Abstract
Hematopoietic precursor cells (HPC) are able to restore hematopoiesis after high-dose chemotherapy and their cryopreservation is routinely employed prior to the autologous hematopoietic cell transplantation (AHCT). Although previous studies showed feasibility of long-term HPC storage, concerns remain about possible negative effects on their potency. To study the effects of long-term cryopreservation, we compared time to neutrophil and platelet recovery in 50 patients receiving two AHCT for multiple myeloma at least 2 years apart between 2006 and 2016, using HPC obtained from one mobilization and collection attempt before the first transplant. This product was divided into equivalent fractions allowing a minimum of 2 × 106 CD34+ cells/kg recipient’s weight. One fraction was used for the first transplant after median storage of 60 days (range, 17–165) and another fraction was used after median storage of 1448 days (range, 849–3510) at the second AHCT. Neutrophil recovery occurred at 14 days (median; range, 11–21) after the first and 13 days (10–20) after the second AHCT. Platelets recovered at a median of 16 days after both procedures. Considering other factors, such as disease status, conditioning and HPC dose, this single institution data demonstrated no reduction in the potency of HPC after long-term storage.
Similar content being viewed by others
Introduction
Hematopoietic precursor cells (HPC) have the potential to develop into all types of blood cells and to reconstitute the immune system after high-dose chemotherapy or radiotherapy. Neutrophil recovery is the earliest milestone in determining the short-term success of hematopoietic recovery from autologous hematopoietic cell transplantation (AHCT). Although many factors affect the time to neutrophil recovery after AHCT, including HPC source, CD34+ cell dose, type of disease, disease status, conditioning regimen and use of growth factors such as granulocyte colony-stimulating factor (G-CSF), significant delays are directly related to the quality of the HPC.1, 2 Consequently, continuous audit of time to neutrophil recovery in all patients is required by the Foundation for the Accreditation of Cellular Therapy (FACT)-Joint Accreditation Committee of International Society for Cellular Therapy & European Society for Blood and Marrow Transplantation (JACIE) International Standards for Cellular Therapy.3 Time to recovery of platelets is also useful to complement the safety monitoring data, however, it is more difficult to capture due to the effect of prophylactic transfusions and lack of daily count monitoring after neutrophil recovery.3
In patients with multiple myeloma, autologous HPC collection is performed after achieving best treatment response, usually after high-dose melphalan conditioning therapy.4, 5, 6 After collection, cells are cryopreserved and stored in liquid nitrogen vapor phase nitrogen tanks. Often one peripheral blood HPC collection yields sufficient cells for two or more transplants. If this happens, the cells can be stored into two or more bags to permit a subsequent transplant. Although previous studies showed the feasibility of long-term HPC storage,7 concerns remain about possible negative effects of this storage and FACT-JACIE International Standards for Cellular Therapy requires transplant centers to demonstrate that cryopreserved and long-term stored HPC maintain their potency.3
Current methodology to assess the potency of cryopreserved HPC is mainly restricted to in vitro colony-forming unit assays.8, 9 To study the possible effect of long-term cryopreservation in vivo, we compared time to post-transplantation neutrophil recovery in patients who received two AHCT for multiple myeloma, at least 2 years apart, using HPC from a single mobilization and collection attempt prior to the first transplantation.
Subjects and methods
Study design, data collection and statistical method
This was a retrospective single center cohort study using prospectively acquired routine clinical and laboratory data. All patients were consented for non-interventional research. The study was conducted in accordance with the Ethical Principles for Medical Research Involving Human Subjects outlined in the Declaration of Helsinki. Eligibility criteria for this analysis included patients who, between January 2006 and April 2016, underwent two AHCT for multiple myeloma at least 2 years apart using HPC obtained by dividing a single mobilization and collection attempt into equivalent fractions. The primary end point of this study was time to neutrophil recovery defined as the time from HPC infusion to the first of 3 consecutive days in which the absolute neutrophil count was >0.5 × 109/L. Secondary end point was time to platelet recovery defined as the time from HPC infusion to the first of 3 consecutive days in which the platelet count was >20 × 109/L without support.
