Abstract
In this research, I examined the role of socioeconomic variations in the prevalence of stunting and underweight among children in Ethiopia. The study aimed to identify key health factors contributing to these disparities in child malnutrition by utilizing concentration indices, concentration curves, and regression-based decomposition analysis. Despite a notable decline in the average rates of stunting and underweight prevalence, the relative and absolute gaps between different demographic and socioeconomic groups have widened in Ethiopia. The empirical analysis revealed that higher levels of maternal education and household wealth significantly benefited children from better socioeconomic backgrounds, making them less likely to experience malnutrition. The disparity in socioeconomic status is the primary driver of inequalities in child malnutrition. The findings suggest that to reduce these disparities, national health policies should focus on promoting maternal literacy and targeting interventions for underprivileged groups.
Key messages
Children from higher socioeconomic backgrounds and mothers' educational levels were less likely to suffer from malnutrition. The disparity in socioeconomic positions is the major cause behind child malnutrition inequities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Access to adequate nutrition is crucial during childhood to grow in good physical shape [66], strengthen the immune system [13, 37, 65], minimize risk to NCDs [11, 38, 44], and appropriate cognitive development [9, 24, 66] at a later age. Healthy children perform better in their education than those who are not [6, 25]. Generally, individuals with sufficient nutrition are more productive with the potential effect to eventually overcome the cycle of poverty. On the other hand, inadequate nutrition increases the likelihood of being ill, and low performance and protects them from fulfilling their potential at later ages [64].
Evidence showed that health outcomes and access to services are not evenly dispersed among different population groups in developing countries. for instance: The mortality rate is higher, and the coverage of health services is lower for those children who are from socio-economically disadvantaged parents than their counterparts [32, 68]. The most used indicators of child health include child malnutrition and child mortality.
Malnutrition is a universal problem [7] that affects everyone at all age levels [33]. However, it would be ideal to pay attention to those who are generally victims and vulnerable groups. Children in developing countries do not have enough food to eat and others who have food, eat unhealthy with lesser micronutrient content. As a result, [10, 26, 40, 53] have mentioned the situation as many children are surviving but by far not thriving. Those children who do not get the necessary nutrients will not grow properly and eventually will tend to be victims of the triple burdens of malnutrition [54] which are undernutrition, hidden hunger, and overweight including obesity.
Child malnutrition is one of the challenging health phenomena these days affecting millions of children aged five years and younger [46, 54]. Though it seems to be there exist very significant progress in the percentage of malnourished children, the number is still huge. The prevalence of child under-nutrition remains disturbing with very slow decreases in stunting prevalence and many children are affected by wasting and other forms of malnutrition [55]. For instance: According to the joint UN, WHO, and WB estimates, there were about 144 million (21.3%) and 47 million (6.9%) children who were stunted and wasted respectively in 2019. Furthermore, malnutrition is among the major causes of child mortality in developing countries [2, 4, 15]. Being able to know the major causes of under-five children’s death is important for designing relevant and protective policies, as well as prioritizing interventions.
There were substantial drop-offs in child mortality and malnutrition during the MDGs. However, those improvements (drop-offs in mortality and malnutrition) are not evenly distributed [5, 21, 56] among various socioeconomic groups. The poor countries experiencing high and persistent disparities in child health [10, 21, 29] are measured by different indicators (including mortality and malnutrition variables). For instance: Asia and Africa are mainly home to all forms of malnutrition making them the most suffering continents. 54% and 40% of under-five children who are stunted globally are from Asia and Africa respectively. Similarly, two out of three wasted under-five children live in Asia, and above one-fourth of the globally wasted children are from Africa. Both Asia and Africa account for about 94% of the stunted and 96% of the globally wasted under-five children. The regional differences are clear to identify.
On top of that, The joint UN, WHO, and WB estimates [55] showed that there were disparities in the reduction level of the prevalence of malnutrition indicators in the past two decades. For instance: In 2000, the stunting prevalence was 37.9% in Africa, 37.8% in Asia (exclusive of Japan), and 38.4% in Oceania without Australia and New Zealand. Stunting prevalence declined to 29.1% in Africa, 21.8% in Asia, and 37% in Oceania in 2019 showing that some regions registered substantial improvement while others remain stagnant on the reduction of the prevalence. Therefore, emphasizing the disparities that exist across different countries and within countries is commendable. Therefore, continued effort must be excreted to maintain a reduction in the inequalities of child health outcomes [12]. Despite those improvements, it looks unlikely that the goals of SDGs will be achieved by 2030.Footnote 1
As Ethiopia is a poor country, the level and trend of child malnutrition prevalence are not different. In Ethiopia, malnutrition is a significant issue and a key factor in determining the population’s health and nutrition. It is especially crucial for young children’s nutrition because they have acute iron deficiency and are consequently at a high risk of dying soon after delivery. For instance: stunning prevalence was significantly high in 2000 at 58% and declined to about 38% in 2016. Underweight prevalence for children under five in the same years was 41% and dropped to 24% [16, 17]. Even if the drop-offs are encouraging, there are about two out of five under-five children who were stunted and one in four children suffering from being underweight. Moreover, there exist differences among children across different groups. last but not least, it is worthy to consider the increasing urbanization rate with migration from rural to urban being the main reason as a result, it is not identified where the unfavorable child health outcomes are concentrated. This is because previously conducted research delivered mixed results about this. For instance, A study by [51] found that children in urban are less likely to be stunted and underweighted because they are better nourished than their counterparts. whereas a study by [28] revealed that due to higher poverty-led migration from rural to urban, urban health advantage is diminishing. Those migrated people live in informal settlements and slum areas making them vulnerable and exposed to ill health.
The general objective of this study is to assess the socioeconomic disparities in child malnutrition in Ethiopia. This will help health policymakers, to identify those groups of societies that need special emphasis and design a policy that aims at vanishing, if possible, otherwise minimizing those inequalities that are preventable or avoidable. This is because understanding the recent trends in child undernutrition disparities and the main determinants is crucial for policy decision-makers.
A preliminary analysis we conducted using data from DHS of Ethiopia revealed that there are significant improvements in the mean of stunting, underweight, and wasting prevalence. we then intended to study this in detail. Using the absolute gaps and relative ratios, there are parallel downward trending changes not diverging trends between the socio-economic and geographical groups of children. The child health indicators are all pro-individuals with higher socio-economic status. As a result, we are motivated to further develop our study on this contextual problem and forward our findings to any policy or program interventions. Scrutinizing the cases about child health inequality, in general, helps policymakers to understand a country’s socio-economic situation and sheds light on the quality of life of the population in the country. There are of course a few studies like [42, 50, 52] demonstrating the determinants that affect child malnutrition, however, negligible attempts are made to empirically investigate the determinants of the inequalities. Finally, to our best knowledge, this is the first research to study the socioeconomic-related disparities in childhood malnutrition in Ethiopia using the standard concentration index and decomposing the contribution of various determinants of health.
Our study addressed the following points. Firstly, we have attempted to see how the malnutrition variables behave or change between the sample periods and across different socioeconomic and demographic groups. This is mainly done using absolute and relative gap analysis. Secondly, we obtained the standard concentration index (to get the magnitude of the inequality), supplemented by the generalized concentration index, and followed by a concentration curve (to see if there exists inequality in health and understand where this inequality is concentrated). Thirdly, we then carried out a multivariate analysis (using LPM, Logit, and probit regressions) with stunting and underweight being explained by selected independent variables. Finally, Coefficients obtained from the multivariate analysis will further be used to decompose the contribution of the covariates to the inequality in health.
