Abstract
Background/Objectives:
There have been few studies on the association of fruit and vegetable (FV) intake with cardiovascular disease (CVD) risk in Asian populations where both dietary habits and disease structure are different from western countries. No study in Asia has found its significant association with stroke. We examined associations of FV intake with mortality risk from total CVD, stroke and coronary heart diseases (CHDs) in a representative Japanese sample.
Methods:
A total of 9112 participants aged from 24-year follow-up data in the NIPPON DATA80, of which baseline data were obtained in the National Nutrition Survey Japan in 1980, were studied. Dietary data were obtained from 3-day weighing dietary records. Participants were divided into sex-specific quartiles of energy adjusted intake of FV. Multivariate-adjusted hazard ratios (HRs) were calculated between strata of the total of FV intake, fruit intake and vegetable intake. The adjustment included age, sex, smoking, drinking habit and energy adjusted intakes of sodium and some other food groups.
Results:
Participants with higher FV intake were older, ate more fish, milk and dairy products and soybeans and legumes and ate less meat. Multivariate-adjusted HR (95% confidence interval; P; P for trend) for the highest versus the lowest quartile of the total of FV intake was 0.74 (0.61–0.91; 0.004; 0.003) for total CVD, 0.80 (0.59–1.09; 0.105; 0.036) for stroke and 0.57 (0.37–0.87; 0.010; 0.109) for CHD.
Conclusions:
The results showed that higher total intake of FVs was significantly associated with reduced risk of CVD mortality in Japan.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) are among the leading causes of death in most developed countries.1, 2, 3 An increasing number of cohort studies, many of them from western countries, have reported beneficial effects of increased intake of fruits and vegetables on coronary heart diseases (CHDs), stroke and CVD mortality.4, 5, 6, 7, 8, 9 In contrast, there have been few studies in Asian populations10, 11, 12, 13 and these effects need to be examined, especially as food intake pattern differs in several aspects from that in western countries: a lower intake of fat, and a higher intake of salt and fish, because salted fish and salted vegetables are common.14, 15, 16, 17, 18, 19 Frequency of obesity is lower in Asia,2, 18 and the distribution of disease also differs: a higher incidence and mortality from stroke than from CHD in Asia.2, 18, 20 In addition to there having been few studies from Asia on the relationship between fruit and vegetable intake and the risk of CVD, the findings have also been inconclusive.10-13 None of the studies reported significant association between vegetable intake and CVD mortality, whereas two cohort studies in Japan found a significant inverse association of fruit intake with CVD mortality.10, 11 We know of no studies that have found associations between fruit and vegetable intake with stroke mortality in other countries in Asia.
NIPPON DATA8021, 22 is a cohort study based on the National Survey on Circulatory Disorders (NSCDs)23 and the National Nutrition Survey (NNS) in Japan in 1980,24 both surveys were originally conducted by the Ministry of Health and Welfare of Japan. Participants were enrolled from 300 survey districts selected from throughout Japan. In light of the limited reports and equivocal findings in Asia, we used data from the NIPPON DATA80 to investigate more fully the associations of fruit and vegetable (FV) intake with mortality from total CVD, stroke and CHD.
Methods
NIPPON DATA80
Cohort studies based on the NSCD23 have been named the National Integrated Project for Prospective Observation of Non-communicable Disease and Its Trends in the Aged (NIPPON DATA).21, 22, 25 The present study analyzed data from the NIPPON DATA80, for which baseline surveys were undertaken in 1980 with integration of dietary data from the NNS. Further details are provided elsewhere.21, 26
In summary, 300 survey districts throughout Japan were randomly selected for the NSCD. Overall, there were 13 771 residents aged 30 years and older in the survey districts, and they were invited to participate in the NSCD in 1980. Among them, 10 546 agreed to participate (76.6% of the target sample) in the NSCD. They were also invited to participate in the NNS conducted in the same year and 3-day dietary record data were obtained. We used both results from NSCD and NNS with permission from the Ministry of Health and Welfare. A total of 10 422 were identified as the same individual by comparing NSCD data and NNS data. Follow-up was made possible through linkage with registration records from municipal governments with updates that were made available as participants move between localities. We excluded those without a residential address, which was needed for linkage to vital statistical records (n=872).