Time to neutrophil recovery was analyzed using paired t-test and a linear regression analysis, considering relative CD34+ cell dose per kilogram of patient’s weight (less at second AHCT (n=10), equivalent at both AHCT (n=31), more at second AHCT (n=9)), melphalan dose ((same melphalan dose at both AHCT (n=22), lower melphalan dose at second AHCT (n=28)) and patient remission status before transplantation (disease status more favorable at second AHCT (n=10), same disease status at both AHCT (n=27), disease status less favorable at second AHCT (n=13)).
HPC collection, processing and transplantation
Autologous peripheral blood HPC leukapheresis was performed using the automated mononuclear cell collection program on the OPTIA SPECTRA apheresis machine (Terumo BCT, Zaventem, Belgium). A minimal cell dose required for a single AHCT was set as 2 × 106/kg of patient’s body weight at the time of collection, so collections with >4 × 106/kg were split into an even number of equivalent fractions prior to cryopreservation. For each collection, a 20% DMSO in 5% human albumin cryoprotectant was manufactured in advance. Cryoprotectant was mixed 1:1 (volume) with the cellular product. Cells were cryopreserved at <200 × 109/L in 10% DMSO using a controlled rate freezer (Planer PLC, Middlesex, UK) to minimize freezing damage. Aseptic preparation of the cellular products was performed in a good manufacturing practice (GMP) facility. Cells were stored in liquid nitrogen vapor phase storage tanks characterized for the temperature gradient that forms within the tank. The processing facility works on a Pharmagraph system, based on the enVigil pharmaceutical data acquisition software package, to monitor the environmental conditions within the GMP suites and the cryostorage facilities.
The conditioning regimen consisted of melphalan given at a dose of 200 mg/m2. A reduced dose of melphalan (usually 100 or 140 mg/m2) was used at the transplantation physicians’ discretion in patients over the age of 65 years, those with severe renal impairment or those with other significant comorbidities. HPC thawing was performed at the bedside by incubation at 37 °C in a temperature-controlled bath and infused within 10 min of thawing. Patients received supportive care, including antimicrobial prophylaxis with antibacterial, antifungal and antiviral agents. G-CSF was administered after both transplants at the dose of 300 μg daily from day +10 until neutrophil recovery. Prophylactic platelet transfusions were administered if platelet count dropped <10 × 109/L. Blood counts were assessed daily from initiation of conditioning until discharge.
Results
Patient cohort characteristics
Fifty patients with multiple myeloma underwent two AHCT performed 2 or more years apart using HPC obtained by dividing a single mobilization and collection attempt into fractions with equivalent numbers of CD34+ cells. HPC used for the first transplant were stored for median 60 days (range, 17–165) and the cells used for the second transplantation were stored for median 1448 days (range, 849–3510). Although equivalent numbers of CD34+ cells were infused with each AHCT, due to weight loss nine patients received relatively higher doses with the second transplantation. The rest maintained or increased their weight, so identical or lower CD34+ cell doses per kilogram of their body weight were administered with the second AHCT in 41 patients. The average CD34+ cell dose at the first AHCT was 3.12 × 106/kg while at the second AHCT the dose was 2.99 × 106/kg. The dose of melphalan given at both AHCT was the same in 22 patients and 28 patients received a lower dose at the second transplant. The remission status was better at the first transplant in 10 patients, worse in 13 patients and equivalent in 27 patients. Details of patients’ and transplant characteristics are summarized in Table 1.
Outcomes
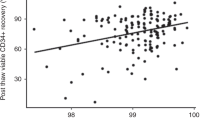
In 39 patients, neutrophil engraftment at second AHCT was achieved at same day or faster than at the first AHCT. In 11 patients, neutrophil recovery occurred later after the second AHCT than after the first AHCT (Figure 1). For the first transplant, the mean time to neutrophil recovery was 14 days (range, 11–21) and for the second transplant this was 13 days (range, 10–20). Although a paired t-test analysis showed a statistically significant difference (P=0.006) favoring neutrophil recovery in the second AHCT, the median time to neutrophil recovery was within the acceptable range for both transplants and the 1-day difference between both AHCT was considered not clinically significant. None of the variables examined in the linear regression analysis were associated with the difference in the time to neutrophil recovery.
