Abstract
Objective: This in vitro investigation should identify the effect of protective liners on dentine bond strength of a polyacid modified resin composite to dentine of primary teeth.
Methods: Forty-two extracted caries-free primary molars were randomly assigned to seven groups (n = 6) and flattened. Six test groups were centrally covered with different protective liners/base materials: Kerr Life (KL), IRM zinc oxide eugenol cement (IRM), Ketac Bond (KB), Vitrebond (VB), Dycal (DY), and mineral trioxide aggregate (MTA). Specimens were bonded with Prime&Bond NT (PB) and restored with Dyract eXtra. The control group (C) did not receive liner pretreatment. After 24-h storage in Aqua dest. (37 °C), specimens were cut and regional microtensile bond strengths of the uncovered areas were tested. Fractography was conducted under a light microscope and further interface/surface analyses were performed under a SEM. Statistical appraisal was carried out using oneway ANOVA (mod. LSD test; p < 0.05).
Results: Independent of the distance to the applied liner, all groups exhibited inferior μ-TBS to dentine of primary teeth compared to the control group (p < 0.05). The results were as follows in MPa(SD) x:significance level/percentage of adhesive fractures: PB: 34 (10)A/72%; KL: 23 (25)B/64%; KB: 15 (12)C/76%; DY 15 (13)C/55%; IRM: 14 (10)C/68%; VB: 12 (10)C/61%; MTA 12 (10)C/69%.
Conclusions: Protective liners significantly reduced μ-TBS to dentine of primary teeth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Protective liners have been applied to deep dentine following caries removal for many decades in order to protect pulp tissue and allow for tertiary dentine formation via active vital odontoblasts (Marchi et al. 2006). These materials are designed to cover and plug open dentinal tubules and to form a tight scaffold between restorative material and pulp (Falster et al. 2002). However, up to now it is not fully proven whether this is really induced by the presence of liners or bases (Marchi et al. 2006; Fuks 2008). There are multiple in vitro studies in the literature which show that a. thin residual dentine areas may allow for monomer diffusion through dentinal tubules (Schmalz et al. 2001), and b. that the critical remaining dentine thickness is double when it comes to primary dentine due to larger tubule diameters and less mineralization overall (Fuks 2008). For this reason, millions of protective liners are still applied on deep dentine areas in permanent as well as primary teeth. However, there is limited information whether these materials reduce dentine bonding behavior of adhesively bonded materials to dentine of primary teeth. Protective liners can be an adhesive alone (Falster et al. 2002), resin modified glass ionomer cement (Itota et al. 2006), calcium hydroxide (Al-Zayer et al. 2003), zinc oxide eugenol (Pinto et al. 2006), or glass ionomer cement (Marchi et al. 2006).
Due to the fact that a remaining dentine thickness of < 500 µm after excavation may be reliably associated with irreversible pulp damage in primary molars especially in proximal cavities, the question arises whether these liners are really helpful for what they are aiming. Although there is scarce evidence in the literature of the field, dentine adhesives may provide the best seal compared to any conventionally applied cement or base material (Buyukgural and Cehhreli 2008). This is also proven in several clinical studies of totally bonded resin composite or compomer restorations in primary teeth (Kramer and Frankenberger 2007, 2010; Casagrande et al. 2008; dos Santos et al. 2009). Potential antimicrobial effects would be even more welcome under these circumstances (Falster 2002; Foley et al. 2004; Duque et al. 2005, 2009; Franzon et al. 2007).
Considering the fact that the clinical use of these lining materials is found everywhere in the world, the question remains whether these materials may affect restoration stability (Lewis et al. 1992) and overall dentine bonding behaviour in the primary dentition which is still crucial for restoration retention, even more than in permanent teeth (Vij et al. 2004; Pinto et al. 2006; Buyukgural and Cehreli 2008).
Therefore, the aim of this study was to evaluate how different protective liners affect the bond strength of a widely used commercial compomer to the remaining free for bonding primary tooth dentine surface area.