Participants aged 80 years and older were also excluded (n=150), as were subjects with missing data on body mass index (BMI), smoking and drinking habit, use of hypertensive medication or on a history of diabetes mellitus (DM), CHD or stroke (n=274). Additional exclusions were made when total energy intake fell below 500 kcal/day or was 5000 kcal/day or higher (n=14).27 The remaining sample that is used in this report comprises 9112 participants (4000 men and 5112 women).
Baseline examinations
The NSCD consisted of history taking, physical examinations, blood tests and a self-administered questionnaire on lifestyle. The survey was conducted at public health centers according to a standardized manual. BMI was calculated as weight (kg) divided by the square of height (m). In the lifestyle questionnaire, participants were asked about their alcohol drinking habit (never, past, occasional or daily drinker), smoking habit (never, past or current smoker), use of antihypertensive medications and their history of DM, CHD and stroke. Questionnaires were administered during face-to-face interviews by trained public health nurses.
Dietary survey
In the NNS, dietary records for an entire household were collected for 3 consecutive days, excluding Saturday, Sunday and national holidays.28 Participants were asked to weigh and record all food and beverages with the amounts that were consumed by any household member. Trained dietitians reviewed and confirmed the accuracy of the data and assigned food codes using standard food tables.29 The dietary records were then used to calculate nutrient and food group intakes per household. Although data on only household intake are available in the NNS in 1980, estimates of individual intake were derived by taking the total intake for a household divided by the number of household members. Refinements in the individual intake values were further made by accounting for differences in proportional amounts consumed by age and sex as reported in the NNS in 1995 when information became available on how food or dishes were shared by family members.26, 30 On the basis of the NNS report, total food intake within a household was proportionally distributed among family members according to a member’s age and sex. Further details on the estimation of individual dietary intake are provided elsewhere.26
End point determination
For the present study, the participants were followed for 24 years until 2004. The procedure used for end point determination in our study has been reported elsewhere.21 Briefly, deaths are identified every 5 years through a search of the National Vital Statistics database with permission from the Management and Coordination Agency, Government of Japan. Collected information included the subject’s residence and cause of death. The underlying causes of death were assigned centrally according to the International Classification of Diseases, Ninth Revision (ICD-9), through the end of 1994 and according to the International Classification of Diseases, Tenth Revision (ICD-10), from the beginning of 1995. Deaths from total CVD (ICD-9: 393-459 and ICD-10: I00 to I99), stroke (ICD-9: 430–438 and ICD-10: I60.0–I69.8) and CHD (ICD-9: 410–414 and ICD-10: I20.0–I25.9) were identified. Approval for the study was obtained from the institutional review board of Shiga University of Medical Science (No. 12–18, 2000).
Statistical analysis
Vegetable intake was calculated as the total of yellow-green and other vegetables (including salted vegetables) and mushrooms. Potatoes were not included in this calculation. Fruit intake was calculated as the total from all fruit (including fruit juice and canned fruit). Food group intake per 1000 kcal, nutrient intake per 1000 kcal and nutrient densities (%kcal) for protein, total fat and carbohydrates were also derived. For the current report, participants were divided into quartiles of total intake of fruits and vegetables, fruits alone and vegetables alone. Quartiles were defined separately for men and women. Differences in baseline characteristics and means of nutritional variables across the quartiles were compared by analysis of variance or the χ2 test.
