Abstract
Intensive care unit (ICU) admission is associated with high mortality in allogeneic hematopoietic stem cell transplant (HSCT) recipients. Whether mortality has decreased recently is unknown. The 497 adult allogeneic HSCT recipients admitted to three ICUs between 1997 and 2011 were evaluated retrospectively. Two hundred and nine patients admitted between 1997 and 2003 were compared with the 288 patients admitted from 2004 to 2011. Factors associated with 90-day mortality were identified. The recent cohort was characterized by older age, lower conditioning intensity, and greater use of peripheral blood or unrelated-donor graft. In the recent cohort, ICU was used more often for patients in hematological remission (67% vs 44%; P<0.0001) and without GVHD (73% vs 48%; P<0.0001) or invasive fungal infection (85% vs 73%; P=0.0003) despite a stable admission rate (21.7%). These changes were associated with significantly better 90-day survival (49% vs 31%). Independent predictors of hospital mortality were GVHD, mechanical ventilation (MV) and renal replacement therapy (RRT). Among patients who required MV or RRT, survival was 29% and 18%, respectively, but dropped to 18% and 6% in those with GVHD. The use of ICU admission has changed and translated into improved survival, but advanced life support in patients with GVHD usually provides no benefits.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is increasingly used for the treatment of malignant and nonmalignant hematologic diseases.1 In many situations, HSCT is considered to be more effective than chemotherapy for preventing a relapse or achieving a cure. HSCT is now the standard of care for numerous diseases including high-risk acute leukemia,2 myelodysplastic syndromes3 and aplastic anemia.4 HSCT is gaining ground as a salvage procedure for hematologic malignancies that respond poorly to chemotherapy.5 Nevertheless, HSCT is associated with numerous and potentially life-threatening adverse events including opportunistic infections,6 conditioning-regimen toxicity, GVHD7 and relapse. Thus, 15–20% of HSCT recipients require intensive care unit (ICU) admission.8, 9
Several studies suggest that ICU admission of allogeneic HSCT recipients may fail to provide benefits. Hospital mortality was as high as 95% among HSCT recipients who required invasive life-sustaining interventions.10, 11, 12, 13 However, these data remain controversial,8 as they come chiefly from small single-center retrospective studies with a mix of autologous and allogeneic HSCT recipients. In a large cohort of allogeneic HSCT recipients with life-threatening complications, we showed that ICU admission was beneficial in a subset of patients but that outcomes were dismal in patients who required invasive mechanical ventilation (MV), exhibited severe acute GVHD, or were admitted to the ICU for >30 days post transplantation.9
Recent reports point to changes in HSCT procedures.14 Conditioning regimens are less toxic and the incidence of GVHD has decreased. Various cell sources are used, and the indications and age range for HSCT have been expanded.15 Moreover, advances in the management of critically ill HSCT recipients have been achieved.16 Earlier and less-invasive management has proved more effective in this population.17, 18, 19 Finally, ICU triage policies have shifted toward the admission of patients who have the best chances of recovering from life-threatening complications. For instance, patients with uncontrolled GVHD and/or refractory malignant disease are now deemed poor candidates for ICU admission.
Whether these changes in HSCT procedures and in ICU admission and management have affected the outcomes of HSCT recipients with life-threatening complications is unknown. Should these changes be associated with decreased mortality, a reappraisal of the determinants of mortality and of admission policies would be warranted.
We therefore performed a multicenter study to assess the impact of recent changes on hospital mortality of HSCT recipients admitted to the ICU. We compared two cohorts, one studied previously and composed of patients admitted to the ICU in 1997–2003 and the other established for this study and composed of patients admitted to the ICU in 2004–2011.
Patients and methods
Patients
Consecutive adults (>16 years) admitted over a 14-year period (1997–2011) to the ICUs of three tertiary-care centers specialized in managing HSCT patients (Saint-Louis Hospital, Paris; Cochin Hospital, Paris and Gustave Roussy Institute, Villejuif, all in France) were included if they had received allogeneic HSCT. We separated the patients admitted between January 1997 and December 2003, who had been included in an earlier study,9 from the patients admitted between January 2004 and August 2011. Before transplant, all patients provided both written HSCT procedure consent and anonymous data-recording consent, in accordance with the Declaration of Helsinki, after receiving full information about benefits and risks (including GVHD, organ failure and death) of the procedure.
