Abstract
Background/Objectives:
Chronic kidney disease (CKD) is a major health concern associated with increased risk of cardiovascular disease, morbidity and mortality. Current CKD practice guidelines overlook dietary fiber, which is chronically low in the renal diet. However, increasing dietary fiber has been proposed to ameliorate the progress of CKD. We therefore conducted a systematic review and meta-analysis on the effect of dietary fiber intake on serum urea and creatinine as classical markers of renal health in individuals with CKD.
Subjects/Methods:
We searched MEDLINE, EMBASE, CINHAL and the Cochrane Library for relevant clinical trials with a follow-up ⩾7 days. Data were pooled by the generic inverse variance method using random-effects models and expressed as mean difference (MD) with 95% confidence intervals (95% CIs). Heterogeneity was assessed by the Cochran Q statistic and quantified by I2.
Results:
A total of 14 trials involving 143 participants met the eligibility criteria. Dietary fiber supplementation significantly reduced serum urea and creatinine levels in the primary pooled analyses (MD, −1.76 mmol/l (95% CI, −3.00, −0.51), P<0.01 and MD, −22.83 mmol/l (95% CI, −42.63, −3.02), P=0.02, respectively) with significant evidence of interstudy heterogeneity only in the analysis of serum urea.
Conclusions:
This is the first study to summarize the potential beneficial effects of dietary fiber in the CKD population demonstrating a reduction in serum urea and creatinine, as well as highlighting the lack of clinical trials on harder end points. Larger, longer, higher-quality clinical trials measuring a greater variety of uremic toxins in CKD are required (NCT01844882).
Similar content being viewed by others
Introduction
Despite the accumulating evidence on the beneficial effects of dietary fiber in ameliorating uremic environments, guidelines make little or no reference to dietary fiber intake for chronic kidney disease (CKD).1, 2, 3, 4, 5, 6 In fact, the renal diet has chronically been deficient in dietary fiber due to concerns over increased potassium and phosphorus intake. As a result, the benefits of fiber including adequate laxation are often overlooked in those with CKD. Stephen and Cummings7 in the early 1980s were among the first to show that dietary fiber consumption increased fecal bacterial mass and nitrogen excretion. Their findings for dietary fiber intake have since been validated by others and support the notion of a lower uremic toxin production by bacterial degradation of dietary and secretory proteins of the gastrointestinal tract,8, 9, 10, 11 as well as improved cardiovascular disease (CVD) risk factor profile and oxidative stress status.12 A recent cohort study13 concluded that participants with the highest dietary cereal fiber intake, compared with those with the lowest, had a 50% reduced risk for incidence of moderate CKD. Furthermore, in the recent Prevención con Dieta Mediterránea study, a significant association was found between greater fiber intake and reduced risk of CKD.14 Unfortunately, according to NHANES III data, the average dietary fiber intake in the CKD population is about 15.4 g/day, which is much lower than the recommended 25–30g/day intake for the general population.15 Considering the potential benefits of dietary fiber and the very low average intake of this nutrient in the CKD population, we have conducted a systematic review and meta-analysis of controlled feeding trials to assess the effect of dietary fiber on serum urea and creatinine as clinical markers of uremia in individuals with CKD.
Subjects and methods
We conducted a systematic review and meta-analysis following the Cochrane Handbook for Systematic Reviews of Interventions16 and have reported our findings according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17, 18 The protocol is registered at Clinicaltrials.gov (NCT01844882).
Study selection
We searched MEDLINE, EMBASE, CINAHL and the Cochrane Library through 1 September 2014 using the search terms '(dietary fiber OR fiber$ OR fibre$ OR polysaccharides OR psyllium$ OR metamucil OR polymers OR carbohydrate$ OR dietary carbohydrate OR fermentable OR fructans OR Asteraceae OR fructooligosaccharide$ OR oligofructose$ OR chicory root$ OR jerusalem artichoke$ OR inulin OR Benefiber OR Unifiber OR lactulose) AND (chronic kidney disease OR CKD OR chronic renal failure OR CRF OR renal insufficiency OR hemodialysis OR haemodialysis OR dialysis)' (Table 1). There was no restriction placed on language and the search was supplemented with manual searches of the reference lists of all selected articles and review articles. We included controlled feeding trials investigating the effect of dietary fiber compared with non-fiber supplemented diets or low-fiber diets on serum urea and creatinine, as well as serum phosphorus, in patients with CKD or on hemodialysis (HD). Trials where protein content varied between treatments were not included in order to isolate the effects of fiber. Trials were excluded if they were <7 days of follow-up (fiber diet duration) or did not provide data on either of the end points of interest.
Data extraction
Each report was independently reviewed and had relevant data extracted by two independent reviewers (LC and AM). Each reviewer also assessed study quality using the Heyland Methodological Quality Score. Non–English language articles were translated. Extracted data included information on study setting, design, randomization, blinding, sample size and participant characteristics; fiber type, dose and comparator; follow-up; macronutrient profile of the background diet; and funding. Disagreements were reconciled by consensus.