Sex- and age-adjusted mortalities were calculated by direct method using Japanese model population in 1985 for each quartile. To examine the association of FV intake with a mortality end point, Cox proportional hazards models were used. Results from the models provided estimates of the hazard ratio (HR) of a fatal event in the top three quartiles of FV intake versus the lowest quartile (the reference). Three models were investigated. Model 1 included sex and age as covariates. In model 2, additional covariates included BMI, smoking and drinking behavior and sodium intake (mg/1000 kcal). In model 3, further adjustments were made for the intakes of meat, fish and shellfish, milk and dairy products and soybeans and legumes. For each model, interaction effects between sex and FV intake were also examined. Separate analyses were conducted for total FV intake, fruit intake alone and vegetable intake alone. In model 3, vegetable intake alone and fruit intake alone were modeled jointly to help determine whether either intake variable had an effect on a mortality end point that was independent of the other intake variable. Trend analyses were also performed using the Cox proportional hazards model, with fruit and vegetable intake quartiles analyzed as a continuous variable.
Sex-specific models were also derived, as were models according to hypertension and diabetes status. Additional models were examined for subjects >60 years old and models for those who were younger. Hypothesis testing was two-sided with a 0.05 level of significance. SPSS v.21.0 for Windows (IBM Corporation, Chicago, IL, USA) was used throughout the analyses.
Results
Characteristics of the study participants across the quartiles of fruit and vegetable intake are shown in Table 1. Approximately 56% percent of participants were women in each quartile. From the bottom to top quartiles, median intake (g/1000 kcal) increased from 113 to 249 in men and from 148 to 332 in women. For both sexes combined, the average age in bottom quartile was 46.1 years and 55.2 years in the top. Moving from low to high fruit and vegetable quartiles, mean intakes (g/1000kcal) of fish and shellfish (49–56), milk and dairy products (34–43) and soybeans and legumes (32–42) increased. Intakes of potassium (1136 –1638 mg/1000 kcal), sodium (2288–2971) and dietary fiber (6.7–10.6 g/1000 kcal) also increased. Conversely, meat intake declined from 30 to 27 g/1000 kcal with rising intake of fruits and vegetables. Use of medications to treat hypertension (7.1–16.0%) and the presence of diabetes (2.3–3.8%) rose with increasing intake of fruits and vegetables.
During the 24-year course of follow-up, there were 823 total CVD deaths, 385 stroke deaths and 165 CHD deaths (Table 2). Table 2 provides sex- and age-adjusted person-year mortalities, and results from the Cox analyses on the association of fruit and vegetable intake with the risk of mortality due to each cause are shown. More numbers of death were included in higher quartiles, but adjusted mortalities tended to be lower because more elderly participants were included in the higher quartiles and age distribution of the standard model population differed from that of the study population.
From Cox analyses, increased intake of fruits and vegetables was significantly associated with a lower risk of mortality for total CVD in all models. The multivariate-adjusted HR (95% confidence interval; P for the HR; P for trend) for the top versus bottom quartiles was 0.77 (0.64–0.93; 0.008; 0.006) in model 1 and 0.74 (0.61–0.91; 0.004; 0.018) in model 3. For stroke mortality, the inverse associations with FVs were less significant. The P value for the HR for the top versus bottom quartile was 0.105 in model 3, whereas risk lowering trend was significant (P for trend=0.036). For CHD, although result of trend analysis was not significant (P for trend=0.109), Q2, Q3 and Q4 were associated with lower risk of mortality with significance or borderline significance. The P values for the HRs were <0.001, 0.052 and 0.010 for the Q2, Q3 and Q4 quartiles versus the bottom quartile, respectively, in model 3. The multivariate-adjusted HR using model 3 for the total of Q2 to Q4 versus Q1 was 0.55 (P=0.001; data not shown).