2 Data and methods
The DHS program collects, analyses, and publishes descriptive data on various health, nutrition, and population categories in most developing countries nationwide. For this study, demographic and Health Survey data of Ethiopia conducted in 2000 and 2016 were used. All surveys are population-based household surveys that are recognized as representative surveys. These surveys are conducted and administered by the Ethiopian Central Statistical Authority, which is supported by ICF and funded by USAID.
The Ethiopia DHS offers a thorough analysis of the nation’s population health, which may be used to inform health policy and assess its effectiveness. The survey’s ability to correctly identify patterns in health outcomes for specific populations, such as those with limited healthcare coverage or those who live in distant locations, is limited. The poll also has the limitation of only measuring those who are willing to participate, and this could lead to selection bias. Last but not least, since DHS surveys are conducted using face-to-face interviews, it is incapable of collecting information on specific health outcomes, such as mental health.
The Ethiopian DHS provides several advantages. The poll is done nationwide and includes a wide range of subjects, including family planning, nutrition, and mother and child health. Additionally, the survey gathers comprehensive data on socioeconomic factors including work and education. This helps in comprehending how these variables could impact health outcomes. Furthermore, the DHS is consistent and well-structured, which facilitates results comparison across geographical regions. In summary, in nations where routine vital registration data is unavailable, demographic and health surveys have become a popular means and are used as a source of data for researchers. Moreover, the Ethiopia DHS was successful in terms of its participatory nature in which many national and international actors were part of it. Local governments (like the Ministry of Health, Central Statistical Authority, Ethiopian Public Health Institute, and so on), and nongovernmental and international development partners (USAID, WB, WHO, and many others) have taken part in the survey series. In the following section, we have described both the outcome variable and selected explanatory variables and presented the method of analysis used.
2.1 Description of variables
The growth of children is highly affected by the nutritional status and health of the population in general. When a person does not eat enough to meet their nutritional demands, it is referred to as malnutrition or undernutrition. The terms” shortage and excess” or” imbalance of nutritional intake” are used to describe malnutrition. As a result, it encompasses undernutrition for dietary deficiencies and overweight or obesity for dietary excesses. Malnutrition can have a variety of negative effects on child health, including a higher risk of getting sick or dying [8, 63]. In line with this, a malnourished child will experience delayed mental development, poor school performance, and reduced intellectual capacity [18].
Malnutrition is the key to understanding the true link between economic status and health among children. The child malnutrition indicators include the prevalence of stunting (low height-for-age), underweight (low weight-for-age), wasting (low weight-for-height), and overweight (high weight-for-age) in children aged 5 years. In our study, we have used stunting and underweight prevalence as the proxies for our dependent variable, child health.
-
1.
Stunting: This is simply low height-for-age. The fact that stunting results from persistent illness, a prolonged period of nutrient deficiency, or inadequate food intake over a long period, is considered the more reliable proxy for child malnutrition. It is not as” sensitive” to a temporary food shortage as other indicators of child malnutrition. Therefore, this study will focus its analysis mainly on under-five malnutrition to empirically examine health disparities.
-
2.
Underweight: It is low weight-for-age. Genetics, inadequate uptake of nutrients, a lack of food intake (often a result of poverty), physical or mental disease, or an eating disorder can all contribute to being underweighted.
Information on the selected forms of malnutrition comes from the demographic and health surveys conducted with women aged 15–49 years (4 DHS reports,Footnote 2 mainly the early and latest surveys). Health status variables are examined in terms of various demographic and socioeconomic factors. Studies have shown that a mother’s educational level and household economic status index [3] are the most important factors that influence children’s health level. Following a comprehensive review of related literature, we have identified the following list of explanatory variables to study inequalities in child health in Ethiopia.
-
1.
Educational status of mother: The educational status of a mother plays a very important role in minimizing risks associated with the nutritional status of her children. It is perceived that educated mothers will have a higher tendency to use prenatal care during pregnancy [1] and antenatal care [14] after giving birth to a child. Following our comprehensive review of related studies that primarily investigated socioeconomic inequality in child malnutrition in different countries where DHS has used a source of data, the variable mothers’ educational status is employed as a dichotomous variable. Before making it dichotomous, we tried to use the categorical version of the variable (No education, elementary, secondary, or higher). However, we checked the pattern/distribution of the data and figured out that more than three-fourths of the observation is with ‘no education’. Therefore, decided to include the variable as a dichotomous variable. We also think that mothers’ education levels should be at least secondary school level to make a significant difference in the health of their children. It should go beyond reading proficiency and require good comprehension to improve a child’s nutritional status through adherence to advised feeding schedules, acquisition of health knowledge, and other factors. Therefore, the mother’s education variable is entered into the analysis as a dichotomous variable, where a value of one indicates that the mother has secondary and higher levels of education (mothers are considered educated) and a value of zero indicates that the child’s mother’s education level is elementary or lower (referred to as uneducated mothers).
-
2.
Household SES (Asset Index): It is acknowledged that all DHS programs have not collected data on household income levels or consumption expenditures, which are used as measures of household socioeconomic status. In situations where such information is lacking, the household wealth index is estimated using a Principal Component Analysis. There is no common consensus on the list of items to be used for estimating the wealth index using PCA. As an example, A study by [41] attempted to compare the SES distribution across cases using only housing characteristics, only access to utilities and infrastructure, only ownership of durable assets, and all three categories together and concluded that combining these three categories does not produce evidence of clumping and truncation. However, using these classifications separately has either a clumping problem or a truncation problem, or both. It is better to include any variable that may reflect the economic status of households so that the distribution of variables varies across households. This is because including a larger number of items in the PCA results in a relatively better distribution of households and comparatively fewer households concentrate on a particular index value (DHS Comparative Reports, 2004). Items that all households possess or that no household possesses have little utility in segregating household socioeconomic status [41] and therefore must be excluded.
-
3.
Age and sex of a child: Child sex and age of the child (measured either in months or years) are among the crucial determinants of a child’s nutritional status (Chen et al., 2007). In poor countries like Ethiopia, a male child is preferred to a female child and as a result, receives more attention. There are studies in developing countries on gender preference and found that families favour having a male child over a female [23, 43]. Conventionally, younger family members in the household receive higher levels of care from household members than older ones. However, this does not necessarily mean that younger children are not at risk of being stunted or underweight. Both age (male and female) and sex (below 1 year, 1–3 years, and 3–5 years) are categorical variables.
-
4.
Other predictors: Other variables include a place of residence (urban or rural), order of childbirth, gender of household head, mother’s age at interview (20, 2029, 30–39, and 40–49), type of sanitation, source of drinking water, and the nine regions and two city governments as predictors. Access to health care is highly dependent on the proximity of services to individuals [31], and it is hypothesized that health services are more likely to be used in urban areas than in rural areas. The inclusion of this variable, therefore, serves to quantify discrepancies in the use of health services and captures geographical inequalities.
2.2 Method of analysis
The concentration index, together with the concentration curve, is a useful tool for measuring health disparities since it reveals how divided society is. Because health resources are distributed more unevenly in more divided societies, the concentration index is higher in those societies. Inequality in health can lead to increased rates of death, morbidity, and disability, as well as social and economic imbalances. The concentration index can be used to track changes in inequality over time because it quantifies the level and direction of inequality in a population. Furthermore, using the concentration index as a gauge of health inequalities can point to potential intervention targets.