Mean and s.d. data on serum urea and creatinine for end of treatment were extracted as the a priori end points, as well as phosphorus post hoc. All trials reported end of treatment values. Missing s.d. values were calculated from available statistics using standard formulae.16 Missing s.d. values were imputed using the pooled s.d. of other trials which report s.d.19 Correlation coefficients for individual trials were derived according to a standard formula.16, 20 In studies where correlation coefficients could not be derived from available data, a pooled correlation coefficient was applied. This pooled correlation coefficient was derived from a meta-analysis of the transformed Z-scores±s.e. of available correlation coefficients. Selected authors were contacted to request additional information.
Statistical analyses
Data were analyzed using Review Manager (RevMan) version 5.2 (Copenhagen, Denmark) for primary pooled analyses and STATA version 11 (StataCorp, College Station, TX, USA) for subgroup analyses. Data were pooled using the generic inverse variance method with random-effects models and data expressed as mean differences (MDs) with 95% confidence intervals (CIs). Inter-study heterogeneity was assessed by the Cochran Q statistic (χ2), with the significance at P<0.10 and quantified by the I2 statistic, where a value of ⩾50% indicates substantial heterogeneity.16 Potential sources of methodological heterogeneity were investigated by sensitivity analyses in which each individual trial was removed systematically and the pooled effect estimates recalculated as well as by a priori subgroup analyses for randomization (yes or no), fiber type (fermentable and non-fermentable), dose (⩽25 g/day, >25 g/day), follow-up (⩽4 week, >4 week), participant type (HD or non-HD) and Heyland Methodological Quality Score (<8, ⩾8). Meta-regression analyses were used to test for subgroup differences. Meta-regression analyses were also performed to assess the possibility of dose–response associations. Where linear relationships were not found, dose response was formally tested using meta-regression, successively adding up to 4th degree (quartic) functions of dose, to assess for improved model fit. Publication bias was investigated by visual inspection of funnel plots and formally tested using Begg21 and Egger22 tests.
Results
Search results
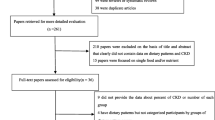
The flow of the literature for identifying trials is depicted in Figure 1. Eligible reports (8051) were identified by the search, and review of the titles and abstracts identified 72 potentially relevant reports for full review of which 60 were excluded. A total of 12 reports8, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 providing data for 14 trials met the eligibility criteria for analyses. Thirteen trials reported data for serum urea (n=123), 12 trials reported data for serum creatinine (n=120) and 7 trials reported data for serum phosphorus (n=66).
Trial characteristics
Trial characteristics are detailed in Table 2. There were 14 trials involving 143 participants described as having CKD or chronic renal failure, 74 of whom were on any type of HD. Participants tended to be middle-aged men (median age, 51.9 years (range: 22–72 years)). Median baseline serum urea was ~25.0 mmol/l (range: 4.9–42.0mmol/l) overall with 25.0 mmol/l (range: 4.9–42.0 mmol/l) for those with CKD and 26.9 mmol/l (range: 21.1–32.0 mmol/l) for HD participants. Median baseline serum creatinine was ~495.7mmol/l (range: 291.7–3180.0 mmol/l) overall with 415.5 mmol/l (range: 291.7–3180.0 mmol/l) for those with CKD and 936.0 mmol/l (range: 777.9–1060.8 mmol/l) for HD participants. Median baseline serum phosphorus was ~1.71 mmol/l (range: 1.1–2.2 mmol/l) overall and 1.45 mmol/l (range: 1.1–2.2 mmol/l) for CKD and 2.0 mmol/l (range: 1.84–2.2 mmol/l) for HD participants.
The trials tended to be small (median number of participants, 9 (range: 3–22)) and to be conducted in European countries (6/14). Most trials were of short duration (median follow-up was 4.5 weeks (range: 1.4–20 weeks)). Four (29%) trials were randomized and all were crossover designs. All trials had a fiber supplemented/high-fiber diet group compared with a non-supplemented/low-fiber diet group. In the majority of studies (12 (86%) trials), fiber was supplemented as fermentable fiber (including gum arabic, psyllium and lactulose). Median fiber dose was 26.9 g/day (range: 3.1–50.0 g/day). The median protein intakes of the diets were ~57 g/day (range: 45–69 g/day). In all trials, intervention and control arms were matched for energy. The majority of trials (86%) were of low study quality as assessed by the Heyland Methodological Quality Score (<8). Blinding was reported in only two trials (14%), both of which were single-blinded. Funding was reported in only three trials (21%) and three trials (21%) reported having study products provided. Conflicts of interest were only reported in one trial (7%) within which no conflicts of interest were declared by the authors.