Results from the Cox analyses using fruit intake alone and vegetable intake alone are shown in Tables 3 and 4, respectively. In both instances, adjustments were made for the other intake variable. The association of increased fruit intake with risk of CVD mortality was similar to that of vegetable intake. Significant inverse associations with the risk of total CVD mortality were observed for each intake variable in model 3. The multivariate-adjusted HR (95% confidence interval; P for the HR; P for trend) for the top versus bottom quartiles in model 3 was 0.79 (0.65–0.96; 0.018; 0.029) for fruit (Tables 3) and 0.81 (0.66–1.00; 0.046; 0.021) for vegetable (Table 4). Although fruit intake was significantly and inversely associated with the risk of stroke mortality, the association with the risk of CHD mortality was less clear. The P values for the HR for the top versus bottom quartile in model 3 were 0.020 for stroke and 0.596 for CHD. Results of analyses using quartiles of vegetable intake also yielded similar results to those using quartiles of total FV intake (Table 4). Significance, however, was weaker for mortality from stroke and CHD. The P values for HR for the top versus bottom quartile in model 3 were 0.165 for stroke and 0.060 for CHD.
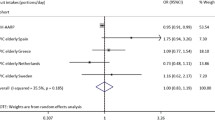
Results of sex-specific analyses are shown in Supplementary Table 1. The overall trends were similar for men and women, with some loss of significance for women. The interaction effect of sex with FV intake was not significant (P=0.167 for total CVD, P=0.608 for stroke and P=0.213 for CHD in model 3; data not shown). In Supplementary Table 2, results from stratifying participants according to the use of antihypertensive medication and a history of DM are shown. In the absence of antihypertensive treatment and a history of DM, intake of fruits and vegetables was significantly and inversely associated with risk of mortality from total CVD, stroke and CHD. The association was less clear for participants receiving treatment for hypertension or who had a history of DM. Dichotomizing participants by age (<60 versus ⩾60 years) yielded similar results for the younger participants and the elderly, with some loss of significance for both groups (Supplementary Table 3).
Discussion
We found a significant inverse association of increased FV intake with the risk of mortality from total CVD in men and women recruited from 300 general population samples from all over Japan. The findings were independent of other confounding factors including age, sex, BMI, smoking and drinking habit, sodium intake and intake of several other food groups. For stroke mortality, the overall trends were similar to total CVD mortality. For CHD, the trend analysis was not significant, but the HR comparing the combined top 3 quartiles with the bottom quartile was significant. This suggests that benefits from consuming fruits and vegetables to lower CHD risk can occur at lower levels of intake than it does for stroke. The associations were similar for both men and women and also evident when the participants were limited to those without antihypertensive medication and a history of DM.
The median intake of fruits and vegetables is 136 g/1000 kcal higher in the top versus bottom quartile for men and 184 g/1000 kcal for women. These excess amounts of intake correspond to an approximate 26% lower risk of CVD. Stroke mortality risk was 20% lower and CHD mortality risk was 43% lower. From meta-analysis by He et al., pooled relative risks for those consuming five or more servings per day compared with fewer than three servings of fruits and vegetables were 0.83 for stroke and 0.74 for CHD mortality.6, 31 In a more recent cohort study on the association of FV intake with CHD mortality, an increase in one serving per day of fruits and vegetables was associated with relative risk of 0.95 for CHD mortality.7 Only cohort studies in western populations were included in these meta-analyses, and sodium intake was not adjusted for any of the studies involved. Our current results including sodium intake as a covariate may be concordant with the results in western populations.
One of the strengths of this study is that participants were enrolled from 300 survey districts randomly selected from throughout Japan, and thus the effect of regional differences was minimized. Another strength is that we used baseline dietary data obtained from 3-day weighing dietary records, a standardized method applied for NNS.28 In many cohort study settings, food frequency questionnaires have often been used. In food frequency questionnaires, participants are asked to indicate their average frequency of food consumption listed in the questionnaires, and portion sizes are not fully considered. It is thus generally difficult to evaluate total energy and salt intake from food frequency questionnaires.32, 33 In this study, we used dietary variables obtained from 3-day weighing dietary records and could use intakes of fruits and vegetables in grams, total energy, sodium intake in mg and other nutrients.