Health research has frequently employed concentration to examine disparities in health outcomes. The degree of health inequality within and between populations has been measured widely using the CI. The CI can be used to assess changes in inequality over time or to evaluate the degree of health disparity between populations with varying levels of socioeconomic development. The concentration index is increasingly used in the literature on socioeconomic inequalities in health [22, 47, 67]. Socioeconomic-related inequalities in health are typically illustrated using a concentration index where individuals are ranked based on their SES [45]. It is used to investigate socioeconomic-related disparities of various health variables. For instance: disparities in malnutrition [62], child mortality [58], child immunization [27], socioeconomic inequalities in child under-nutrition [35, 61], healthcare utilization [31], and so on. The problem with the concentration index as a measurement of health inequality is that it ignores the middle group as it merely emphasizes the two extreme cases: the poorest and wealthiest groups.
The concentration curve which corresponds to the concentration index is used to show if there exists socioeconomic-related disparity in health outcomes and if this disparity is more concentrated in one group than its counterpart. However, the Concentration curve will not show us the magnitude of the health disparities [60] which allows us to compare different cases. The concentration index can be estimated from the concentration curve as twice the area between the concentration curve and the line of equality [31]. The estimation of the Concentration Index for under-five child malnutrition will be made following the technique [35]. Given that CI is straightforward, simple to apply, and has been proven to be accurate, the concentration index is an excellent way to quantify child health disparities in Ethiopia.
If we have n individuals (1, 2,…, n) ranked using their SES variable (y1, y2,….yn) where the poorest is ranked 1st and the richest individual ranked nth (that is: r1, r2,….,rn), and health variable (under-five underweight and stunting rate) we are interested in individual i is denoted by hi where i = 1, 2, …,n the standard or relative CI can be estimated as follows:
where µ is the average health status of the population that is:
A negative (positive) CI shows the burden is concentrated around the most disadvantaged (advantaged) individuals. This is also shown by the concentration curve above (below) the line of equality indicates the concentration of ill health among the poorest (well-off). A concentration index that is based on covariance between health variables and the fractional rank of individuals based on socioeconomic status is a convenient estimation [36]. The covariance-based concentration index is determined by the relationship between the health variable we are interested in and the SES-based rank of individuals. It does not depend on the socioeconomic status itself [60]. While the sign of CI reflects the direction of the relationship between the rank and health variable, the magnitude indicates the variability of the health variable among groups and the strength of the relationship.
2.3 Decomposing the socioeconomic related disparities
The decomposition analysis in the simplest terms is to show how socioeconomic-based disparities in health are explained by various determinants of health. The study by [62] has introduced regression-based decomposition analysis to study how disparities in the determinants of child health contribute to inequalities in child health outcomes using data from Vietnam. As presented in the work of [60], the main objective of such decomposition analysis using regression is to explain socioeconomic-related disparities in health using a set of k determinants. In line with this, as discussed in the above section, the dependent variables are dichotomized binary variables where the variable stunting takes value one if stunted and zero otherwise. The same is true for the other under-nutrition variables. When the dependent variable is a binary health outcome variable, a variety of methods can be used for the decomposition analysis, including the linear probability model, probit/logit, and GLM. In this study, we have attempted to employ the first three techniques (LPM, logit, and probit models) and undertake a comparison of results. We then used a post-estimation link test to check the model specification.
The decomposition starts from a linear representation of the health variable, h being explained by a set of predictors X1, X2… Xk.
Mathematically,
where βk and ϵi are the coefficients of the k-determinants and the error term respectively.
The above kind of representation is also referred to as health-oriented decomposition. The set of predictors included in the linear regression includes the mother’s level, education, residence, sex of a child, mother’s age during birth, and regions. By substituting the above expression into Eq., the standard CI can be further rewritten as follows given the relationship between the health variable hi and its determinants Xk. That is, Recall Eqs. (1) and (3) as:
- 1.:
-
$${c}_{h}=\frac{2}{n\mu }(\sum_{i=1}^{n}{h}_{i}{r}_{i})$$
- 2:
-
$${h}_{i}= {\beta }_{0}+{\beta }_{1}{X}_{1i}+ {\beta }_{2}{X}_{2i}+\dots \dots \dots \dots \dots .+ {\beta }_{k}{X}_{ki}+ {\varepsilon }_{i}$$
upon substituting equation (2) into equation (1) as follows:
The mean of the rank: \({r}_{i}=\frac{1}{2}\)
and from Eq. (1) – 1\({c}_{h}=\frac{2}{n\mu }(\sum_{i=1}^{n}{h}_{i}{r}_{i})\), we will obtain the following by rearranging:
According to those expressions, we can further apply the manipulations as follows
Having those in mind and inserting them in Eq. (4), we will have the following general equation:
By expanding terms and assuming \(\mu = {\beta }_{0}+ \sum {\beta }_{k}{\overline{x} }_{k}\), we will get.
where, \({\overline{x} }_{k}, {C}_{k} and {GC}_{\varepsilon }\) are the averages of \({x}_{k}\), CI for \({x}_{k}\), and the generalized concentration index for the error term respectively. The standard Concentration index presented above is therefore composed of two parts: ‘the explained’ (the sum of concentration indices of all the regressors which are weighted by the elasticities of h w.r.t each) \({x}_{k}, \left(\frac{{\beta }_{k}{\overline{x} }_{k}}{\mu }\right)\text{and}\) ‘the unexplained component’ which reflects the inequality not explained by variation SES in the \({x}_{k}\). The residual GCϵ is expressed as:
Doorslaer and his co-authors [62] have recommended the following steps to be followed while undertaking regression-based decomposition analysis of socioeconomic-related disparities in health.
-
Running an appropriate model: run a model of health variable (h) on all k-determinants (X’s) and obtain the coefficients of the regressors, βk
-
The mean values: after regressing the health variable against the X’s, the next step is to estimate the mean of the dependent and explanatory variables \({\mu }_{h}\) and \({\overline{x} }_{k}\)
-
Concentration Indices: obtain CI for h and Xk that is, the Ch, Ck, and GC by applying the same technique as
\(C\left(h|y\right)=\frac{2}{n\mu }\left(\sum_{i=1}^{n}{h}_{i}{r}_{i}\right)-1\).
2.3.1 Contribution of each explanatory variable to the inequality in health:
-
Estimate the following two types of contributions for each explanatory variable:
-
A.
Absolute Contribution: \(\left(\frac{{\beta }_{k}{\overline{x} }_{k}}{\mu }\right)*{C}_{k}\) which is obtained by multiplying the health variable elasticity w.r.t the explanatory variable by its CI.
-
B.
Percentage contribution: \(\left(\frac{{\beta }_{k}{\overline{x} }_{k}}{\mu }\right)*\frac{{C}_{k}}{{C}_{h}}\) divides the absolute contribution by the CI of the health variable.
-
A.
Finally, the researchers have decomposed the changes of concentration indices in the under-five and stunting between the earliest and most recent demographic and health surveys using Oaxaca decompositionFootnote 3, a recommendation by [62].
The expression is derived simply by applying the Oaxaca-type decomposition to Eq. (5) and every variable included in the expression represents a two-period case which is the 2000 DHS and 2016 DHS. The first term of the RHS indicates the difference of CI of the predictors at time t weighted by the elasticity of the health variable concerning the explanatory variables at time t and the second term in the RHS reflects the differences in the elasticities of the health variable in two periods which is weighted by the concentration index of the explanatory variable at the earliest period. Finally, the last term in the RHS is simply the change in the generalized concentration of the unexplained component.