Pooled correlation coefficients were imputed and applied to five trials (38%) for serum urea, seven trials (58%) for serum creatinine and four trials (57%) for serum phosphorus.
The pooled effect of fiber on serum urea is shown in Figure 2. Fiber significantly reduced serum urea in the primary pooled analysis (MD, −1.76mmol/l (95% CI, −3.00, −0.51), P=0.006). There was significant evidence of interstudy heterogeneity. Sensitivity analyses in which each trial was systematically removed did not change the statistical significance of the interstudy heterogeneity or the urea lowering effects. The pooled effect of fiber on serum creatinine is shown in Figure 3. Similarly, dietary fiber supplementation significantly reduced serum creatinine in the overall analysis (MD, −22.83 (95% CI, −42.63, −3.02), P=0.02), however, without evidence of heterogeneity (P=0.19). A priori subgroup analyses did not reveal any significant effect modifications (Supplementary Figures 1 and 2). To assess the possibility of a dose–response association on serum urea, MD was plotted against mean dose, and no obvious linear or non-linear association between dose and MD was observed for urea (Supplementary Figure 3). Dose response was formally tested using meta-regression, successively adding up to 4th degree (quartic) functions of dose, and none of these improved model fit, confirming a lack of non-linear dose–response effects (Supplementary Table 1). However, there was a significant dose response observed for creatinine where increasing dose of fiber resulted in a greater reduction in serum creatinine (Supplementary Figure 4).
Forest plot for the effect of dietary fiber on serum urea concentration (mmol/l). Data are expressed as weighted mean differences (MDs) with 95% CI using generic inverse variance random-effects models. Pooled effect estimates are shown as diamonds. Inter-study heterogeneity was tested by Cochran’s Q statistic (χ2) at a significance level of P<0.10 and quantified by I2, where I2⩾50% is considered to be evidence of substantial heterogeneity. Subgroup analysis for dose were assessed by χ2at a significance level of P<0.05. CI, confidence interval.
Forest plot for the effect of dietary fiber on creatinine concentration (mmol/l). Data are expressed as weighted mean differences (MDs) with 95% CI using generic inverse variance random-effects models. Pooled effect estimates are shown as diamonds. Inter-study heterogeneity was tested by Cochran’s Q statistic (χ2) at a significance level of P<0.10 and quantified by I2, where I2⩾50% is considered to be evidence of substantial heterogeneity. Subgroup analysis for dose were assessed by χ2 at a significance level of P<0.05. CI, confidence interval.
Overall, there was no significant pooled effect seen on serum phosphorus (Figure 4).
Forest plot for the effect of dietary fiber on phosphorus concentration (mmol/l). Data are expressed as weighted mean differences (MDs) with 95% CI using generic inverse variance random-effects models. Pooled effect estimates are shown as diamonds. Inter-study heterogeneity was tested by Cochran’s Q statistic (χ2) at a significance level of P<0.10 and quantified by I2, where I2⩾50% is considered to be evidence of substantial heterogeneity. Subgroup analysis for dose were assessed by χ2 at a significance level of P<0.05. CI, confidence interval.
Discussion
This study is the first to summarize in detail previously conducted controlled clinical trials on the effects of dietary fiber in CKD. This systematic review and meta-analysis of 14 controlled feeding trials in 143 participants with CKD demonstrated that dietary fiber can reduce serum concentrations of urea and creatinine with a dose-dependent response for serum creatinine.
By definition, dietary fibers are non-digestible carbohydrates and lignans that escape digestion and arrive intact in the large intestine. However, the physiological effects of various fibers depend in part on their physico-chemical properties that can result in non-fermentable or fermentable fibers. In the current meta-analyses of the effects on serum urea and creatinine, the majority of the trials (12 out of 13) used fermentable fiber types (psyllium, gum arabic, inulin and lactulose). Therefore, our a priori subgroup analyses were limited in their ability to detect a difference between fiber types as there was only one trial using non-fermentable fibers. Our subgroup analyses demonstrated that within those trials with fermentable fibers, the results were very similar to the overall analyses, thus the results of our primary analyses may be driven by fermentable fibers. Fermentable fibers are known to stimulate colonic bacterial growth, fecal mass and short-chain fatty acid production. These changes can, in CKD, influence the uremic environment.
