy expenditure and time spent in different intensities. EI was calculated based on change in body composition and total daily energy expenditure.
Results:
A total of 379 participants provided valid data. On average, participants experienced a significant weight gain of 1.2±4.3 kg during the 12-month observation period, which was associated with an increase in %BF (0.8±3.2 %). Average time spent in moderate-to-vigorous PA (MVPA) decreased significantly, whereas EI remained constant. Optimal linear mixed models, adjusting for age and sex, showed an inverse effect of MVPA on BMI and %BF, whereas EI only directly affected BMI (P<0.001). There was also a significant inverse effect of BMI and %BF on MVPA (P<0.001).
Conclusions:
Results of this study indicate an inverse reciprocal association between MVPA and measures of adiposity. Thus, primary preventive actions are warranted to avoid excess weight gain, which may result in a vicious cycle of weight gain and low PA.
Similar content being viewed by others
Introduction
Excess body weight is the result of a long-term imbalance between energy intake (EI) and energy expenditure. Even though a genetic predisposition and physiologic constraints need to be considered,1, 2 low levels of physical activity (PA) and high EI have been predominantly considered as major contributors to the current obesity epidemic.3 The ongoing debate regarding the role of EI and energy expenditure/PA, however, mirrors the limited evidence on the prospective association between PA, diet and body fatness.
The inverse association between PA and body weight or adiposity has been predominantly shown in cross-sectional studies, but evidence on the prospective effect of PA on body weight and body composition remains inconclusive.4 Some longitudinal studies indicate that weight gain may be a precursor of lower PA, rather than a consequence of low PA levels.5, 6, 7, 8 Other studies, however, have shown a reduction in body weight in adults who increase their activity levels, whereas weight gain was more pronounced in adults who decreased their PA.9, 10, 11, 12 These contradictory results may be explained by the limited accuracy of self-reported PA13 and a regression dilution bias as a result of differences in measurement error.14 A lack of adjustment for potential confounders including baseline measures of PA and body weight could affect findings as well.10 Further, two time points (baseline and post-measurements) may not be sufficient to show a clear longitudinal pattern of the variables of interest. Of additional concern is the omission of EI in previous studies, despite its impact on energy balance.15 The omission of EI may have been due to difficulties in the accurate assessment of dietary intake in natural settings, as it also relies on self-report.16, 17 There is, however, also the potential of a bi-directional relationship between PA and body weight or adiposity, which could explain these seemingly contradicting results.14 Such a reciprocal association between PA and body composition, however, has been largely ignored in the analytical approach used in previous studies.
Additional research on the reciprocal effects of PA and body composition on each other could provide valuable information regarding our understanding of the regulation of energy balance. The present study uses objective measures of PA to examine the longitudinal interaction of time spent sedentary, in light PA and moderate-to-vigorous PA (MVPA) with measures of adiposity, while considering EI and demographic characteristics as potential confounders. To account for potential differences in the regulation of energy balance, normal weight and overweight/obese adults were examined separately.
Subjects and methods
The present analysis uses data from an ongoing observational study on primary and secondary determinants of weight change. Details of the methodology of the Energy Balance Study, which is conducted in an urban area in South Carolina, have been published previously.18 In brief, 430 (49.3% male) adults between 21 and 35 years of age were recruited via flyers, e-mail listservs and social media as this population is at particular risk for decreasing metabolic rate and weight gain.19, 20 Sample size calculations were based on average weight change in this population. Assuming an effect size of 1±7 kg change in body weight over 12 months, a sample size of 385 would be required to obtain statistical power of 0.8 with alpha set at 0.05. Exclusion criteria were designed to select a group of individuals with no major acute or chronic conditions who had not made any large changes in health behaviors in the previous months. Exclusion criteria also included a BMI above 35 kg/m2 or below 19 kg/m2, pregnancy in the previous 12 months and planned births. Women who planned on changing their use of contraceptive medications during the study were excluded as well due to concern over potential changes in body water and appetite. The study protocol was approved by the University of South Carolina Institutional Review Board and is in accordance with the declaration of Helsinki. Written informed consent was obtained from participants prior to data collection.
Measurements
All measurements were obtained by trained and certified research staff and were repeated every 3 months over a period of 1 year. In addition to objective assessments of body composition and PA, participants completed an extensive medical history and demographic information form.