3 Results and discussion
3.1 Descriptive statistics
Table 1 presents the mean, corresponding standard deviation, and description of the selected socioeconomic covariates and indicators of child malnutrition discussed in the previous section. The determinants of child health disparities were selected after reviewing relevant and similar studies conducted in other developing and developed countries using the DHS database. In all tables below, the analyses consider the sampling weights of the DHS surveys. The undernutrition variables are estimated according to the WHO z-score, which is less than − 2. According to our estimation, the weighted level of prevalence of stunting, wasting, and being underweight was about 57.6%, 12.4%, and 40.9% respectively in 2000 and decreased to 38.3%, 10.1%, and 23.7% in 2016 in that order. There is a massive improvement in the level of prevalence of stunting and underweight between 2000 and 2016, but the changes in wasting are not substantial. Children’s health is strongly associated with the conventional socioeconomic exposure of children’s families (more specifically, the mother’s educational status and wealth). Therefore, the mother’s educational status is included as a dummy variable: educated (if her educational level is a secondary school or above) and uneducated (below secondary school). Similarly, the wealth index is estimated from the demographic and health surveys and quintiles are formed.
According to the descriptive analysis presented in Table 1, the mean scores for access to improved drinking water and sanitation sources were 0.279 and 0.194, respectively, in 2000. While the mean score for access to an improved source of drinking increased to 0.619 the mean score for improved sanitation declined to 0.172 in 2016. In line with this, the DHS final report of the country has also confirmed that the sanitation coverage of the country has shown a declining trend. While it can be challenging to identify the precise causes for the decline, they are probably a result of several variables such as poverty; the pace of population increase outweighs the intervention/effort from the government to increase sanitation coverage and a lack of resources. Differences in sample sizes, households selected, enumeration areas and other related characteristics between the two-survey series may also contribute to the decline in the mean of sanitation coverage.
Other demographic and socioeconomic determinants such as sex of the child, age of the child in the month, age of the mother at birth, sex of the head of the household, and area of residence appear to have a direct or indirect effect on the child’s nutritional status are also included in the analysis. Finally, nine regional states and two city governments are included to capture whether there are regional differences.
3.2 Trends and changes of inequalities in under-nutrition indicators
As we can see from Table 2, there has been a sharp and significant decline in stunting and underweight rates, but the improvement in wasting in children under five has been slow and stagnant. The table summarizes the absolute gap and relative inequality in child undernutrition across selected socioeconomic covariates and changes in these indicators from 2000 to 2016.
Across all variables, there has been a decline in the prevalence of stunting and underweight. For example: nationally, the prevalence of stunting and underweight decreased by approximately 19% and 17.4%, respectively, between the first and last DHS. This is a major achievement in terms of improvements; however, these rates are still higher and require further action to protect children from persistent malnutrition, affecting them later in life. In addition, the absolute differences in the prevalence of stunting and underweight across categories are positive, indicating that disease-related variables are higher in the hypothesized disadvantaged groups (for example a child whose mother is uneducated, who lives in rural areas, has low SES, heads a female-headed household, and has an unimproved source of drinking water).
Table 2 demonstrates the extent of child malnutrition from 2000 to 2016 Demographic and Health Surveys across quintiles, ordered from poorest to richest. The prevalence of both stunting and underweight was relatively higher among children whose families ranked lower. As discussed in the previous section, both the concentration index and concentration curves have been criticized because they say nothing about the middle groups [62]. Instead, they emphasize the two extremes: the privileged and unprivileged individuals or groups. As can be seen in the charts, the relative disparity between the poorest and the richest in stunting prevalence in 2016 is visible.
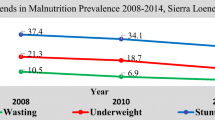
Similarly, the differences in the prevalence of underweight can be observed between socioeconomic groups in both 2000 and 2016. In both cases, the forms of child undernutrition are higher in the socioeconomically disadvantaged groups than in the comparison group. For instance: Fig. 1 shows the trend of stunting and underweight prevalences across mothers’ educational attainment. This chart indicated that the prevalence is higher among those children whose mothers are relatively less educated.
Some of the improvements in child malnutrition indicators are in favour of advantaged groups, leading to an increase in inequality between groups, while others are in favour of disadvantaged groups, leading to a decrease in inequality. For example, the absolute difference in the prevalence of stunting among children living in rural and urban areas was about 11.2% in 2000, and the difference has increased to 13.7% in 2016. This means that the gap has widened and a child living in the city has benefited more than a child living in the countryside.
In contrast, the gap between rural and urban underweight rates has decreased from 14 to 11%. Similarly, the absolute and relative differences in both forms of child undernutrition by gender of the household head have narrowed. The table shows that children from households headed by men are less likely to be affected by stunting and underweight than children from households headed by women. Both the prevalence of stunting and underweight have improved significantly among children from the poorest and richest nodes. However, the difference between the richest and poorest increased from 11.6% to 19.6% for stunting prevalence and from 13.2% to 16% for underweight prevalence within the reported period. In summary, absolute differences in the prevalence of stunting and underweight have not consistently decreased across household wealth quintiles and other demographic and socioeconomic indicators.
The different concentration indices of child undernutrition variables are summarized in Table 3. The type of concentration index used in this study is the standard concentration index supplemented by the generalized concentration index. However, the Wagstaff Index (W) and Erreygers Index (E) are also obtained for the indicators. The purpose of estimating these indices is simply to support the results of the absolute relative (standard) and absolute (generalized) concentration indices. It is shown that all types of CIs for the prevalence of stunting, wasting, and underweight in 2000 and 2016 are negative and statistically significant. These estimates showed that the burden is concentrated among the unprivileged groups of children whose families have lower socioeconomic exposure.
As is depicted in the figure, the absolute concentration curve for the indicators of child malnutrition is above the line of equality. This confirms that the problem is heavily concentrated among children from the lower wealth quintile. These curves only show whether socioeconomic inequalities in health (disease) outcomes exist, or whether inequality is more pronounced at one time than another, in a group, region, or country. It does not generate an estimate of the level of inequality that we use to make comparisons between individuals, groups, regions, or countries.
According to the [45] guide to estimating the concentration index, inequality indices can be estimated for binary or categorical variables and compared across different groups. In this study, inequality indices are estimated across different demographic and socioeconomic indicators (rural/urban, educated/uneducated mothers, wealth quintiles, mother’s age at birth, child’s sex, and household heads) and tested with the null hypothesis of no differences between groups. This is done by comparing wealth-related differences in child malnutrition indicators (prevalence of stunting, and underweight) between the above groups.
Since individuals are ranked by their socioeconomic status (proxied by asset index), a negative concentration index indicates that the ill health variable, malnutrition, is highly concentrated among the poor. Given that we have negative concentration indices according to the table presented above, inequalities in malnutrition indicators are said to be increasing, if the value of the index is close to -1 compared to its counterpart. For instance: according to our estimation in Table 4, the concentration indices of stunting prevalence have shown an increasing trend at all levels: be at national, urban, and rural levels. The index at the national level was -0.0314 in 2000 and increased to -0.09587 in 2016, in urban areas the index increased from -0.147 in 2000 to -0.303 in 2016. Finally, the concentration index in rural areas was -0.014 and -0.060 in 2000 and 2016 respectively. Those indices demonstrated that there exists a noticeable worsening in the level of inequalities in child malnutrition.
The changes in the concentration index suggest a larger increase in inequality for most indicators among rural children compared to urban children between 2000 and 2016. This is further supported by the higher estimated standard concentration index for rural areas. A possible explanation lies in the limited variation of certain assets within rural households. Owning no durable assets, having similar access to utilities and infrastructure, and possessing comparable housing characteristics (number of rooms and building materials) across households reduces the ability of the asset index to differentiate wealth quintiles in rural areas.
As is discussed in the previous sections, PCA generates a well-informing asset index, when the asset is unequally distributed between households [41]. In other words, if an asset is owned by all households or is not owned by any household, it will have insignificant use in differentiating households using their SES. Households who are living in urban in contrast, have a significant difference in terms of the durable assets they own, and the establishment of an asset index based on the PCA can show us very important variance between the richest and poorest households.