Dietary fiber may reduce serum urea by altering the urea enterohepatic cycling, by causing the proliferation of large-intestine microflora and the trapping of protein nitrogen in the microbial bodies, as well as in the elevation of ammonium (NH4) in the feces due to the reduction in pH by short-chain fatty acids and the conversion of diffusible ammonia (NH3) to the less-diffusible NH4.34 These processes result in increased nitrogen excretion via feces. Animal studies have demonstrated that active fermentation stimulates bacterial growth and leads to a considerable enlargement of the colonic contents and lead to cecal wall hypertrophy,35, 36, 37 an effect that may be explained by an increase in short-chain fatty acids availability through carbohydrate (e.g. butyrate) fermentation.38, 39 Resistant starches (mainly undigestible carbohydrates) have shown to have the greatest trophic effects on colonic mucosa.40, 41, 42 Although human data are lacking, it is possible that fermentable carbohydrates exert similar effects in humans.43 This trophic effect in turn stimulates the exchanges of urea and ammonia nitrogen between blood and digestive lumen.35, 36, 44, 45 Urea has been demonstrated to be permeable through the colon.46 Similarly, creatinine is transportable across the intestinal epithelium47 and has been proposed to be metabolized by intestinal bacteria.48, 49 As creatinine is a metabolic byproduct of muscle metabolism and its plasma concentration is relatively constant due to low variability in muscle turnover, the reduction in serum creatinine observed may be due to increased creatinine degradation by bacterial creatinase throughout the bowel and thus potential loss to the creatinine pool.49 Although the mechanism is unclear, creatinine is the most widely used indirect measure of the estimated glomerular filtration rate, which is the most commonly used marker of renal function clinically.
Of great importance is the fact that the majority of CKD patient deaths are due to CVD rather than progression to end-stage renal disease50 and it has been well demonstrated that dietary fiber improves a variety of CVD risk factors. Intrinsically, dietary fiber has been demonstrated to dampen glycemic excursions, improve cholesterol and improve blood pressure,51, 52, 53 which have been associated with improved renal function54, 55 as well as decreased CVD risk.50, 56, 57, 58 Extrinsically, dietary fiber consumed as either a supplement or through high-fiber foods, displaces other foods in the diet that may not be beneficial for renal function or increase the risk of CVD. For example, oats and barley may replace bread and rice, the former of which are rich in beta-glucan and have been demonstrated to lower cholesterol and blood pressure and elicit a lower glycemic response.59, 60 Finally, dietary fiber has been associated with reduced inflammation, which is elevated in CKD and CVD.61 Krishnamurthy et al.,15 using data from the National Health and Nutrition Examination Study III including just under 15 000 participants, concluded that a high total dietary fiber intake was associated with lower risk of inflammation and that these associations were stronger in those with kidney disease compared to those without. The study also found that a high total dietary fiber intake was inversely related to mortality in those with kidney disease. Therefore, there may be a potential for fiber to assist in reducing the burden of not only nitrogenous waste products that contribute to uremia, but also by reducing CVD risk factors such as inflammation, glycemic control, cholesterol and blood pressure.
From the present systematic review, all clinical trials of dietary fiber in CKD were retrieved and the discernible lack of trials assessing other uremic retention solutes was clearly evident. However, the limited studies that have been done suggest dietary fiber supplementation may also be beneficial. Protein-bound uremic retention solutes have gained more attention recently due to the fact that several groups have demonstrated direct associations with overall mortality and CVD in end-stage renal disease, as well as in CKD.8, 62, 63, 64 Specifically, these include p-cresol and indoxyl sulfates, which originate from bacterial protein fermentation in the large intestine.11 Both have also individually been associated with progression of CKD.10, 65 Meijers et al.8 demonstrated in addition to a significant reduction in serum urea, that serum p-cresol sulfate concentrations were significantly reduced by 20% in HD patients given oligofructose-enriched inulin for 4 weeks. In addition, Meyer et al.66 have discussed how dietary fiber may be associated with reducing protein fermentation and thus reducing production of p-cresols and indoxyls as well as amines. A recent meta-analysis of the effect of pre- and probiotics on p-cresol and indoxyl sulfate levels in mostly healthy individuals demonstrated a significant reduction overall.67 Therefore, dietary fiber supplementation may also act to affect multiple uremic retention solutes to improve CKD, however, further studies are warranted to support these potential effects.
Limitations of our analyses include the small number, small sample sizes (only one trial had >20 participants), short follow-up (median follow-up was only 4.5 weeks) and low quality (<15% were of high quality) of the available trials. Other limitations include the lack of description of trial characteristics, including the stage of CKD, the degree of renal impairment (baseline estimated glomerular filtration rate), fiber intake at baseline, body weight and body mass index. Thus, future high-quality, randomized controlled trials in a CKD population with larger sample sizes and longer follow-up are warranted.
The strengths of our analyses include that the median fiber dose used in the available trials was ~27g/day, which is in keeping with that recommended for adults, and all trials were controlled for dietary protein and had a crossover design, which minimizes the effects of confounders.
Practical implications
With regard to the feasibility in the CKD population, achieving higher fiber intakes remains a concern because of increased potassium and phosphorus levels, which can potentially have deleterious effects in CKD.68, 69 However, there are options for this group to increase their fiber intakes through low potassium and phosphorus fruits and vegetables and possibly fiber supplements without added phosphorus or potassium. In addition, the bioavailability of phosphorus and potassium in high-fiber foods is lower compared with other phosphorus and potassium foods, especially processed foods.