Anthropometrics and body fatness
Height (cm) and weight (kg) were measured according to standard laboratory procedures with participants in surgical scrubs. Height was measured to the nearest 0.1 cm using a wall-mounted stadiometer (Model S100, Ayrton Corp., Prior Lake, MN, USA) and weight was measured to the nearest 0.1 kg using an electronic scale (Healthometer model 500KL, McCook, IL, USA). BMI (kg/m2) was calculated based on the average of three height and weight measurements at each time point. In addition, total fat and fat-free mass were measured via dual energy X-ray absorptiometry (GE Healthcare Lunar model 8743, Waukesha, WI, USA) and percent body fat (%BF) was calculated.
Physical activity
The SenseWear Mini Armband (Body Media Inc., Pittsburgh, PA, USA) was used to objectively assess energy expenditure and PA. Combining tri-axial accelerometry with measurements of skin temperature, heat flux, galvanic skin response and near body temperature, the armband has been shown to provide accurate estimates of energy expenditure in free-living adults.21 Participants were asked to wear the armband continuously for 10 days during the respective measurement periods. Compliance was defined as at least 7 days (including 2 weekend days) with more than 18 h/day of verifiable wear time. When the armband was not on their body, participants recorded their activities in a log. Activities during non-wear time were matched to metabolic equivalents (METs) based on the 2011 Compendium of Physical Activities22 and non-classified activities were entered as 1.5 METs. These METs were then multiplied by the participant’s resting metabolic rate to compute energy expenditure for the time when the armband was not worn, resulting in 24-h of energy expenditure and time spent at different intensities at every time point. Resting metabolic rate was measured in the morning after a 12-h fast and 24-h abstention from exercise via indirect calorimetry (True One 2400, Parvo Medics, Sandy, UT, USA).
Using SenseWear’s proprietary software (Version 7.0 professional), total daily energy expenditure and time spent at different intensities were estimated. Specifically, sedentary time, excluding sleep (sedentary <1.5 METs), time spent in light PA (1.5 METs⩽ light PA <3 METs) and time spent in MVPA (MVPA ⩾3.0 METs) was determined at the respective measurement period.
Energy intake
Owing to the lack of accuracy of self-reported dietary intake,16 total daily energy intake (TDEI) was calculated based on total daily energy expenditure and change in fat mass and fat-free mass for each 3-month period;23, 24 an increase in mass is associated with a positive energy balance (that is, EI is higher than total daily energy expenditure), whereas a decrease in body mass is associated with a negative energy balance (that is, EI is lower than total daily energy expenditure). Assuming an energy density of 1020 and 9500 kcal/kg for fat-free mass and fat mass, respectively, TDEI was calculated for each 3 months interval as follows:

TDEI, total daily energy intake; TDEE, average total daily energy expenditure at respective time points; ΔFFM, change in fat-free mass (kg) over time; ΔFM, change in fat mass (kg) over time; Δt, days between two measurement times.
Statistical analysis
Descriptive statistics were calculated for baseline and follow-up measurements. On confirmation of a normal distribution, differences between participants classified as normal weight (baseline BMI <25 kg/m2) and overweight/obese (baseline BMI ⩾25 kg/m2) were analyzed by analysis of covariance, adjusting for age, sex, ethnicity and education. Linear mixed models, which account for both within- and between-subject variation in the data were used to examine the prospective association between PA, TDEI and measures of adiposity. To account for the four available measures of TDEI (difference between 3-month intervals), measures for body fatness and PA were adjusted accordingly by calculating average values for each 3-month period. For each variable of interest, an initial model with the main independent predictors adjusting for demographic covariates including, sex, race, education, employment, income, marital status and age was developed. Subsequently, a stepwise variable selection procedure along with the Akaike information criterion was used to determine the optimal model. Multicollinearity was checked for the predictors by calculating the variance inflation where variance inflation>5 was identified as collinearity. The analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC, USA) using a significance level of P<0.05 with Bonferroni correction for multiple comparisons.