3.3 Results of the empirical analysis
In the preceding sections, it is attempted to discuss the findings of descriptive analysis and standard concentration indices of inequalities in children’s malnutrition forms across different groups. The results of descriptive analysis and concentration indices generated mixed trends regarding the disparities in children’s malnutrition: that is, their results demonstrated both widening and contracting disparities. However, those results might not be vigorous and may be subject to biasedness. A study by [20] concluded that the number of pieces of literature investigating the impact of socioeconomic inequalities on health outcomes and differences in the level of ill-health outcomes among individuals and groups is growing but the explanation about the degree of the differences and explanation of the differences in the inequalities is not sufficiently documented. In the succeeding sections, a discussion of the results of multivariate analysis is presented. In case the dependent variable is a categorical (binary) variable, OLS regression, marginal effects from probit analysis, GLM, LPM, and non-linear logit model can be used to undertake the analysis including the decomposition analysis [59]. As a result, we have employed the Linear Probability model, logit, and probit models where child ill-health variables are predicted by a set of determinants. The purpose of employing all those techniques is simply not beyond checking their consistency. Those techniques have generated comparable results, and the coefficients of the determinants will be used in decomposing and estimating the absolute and percentage contribution of the determinants to the socioeconomic inequalities in child health. Studies on disparities in children’s malnutrition are used to establish a relationship between the malnutrition forms and the wealth of their families as well as demographic and socioeconomic experiences. As a result, the main emphasis of the analysis will be given on how the convenient socioeconomic indicators (household socioeconomic rank based on the estimated asset index and mother’s educational status) are contributing towards the socioeconomic disparities in child malnutrition forms.
Table 5 recapitulates the multivariate analysis of inequality in the variable child undernutrition (which is the prevalence of stunting) explained by various inequalities in health determinants. We ran LPM, logit, and probit models for the variable stunting (= 1 if stunted, 0 otherwise) on the Xk determinants, and the models generated comparable results. The coefficients from the LPM with OLS estimates are easy to interpret because they are the marginal effects. However, the interpretation of the coefficients from the probit and logit is not straightforward. The sign of the coefficients from the latter models explains the likelihood that children are stunted relative to the reference groups. Negative (positive) coefficients indicate that the target groups have a lower (higher) probability of stunted compared to the reference groups. Interpreting the magnitude of the probability of being Stunted is more complicated than the estimates from OLS. With LPM, the coefficients of the independent variables are the magnitude of the marginal effect of the covariates on our dependent variable.
The study revealed an inverse association between household socioeconomic status and the prevalence of stunting and underweight in children. Linear Probability Model (LPM) results showed a clear trend: children from wealthier households were less likely to be stunted compared to those from poorer households. Specifically, children from the middle, richer, and richest households had a progressively lower probability of stunting by 9%, 11%, and 14.4%, respectively, compared to children from the poorest households (although the effect for the poorest group wasn't statistically significant). These findings were echoed in the logit model, where the probability of stunting decreased incrementally across wealth quintiles, with the richest group having a 15.4% lower probability compared to the second-richest group. However, the analysis of the 2000 Demographic and Health Survey (DHS) data did not find a statistically significant association between SES and the probability of a child being malnourished.
According to the regression results summarized in Table 6 for the underweight frequency indicator, the probability of a child suffering from being underweight is strongly related to the socioeconomic status of the household. We confirmed that inequality in SES causes inequality in the probability of a child being undernourished as measured by being underweight. From the model LPM, a child is 3.4%, 7.8%, 13.4%, and 10.7% more likely to be underweight if he or she comes from a poorer, middle, richer, and richest household, respectively. The marginal effect of household socioeconomic exposure on the probability of a child being malnourished supports the findings obtained from LPM. Holding other things constant, the odds of a child being malnourished are 3.3%, 7.7%, 13%, and 10.4% lower than the poorest in rank when the family’s SES is in the 2nd to 5th percentile.
Building on the previous section, a mother's educational attainment significantly impacts her children's nutritional status. Mothers with higher education are more likely to utilize prenatal and postnatal care, ultimately reducing the risk of child malnutrition. In this study, mothers were categorized as "uneducated" (primary education or less) and “educated” (secondary education or more). The regression results align with these expectations. Children with uneducated mothers have a significantly higher probability of stunting. Compared to children of educated mothers, the likelihood of stunting increases by 16.2% according to the linear probability model (LPM) and 11.8% according to the logit model.
In terms of the age of a child, the results are statistically significant and confirm our expectations. The results from LPM show that the marginal effect of a child aged 13–36 months and 37–59 months has a higher probability of stunting than a child aged 0–12 months. In 2000, controlling for other covariates, a child aged 13–36 months and 37–59 months is 34.8% and 34.2% more likely to be stunted than a child aged 0–12 months, respectively. Similarly, the probabilities for these age groups of being stunted decreased to about 27% and 25.1%, respectively. The same is true for the results from the logit and probit models (which are attached at the end of this document). According to the logit model, a child aged 13–36 months is 27.9% more likely to be stunted than a child aged 0–12 months.
For children 37–59 months old, the probability of being stunted is estimated to be 25.8% higher than for children 0–12 months old. The results from LPM and logit regressions using the 2016 data give us very comparable probabilities. The results for the underweight indicator are also similar. Daughters/sons who are younger than household members receive more care from household members compared to those who are older. Children aged 13–36 months and 37–59 months have a higher probability of suffering from being underweight than the reference group (children aged 0–12 months). The LPM regression results show that holding all other covariates constant, 13–36 and 37–59-month-old children have a 16.6% and 16.3% higher probability of suffering from being underweight than the children aged 0–12 months. In 2016, the probability of being underweight for their age was 10.3% and 13% higher in the above age groups, respectively. Complementing this, the logit model produces very similar probabilities. The probabilities for children aged 13–36 and 37–59 months of being underweight were 10.3% and 12.9%, respectively, which are very similar coefficients to the LPM regression results.
Other variables such as a child’s birth order, the child’s sex, the head of the household, the source of drinking water, and regional conditions also have a significant impact on child malnutrition disparities. Children who do not have access to an improved source of water for drinking are affected by both stunting and being underweight. The motivation for including regional state and city governments in the analysis was to capture any regional effect and to examine who was doing better than who. According to Table 6, in 2000, the probability of being underweight for age was relatively lower in Afar, Oromia, Somali, Gambella, Harari, Addis Ababa, and Diredawa regions compared to Tigray regional state. In 2016, children from the only Somali region, Gambella region, and Addis Ababa city are less likely to be stunted compared to Tigray regional state. Children from Harar town, Diredawa town, and Addis Ababa town were less likely to be underweight in 2000 than in the reference region. Gumuz region, Addis Ababa town, and Diredawa town performed better than Tigray regional state in 2016.
In conclusion, there is still a significant difference between the regional states in terms of the likelihood of being undernourished. The variable “type of household sanitation” is not statistically significant in all models, so it does not contribute to the inequalities in child malnutrition. Another important variable that is found to have a significant effect on inequalities in stunting and underweight according to the regression results is the age of the mother. For example, according to the result of LPM, the older the mother is, the lower the probability that a child is smaller than his mother for his age. The estimated probabilities are 5.3%, 9.1%, and 9.8% lower for a child whose mother’s age is 20–29 years, 30–39 years, and 40–49 years, respectively, compared to a mother less than 19 years old.