Although the present meta-analysis demonstrates significant reductions in the classical biomarkers of uremia, serum urea and creatinine, with increasing intake of dietary fiber, we are unsure whether this affects actual renal function. The search criteria employed in the current meta-analysis allowed for the capture of all clinical feeding trials using dietary fiber in a population with impaired renal function and highlighted the lack of literature, especially on other biomarkers of renal function, including serum calcium and potassium, urinary markers and glomerular filtration rate. For example, among the identified studies, only one had reported results for glomerular filtration rate. Therefore, an important implication of the current meta-analysis is that future studies evaluating the impact of dietary fiber supplements on kidney function should rely on 'creatinine-free' indices of renal function (for example, using cystatin C) or on actually measured glomerular filtration rate.
Overall, these results are important for patients, physicians and clinicians as they highlight the potential multifactorial benefits of consuming dietary fiber in the CKD population in which intakes are currently low.
Conclusion
Pooled analyses of controlled feeding trials show that dietary fiber supplementation in the diet of those with CKD leads to a reduction in serum urea and creatinine as clinical biomarkers of renal function and in a dose-dependent manner for serum creatinine.
References
KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Diabetes and Kidney Diseases. Am J Kidney Dis 2007; 2: S1–S180
Fouque D, Vennegoor M, ter Wee P, Wanner C, Basci A, Canaud B et al. EBPG guideline on nutrition. Nephrol Dial Transplant. 2007; 22: ii45–ii87.
Harris D, Thomas M, Johnson D, Nicholls K, Gillin A . Caring for Australasians with renal I. The CARI guidelines. Prevention of progression of kidney disease. Nephrology 2006; 11: S2–197.
Levin A, Hemmelgarn B, Culleton B, Tobe S, McFarlane P, Ruzicka M et al. Guidelines for the management of chronic kidney disease. CMAJ 2008; 179: 1154–1162.
Kopple JD . National kidney foundation K/DOQI clinical practice guidelines for nutrition in chronic renal failure. Am J Kidney Dis 2001; 37: S66–S70.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO Clinical Practice Guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013; 3: 1.
Stephen AM, Cummings JH . Mechanism of action of dietary fibre in the human colon. Nature 1980; 284: 283–284.
Meijers BK, De Preter V, Verbeke K, Vanrenterghem Y, Evenepoel P . p-Cresyl sulfate serum concentrations in haemodialysis patients are reduced by the prebiotic oligofructose-enriched inulin. Nephrol Dial Transplant 2010; 25: 219–224.
Meyer TW, Hostetter TH . Uremia. N Engl J Med 2007; 357: 1316–1325.
Schepers E, Glorieux G, Vanholder R . The gut: the forgotten organ in uremia? Blood Purif 2010; 29: 130–136.
Evenepoel P, Meijers BK, Bammens BR, Verbeke K . Uremic toxins originating from colonic microbial metabolism. Kidney Int Suppl 2009; 114: S12–S19.
Sánchez-Muniz F . Dietary fiber and cardiovascular health. Nutricion Hospitalaria 2012; 27: 31–45.
Gopinath B, Harris DC, Flood VM, Burlutsky G, Brand-Miller J, Mitchell P . Carbohydrate nutrition is associated with the 5-year incidence of chronic kidney disease. J Nutr 2011; 141: 433–439.
Diaz-Lopez A, Bullo M, Basora J, Martinez-Gonzalez MA, Guasch-Ferre M, Estruch R et al. Cross-sectional associations between macronutrient intake and chronic kidney disease in a population at high cardiovascular risk. Clin Nutr 2013; 32: 606–612.
Krishnamurthy VM, Wei G, Baird BC, Murtaugh M, Chonchol MB, Raphael KL et al. High dietary fiber intake is associated with decreased inflammation and all-cause mortality in patients with chronic kidney disease. Kidney Int 2012; 81: 300–306.
Higgins JP GS, ed. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. The Cochrane Collaboration; 2011 Accessed at www.cochrane-handbookorg on 22 December 2011 [Internet].
Moher D CD, Eastwood S, Olkin I, Rennie D, Stroup DF . Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet 1999; 354: 1896–1900.
Moher D LA, Tetzlaff J, Altman DG . PRISMA Group Preferred statement. Ann Intern Med 2009; 151: 264–269
Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N . Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol 2006; 59: 7–10
Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A . Meta-analyses involving cross-over trials: methodological issues. nt J Epidemiol. 2002; 31: 140–149.
Begg CB . A measure to aid in the interpretation of published clinical trials. Stat Med 1985; 4: 1–9.
Egger M, Davey Smith G, Schneider M, Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634.