HSCT procedures
The stem cells were mobilized peripheral blood cells, bone marrow cells or cord-blood cells. Various conditioning regimens were used. Myeloablative conditioning regimens included either high-dose BU (>8 mg/Kg orally or i.v. equivalent) or high-dose total body irradiation (⩾8 Gy fractionated dose), both combined with CHOP. Regimens not meeting these criteria were classified as reduced-intensity conditioning.20 All patients received GVHD prophylaxis with CsA plus MTX or CsA plus mycophenolate mofetil or CsA alone according to local guidelines that were afterwards stated by international recommendations.21 Methylprednisolone (>1 mg/Kg/day) was introduced promptly as first-line treatment in case of acute GVHD symptoms. Second-line treatments varied across centers and study periods.
ICU admission policy
In all three centers, the transplant team determined HSCT indications and chose conditioning regimens and GVHD prophylaxis according to guidelines. In patients with life-threatening complications, the hematologists and intensivists in charge of the patient decided together whether to admit the patient to the ICU, at the time of clinical deterioration or prophylactically. In all three centers, hematologists and intensivists were on site 24/7.
Reasons for ICU admission were recorded on the basis of main symptoms at ICU admission. Acute respiratory failure was defined as oxygen saturation <90% or PaO2 <60 mm Hg on room air combined with severe dyspnea at rest with an inability to speak in sentences or a respiratory rate >30 breaths/min or clinical signs of respiratory distress.17 Shock was defined as previously reported.22 Life-supporting interventions, antimicrobial agents, prophylactic treatments and diagnostic procedures were administered at the discretion of the attending intensivists, who followed best clinical practice and guidelines. Successful noninvasive ventilation (NIV) was defined as NIV not followed by MV. Corticosteroids, hematopoietic growth factors, immunosuppressive drugs and other cancer-related treatments were prescribed by the hematologist in charge of each patient in accordance with institutional guidelines. Neutropenia was defined as a neutrophil count <0.5 Giga/L. Invasive aspergillosis was defined according to EORTC/MSG guidelines.23
Data collection
The data were extracted from the medical charts. The ICU admission date was used to compute survival lengths and outcomes. Disease stages were defined according to international guidelines as remission, progression or chronic phase. We considered only cases of acute GVHD that met all published criteria and were greater than grade 2.24 Histological documentation was available in the vast majority of cases. MV was not considered if used for a scheduled procedure. In patients with multiple ICU admissions, only the first admission after HSCT was analyzed.
Statistical analysis
The data were described as percentage for discrete variables and median (interquartile range) for continuous variables. Fisher’s exact test and Wilcoxon’s nonparametric rank sum test, respectively, were used to compare these two types of variables. ICU survival was determined on the basis of a nonparametric estimate of the cumulative incidence function, considering ICU discharge as an event competing with death during the ICU stay. Gray’s test was used to compare cumulative incidence functions.
Kaplan–Meier plots were constructed to estimate 90-day survival. Cox regression models were used to identify factors associated with death within 90 days in the recent cohort. All parameters significantly associated with 90-day survival with P<0.05 by univariate analyses were included in the multivariate Cox regression model.
All statistical tests were two-sided, with P-values ⩽0.05 indicating statistical significance. Statistical analyses were performed using SAS 9.3 (SAS Inc., Cary, NC, USA) and R 2.14.0 (http://www.R-project.org/) packages.
Results
Over the study period, 2286 allogeneic HSCT procedures were performed in the three centers. ICU admission rates were 22.8% and 20.4% in the recent and early periods, respectively (P=0.17) (Figure 1).