Disparities in child malnutrition according to the place of residence (urban and rural) produce mixed results in recent studies. There is scattered evidence that the gap is narrowing and that migration contributes to this effect. Poverty and malnutrition are gradually shifting from rural to urban areas in developing countries. Thus, the number of urban poor and malnourished is increasing faster than the number of rural poor. Other studies have shown that urban children are better nourished and less likely to be stunted and underweight than their rural counterparts [21, 51]. According to [51], urban children are less likely to be stunted and underweight because they are better nourished than their rural counterparts. Increased poverty-related migration from rural to urban areas decreases the urban health advantage [28]. These migrated people live in informal settlements and slums, making them vulnerable to disease. All our regression results showed that a child living in rural areas is less likely to be stunted and more likely to be underweight than a child living in urban areas. However, the relationship is not statistically significant.
3.4 Decomposition analysis
Once we obtain the coefficients of the determinants of health inequality, we can proceed to decompose the contribution of the covariates to inequality in child malnutrition. Tables 7 and 8 show the absolute and percentage contribution of health determinants to inequalities in child undernutrition (stunting and underweight prevalence). The primary aim of these tables is to distinguish the main demographic and socioeconomic determinants of health that contribute to inequalities in poor health indicators at a representative national level.
Generally speaking, based on the data from 2000 Ethiopia DHS, the selected explanatory variables contribute to around 97% of the disparities in stunting prevalence, and only 10% of the inequality in underweight is explained by the inequalities in the determinant of inequality if underweight. Mothers’ educational status contributes substantially to the disparity with about 31.3% followed by socioeconomic status which contributes about 30.4%. This indicates that the percentage contribution of inequalities in both variables (education level of mothers and SES) accounts for around 62% of the inequality in stunting. Likewise, being born at later orders have also an appreciable contribution to the inequality in stunting. According to the decomposition in Table 7, inequalities in mothers’ educational status, socioeconomic status, and child’s birth order have contributed significantly and can be considered the most important determinants of inequality in stunting.
The decomposition of the contribution of inequalities in the determinants of health to the inequalities in stunting and underweight prevalence using the DHS 2016 are summarized below. According to the decomposition analysis, the explanatory variables have contributed to about 92.6% and 93.8% of the inequalities in stunting and underweight prevalence respectively. The unexplained component of the inequality in stunting is 7.4% and 6.2% in underweight. Compared to the decomposition analysis discussed above, this one is relatively explained better by the perspective covariates. Both socioeconomic position and educational level of mothers have contributed more than 90% to the inequality in stunting and about 80% to the disparities in underweight prevalence. The birth order of a child has also a relatively significant contribution to the inequality: those children who are born later orders are more likely to be malnourished. The contribution of birth order accounts for about 4.5% of the inequality.
Bringing Tables 7 and 8 together, we can also compare the percentage contribution of the major determinants of health to the disparities in child malnutrition. In 2000, all the corresponding variables explained the disparities in stunting more than they did in 2016. The percentage contribution of the socioeconomic position of households has increased from 30% in 2000 to 77% in 2016. However, the percentage contribution of mothers’ education declined from 31% in 2000 to 13.5% in 2016. Even if there exist fluctuations in the percentage contribution of the important and conventional socioeconomic indicators (mother’s education status and wealth index of households), both remain the driving variables for the inequality in child malnutrition in Ethiopia.
Like other poor countries, it is revealed that in Ethiopia there were considerable improvements in dropping off child malnutrition indicators (both stunting and underweight, whereas the changes in wasting prevalence, are not large enough) in the past decades. However, those global improvements are not evenly distributed [5, 21, 56] among various socioeconomic groups. The same is true in the case of Ethiopia; despite the improvements in the indicators under study between 2000 and 2016, some of the improvements are in favour of the advantaged groups causing the inequality between groups to increase and few other improvements are in favour of the disadvantaged ones leading the inequality level to be contacted. The absolute gap in stunting prevalence among children living in rural and urban was about 11.2% in 2000 and the gap increased to 13.7% in 2016. This implies the gap has increased and a child in an urban has benefited more than a child living in a rural.
In contrast to this, the difference between the underweight rate in rural and urban has dropped from 14 to 11%. Residence locations and distance to get healthcare services are the most common geographical factors [19, 48] that contribute to higher child health problems. A serious concern is that most child health problems happen from causes that can be easily manageable or preventable. The life chances of children vary dramatically by location and early life experience. A girl born in a poor neighborhood can expect to spend more of her life suffering from health problems than had she been born to rich relatives.
Likewise, the absolute gaps and relative gaps in both forms of children’s malnutrition were contracted by the sex of the household head. Both stunting and underweight prevalence among children from the poorest and richest knots have significantly improved. However, the difference between the richest and poorest in the stunting prevalence has increased from 11.6% to 19.6% and underweight prevalence has increased from 13.2% to 16% respectively within the specified period. To sum up, the absolute gaps in stunting and underweight prevalence have not consistently declined across household wealth quintiles and other demographic and socioeconomic indicators.
3.4.1 The findings from the empirical analysis are statistically significant and consistent
With other empirical studies when it comes to a child’s age. According to LPM results, children between the ages of 13 and 36 months and 37 and 59 months are more likely to be stunted than children between the ages of 0 and 12 months. A child’s likelihood of being stunted increases as they become older, according to studies conducted using the data from DHS 2000 and DHS 2016. The likelihood of being stunted dropped for these age groups from 2000 to 2006, indicating that the unfavorable health effects are getting better. The underweight indicator produces similar findings. Daughters and sons who are younger than household members get more attention from the family than those who are older do. Children between the ages of 13 and 36 months and 37 and 59 months are more likely than the reference group to be underweight (children aged 0–12 months).
4 Conclusion and policy implication
The study’s general objective is to explore the socioeconomic disparities in child malnutrition in Ethiopia and investigate which groups have benefited more than those from the improvements in the mean of the adverse health indicators between the periods 2000 and 2016. The study also aimed to identify the major health determinants contributing to the inequalities in child malnutrition. The disparities in access to nutrition and/or health services caused by a child’s birth circumstances, such as parental background, geographic location, etc., are detrimental to a child’s proper development and increase the risk of child mortality and illness, which later results in poor adult health outcomes. This age group demands special consideration in and of itself since maturity exhibits the long-term effects of health issues present in childhood.
The constructed concentration curve confirmed that there exist pro-poor inequalities in child malnutrition indicators. The curve lying above the equality line implies problems are concentrated on those children from the lower wealth quintile. Those curves only show whether socioeconomic health disparities (ill health) outcomes exist or not. It does not generate an estimate of the inequality level which we will use to make comparisons. From the empirical analysis, we have shown that the estimated asset index of households favored those children who are in a better position in the socioeconomic rank. Poverty can lead to child malnutrition [57] and this malnutrition might be persistent and can in turn trap them in poverty [30]. It is found from the regression techniques that a child from a higher socioeconomic status of the household is less likely to be malnourished than their counterparts. This result supports the findings by [31, 39, 50].
In the same fashion, the impact of a mother’s educational level is found to be another crucial determinant of disparities in child malnutrition. The presence of differences in the level of a mother’s educational status results in inequalities in child health in general which are studied using the malnutrition indicators. The likelihood of being short for age and underweight prevalence will be higher for those children who are a son of uneducated mothers. This is directly related to their commitment to using healthcare services both before and after the delivery of a baby. Educated mothers will use prenatal care services during pregnancy and educated lactating mothers will use antenatal care services properly. Higher education levels of mothers will result in higher utilization of healthcare services [49]. This kind of care service is directly related to a minimal risk factor for a child. Differences in those practices will cause inequalities in the probabilities of a child being malnourished (shorter for age and underweight prevalence). The multivariate and decomposition analysis of the study has confirmed this kind of association between the education level of a mother and the inequalities in the probability of child malnutrition forms.