Salmean YA, Segal MS, Langkamp-Henken B, Canales MT, Zello GA, Dahl WJ . Foods with added fiber lower serum creatinine levels in patients with chronic kidney disease. J Ren Nutr 2013; 23: e29–e32.
Younes H, Egret N, Hadj-Abdelkader M, Remesy C, Demigne C, Gueret C et al. Fermentable carbohydrate supplementation alters nitrogen excretion in chronic renal failure. J Ren Nutr 2006; 16: 67–74.
Rampton DS, Cohen SL, Crammond VD, Gibbons J, Lilburn MF, Rabet JY et al. Treatment of chronic renal failure with dietary fiber. Clin Nephrol 1984; 21: 159–163.
Bliss DZ, Stein TP, Schleifer CR, Settle RG . Supplementation with gum arabic fiber increases fecal nitrogen excretion and lowers serum urea nitrogen concentration in chronic renal failure patients consuming a low-protein diet. Am J Clin Nutr 1996; 63: 392–398.
Rivellese A, Parillo M, Giacco A, De Marco F, Riccardi G . A fiber-rich diet for the treatment of diabetic patients with chronic renal failure. Diabetes Care 1985; 8: 620–621.
Parillo M, Riccardi G, Pacioni D, Iovine C, Contaldo F, Isernia C et al. Metabolic consequences of feeding a high-carbohydrate, high-fiber diet to diabetic patients with chronic kidney failure. Am J Clin Nutr 1988; 48: 255–259.
Burgess MB, Littlefield D . Effect of wheat bran supplementation on colonic function and serum mineral levels in chronic renal failure hemodialysis patients. Dial Transpl 1987; 16: 184–189.
Yatzidis H, Koutsicos D, Digenis P . Oral locust bean gum therapy of uremia - favorable effects on biological abnormalities and hypertension. Dial Transpl 1980; 9: 313–317.
Miura M, Nomoto Y, Sakai H . Short term effect of lactulose therapy in patients with chronic renal failure. Tokai J Exp Clin Med 1989; 14: 29–34.
Miyazaki M, Aoyagi K, Tojo S . [Lactulose therapy for chronic renal failure]. Nihon Jinzo Gakkai shi 1984; 26: 1091–1098.
Pender FT . The effect of increasing the dietary fibre content of diets of patients with chronic renal failure treated by haemodialysis at home. J Hum Nutr Diet 1989; 2: 423–427.
Vince AJ, McNeil NI, Wager JD, Wrong OM . The effect of lactulose, pectin, arabinogalactan and cellulose on the production of organic acids and metabolism of ammonia by intestinal bacteria in a faecal incubation system. Br J Nutr 1990; 63: 17–26.
Levrat MA, Behr SR, Remesy C, Demigne C . Effects of soybean fiber on cecal digestion in rats previously adapted to a fiber-free diet. J Nutr 1991; 121: 672–678.
Younes H, Garleb K, Behr S, Remesy C, Demigne C . Fermentable fibers or oligosaccharides reduce urinary nitrogen excretion by increasing urea disposal in the rat cecum. J Nutr 1995; 125: 1010–1016.
Younes H DC, Behr S, Rémésy C . Resistant starch exerts an uremia lowering effect by enhancing urea disposal in the large intestine. Nutr Res 1995; 15: 1199–1210.
Young GP, Gibson PR . Butyrate and the human cancer cell. In: Cummings JH, Rombeau JL, Sakata T (eds). Physiological and Clinical Aspects of Short-chain fatty acids. Cambridge University Press: Cambridge, UK, 1995,, pp 319–336.
Canani RB, Costanzo MD, Leone L, Pedata M, Meli R, Calignano A . Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J Gastroenterol 2011; 17: 1519–1528.
Bauer-Marinovic M, Florian S, Muller-Schmehl K, Glatt H, Jacobasch G . Dietary resistant starch type 3 prevents tumor induction by 1,2-dimethylhydrazine and alters proliferation, apoptosis and dedifferentiation in rat colon. Carcinogenesis 2006; 27: 1849–1859.
Demigne C, Remesy C . Influence of unrefined potato starch on cecal fermentations and volatile fatty acid absorption in rats. J Nutr 1982; 112: 2227–2234.
Aufreiter S, Kim JH, O'Connor DL . Dietary oligosaccharides increase colonic weight and the amount but not concentration of bacterially synthesized folate in the colon of piglets. J Nutr 2011; 141: 366–372.
Jahns F, Wilhelm A, Jablonowski N, Mothes H, Radeva M, Wolfert A et al. Butyrate suppresses mRNA increase of osteopontin and cyclooxygenase-2 in human colon tumor tissue. Carcinogenesis 2011; 32: 913–920.
Demigne C, Levrat MA, Remesy C . Effects of feeding fermentable carbohydrates on the cecal concentrations of minerals and their fluxes between the cecum and blood plasma in the rat. J Nutr 1989; 119: 1625–1630.