HSCT procedures
Throughout the study period, 497 HSCT recipients were admitted to the ICUs in the three centers (Saint-Louis: 213; IGR: 185; and Cochin, 99), including 209 patients in 1997–2003 and 288 in 2004–2011. HSCT techniques (Table 1) changed over the study period, becoming more heterogeneous as a result of tailoring to patient age and comorbidities, whereas previously sibling-donor bone marrow transplantation preceded by myeloablative conditioning was the standard method. In the recent cohort, HSCT recipients were older (48 vs 41 years, P<0.0001), a finding probably relevant to the greater use of reduced-intensity conditioning in recent years (Supplementary Figure 1). In the recent cohort, significantly fewer patients underwent HSCT for CML and significantly more patients received HSCT for mature lymphoid malignancies and myelodysplastic syndromes. This translated into an increase in the time from diagnosis to HSCT in the recent period (16 (6–48) vs 12 months (6–26), P=0.008). The median European Group for Blood and Marrow Transplantation risk score was 3 (2–5) in the recent cohort.
HSCT characteristics at ICU admission
Table 2 shows patient characteristics at ICU admission and management according to study period. In patients not admitted directly to the ICU, admission occurred 19 days after hospital admission with no differences across admission periods (19 (7–33) vs 19.5 (6–30) days). ICU admission occurred for >30 days after HSCT in 37% and 33% of the recent and early cohort patients, respectively (P=0.28). Implementation of recent triage policies6, 9, 25 was illustrated by significant reductions in the proportions of patients admitted with severe acute GVHD grade 3–4, high-dose steroid treatment or uncontrolled hematological disease or fungal infection (Table 2).
In the recent cohort, ICU admission was more frequently used for patients who required intensive monitoring (10% vs 2%), whereas severe kidney injury at ICU admission was significantly less common. These changes translated into a decrease in organ dysfunctions in the recent cohort, with a SOFA score at ICU admission of 7 (4.25–9) vs 8 (5–11) in the early cohort, whereas overall severity measured by the SAPSII remained stable (42 (33–56) vs 41 v30–57); P=0.49). NIV was more often successful in the recent cohort (51 vs 33%; P=0.03) MV duration was shorter, suggesting benefits from earlier ICU admission and faster initiation of life-sustaining treatments. Coma was a stable purpose of admission and accounted for 29 (10%) patients, whereas altered mental status was present in 58 (20%) mostly in combination to hypoxemia or septic shock.
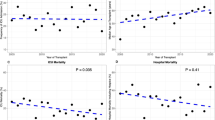
Hospital survival
Table 2 shows the main outcomes according to study period. Hospital mortality was significantly lower in the recent cohort in all three centers and the decrease was greatest in the subgroup requiring MV (3-month mortality after MV, 70% vs 84% in the early cohort) (Figure 2) or vasoactive drugs. Nearly all patients managed with renal replacement therapy (RRT) died in both cohorts. Mortality did not decrease over time in the subset of patients managed without life-sustaining interventions. MV use in patients with GVHD grade 3–4 was associated with high day-90 mortality rates in the recent and early cohorts (82% and 85%, respectively) (Figure 2). Only three patients mechanically ventilated with acute GVHD grade 3–4 remain long-time survivors in the recent cohort (91% OS rate).
The main causes of death in the recent cohort were infections (30.6%), malignancy relapse (12.6%), other defined noninfectious complications (35.7%), including veno-occlusive disease in 5% and thrombotic microangiopathy in 3.5%, and organ failures of unknown cause (13%). Treatment-limitation decisions were implemented in 47% and 12% of patients who died in the recent and early cohorts, respectively (P<0.0001).
Independent predictors of hospital mortality
In the univariate analysis of day-90 mortality in the 2004–2011 cohort (Supplementary Table 1), demographic parameters, HSCT modalities and neutropenia had no influence on the risk of death. GVHD grade 3–4 and number of organ dysfunctions at ICU admission were the main determinants of mortality. The risk of death was increased twofold in the small subset of patients admitted with CMV reactivation or invasive fungal infections other than invasive aspergillosis. However, hazard ratio of day-90 mortality did not changed significantly between the two periods for patients with invasive aspergillosis (Supplementary Table 2).
As there were no major differences in patient’s characteristics with the early cohort, we looked for interactions between period and effects of all covariates on risk of death. Acute respiratory failure, acute renal failure and CMV reactivation had a greater impact on the risk of death in the recent cohort (Supplementary Table 3).