Vegetable consumption is often associated with high salt intake in Japan; some people often use table soy sauce on salted vegetables and vegetables cooked with soy sauce are common in Japan.34 From Japanese cohort studies, Takachi et al. reported a significant inverse association of fruit intake with risk of mortality from total CVD, but not of vegetable intake, in which sodium intake was not adjusted.10 Nagura et al. also reported a significant inverse association of fruit intake with risk or mortality from CVD, but not for vegetable intake, although they adjusted sodium intake.11 They both used dietary data obtained from food frequency questionnaires. In Japan, 10% of daily salt intake is derived from salted vegetables (tsukemono).34, 35 As salt reduction is well established as the most important factor in explaining the large declines in CVD risk in Japan during the past 30 years,36 recommendations to encourage the intake of vegetables need to coincide with vigorous recommendations to avoid salty vegetables. Our current results suggest a beneficial effect of increased vegetable intake while avoiding increased salt intake and the importance of considering sodium intake in evaluation of the effects of dietary factors on CVDs, especially in Japan.
The possible protective effect of fruits and vegetables on CVD mortality might be mediated through well-established CVD risk factors. Fruits and vegetables are important sources of potassium, dietary fiber, folate and various antioxidants. In a randomized controlled trial using meals with increased intake of fruits and vegetables, with a subsequent rise in 24-hurinary potassium excretion, blood pressure was decreased effectively.37, 38 Many controlled trials also reported increased potassium intake and decreased blood pressure.39, 40 In a study in which usual salt was replaced with potassium-enriched salt in meals prepared for the elderly for 31 months, reduced CVD mortality was observed;41 this effect might have been attributable to both reduced sodium intake and increased potassium intake. Because hypertension is a major risk factor for CVD, the blood-pressure-lowering effect of potassium in fruits and vegetables might be a major mechanism contributing to a reduced risk of CVD. The effects of dietary fiber on CVD and CVD risk factors were also reported elsewhere; the reported beneficial effects with increased intake of dietary fiber were lower serum cholesterol levels and improved glycemia and insulin sensitivity.42 Fruits and vegetables are rich in antioxidants, and associations of dietary intake or serum concentration of certain antioxidants with CVD outcomes have been examined and beneficial effects have been reported.43 The protective effect of FV intakes on CVD mortality in this study may be based on the total effect of these factors attributable to fruits and vegetables.
There are some limitations in this study. Subjects in the present data set were followed up to 24 years, and participants in a wide age range were included: 30–79 years of age. As data on only household intake were available, individual intake had to be measured by using estimates of average intake patterns in Japan for an individual’s age and sex based on the NNS survey. The dietary intake of an entire household was proportionally distributed among individual household members by accounting for typical sex and age intakes derived from the NNS. Although the way in which foods are shared within and between families is likely to vary, the extent of this variation could not be assessed in this study. Dietary record data were collected only on weekdays. Potential day-of-week effects on food and nutrient intake were also not taken into account.44 The dietary assessment was carried out only once at baseline, and change of dietary habit over the follow-up period was not accounted for. The status of CVD risk factors and other lifestyle factors may have changed after the baseline survey. There may also be a possibility that we could not adjust for other potential confounding factors. For instance, individuals who eat more fruits and vegetables have higher levels of physical exercise, which was not included in the current study. The inherent measurement error in these assessments could cause bias in the results. However, any bias from measurement error would probably tend to attenuate the identified protective effect of fruits and vegetables, and the sizes of the reductions in stroke and CHD risk seen in our study could have been underestimated.
In summary, the results of the analyses present a beneficial association between increased intake of fruits and vegetables and CVD mortality in Japanese men and women, which supports the recommendation to eat a sufficient amount of fruits and vegetables while avoiding increased sodium intake to prevent CVD.
References
Yusuf S, Reddy S, Ounpuu S, Anand S . Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001; 104: 2746–2753.
Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation 2008; 118: 2702–2709.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB et al. Executive summary: heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 2013; 127: 143–152.
Bazzano LA, He J, Ogden LG, Loria CM, Vupputuri S, Myers L et al. Fruit and vegetable intake and risk of cardiovascular disease in US adults: the first National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Am J Clin Nutr 2002; 76: 93–99.