According to the DHS statistics, we have determined that considerable percentages of moms who are classified as uneducated in our study had education levels below elementary. As a result, there should be an intervention that aims to increase the proportion of educated mothers, which in turn leads to a decreased inequality in mothers’ educational attainment, to bring about favorable results in the child health we are interested in. We firmly believe that improving the percentage of educated mothers and so reducing the educational disparity between mothers can have a significant impact on children’s nutritional health. This will then have the desired effect on the nation’s disparities in child malnutrition. There are numerous advantages to improving nutritional status that cannot be overstated, including better health and survival, cognitive development, and future human capital.
In poor countries like Ethiopia, a male child is preferred to a female child and as a result, receives more attention. There are studies in developing countries on gender preference and found that families favor having a male child over a female [23, 43]. The main reason for this type of preference is related to the possible future contribution of children when they grow up. When daughters marry, they will take over some of the family resources and serve their husband’s families. A son, on the other hand, will guard, protect, and secure the family and help it increase its wealth before and after marriage. The nutritional status of a child also responds to the level of care and feeding practices he has experienced.
As it is discussed above, the difference in socioeconomic positions and the mother’s educational status are the major contributors/determinants to inequalities in child malnutrition. Even if the literacy rate in Ethiopia is growing higher, there is still huge room for improvement which will have a direct and indirect impact on the inequalities in child health. If differences in the education level of mothers are minimized, then the inequality in the utilization of healthcare services will also decline to imply that the inequality in child malnutrition will decline.
To the best of our knowledge, this is a comprehensive study that used data from the two extreme periods of DHS in the context of Ethiopia. Despite the comprehensive review of related literature, we have made in the context of developed and developing context, we want to highlight the main limitations of the study and forward some directions of future research perspectives.
DHS is typically thought to be nationally representative and is gathered in both urban and rural settings. However, in developing nations like Ethiopia where there are large disparities in living standards, combining data from rural and urban areas may not be able to accurately determine an individual’s or household’s SES rank. This is because most rural households lack durable assets, have few assets, have similar housing characteristics (such as the number of rooms and the type of construction materials used), and have similar access to utilities and infrastructure (that is, lack formal sanitation facilities and source of water). When the distribution of the variables varies between households, principal component analysis functions at its best. The list of variables to be utilized for computing the wealth index using PCA is not widely agreed upon. Ref. [41] made an effort to compare the SES distribution across cases using only housing characteristics, only access to infrastructure and utilities, only ownership of durable assets, and all three categories combined. Mckenzie concluded that combining all three categories does not result in evidence of clumping and truncation. It is preferable to include any variable that may reflect the economic status of households so that the distribution of variables differs among households. This is because a larger number of items results in a generally better distribution of households in the PCA. Items that are owned by all households or none provide little purpose in classifying household socioeconomic status [41], hence they must be eliminated.
It is therefore recommended to investigate if constructing a wealth index for rural and urban separately explains the socioeconomic status better than constructing an index at the national level. As an alternative, it would be great if other indicators, such as consumption expenditure or household income levels, could be utilized in conjunction with the other variables. To put it another way, I strongly advise future researchers to investigate the consistency of results from consumption expenditure- or household income-based classification and socioeconomic status indices based on principal component analysis.
Data availability
Data is freely available in the DHS website.
Notes
Reduce under-five mortality to at least as low as 25 per 1,000 live births in every country.
Ethiopia DHS; 2000, 2005, 2011, and 2016. Final report of DHS 2019 was in progress during the preparation of the work.
Blinder (1973) and Oaxaca (1973) [34] have formulated a technique which was initially used to study labor market outcome by groups. Those days, Oaxaca decomposition is also being used to study differences between two groups in the mean of health variable.
References
Al-Ateeq MA, Al-Rusaiess AA. Health education during antenatal care: the need for more. Int J Women Health. 2015;7:239.
Amsalu S, Tigabu Z. Risk factors for severe acute malnutrition in children under the age of five: a case-control study. Ethiop J Health Dev. 2008;22:1–96.
Bado AR, Appunni SS. Decomposing wealth-based inequalities in under-five mortality in west africa. Iran J Public Health. 2015;44(7):920.
Bain LE, Awah PK, Geraldine N, Kindong NP, Siga Y, Bernard N, Tanjeko AT. Malnutrition in sub–saharan africa: burden, causes and prospects. Pan Afr Med J. 2013. https://doi.org/10.11604/pamj.2013.15.120.2535.
Barros FC, Victora CG, Scherpbier R, Gwatkin D. Socioeconomic inequities in the health and nutrition of children in low/middle income countries. Rev Saude Publica. 2010;44:1–16.
Basch CE. Healthier students are better learners: a missing link in school reforms to close the achievement gap. J School Health. 2011;81(10):593–8.
Benson T, Shekar M, et al. Trends and issues in child undernutrition. In: Jamison DT, Feachem RG, Makgoba MW, et al., editors. Disease and mortality in Sub-Saharan Africa. 2nd ed. Washington: The International Bank for Reconstruction and Development/The World Bank; 2006.
Bhutta ZA, Berkley JA, Bandsma RH, Kerac M, Trehan I, Briend A. Severe childhood malnutrition. Nat Rev Dis Primers. 2017;3(1):1–18.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, Mathers C, Rivera J, Child Undernutrition Study Group, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–60.
Bredenkamp C, Buisman LR, Van de Poel E. Persistent inequalities in child undernutrition: evidence from 80 countries, from 1990 to today. Int J Epidemiol. 2014;43(4):1328–35.
Bruins MJ, Van Dael P, Eggersdorfer M. The role of nutrients in reducing the risk for noncommunicable diseases during aging. Nutrients. 2019;11(1):85.
Chao F, You D, Pedersen J, Hug L, Alkema L. National and regional under-5 mortality rate by economic status for low-income and middle-income countries: a systematic assessment. Lancet Glob Health. 2018;6(5):e535–47.
Childs CE, Calder PC, Miles EA. Diet and immune function. Nutrients. 2019. https://doi.org/10.3390/nu11081933.
Chopra I, Juneja SK, Sharma S. Effect of maternal education on antenatal care utilization, maternal and perinatal outcome in a tertiary care hospital. Int J Reprod Contracept Obstetr Gynecol. 2019;8(1):248.
De P, Chattopadhyay N. Effects of malnutrition on child development: evidence from a backward district of India. Clin Epidemiol Glob Health. 2019;7(3):439–45.
Demographic and Health Survey Report. Central statistical authority and orc macro calverton, Maryland, USA. 2000.
Demographic and Health Survey Report. Central statistical authority and Icf international macro calverton, Maryland, USA. 2016.
Dewey KG, Begum K. Long-term consequences of stunting in early life. Maternal Child Nutr. 2011;7:5–18.
Fang P, Dong S, Xiao J, Liu C, Feng X, Wang Y. Regional inequality in health and its determinants: evidence from china. Health Policy. 2010;94(1):14–25.
Feinstein JS. The relationship between socioeconomic status and health: a review of the literature. Milbank Q. 1993. https://doi.org/10.2307/3350401.
Fotso J-C. Child health inequities in developing countries: differences across urban and rural areas. Int J Equity Health. 2006;5(1):1–10.
Fotso J-C, Kuate-Defo B. Socioeconomic inequalities in early childhood malnutrition and morbidity: modification of the household-level effects by the community SES. Health Place. 2005;11(3):205–25.
Fuse K. Variations in attitudinal gender preferences for children across 50 less-developed countries. Demogr Res. 2010;23:1031–48.
Gebre A, Reddy PS, Mulugeta A, Sedik Y, Kahssay M. Prevalence of malnutrition and associated factors among under-five children in pastoral communities of Afar regional state, northeast Ethiopia: a community-based cross-sectional study. J Nutr Metab. 2019;2019:1.