In the multivariate analysis of day-90 mortality in the 2004–2011 cohort, three variables independently predicted death, namely, RRT, MV and GVHD grade 3–4 (Table 3).
Discussion
The survival of HSCT recipients admitted to the ICU has improved in recent years. Although the proportion of HSCT recipients admitted to the ICU has remained unchanged, modifications in HSCT practices and changes in ICU triage have decreased the ICU admission of patients with refractory malignancies, uncontrolled GVHD or invasive fungal infections. Earlier ICU admission in recent years has increased the use of NIV. Finally, most patients with acute GVHD who required MV died.
The characteristics of HSCT recipients admitted to the ICU and those of the overall HSCT recipient population have changed in several ways over time and we thus decided not to confine our analysis to a homogeneous subgroup of patients in order account for these changes. In the early cohort, myeloablative conditioning was used in the vast majority of the patients, who therefore had a period of profound neutropenia associated with a high risk of bacterial or fungal sepsis.9 in the past, the time from HSCT to ICU admission predicted recovery from the critical illness in parallel with neutrophil count restoration. Now, however, reduced-intensity conditioning is widely used in HSCT centers, as documented by many cohort studies,26, 27 and time to ICU admission is no longer a relevant predictor. The use of peripheral blood stem cells and unrelated donors has been reported to increase the rate of chronic and acute GVHD, respectively.28, 29 However, these two modalities had no influence on mortality in our study, perhaps as a result of our ICU admission policies, acute GVHD grade 3–4 remains the strongest predictor by far of post-ICU survival in patients requiring life-sustaining interventions. In several cohorts of allogeneic HSCT recipients, nearly all severe GVHD patients who were given MV died.8, 30, 31, 32, 33, 34 Steroid sensitivity over time and the active or remission status of GVHD at ICU admission are crucial factors but are rarely assessed. Whether these factors may explain the improved survival in our recent cohort is unknown. Also, biological data are lacking to explain the detrimental interaction between GVHD and >90% mortality after life-sustaining interventions.
Our study provides information about the role for concomitant infection. CMV reactivation is associated with direct organ toxicities35 and with treatment-related BM and kidney damage. Moreover, it is a surrogate for the underlying immunosuppression and has consistently been reported to affect outcomes of allogeneic HSCT recipients, as well as of all ICU patients with immunosuppression-related acute illnesses.36, 37 Finally, invasive aspergillosis is not associated with impaired outcomes presumably owing to the widespread use of active antifungal therapies, whereas other invasive fungal infections still remain of adverse prognostic significance.38
A possible explanation for the improved survival in our recent cohort is ICU admission at an earlier phase of organ dysfunction. ICU admission with one or no organ failure is associated with better performance of therapeutic and diagnostic procedures.16, 17 Although organ dysfunction severity was not significantly different between our two cohorts, patients in the recent cohort more often received one or no life-sustaining interventions (65% vs 55%), probably as a result of earlier admission. Earlier, NIV initiation increases the success rate of this intervention.39 Survival did not increase among patients who required RRT. Many factors can cause kidney damage, which is extremely common and affects the prognosis in HSCT recipients.40, 41 In both cohorts, 95% of patients managed with RRT died after a median of <2 weeks after ICU admission. In the vast majority of these patients, renal failure was associated with sepsis at the terminal stage of multiple organ failure.
The main finding from our study is that allogeneic HSCT recipients fall into two categories. Patients admitted without severe GVHD and before the development of multiple organ failure should be considered for full-code ICU management regardless of their transplant characteristics, as their chances of survival are similar to those of other patients with immunosuppression. On the other hand, patients with uncontrolled GVHD, or refractory hematological disease still have dismal outcomes after ICU admission and should therefore be offered high-quality palliative care without invasive procedures. Very few data are available about treatment-limitation decisions for HSCT recipients, and the factors that determine the intensity of care in this population are unknown. The increase in the observed treatment-limitation decisions may have been the result of an increasing proportion of patients admitted for an ICU trial.25 Indeed, it was shown already that the evolution after few days of organ failures number was a robust prognosticator of short-term survival and thus futile prolonged ICU stay in these patients.