Dauchet L, Amouyel P, Hercberg S, Dallongeville J . Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr 2006; 136: 2588–2593.
He FJ, Nowson CA, Lucas M, MacGregor GA . Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens 2007; 21: 717–728.
Crowe FL, Roddam AW, Key TJ, Appleby PN, Overvad K, Jakobsen MU et al. Fruit and vegetable intake and mortality from ischaemic heart disease: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart study. Eur Heart J 2011; 32: 1235–1243.
Streppel MT, Sluik D, van Yperen JF, Geelen A, Hofman A, Franco OH et al. Nutrient-rich foods, cardiovascular diseases and all-cause mortality: the Rotterdam study. Eur J Clin Nutr 2014; 68: 741–747.
Oyebode O, Gordon-Dseagu V, Walker A, Mindell JS . Fruit and vegetable consumption and all-cause, cancer and CVD mortality: analysis of Health Survey for England data. J Epidemiol Community Health 2014; 68: 856–862.
Takachi R, Inoue M, Ishihara J, Kurahashi N, Iwasaki M, Sasazuki S et al. Fruit and vegetable intake and risk of total cancer and cardiovascular disease: Japan Public Health Center-Based Prospective Study. Am J Epidemiol 2008; 167: 59–70.
Nagura J, Iso H, Watanabe Y, Maruyama K, Date C, Toyoshima H et al. Fruit, vegetable and bean intake and mortality from cardiovascular disease among Japanese men and women: the JACC Study. Br J Nutr 2009; 102: 285–292.
Nakamura K, Nagata C, Oba S, Shimizu H . Fruit and vegetable intake and mortality from cardiovascular disease are inversely associated in Japanese women but not in men. J Nutr 2008; 138: 1129–1134.
Odegaard AO, Koh WP, Yuan JM, Gross MD, Pereira MA . Dietary patterns and mortality in a Chinese population. Am J Clin Nutr 2014; 100: 877–883.
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 1988; 297: 319–328.
Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C et al. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens 2003; 17: 623–630.
Okuda N, Ueshima H, Okayama A, Saitoh S, Nakagawa H, Rodriguez BL et al. Relation of long chain n-3 polyunsaturated fatty acid intake to serum high density lipoprotein cholesterol among Japanese men in Japan and Japanese-American men in Hawaii: the INTERLIPID study. Atherosclerosis 2005; 178: 371–379.
Brown IJ, Tzoulaki I, Candeias V, Elliott P . Salt intakes around the world: implications for public health. Int J Epidemiol 2009; 38: 791–813.
Iso H . Lifestyle and cardiovascular disease in Japan. J Atheroscler Thromb 2011; 18: 83–88.
Miyagawa N, Miura K, Okuda N, Kadowaki T, Takashima N, Nagasawa SY et al. Long-chain n-3 polyunsaturated fatty acids intake and cardiovascular disease mortality risk in Japanese: a 24-year follow-up of NIPPON DATA80. Atherosclerosis 2014; 232: 384–389.
Hu D, Yu D . Epidemiology of cardiovascular disease in Asian women. Nutr Metab Cardiovasc Dis 2010; 20: 394–404.
NIPPON DATA80 Research Group. Impact of elevated blood pressure on mortality from all causes, cardiovascular diseases, heart disease and stroke among Japanese: 14 year follow-up of randomly selected population from Japanese – NIPPON DATA80. J Hum Hypertens 2003; 17: 851–857.
NIPPON DATA80 Research Group. Risk assessment chart for death from cardiovascular disease based on a 19-year follow-up study of a Japanese representative population. Circ J 2006; 70: 1249–1255.
Japanese Ministry of Health and Welfare National Survey on Circulatory Disorders, 1980 (in Japanese). Japan Heart Foundation: Tokyo, 1982.
Japanese Ministry of Health and Welfare The National Nutrition Survey in Japan, 1980 (in Japanese). Daiichi Shuppan: Tokyo, 1982.