Differences between time to neutrophil recovery after first and second autologous transplantation. In only 11 of 50 patients, autografted for myeloma twice, at least 2 years apart using HPC from the same collection, there was a longer time to neutrophil recovery after the second transplantation (dots below 0). The time to neutrophil recovery was identical in nine patients (dots at 0) and faster with second transplant in 30 patients (dots above 0).
Forty-seven patients were evaluable in the comparison of time to platelet recovery; two patients maintained a platelet count >20 × 109/L throughout the first AHCT, and another patient died while still receiving prophylactic transfusion during the second AHCT. The median times to platelet recovery were identical after first and second AHCT at 16 days (range, 8–23).
Discussion
Current quality methods to validate cryopreserved HPC viability, such as colony-forming units and post-thaw CD34+ counts still generate concern in the transplant setting as they are unable to fully guarantee in vivo functionality.7 Consequently, new ideas aimed to monitor quality assurance are in continuous demand.
We have compared neutrophil recovery in myeloma patients who underwent two autologous transplants using short-term or long-term stored cryopreserved HPCs from the same collection and our data suggest that the potency of HPC was not reduced after long-term storage in our institution.
The design of this study eliminated a number of important variables influencing hematopoietic recovery related to HPC mobilization, harvest, processing and freezing as this was identical for the both first and second transplants enabling us to concentrate on the actual length of product storage. We also made maximal effort to make adjustments for potentially important clinical variables capable of influencing the time to hematopoietic recovery, namely loss of patient body weight leading to relatively higher CD34 dose, reduction of melphalan dose or more remission status, so the observed difference is not biased.4, 5, 6
Further studies are needed to clarify whether the shorter engraftment with longer storage is related to biological changes during storage. However, these data are reassuring as they indicate that long storage of hematopoietic cells does not negatively impact on neutrophil and platelet engraftment in AHCT provided that strict quality assurance measures are in place. Such quality measures are paramount as there is no other method capable reliably assessing cell viability after cryopreservation.7, 8, 9
References
Park B, Yoo KH, Kim C . Hematopoietic stem cell expansion and generation: the ways to make a breakthrough. Blood Res 2015; 50: 194–203.
Cook G, Liakopoulou E, Pearce R, Cavet J, Morgan GJ, Kirkland K et al. Factors influencing the outcome of a second autologous stem cell transplant (ASCT) in relapsed multiple myeloma: a study from the British Society of Blood and Marrow Transplantation Registry. Biol Blood Marrow Transplant 2011; 17: 1638–1645.
FACT-JACIE International Standards for hematopoietic cellular therapy product collection, processing, and administration. http://www.jacie.org/standards/6th-edition-2015.
Palumbo A, Cavallo F, Gay F, Di Raimondo F, Ben Yehuda D, Petrucci MT et al. Autologous transplantation and maintenance therapy in multiple myeloma. N Engl J Med 2014; 371: 895–905.
Moreau P, Attal M, Facon T . Frontline therapy of multiple myeloma. Blood 2015; 125: 3076–3084.
Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K et al. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med 2003; 348: 1875–1883.
Morgenstern DA, Ahsan G, Brocklesby M, Ings S, Balsa C, Veys P et al. Post-thaw viability of cryopreserved peripheral blood stem cells (PBSC) does not guarantee functional activity: important implications for quality assurance of stem cell transplant programmes. Br J Haematol 2016; 174: 942–951.
Aird W, Labopin M, Gorin NC, Antin JH . Long-term cryopreservation of human stem cells. Bone Marrow Transplant 1992; 9: 487–490.
Berz D, McCormack EM, Winer ES, Colvin GA, Quesenberry PJ . Cryopreservation of hematopoietic stem cells. Am J Hematol 2007; 82: 463–472.
Acknowledgements
This research was not directly funded. All authors are supported by the National Institute for Health Research Biomedical Research Centre based at Imperial College Healthcare NHS Trust and Imperial College London. Authors are grateful to all the clinical, laboratory and administrative staff, and also to all the patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pavlů, J., Auner, H., Szydlo, R. et al. Analysis of hematopoietic recovery after autologous transplantation as method of quality control for long-term progenitor cell cryopreservation. Bone Marrow Transplant 52, 1599–1601 (2017). https://doi.org/10.1038/bmt.2017.113
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2017.113
- Springer Nature Limited