Results
A total of 379 participants (49.1% male) provided valid data for at least three measurement time points and where subsequently included in the analysis. Average armband wear time for participants included in the analysis was 23.3±0.6 h/day. There was no difference in baseline characteristics between participants included in the analysis and those excluded owing to missing follow-up data. Average age at baseline was 27.8±3.8 years. Almost two-thirds (65.4%) of the participants were Caucasian with the majority having a College degree (85.5%). At baseline, 51.2% were classified as overweight/obese. There was no significant difference for sex, ethnicity and education between normal weight and overweight/obese participants. Normal weight participants, however, were younger (27.2±3.6 vs 28.3±3.9, P=0.005), and spent more time in MVPA and less time in sedentary or light PA than their overweight/obese peers (P<0.001). TDEI was higher in overweight/obese (P<0.001). These results remained after controlling for age, sex, ethnicity and education (Table 1).
Participants experienced an average estimated weight gain, based on linear mixed models, of 1.2±4.3 kg (P<0.001) associated with an increase in %BF (0.8±3.2 %, P<0.001). There was no difference in weight gain between normal weight and overweight/obese participants. Individual weight change ranged from a weight loss of 14.0 kg/year to a weight gain of 13.0 kg/year and change in %BF was between −10.1 and 7.5%. Average time spent in MVPA decreased significantly (−6.5±58.7 min/day, P=0.002), whereas there was no significant change in TDEI (2.3±503.1 kcal/day, P=0.931). Sedentary time and time spent in light PA did not change significantly (change of 5.2±86.7 min/day and 1.8±55.9 min/day, respectively, P⩾0.243). As shown for measures of body fatness, progression of measures of PA and TDEI did not differ between normal weight and overweight/obese participants.
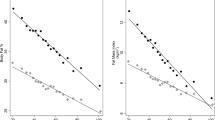
For the total sample the optimal linear mixed models, adjusting for sex and age, revealed a significant effect of time spent in MVPA and TDEI on BMI (Table 2). The inverse effect of MVPA was more pronounced than the direct effect of TDEI on BMI. Adjusting for multiple comparisons there was no significant effect of TDEI on %BF, whereas the significant effect of MVPA remained. Time spent in sedentary or light PA did not affect either measure of adiposity. Both, BMI and %BF, also affected time spent in MVPA (Est.BMI=−4.413, s.e.=0.432; Est.%BF=−2.694, s.e.= 0.230; P<0.001), whereas there was no significant effect of BMI or %BF on sedentary time. These results were essentially unchanged when participants who lost weight (weight loss >5%), maintained body weight (weight change ⩽5%) or gained weight (weight gain >5%) over the 12-month observation period were analyzed separately.
The effect of TDEI and time spent in MVPA on measures of adiposity remained when analyzing normal weight and overweight/obese participants separately. MVPA affected BMI and %BF, whereas the effect of TDEI was only significant for BMI (Table 3). Sedentary time affected BMI in normal weight participants, but there was no effect of sedentary time on measures of adiposity in overweight/obese. There was, however, a significant direct effect of BMI on sedentary time (Est.=2.612, s.e.=0.982, P=0.008) in overweight/obese. As shown for the total sample MVPA was significantly affected by BMI and %BF in both BMI categories (Table 4).
Discussion
Although there is considerable evidence on the cross-sectional association between body composition and PA, information on the longitudinal relationship between these correlates of energy balance remains limited. Previous studies have shown an inverse effect of PA on subsequent weight gain25, 26, 27 but body weight has also been shown to affect subsequent PA.5, 6, 7 These studies, however, relied on self-reported PA, which was assessed during only two time points and focused mainly on a one-directional association between PA and body composition. Using objective measures of PA and adiposity along with calculated EI over several time points, the present study indicates a reciprocal association between time spent in MVPA and adiposity in young adults. There was no effect of sedentary time on %BF and the longitudinal association between sedentary time and BMI differed between normal weight and overweight/obese adults. In normal-weight participants sedentary time affected BMI, whereas in overweight/obese participants there was a direct effect of BMI on sedentary time. Of additional interest is the fact that TDEI was directly associated with BMI, whereas the effect on %BF was limited.