Okayama A, Kadowaki T, Okamura T, Hayakawa T, Ueshima H . Age-specific effects of systolic and diastolic blood pressures on mortality due to cardiovascular diseases among Japanese men (NIPPON DATA80). J Hypertens 2006; 24: 459–462.
Okuda N, Miura K, Yoshita K, Matsumura Y, Okayama A, Nakamura Y et al. Integration of data from NIPPON DATA80/90 and National Nutrition Survey in Japan: for cohort studies of representative Japanese on nutrition. J Epidemiol 2010; 20: S506–S514.
Willet W . Nutritional Epidemiology, 3rd edn. Oxford University Press: New York, 2012.
Yoshiike N, Matsumura Y, Iwaya M, Sugiyama M, Yamaguchi M . National Nutrition Survey in Japan. J Epidemiol 1996; 6: S189–S200.
The Resources Council, Science and Technology Agency of Japan The Standard Tables of Food Composition in Japan (3rd revised edn; in Japanese). Printing Bureau, Ministry of Finance: Tokyo, Japan, 1963.
Iwaoka F, Yoshiike N, Date C, Shimada T, Tanaka H . A validation study on a method to estimate nutrient intake by family members through a household-based food-weighing survey. J Nutr Sci Vitaminol 2001; 47: 222–227.
He FJ, Nowson CA, MacGregor GA . Fruit and vegetable consumption and stroke: meta-analysis of cohort studies. Lancet 2006; 367: 320–326.
Kipnis V, Midthune D, Freedman L, Bingham S, Day NE, Riboli E et al. Bias in dietary-report instruments and its implications for nutritional epidemiology. Public Health Nutr 2002; 5: 915–923.
Wakai K . A review of food frequency questionnaires developed and validated in Japan. J Epidemiol 2009; 19: 1–11.
Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc 2010; 110: 736–745.
Okuda N, Stamler J, Brown IJ, Ueshima H, Miura K, Okayama A et al. Individual efforts to reduce salt intake in China, Japan, UK, USA: What did people achieve? The INTERMAP Population Study. J Hypertens 32: 2385–2392.
Miura K . Epidemiology and prevention of hypertension in Japanese: how could Japan get longevity? EPMA J 2011; 2: 59–64.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001; 344: 3–10.
Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER 3rd, Lin PH et al. Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial. Am J Clin Nutr 2001; 74: 80–89.
Houston MC . The importance of potassium in managing hypertension. Curr Hypertens Rep 2011; 13: 309–317.
Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP . Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 2013; 346: f1378.
Chang HY, Hu YW, Yue CS, Wen YW, Yeh WT, Hsu LS et al. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr 2006; 83: 1289–1296.
Anderson JW, Baird P, Davis RH Jr, Ferreri S, Knudtson M, Koraym A et al. Health benefits of dietary fiber. Nutr Rev 2009; 67: 188–205.
Ceriello A . Possible role of oxidative stress in the pathogenesis of hypertension. Diabetes Care 2008; 31: S181–S184.
Gibson S . Principles of Nutritional Assessment. Oxford University Press: New York, USA, 1990.