Our study has several limitations. We compared a recent cohort with a historical cohort included in an earlier study by our group, and the data for both cohorts were collected retrospectively. This study design allowed us to detect changes between the two time periods but provided no information on the reasons for those changes. Implementation of ICU admission policy guidelines should be a priority for transplantations center to help clinicians to deal with this decision and a prospective evaluation of such implementation will surely help us to better discriminate the areas of further advances needs. One possible reason for an improvement in survival is a decrease in the severity of the acute illness or underlying hematological disease. Acute illness severity was similar during the two periods, however, as shown by the organ dysfunctions; SAPSII; and use of MV, vasoactive drugs and RRT. All three centers are specialized in HSCT, and their ICUs and intensivists have considerable experience with HSCT recipients. Case volume affects the outcomes of these patients,42 and our findings may therefore have limited applicability to less experienced centers. However, allogeneic HSCT is a highly sophisticated treatment that should be delivered in specialized centers with specialized ICUs.
In summary, although HSCT procedures have changed over time, MV in patients with severe GVHD remains associated with dismal survival rates. In contrast, full-code ICU management should be offered to other critically ill HSCT recipients, as their survival rates have improved. Hematologists and intensivists should continue to work to build formal recommendations regarding appropriate care intensity for allogeneic HSCT recipients with critical illnesses. Such guidelines would also help clinicians provide clear information to their patients.
References
Gratwohl A, Baldomero H, Gratwohl M, Aljurf M, Bouzas LF, Horowitz M et al. Quantitative and qualitative differences in use and trends of hematopoietic stem cell transplantation: a Global Observational Study. Haematologica 2013; 98: 1282–1290.
Goldstone AH, Richards SM, Lazarus HM, Tallman MS, Buck G, Fielding AK et al. In adults with standard-risk acute lymphoblastic leukemia, the greatest benefit is achieved from a matched sibling allogeneic transplantation in first complete remission, and an autologous transplantation is less effective than conventional consolidation/maintenance chemotherapy in all patients: final results of the International ALL Trial (MRC UKALL XII/ECOG E2993). Blood 2008; 111: 1827–1833.
Chang C, Storer BE, Scott BL, Bryant EM, Shulman HM, Flowers ME et al. Hematopoietic cell transplantation in patients with myelodysplastic syndrome or acute myeloid leukemia arising from myelodysplastic syndrome: similar outcomes in patients with de novo disease and disease following prior therapy or antecedent hematologic disorders. Blood 2007; 110: 1379–1387.
Scheinberg P, Young NS . How I treat acquired aplastic anemia. Blood 2012; 120: 1185–1196.
Carella AM, Cavaliere M, Lerma E, Ferrara R, Tedeschi L, Romanelli A et al. Autografting followed by nonmyeloablative immunosuppressive chemotherapy and allogeneic peripheral-blood hematopoietic stem-cell transplantation as treatment of resistant Hodgkin’s disease and non-Hodgkin’s lymphoma. J Clin Oncol 2000; 18: 3918–3924.
Upton A, Kirby KA, Carpenter P, Boeckh M, Marr KA . Invasive aspergillosis following hematopoietic cell transplantation: outcomes and prognostic factors associated with mortality. Clin Infect Dis 2007; 44: 531–540.
Socié G, Blazar BR . Acute graft-versus-host disease: from the bench to the bedside. Blood 2009; 114: 4327–4336.
Afessa B, Azoulay E . Critical care of the hematopoietic stem cell transplant recipient. Crit Care Clin 2010; 26: 133–150.
Pène F, Aubron C, Azoulay E, Blot F, Thiéry G, Raynard B et al. Outcome of critically ill allogeneic hematopoietic stem-cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol 2006; 24: 643–649.
Soubani AO, Kseibi E, Bander JJ, Klein JL, Khanchandani G, Ahmed HP et al. Outcome and prognostic factors of hematopoietic stem cell transplantation recipients admitted to a medical ICU. Chest 2004; 126: 1604–1611.
Afessa B, Tefferi A, Dunn WF, Litzow MR, Peters SG . Intensive care unit support and Acute Physiology and Chronic Health Evaluation III performance in hematopoietic stem cell transplant recipients. Crit Care Med 2003; 31: 1715–1721.