The positive effect of MVPA on body composition has been shown in various intervention studies.28, 29 The effect of a change in body composition on subsequent PA, however, needs to be considered as well. Increased body weight may hinder participation in MVPA owing to musculoskeletal problems and exhaustion,5 highlighting the need for dietary adjustments in order to induce weight loss and facilitate long-term weight maintenance.30, 31 Nevertheless, it has been argued that energy balance cannot be maintained under conditions of low PA and that low EI may jeopardize the intake of essential nutrients.32 The present study further shows a limited effect of EI on body composition. Energy restriction is associated with a loss in fat mass and fat-free mass, which minimizes the change in %BF. Exercise-induced weight loss, on the other hand, preserves fat-free mass, resulting in a reduction in %BF.33 This is of particular importance as relative fat mass, rather than BMI, has been associated with various metabolic abnormalities and health outcomes.34, 35 In addition, energy restriction is associated with compensatory changes in biological systems, such as a decrease in resting metabolic rate and fat oxidation36, 37 along with a reduction in PA38 that facilitate weight re-gain. With exercise-induced weight loss resting metabolic rate is maintained or even increased, which facilitates weight-loss maintenance.39, 40
Given the reciprocal association between MVPA and body fatness, dietary intake, nevertheless, has an important role in long-term weight management. To avoid excess weight gain, which inversely affects PA, a healthy, well-balanced diet, rather than caloric restriction, should be endorsed. A recent meta-analysis, for example, showed benefits of a Mediterranean diet on body weight, independent of EI.31 Particularly, high consumption of fruits and vegetables, whole grains, pasta, rice and fish, with low consumption of red meat has been associated with lower body weight.31, 41 Such a dietary pattern is further associated with lower intakes of processed foods that include high amounts of sugar and sodium, which are commonly associated with excess body weight.42 The reciprocal association between MVPA and measures of body fatness further emphasizes the fact that weight management should start early and focus on maintaining a healthy body weight rather than focusing solely on weight loss in overweight/obese patients. Primary prevention strategies, addressing the importance of an overall healthy lifestyle including diet and PA, are needed to prevent a vicious cycle of increased body fatness and low levels of MVPA.
The prospective association between sedentary time and BMI was less pronounced and reached significance only in normal-weight participants, whereas the association between %BF and sedentary time was non-significant. Even though sedentary time has been associated with type 2 diabetes, metabolic syndrome as well as cardiovascular-disease and all-cause mortality43, 44 results of the present study indicate that higher PA intensities seem to be the major determinant for body fatness. This is further supported by the lack of association between time spent in light PA and BMI or %BF. Consistent with findings of the present study, a large cohort study did not show an association between sedentary behavior and risk of obesity either.45 It has, therefore, been argued that sedentary time has no effect on body composition beyond that attributed to lack of PA per se.9 Higher body fat, however, has been associated with greater sedentary time46 and the present study showed a direct effect of BMI on sedentary time in overweight/obese participants. To enhance the understanding of the prospective association between sedentary time and body composition, additional information about the accumulation of sedentary time may be necessary, as Chau et al.47 argue that leisure-time sitting has a stronger association with obesity compared with occupational sitting. Further, the type of sedentary behavior may be of importance as particularly TV time has been associated with various measures of body fatness, which in part was explained by a higher caloric intake while watching TV.48
The assessment of sedentary time in the present study does not allow for the differentiation between different types of sedentary pursuits. Nevertheless, the objective assessment of both PA and sedentary time should be considered a strength of the study. Some other limitations, however, need to be addressed when interpreting the findings of this study. The study population consisted predominantly of white participants with a college degree. An average physical activity level of 1.8±0.2 indicates a relatively active population and the prevalence of overweight/obesity was lower than that of the general US population.49 It is possible that EI has a stronger effect on adiposity in a less-active sample. Thus, additional research in other sub-populations or a more representative sample is needed. In addition, energy intake was calculated based on change in fat mass and fat-free mass, rather than being directly assessed. Calculated energy intake also does not provide any information on dietary intake, which has been shown to be associated with body weight, independent of total energy intake.31 Given the limited accuracy of self-reported energy intake, the inclusion of calculated energy intake, nevertheless, should be considered a strength of the present study as it is an important component in the concept of energy balance. Further, the assessment of key variables at multiple time points allowed for a more elaborate evaluation of the complex interaction of PA, TDEI and adiposity. Taken together this study adds valuable information on the prospective association of key variables contributing to energy balance.