Levrat MA, Rémésy C, Demigné C . Very acidic fermentations in the rat cecum during adaptation to a diet rich in amylase-resistant starch (crude potato starch). Nutr Biochem 1991; 2: 31–36.
Moran BJ, Jackson AA . 15N-urea metabolism in the functioning human colon: luminal hydrolysis and mucosal permeability. Gut 1990; 31: 454–457.
Turner JR, Cohen DE, Mrsny RJ, Madara JL . Noninvasive in vivo analysis of human small intestinal paracellular absorption: regulation by Na+-glucose cotransport. Dig Dis Sci 2000; 45: 2122–2126.
Jones JD, Burnett PC . Creatinine metabolism in humans with decreased renal function: creatinine deficit. Clin Chem 1974; 20: 1204–1212.
Dunn SR, Gabuzda GM, Superdock KR, Kolecki RS, Schaedler RW, Simenhoff ML . Induction of creatininase activity in chronic renal failure: timing of creatinine degradation and effect of antibiotics. Am J Kidney Dis 1997; 29: 72–77.
Weiner DE, Tighiouart H, Amin MG, Stark PC, MacLeod B, Griffith JL et al. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. J Am Soc Nephrol 2004; 15: 1307–1315.
Vuksan V, Jenkins DJ, Spadafora P, Sievenpiper JL, Owen R, Vidgen E et al. Konjac-mannan (glucomannan) improves glycemia and other associated risk factors for coronary heart disease in type 2 diabetes. A randomized controlled metabolic trial. Diabetes Care 1999; 22: 913–919.
Streppel MT, Arends LR, van 't Veer P, Grobbee DE, Geleijnse JM . Dietary fiber and blood pressure: a meta-analysis of randomized placebo-controlled trials. Arch Intern Med 2005; 165: 150–156.
Brown L, Rosner B, Willett WW, Sacks FM . Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr 1999; 69: 30–42.
Schrijvers BF, De Vriese AS, Flyvbjerg A . From hyperglycemia to diabetic kidney disease: the role of metabolic, hemodynamic, intracellular factors and growth factors/cytokines. Endocr Rev 2004; 25: 971–1010.
Blood Pressure Lowering Treatment Trialists Collaboration. Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials. BMJ 2013; 347: f5680.
Threapleton DE, Greenwood DC, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C et al. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ 2013; 347: f6879.
He M, van Dam RM, Rimm E, Hu FB, Whole-grain Qi L . cereal fiber, bran, and germ intake and the risks of all-cause and cardiovascular disease-specific mortality among women with type 2 diabetes mellitus. Circulation 2010; 121: 2162–2168.
Liu S, Buring JE, Sesso HD, Rimm EB, Willett WC, Manson JE . A prospective study of dietary fiber intake and risk of cardiovascular disease among women. J Am Coll Cardiol 2002; 39: 49–56.
Jenkins DJ, Kendall CW, Vuksan V, Vidgen E, Parker T, Faulkner D et al. Soluble fiber intake at a dose approved by the US Food and Drug Administration for a claim of health benefits: serum lipid risk factors for cardiovascular disease assessed in a randomized controlled crossover trial. Am J Clin Nutr 2002; 75: 834–839.
Tosh SM . Review of human studies investigating the post-prandial blood-glucose lowering ability of oat and barley food products. Eur J Clin Nutr 2013; 67: 310–317.
North CJ, Venter CS, Jerling JC . The effects of dietary fibre on C-reactive protein, an inflammation marker predicting cardiovascular disease. Eur J Clin Nutr 2009; 63: 921–933.
Bammens B, Evenepoel P, Keuleers H, Verbeke K, Vanrenterghem Y . Free serum concentrations of the protein-bound retention solute p-cresol predict mortality in hemodialysis patients. Kidney Int 2006; 69: 1081–1087.
Meijers BK, Bammens B, De Moor B, Verbeke K, Vanrenterghem Y, Evenepoel P . Free p-cresol is associated with cardiovascular disease in hemodialysis patients. Kidney Int 2008; 73: 1174–1180.
Liabeuf S, Barreto DV, Barreto FC, Meert N, Glorieux G, Schepers E et al. Free p-cresylsulphate is a predictor of mortality in patients at different stages of chronic kidney disease. Nephrol Dial Transplant 2010; 25: 1183–1191.
Niwa T, Nomura T, Sugiyama S, Miyazaki T, Tsukushi S, Tsutsui S . The protein metabolite hypothesis, a model for the progression of renal failure: an oral adsorbent lowers indoxyl sulfate levels in undialyzed uremic patients. Kidney Int Suppl 1997; 62: S23–S28.
Meyer TW, Hostetter TH . Uremic solutes from colon microbes. Kidney Int 2012; 81: 949–954.