Price KJ, Thall PF, Kish SK, Shannon VR, Andersson BS . Prognostic indicators for blood and marrow transplant patients admitted to an intensive care unit. Am J Respir Crit Care Med 1998; 158: 876–884.
Groeger JS, Lemeshow S, Price K, Nierman DM, White P Jr, Klar J et al. Multicenter outcome study of cancer patients admitted to the intensive care unit: a probability of mortality model. J Clin Oncol 1998; 16: 761–770.
Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med 2010; 363: 2091–2101.
Bayraktar UD, Shpall EJ, Liu P, Ciurea SO, Rondon G, de Lima M et al. Hematopoietic cell transplantation-specific comorbidity index predicts inpatient mortality and survival in patients who received allogeneic transplantation admitted to the intensive care unit. J Clin Oncol 2013; 31: 4207–4214.
Azoulay E, Mokart D, Pène F, Lambert J, Kouatchet A, Mayaux J et al. Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium—a groupe de recherche respiratoire en réanimation onco-hématologique study. J Clin Oncol 2013; 31: 2810–2818.
Azoulay E, Mokart D, Lambert J, Lemiale V, Rabbat A, Kouatchet A et al. Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med 2010; 182: 1038–1046.
Lengliné E, Raffoux E, Lemiale V, Darmon M, Canet E, Boissel N et al. Intensive care unit management of patients with newly diagnosed acute myeloid leukemia with no organ failure. Leuk Lymphoma 2012; 53: 1352–1359.
Azoulay E, Soares M, Darmon M, Benoit D, Pastores S, Afessa B . Intensive care of the cancer patient: recent achievements and remaining challenges. Ann Intensive Care 2011; 1: 5.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant 2009; 15: 1628–1633.
Ruutu T, Gratwohl A, de Witte T, Afanasyev B, Apperley J, Bacigalupo A et al. Prophylaxis and treatment of GVHD: EBMT-ELN working group recommendations for a standardized practice. Bone Marrow Transplant 2014; 49: 168–173.
Legrand M, Max A, Peigne V, Mariotte E, Canet E, Debrumetz A et al. Survival in neutropenic patients with severe sepsis or septic shock. Crit Care Med 2012; 40: 43–49.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 2008; 46: 1813–1821.
Rowlings PA, Przepiorka D, Klein JP, Gale RP, Passweg JR, Henslee-Downey PJ et al. IBMTR Severity Index for grading acute graft-versus-host disease: retrospective comparison with Glucksberg grade. Br J Haematol 1997; 97: 855–864.
Lecuyer L, Chevret S, Thiery G, Darmon M, Schlemmer B, Azoulay E . The ICU trial: a new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med 2007; 35: 808–814.
Pasquini MC, Wang Z, Horowitz MM, Gale RP . 2010 report from the Center for International Blood and Marrow Transplant Research (CIBMTR): current uses and outcomes of hematopoietic cell transplants for blood and bone marrow disorders. Clin Transpl 2010, 87–105.
Passweg JR, Baldomero H, Bregni M, Cesaro S, Dreger P, Duarte RF et al. Hematopoietic SCT in Europe: data and trends in 2011. Bone Marrow Transplant 2013; 48: 1161–1167.
Kawase T, Morishima Y, Matsuo K, Kashiwase K, Inoko H, Saji H et al. High-risk HLA allele mismatch combinations responsible for severe acute graft-versus-host disease and implication for its molecular mechanism. Blood 2007; 110: 2235–2241.
Anasetti C, Logan BR, Lee SJ, Waller EK, Weisdorf DJ, Wingard JR et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med 2012; 367: 1487–1496.
Afessa B, Tefferi A, Hoagland HC, Letendre L, Peters SG . Outcome of recipients of bone marrow transplants who require intensive-care unit support. Mayo Clin Proc 1992; 67: 117–122.
Benz R, Schanz U, Maggiorini M, Seebach JD, Stussi G . Risk factors for ICU admission and ICU survival after allogeneic hematopoietic SCT. Bone Marrow Transplant 2014; 49: 62–65.