Conclusions
In conclusion, results of this observational study suggest a reciprocal association between time spent in MVPA and adiposity in young adults. Even though MVPA has been emphasized as effective means in the regulation of body weight,50 it may be hindered by increased body weight. It is, therefore, necessary to take preventive measures that avoid the accumulation of excess weight and body fat at early stages and assure sufficient amounts of PA. More research, however, is warranted to increase the understanding of the prospective association between the complex interaction of diet, PA and body composition as a better understanding of the long-term regulation of energy balance is crucial for the development of effective initiatives addressing the current obesity epidemic and long-term weight management.
References
Jéquier E, Tappy L . Regulation of body weight in humans. Physiol Rev 1999; 79: 451–480.
Bell CG, Walley AJ, Froguel P . The genetics of human obesity. Nat Rev Genet 2005; 6: 221–234.
Pereira-Lancha LO, Campos-Ferraz PL, Lancha AH . Obesity: considerations about etiology, metabolism, and the use of experimental models. Diabetes Metab Syndr Obes 2012; 5: 75–87.
Summerbell CD, Douthwaite W, Whittaker V, Ells LJ, Hillier F, Smith S et al. The association between diet and physical activity and subsequent excess weight gain and obesity assessed at 5 years of age or older: a systematic review of the epidemiological evidence. Int J Obes (Lond) 2009; 33 (Suppl 3), S1–S92.
Golubic R, Ekelund U, Wijndaele K, Luben R, Khaw KT, Wareham NJ et al. Rate of weight gain predicts change in physical activity levels: a longitudinal analysis of the EPIC-Norfolk cohort. Int J Obes (Lond) 2013; 37: 404–409.
Petersen L, Schnohr P, Sørensen TI . Longitudinal study of the long-term relation between physical activity and obesity in adults. Int J Obes Relat Metab Disord 2004; 28: 105–112.
Bak H, Petersen L, Sørensen TI . Physical activity in relation to development and maintenance of obesity in men with and without juvenile onset obesity. Int J Obes Relat Metab Disord 2004; 28: 99–104.
May AM, Bueno-de-Mesquita HB, Boshuizen H, Spijkerman AM, Peeters PH, Verschuren WM . Effect of change in physical activity on body fatness over a 10-y period in the Doetinchem Cohort Study. Am J Clin Nutr 2010; 92: 491–499.
Hamer M, Brunner EJ, Bell J, Batty GD, Shipley M, Akbaraly T et al. Physical activity patterns over 10 years in relation to body mass index and waist circumference: the Whitehall II cohort study. Obesity (Silver Spring) 2013; 21: E755–E761.
Mekary RA, Feskanich D, Malspeis S, Hu FB, Willett WC, Field AE . Physical activity patterns and prevention of weight gain in premenopausal women. Int J Obes (Lond) 2009; 33: 1039–1047.
Schmitz KH, Jacobs DR, Leon AS, Schreiner PJ, Sternfeld B . Physical activity and body weight: associations over ten years in the CARDIA study. Coronary Artery Risk Development in Young Adults. Int J Obes Relat Metab Disord 2000; 24: 1475–1487.
Littman AJ, Kristal AR, White E . Effects of physical activity intensity, frequency, and activity type on 10-y weight change in middle-aged men and women. Int J Obes (Lond) 2005; 29: 524–533.
Wareham NJ, Rennie KL . The assessment of physical activity in individuals and populations: why try to be more precise about how physical activity is assessed? Int J Obes Relat Metab Disord 1998; 22 (Suppl 2), S30–S38.
Hutcheon JA, Chiolero A, Hanley JA . Random measurement error and regression dilution bias. BMJ 2010; 340: c2289.
Basterra-Gortari FJ, Bes-Rastrollo M, Pardo-Fernández M, Forga L, Martinez JA, Martínez-González MA . Changes in weight and physical activity over two years in Spanish alumni. Med Sci Sports Exerc 2009; 41: 516–522.
Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van't Veer P . Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr 2009; 101 (Suppl 2), S73–S85.
Livingstone MB, Black AE . Markers of the validity of reported energy intake. J Nutr 2003; 133 (Suppl 3), S895–S920.