Glewwe P. The impact of child health and nutrition on education in developing countries: theory, econometric issues, and recent empirical evidence. Food Nutr Bull. 2005;26(2suppl2):S235–50.
Gordon D, Nandy S, Pantazis C, Townsend P, Pemberton SA. Child poverty in the developing world. Bristol: Policy Press; 2003.
Gwatkin D, Rutstein S, Johnson K, Suliman EA, Wagstaff A, Amozou A. Initial country-level information about socioeconomic differences in health, nutrition, and population. Washington, DC: World BanK; 2003.
Harpham T. Urban health in developing countries: what do we know and where do we go? Health Place. 2009;15(1):107–16.
Heaton TB, Crookston B, Pierce H, Amoateng AY. Social inequality and children’s health in africa: a cross sectional study. Int J Equity Health. 2016;15(1):1–14.
Hoerder D. Undernutrition causes poverty however solutions exist. New York: UNICEF; 2009.
Hosseinpoor AR, Van Doorslaer E, Speybroeck N, Naghavi M, Mohammad K, Majdzadeh R, Delavar B, Jamshidi H, Vega J. Decomposing socioeconomic inequality in infant mortality in iran. Int J Epidemiol. 2006;35(5):1211–9.
Houweling TA, Kunst AE. Socio-economic inequalities in childhood mortality in low-and middle-income countries: a review of the international evidence. Br Med Bull. 2010;93(1):7–26.
Development Initiatives. Global nutrition report: shining a light to spur action on nutrition. Bristol: Development initiatives; 2018.
Jann B. The blinder–oaxaca decomposition for linear regression models. Stand Genomic Sci. 2008;8(4):453–79.
Kakwani N, Wagstaff A, Van Doorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. Journal of econometrics. 1997;77(1):87–103.
Kakwani NC. Income inequality and poverty. New York: World Bank; 1980.
Karacabey K, Ozdemir N. The effect of nutritional elements on the immune system. J Obes Wt Loss Ther. 2012;2:152.
Kraemer K, Cordaro JB, Fanzo J, Gibney M, Kennedy E, Labrique A, Steffen J, Eggersdorfer M. Diet and non-communicable diseases: an urgent need for new paradigms. In: Kraemer K, editor. Good nutrition: perspectives for the 21st century. Basel: Karger Publishers; 2016. p. 105–18.
Kumar A, Kumari D, Singh A. Increasing socioeconomic inequality in childhood undernutrition in urban india: trends between 1992–93, 1998–99 and 2005–06. Health Policy Plan. 2015;30(8):1003–16.
Lu C, Cuartas J, Fink G, McCoy D, Liu K, Li Z, Daelmans B, Richter L. Inequalities in early childhood care and development in low/middle-income countries: 2010–2018. BMJ Glob Health. 2020;5(2): e002314.
McKenzie DJ. Measure inequality with asset indicators. Technical report, BREAD working paper, 2003.
Megabiaw B, Rahman A. Prevalence and determinants of chronic malnutrition among under-5 children in ethiopia. Int J Child Health Nutr. 2013;2(3):230–6.
Ndu AC, Uzochukwu BSC. Child gender preferences in an urban and rural community in enugu, eastern nigeria. Int J Med Health Dev. 2011;16(1):24–9.
Nguyen TT, Hoang MV. Non-communicable diseases, food and nutrition in vietnam from 1975 to 2015: the burden and national response. Asia Pacific J Clin Nutr. 2018;27(1):19–28.
O’Donnell O, O’Neill S, Van Ourti T, Walsh B. Conindex: estimation of concentration indices. Stand Genomic Sci. 2016;16(1):112–38.
Rice AL, Sacco L, Hyder A, Black RE. Malnutrition as an underlying cause of childhood deaths associated with infectious diseases in developing countries. Bull World Health Org. 2000;78(10):1207–21.
Sastry N. Trends in socioeconomic inequalities in mortality in developing countries: the case of child survival in Sao paulo, Brazil. Demography. 2004;41(3):443–64.
Schoeps A, Gabrysch S, Niamba L, Sié A, Becher H. The effect of distance to health-care facilities on childhood mortality in rural Burkina faso. Am J Epidemiol. 2011;173(5):492–8.
Shrestha B. Mother’s education and antenatal care visits in Nepal. Tribhuvan Univ J. 2018;32(2):153–64.
Skaftun EK, Ali M, Norheim OF. Understanding inequalities in child health in Ethiopia: health achievements are improving in the period 2000–2011. PLoS ONE. 2014;9(8):e106460.
Smith LC, Ruel MT, Ndiaye A. Why is child malnutrition lower in urban than in rural areas? Evidence from 36 developing countries. World Dev. 2005;33(8):1285–305.
Tasic H, Akseer N, Gebreyesus SH, Ataullahjan A, Brar S, Confreda E, Conway K, Endris BS, Islam M, Keats E, et al. Drivers of stunting reduction in Ethiopia: a country case study. Am J Clin Nutr. 2020;112(Supplement 2):875S-893S.
UNICEF. 2020. https://www.unicef.org/media/60806/file/sowc-2019.pdf. 2019. Accessed 13 Oct 2020.
UNICEF. Children, food, and nutrition: growing well in a changing world. New York: UNICEF; 2020.
UNICEF-WHO-WB. United nations children’s fund, world health organization, the World bank. Unicef-WHO-WB joint child malnutrition estimates. New York: UNICEF; 2024.
Van de Poel E, Hosseinpoor AR, Speybroeck N, Van Ourti T, Vega J. Socioeconomic inequality in malnutrition in developing countries. Bull World Health Org. 2008;86(4):282–91.
Vorster HH, Kruger A. Poverty, malnutrition, underdevelopment and cardiovascular disease: a South African perspective. Cardiovasc J Afr. 2007;18(5):321–4.
Wagstaff A. Socioeconomic inequalities in child mortality: comparisons across nine developing countries. Bull World Health Organ. 2000;78:19–29.
Wagstaff A. The concentration index of a binary outcome revisited. Health Econ. 2011;20(10):1155–60.
Wagstaff A, O’ Donnell O, Van Doorslaer E, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation. New York: World Bank Publications; 2007.
Wagstaff A, Paci P, Van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33(5):545–57.
Wagstaff A, Van Doorslaer E, Watanabe N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J Econom. 2003;112(1):207–23.
Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, Demaio A. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395(10217):75–88.
WHO-Report. The importance of infant and young child feeding and recommended practices in infant and young child feeding: model chapter for textbooks for medical students and allied health professionals. Geneva: World Health Organization; 2024.
WHO-Report. Who report on nutrition. Geneva: World Health Organization Homepage; 2024.
Woldehanna T, Behrman JR, Araya MW. The effect of early childhood stunting on children’s cognitive achievements: evidence from young lives Ethiopia. Ethiop J Health Dev. 2017;31(2):75–84.
Zere E, McIntyre D. Inequities in under-five child malnutrition in South Africa. Int J Equity Health. 2003;2(1):1–10.
Zere E, Oluwole D, Kirigia JM, Mwikisa CN, Mbeeli T. Inequities in skilled attendance at birth in Namibia: a decomposition analysis. BMC Pregnancy Childbirth. 2011;11(1):1–10.
Acknowledgements
No funding.
Author information
Authors and Affiliations
Contributions
This work is sole-authored, and everything in the manuscript belongs to the author.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study does not include any human or animal object; therefore, ethical approval is unnecessary.
Competing interests
The authors declares that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gebregergis, C.M. Socioeconomic determinants of child malnutrition: Evidence from Ethiopia. Discov glob soc 2, 47 (2024). https://doi.org/10.1007/s44282-024-00062-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44282-024-00062-8