Acknowledgements
This study was supported by a Grant-in-Aid from the Ministry of Health, Labor and Welfare under the auspices of the Japanese Association for Cerebro-cardiovascular Disease Control, a Research Grant for Cardiovascular Diseases (7A-2) from the Ministry of Health, Labor and Welfare and a Health and Labor Sciences Research Grant, Japan (Comprehensive Research on Aging and Health (H11-Chouju-046, H14-Chouju-003, H17-Chouju-012, H19-Chouju-Ippan-014) and Comprehensive Research on Life-Style Related Diseases including Cardiovascular Diseases and Diabetes Mellitus (H22-Jyunkankitou-Seisyu-Sitei-017, H25-Jyunkankitou-Seisyu-Sitei-022)).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
The NIPPON DATA80/90 Research Group Chairperson: Hirotsugu Ueshima (Department of Health Science, Shiga University of Medical Science, Otsu, Shiga, Japan). Co-chairpersons: Akira Okayama (Research Institute of Strategy for Prevention, Tokyo, Japan) for the NIPPON DATA80, and Tomonori Okamura (Department of Preventive Medicine and Public Health, Keio University, Tokyo, Japan) for the NIPPON DATA90. Research members: Shigeyuki Saitoh (Sapporo Medical University School of Health Science, Sapporo, Hokkaido, Japan), Kiyomi Sakata (Department of Hygiene and Preventive Medicine, Iwate Medical University, Morioka, Iwate, Japan), Atsushi Hozawa (Department of Preventive Medicine and Epidemiology, Tohoku Medical Megabank Organization, Tohoku University, Sendai, Miyagi, Japan), Takehito Hayakawa (Department of Hygiene and Preventive Medicine, Fukushima Medical University, Fukushima, Japan), Yosikazu Nakamura (Department of Public Health, Jichi Medical University, Shimotsuke, Tochigi, Japan), Yasuhiro Matsumura (Faculty of Health and Nutrition, Bunkyo University, Chigasaki, Kanagawa, Japan), Nobuo Nishi (Center for International Collaboration and Partnership, National Institute of Health and Nutrition, Tokyo, Japan), Nagako Okuda (Department of Nutritional Epidemiology, National Institute of Health and Nutrition, Tokyo, Japan), Fumiyoshi Kasagi (Institute of Radiation Epidemiology, Radiation Effects Association, Tokyo, Japan), Toru Izumi (Faculty of Medicine, Kitasato University, Sagamihara, Kanagawa, Japan), Toshiyuki Ojima (Department of Community Health and Preventive Medicine, Hamamatsu University School of Medicine, Hamamatsu, Shizuoka, Japan), Koji Tamakoshi (Department of Public Health and Health Information Dynamics, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan), Hideaki Nakagawa (Department of Epidemiology and Public Health, Kanazawa Medical University, Kanazawa, Ishikawa, Japan), Katsuyuki Miura, Takayoshi Ohkubo, Yoshikuni Kita (Department of Health Science, Shiga University of Medical Science, Otsu, Shiga, Japan), Yasuyuki Nakamura (Cardiovascular Epidemiology, Kyoto Women’s University, Kyoto, Japan), Katsushi Yoshita (Osaka City University Graduate School of human life science, Osaka, Japan), Aya Kadota (Department of School Nursing and Health Education, Osaka Kyoiku University, Kashiwara, Osaka, Japan), Kazunori Kodama (Radiation Effects Research Foundation, Hiroshima, Japan) and Yutaka Kiyohara (Department of Environmental Medicine, Kyushu University, Fukuoka, Japan).
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Okuda, N., Miura, K., Okayama, A. et al. Fruit and vegetable intake and mortality from cardiovascular disease in Japan: a 24-year follow-up of the NIPPON DATA80 Study. Eur J Clin Nutr 69, 482–488 (2015). https://doi.org/10.1038/ejcn.2014.276
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.276
- Springer Nature Limited
This article is cited by
-
Dietary practices, food purchasing, and perceptions about healthy food availability and affordability: a cross-sectional study of low-income Malaysian adults
BMC Public Health (2022)
-
Projections of disability-adjusted life years for major diseases due to a change in vegetable intake in 2017–2040 in Japan
BMC Public Health (2021)
-
A lower maximum bite force is a risk factor for developing cardiovascular disease: the Suita study
Scientific Reports (2021)
-
Cooking skills related to potential benefits for dietary behaviors and weight status among older Japanese men and women: a cross-sectional study from the JAGES
International Journal of Behavioral Nutrition and Physical Activity (2020)
-
Relationship between carbohydrate and dietary fibre intake and the risk of cardiovascular disease mortality in Japanese: 24-year follow-up of NIPPON DATA80
European Journal of Clinical Nutrition (2020)