Hand G, Shook R, Paluch A, Baruth M, Crowley P, Jaggers J et al. The Energy Balance Study: The design and baseline results for a longitudinal study of energy balance. Res Q Exerc Sport 2013; 84: 275–286.
Ogden C, Carroll M, Kit B, Flegal K Prevalence of Obesity in the United States, 2009-2010 NCHS data brief. no 82, National Center for Health Statistics: Hyattsville, MD, USA, 2012.
Sheehan TJ, DuBrava S, DeChello LM, Fang Z . Rates of weight change for black and white Americans over a twenty year period. Int J Obes Relat Metab Disord 2003; 27: 498–504.
Johannsen DL, Calabro MA, Stewart J, Franke W, Rood JC, Welk GJ . Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc 2010; 42: 2134–2140.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C et al. 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 2011; 43: 1575–1581.
Thomas DM, Schoeller DA, Redman LA, Martin CK, Levine JA, Heymsfield SB . A computational model to determine energy intake during weight loss. Am J Clin Nutr 2010; 92: 1326–1331.
Thomas DM, Bouchard C, Church T, Slentz C, Kraus WE, Redman LM et al. Why do individuals not lose more weight from an exercise intervention at a defined dose? An energy balance analysis. Obes Rev 2012; 13: 835–847.
Wagner A, Simon C, Ducimetière P, Montaye M, Bongard V, Yarnell J et al. Leisure-time physical activity and regular walking or cycling to work are associated with adiposity and 5 y weight gain in middle-aged men: the PRIME Study. Int J Obes Relat Metab Disord 2001; 25: 940–948.
Waller K, Kaprio J, Kujala UM . Associations between long-term physical activity, waist circumference and weight gain: a 30-year longitudinal twin study. Int J Obes (Lond) 2008; 32: 353–361.
Sternfeld B, Wang H, Quesenberry CP, Abrams B, Everson-Rose SA, Greendale GA et al. Physical activity and changes in weight and waist circumference in midlife women: findings from the Study of Women's Health Across the Nation. Am J Epidemiol 2004; 160: 912–922.
Ross R, Janssen I . Physical activity, total and regional obesity: dose-response considerations. Med Sci Sports Exerc 2001; 33 (Suppl 6), S521–S529.
Lee S, Kuk JL, Davidson LE, Hudson R, Kilpatrick K, Graham TE et al. Exercise without weight loss is an effective strategy for obesity reduction in obese individuals with and without Type 2 diabetes. J Appl Physiol (1985) 2005; 99: 1220–1225.
Brown T, Avenell A, Edmunds LD, Moore H, Whittaker V, Avery L et al. Systematic review of long-term lifestyle interventions to prevent weight gain and morbidity in adults. Obes Rev 2009; 10: 627–638.
Esposito K, Kastorini CM, Panagiotakos DB, Giugliano D . Mediterranean diet and weight loss: meta-analysis of randomized controlled trials. Metab Syndr Relat Disord 2011; 9: 1–12.
Caballero B . The global epidemic of obesity: an overview. Epidemiol Rev 2007; 29: 1–5.
Washburn RA, Szabo AN, Lambourne K, Willis EA, Ptomey LT, Honas JJ et al. Does the method of weight loss effect long-term changes in weight, body composition or chronic disease risk factors in overweight or obese adults? A systematic review. PLoS One 2014; 9: e109849.
Oliveros E, Somers VK, Sochor O, Goel K, Lopez-Jimenez F . The concept of normal weight obesity. Prog Cardiovasc Dis 2014; 56: 426–433.
Bastien M, Poirier P, Lemieux I, Després JP . Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis 2014; 56: 369–381.
Schwartz A, Kuk JL, Lamothe G, Doucet E . Greater than predicted decrease in resting energy expenditure and weight loss: results from a systematic review. Obesity (Silver Spring) 2012; 20: 2307–2310.
Filozof CM, Murúa C, Sanchez MP, Brailovsky C, Perman M, Gonzalez CD et al. Low plasma leptin concentration and low rates of fat oxidation in weight-stable post-obese subjects. Obes Res 2000; 8: 205–210.
Bonomi AG, Soenen S, Goris AH, Westerterp KR . Weight-loss induced changes in physical activity and activity energy expenditure in overweight and obese subjects before and after energy restriction. PLoS One 2013; 8: e59641.