Depuydt P, Kerre T, Noens L, Nollet J, Offner F, Decruyenaere J et al. Outcome in critically ill patients with allogeneic BM or peripheral haematopoietic SCT: a single-centre experience. Bone Marrow Transplant 2011; 46: 1186–1191.
Gilli K, Remberger M, Hjelmqvist H, Ringden O, Mattsson J . Sequential Organ Failure Assessment predicts the outcome of SCT recipients admitted to intensive care unit. Bone Marrow Transplant 2010; 45: 682–688.
Scales DC, Thiruchelvam D, Kiss A, Sibbald WJ, Redelmeier DA . Intensive care outcomes in bone marrow transplant recipients: a population-based cohort analysis. Crit Care 2008; 12: R77.
Moins-Teisserenc H, Busson M, Scieux C, Bajzik V, Cayuela J-M, Clave E et al. Patterns of cytomegalovirus reactivation are associated with distinct evolutive profiles of immune reconstitution after allogeneic hematopoietic stem cell transplantation. J Infect Dis 2008; 198: 818–826.
Heininger A, Haeberle H, Fischer I, Beck R, Riessen R, Rohde F et al. Cytomegalovirus reactivation and associated outcome of critically ill patients with severe sepsis. Crit Care 2011; 15: R77.
Limaye AP, Kirby KA, Rubenfeld GD, Leisenring WM, Bulger EM, Neff MJ et al. Cytomegalovirus reactivation in critically ill immunocompetent patients. JAMA 2008; 300: 413–422.
Burghi G, Lemiale V, Seguin A, Lambert J, Lacroix C, Canet E et al. Outcomes of mechanically ventilated hematology patients with invasive pulmonary aspergillosis. Intensive Care Med 2011; 37: 1605–1612.
Adda M, Coquet I, Darmon M, Thiery G, Schlemmer B, Azoulay E . Predictors of noninvasive ventilation failure in patients with hematologic malignancy and acute respiratory failure. Crit Care Med 2008; 36: 2766–2772.
Singh N, McNeely J, Parikh S, Bhinder A, Rovin BH, Shidham G . Kidney complications of hematopoietic stem cell transplantation. Am J Kidney Dis 2013; 61: 809–821.
Canet E, Lengline E, Zafrani L, Peraldi M-N, Socié G, Azoulay E . Acute Kidney Injury in critically ill Allo-HSCT recipients. Bone Marrow Transplant 2014; 49: 1121–1122.
Zuber B, Tran T-C, Aegerter P, Grimaldi D, Charpentier J, Guidet B et al. Impact of case volume on survival of septic shock in patients with malignancies. Crit Care Med 2012; 40: 55–62.
Acknowledgements
This work was supported by the Groupe de Recherche en Réanimation Oncohématologique (Grrr-OH).
Author Contributions
EA coordinated the research; EL, ASM, FP and FB collected and assembled the data; SC performed the statistical analysis; all authors analyzed the data and approved the final manuscript. EL and EA wrote the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Bone Marrow Transplantation website
Supplementary information
Rights and permissions
About this article
Cite this article
Lengliné, E., Chevret, S., Moreau, AS. et al. Changes in intensive care for allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant 50, 840–845 (2015). https://doi.org/10.1038/bmt.2015.55
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2015.55
- Springer Nature Limited
This article is cited by
-
AKI treated with kidney replacement therapy in critically Ill allogeneic hematopoietic stem cell transplant recipients
Bone Marrow Transplantation (2024)
-
Impact of pre-transplant individual comorbidities on risk of ICU admission and survival outcomes following allogeneic hematopoietic stem cell transplantation
Bone Marrow Transplantation (2023)
-
Impact of chronic graft-versus-host-disease on intensive care outcome in allogeneic hematopoietic stem cell recipients
Bone Marrow Transplantation (2023)
-
Allogeneic stem cell transplant recipients admitted to the intensive care unit during the peri-transplant period have unfavorable outcomes—results of a retrospective analysis from a German university hospital
Annals of Hematology (2022)
-
Clinical diagnostic accuracy of respiratory failure in critically ill hematopoietic stem cell transplant patients
International Journal of Hematology (2022)