Rossi M, Klein K, Johnson DW, Campbell KL . Pre-, pro-, and synbiotics: do they have a role in reducing uremic toxins? A systematic review and meta-analysis. Int J Nephrol 2012; 2012: 673631.
Palmer SC, Hayen A, Macaskill P, Pellegrini F, Craig JC, Elder GJ et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA 2011; 305: 1119–1127.
Putcha N, Allon M . Management of hyperkalemia in dialysis patients. Semin Dial 2007; 20: 431–439.
Acknowledgements
LC and PBD designed the research. LC and AM conducted the research. LC and AM analyzed the data. LC and PBD wrote the paper. LC, AM, JLS, DJAJ and PBD were responsible for critical revision of the manuscript. PBD had primary responsibility for final content. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
LC works as a casual Clinical Research Coordinator at GI Laboratories, Toronto, Canada. LC and AM have received research support from the Canadian Institutes of Health Research (CIHR). JLS has received research support from the CIHR, Calorie Control Council, The Coca-Cola Company (investigator initiated, unrestricted grant), Pulse Canada and The International Tree Nut Council Nutrition Research & Education Foundation. He has received travel funding, speaker fees and/or honoraria from the American Heart Association (AHA), American Society for Nutrition (ASN), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH), Canadian Diabetes Association (CDA), Canadian Nutrition Society (CNS), Calorie Control Council, Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD), International Life Sciences Institute (ILSI) North America, International Life Sciences Institute (ILSI) Brazil, Abbott Laboratories, Pulse Canada, Dr. Pepper Snapple Group and The Coca-Cola Company. He is on the Clinical Practice Guidelines Expert Committee for Nutrition Therapy of both the Canadian Diabetes Association (CDA) and European Association for the study of Diabetes (EASD), as well as being on the American Society for Nutrition (ASN) writing panel for a scientific statement on the metabolic and nutritional effects of fructose, sucrose and high-fructose corn syrup. He is an unpaid scientific advisor for the International Life Science Institute (ILSI) North America, Food, Nutrition and Safety Program (FNSP). His wife is an employee of Unilever Canada. DJAJ holds an unrestricted grant from the Coca-Cola Company and has served on the scientific advisory board for or received research support, consultant fees or honoraria from Barilla, Solae, Unilever, Hain Celestial, Loblaws Supermarkets, Sanitarium Company, Herbalife International, Pacific Health Laboratories Inc, Metagenics/MetaProteomics, Bayer Consumer Care, Oldways Preservation Trust, The International Tree Nut Council Nutrition Research & Education, The Peanut Institute, Procter and Gamble Technical Centre Limited, Griffin Hospital for the development of the NuVal System, Pepsi Company, Soy Advisory Board of Dean Foods, Alpro Soy Foundation, Nutritional Fundamentals for Health, Pacific Health Laboratories, Kellogg’s, Quaker Oats, The Coca-Cola Sugar Advisory Board, Agrifoods and Agriculture Canada (AAFC), Canadian Agriculture Policy Institute (CAPI), Abbott Laboratories, the Almond Board of California, the California Strawberry Commission, Orafti, the Canola and Flax Councils of Canada, Pulse Canada and the Saskatchewan Pulse Growers. DJAJ also holds additional grant support from the Canadian Institutes of Health Research, Canadian Foundation for Innovation, Ontario Research Fund and Advanced Foods and Material Network. DJAJ’s spouse is a vice president and director of research at GI Laboratories (Toronto, Ontario, Canada). PBD declares no conflict of interest.
Additional information
This study was presented in part at the Canadian Nutrition Society conference, St. John’s Newfoundland, 5–7 June 2014.
Supplementary Information accompanies this paper on European Journal of Clinical Nutrition website
Supplementary information
Rights and permissions
About this article
Cite this article
Chiavaroli, L., Mirrahimi, A., Sievenpiper, J. et al. Dietary fiber effects in chronic kidney disease: a systematic review and meta-analysis of controlled feeding trials. Eur J Clin Nutr 69, 761–768 (2015). https://doi.org/10.1038/ejcn.2014.237
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.237
- Springer Nature Limited
This article is cited by
-
The benefits of dietary fiber: the gastrointestinal tract and beyond
Pediatric Nephrology (2023)
-
Metagenome-wide analysis uncovers gut microbial signatures and implicates taxon-specific functions in end-stage renal disease
Genome Biology (2023)
-
Low adherence to CKD-specific dietary recommendations associates with impaired kidney function, dyslipidemia, and inflammation
European Journal of Clinical Nutrition (2021)
-
Healthy adult vegetarians have better renal function than matched omnivores: a cross-sectional study in China
BMC Nephrology (2020)
-
The effects of 16-weeks of prebiotic supplementation and aerobic exercise training on inflammatory markers, oxidative stress, uremic toxins, and the microbiota in pre-dialysis kidney patients: a randomized controlled trial-protocol paper
BMC Nephrology (2020)