Potteiger JA, Kirk EP, Jacobsen DJ, Donnelly JE . Changes in resting metabolic rate and substrate oxidation after 16 months of exercise training in overweight adults. Int J Sport Nutr Exerc Metab 2008; 18: 79–95.
Wilmore JH, Stanforth PR, Hudspeth LA, Gagnon J, Daw EW, Leon AS et al. Alterations in resting metabolic rate as a consequence of 20 wk of endurance training: the HERITAGE Family Study. Am J Clin Nutr 1998; 68: 66–71.
Shay CM, Van Horn L, Stamler J, Dyer AR, Brown IJ, Chan Q et al. Food and nutrient intakes and their associations with lower BMI in middle-aged US adults: the International Study of Macro-/Micronutrients and Blood Pressure (INTERMAP). Am J Clin Nutr 2012; 96: 483–491.
Drenowatz C, Shook RP, Hand GA, Hébert JR, Blair SN . The independent association between diet quality and body composition. Sci Rep 2014; 4: 4928.
Proper KI, Singh AS, van Mechelen W, Chinapaw MJ . Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med 2011; 40: 174–182.
Duvivier BM, Schaper NC, Bremers MA, van Crombrugge G, Menheere PP, Kars M et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS One 2013; 8: e55542.
Pulsford RM, Stamatakis E, Britton AR, Brunner EJ, Hillsdon MM . Sitting behavior and obesity: evidence from the Whitehall II study. Am J Prev Med 2013; 44: 132–138.
Ekelund U, Brage S, Besson H, Sharp S, Wareham NJ . Time spent being sedentary and weight gain in healthy adults: reverse or bidirectional causality? Am J Clin Nutr 2008; 88: 612–617.
Chau JY, van der Ploeg HP, Merom D, Chey T, Bauman AE . Cross-sectional associations between occupational and leisure-time sitting, physical activity and obesity in working adults. Prev Med 2012; 54: 195–200.
Cleland VJ, Schmidt MD, Dwyer T, Venn AJ . Television viewing and abdominal obesity in young adults: is the association mediated by food and beverage consumption during viewing time or reduced leisure-time physical activity? Am J Clin Nutr 2008; 87: 1148–1155.
Flegal KM, Carroll MD, Kit BK, Ogden CL . Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012; 307: 491–497.
Saris WH, Blair SN, van Baak MA, Eaton SB, Davies PS, Di Pietro L et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev 2003; 4: 101–114.
Acknowledgements
We wish to thank the study participants and the Energy Balance Study team. Funding for the study was provided by an unrestricted grant from The Coca Cola Company. The sponsor had no role in the study design, collection, analysis and interpretation of data, or preparation and submission of this manuscript.
Author contributions
GAH and SNB conceived the energy balance study. RPS managed data collection. CD and BC analyzed the data with PTK contributing to the interpretation. CD drafted the initial manuscript with important intellectual contributions from all co-authors. All authors read and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The study has been funded by an unrestricted grant from The Coca Cola Company. The sponsor had no role in the study design, collection, analysis and interpretation of data, or preparation and submission of this manuscript. Gregory A Hand received financial support from NIH, CDC, HRSA, the American Heart Association, Body Media and The Coca Cola Company. Peter T Katzmarzyk received financial support from NIH and The Coca Cola Company. Steven N Blair has received research funding from the following organizations/companies: National Institutes of Health, Department of Defense, Body Media, and The Coca Cola Company. He is on Scientific/Medical Advisory Boards for the following organizations/companies: Technogym, Santech, Clarity, International Council on Active Aging, Cancer Fit Steps for Life. The remaining authors have no conflict to declare.
Rights and permissions
About this article
Cite this article
Drenowatz, C., Cai, B., Hand, G. et al. Prospective association between body composition, physical activity and energy intake in young adults. Eur J Clin Nutr 70, 482–487 (2016). https://doi.org/10.1038/ejcn.2015.133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.133
- Springer Nature Limited
This article is cited by
-
Sedentary Behavior and Body Weight and Composition in Adults: A Systematic Review and Meta-analysis of Prospective Studies
Sports Medicine (2018)
-
The association of change in physical activity and body weight in the regulation of total energy expenditure
European Journal of Clinical Nutrition (2017)