Materials and methods
After approval by a local ethics committee (AZ 143/09), forty-two primary molars were collected after written informed consent of the parents. Teeth were collected through natural exfoliation or extracted due to therapeutic reasons (including orthodontic extractions) by primary care dentists who had received training regarding the tooth storage protocol. Specimens were stored immediately after extraction for a maximum of 28 days in 0.5% chloramine T vials which were provided to the primary care dentists in advance to the extraction (Frankenberger et al. 2001; Kramer et al. 2014; Boutsioukis et al. 2017). The vials were then posted to the laboratory. The teeth were debrided and refrigerated until use in the study. Microtensile bond strength experiments were done in accordance with protocols initially published by Pashley (1999). The authors have more than 20 years' experience with the technique which has been previously described in detail (Frankenberger et al. 2001; Kramer et al. 2014). The experiments were carried out by the second and third authors (SN, SL) who were calibrated by comparing results of control group with previous published data by Kramer in 2014. Primary molars were ground flat from occlusally with a silicon carbide sandpaper in roughness P 600—Grit 360 (Grinder-Polisher Beta, Buehler, Lake Bluff, USA; Fig. 1). A standardized smear layer was formed by further polishing the dentine with P 1200—Grit 600 sandpaper for 60 s manually forming "8-routes" in order to remove debris and to create the smear layer zone (Buehler Met II P600 silicone carbide paper, Buehler). Specimens that after preparation exhibited carious dentine, thin dentine layer (< 0.5 mm) or pulp exposure, were excluded from the experiments.
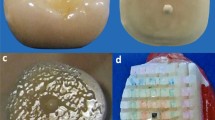
Experimental setup. a Deciduous molar crown before cutting. b Flat ground specimen with thinly applied protective liner in the centre (here: Kerr Life) with a diameter of 2 mm. c Bonded specimen, the adhesive was directly applied over the covered surface. d Resin-dentin specimens after cutting for microtensile bond strenght testing. The area covered with liners is marked with black ink (arrow). Different distances from the blob are coloured red (1 mm), green (2 mm), and blue (3 mm)
Dentine areas of the control group (n = 6) were bonded using Prime&Bond NT and incrementally built up with Dyract eXtra shade A2 (both Dentsply Sirona, Konstanz, Germany; Table 1). Light-curing was performed for 20 s each (800 mW/cm2; Satelec Mini LED, KaVo, Biberach, Germany). The compomer restorative was applied using a CompoRoller (KerrHawe, Bioggio, Switzerland) in 1 mm layers. Specimens were then stored for 24 h in aqua dest. at 37 °C (Oven B20, Kulzer Dental, Hanau, Germany). In the six groups where a liner was used (n = 6 each), a 2-mm blob of liner was applied in the centre of the dentine disc prior to the application of the adhesive. Six different materials which are listed in Table 2 were used. The base materials were applied using a periodontal probe by use of an adhesive tape with a 2-mm hole (Fig. 1). After completed curing time (Table 2), another minute waiting time was added and then the specimens were bonded. Bonding and restorative procedure were exactly like in the control group. The location of the lining was marked with black ink (Fig. 1). Specimens were then fixed on metal moulds using glue wax (Supradent, Chemisches Dental-Labor Oppermann-Schwedler, Bonn, Germany) and cut in sticks (Isomet 1000 Low Speed Saw, Buehler; Isomet Wafering Blade Series 15LC, Buehler; Fig. 1). The distance between cuts was 1 mm, resulting in 0.7 × 0.7 mm stick diameters. Sticks were differently coloured in order to be able to backtrack its location in relation to the lining (Fig. 1, Fig. 2). Sticks were then removed from the glue wax using a scalpel (N015, Feather-Safety Razor Co. LTD, Osaka, Japan).
After exact measuring of height and width of the bonded interface, sticks were immediately loaded in tension (TC-550, Syndicad, Munich, Germany, crosshead speed 1 mm/min, 40 N) until failure occurred (TC-550 Measuring software V 2.1.0.4558, Certiga Engineering Solutions, Syndicad; Fig. 4). Pre-test failures were recorded as 0 MPa. Fracture analysis was carried out under 40× magnification in a fluorescence microscope (Nikon AZ100, Tokyo, Japan; Fig. 3). Judgement criteria were as follows: Fracture inside the adhesive, fracture in dentine, mixed fracture in adhesive and polyacid-modified composite, mixed fracture in adhesive and dentine, mixed fracture in adhesive, polyacid-modified composite, and dentine, mixed fracture in liner and dentine, and mixed fracture in liner, dentine, and adhesive. For statistical appraisal, adhesive fractures, cohesive fractures, and PTFs were pooled.
Selected specimens were investigated using SEM (Amray 1610 Turbo, Liebscher, Wetzlar, Germany) by means of epoxy replicas (Alpha Die MF, Schütz, Rosbach, Germany) sputtered with gold (Sputter Coater SC 502, Polaron, Fisons Instruments, New Haven, UK).When original specimens were evaluated, they were rinsed with NaOCl for 20 min and then washed in 20% HCl. Critical point drying was achieved by 20 min each in 60/70/80/90% ethanol and finally 60 min in 100% ethanol. Drying was carried out with Bis(trimethylsilyl)amine (Merk Schuchardt, Hohenbrunn, Germany).
Statistical analysis of data was computed using SPSS 15 (SPSS Inc, Chicago IL, USA). Kolmogorov-Smirnov test was used to evaluate normal distribution of data. This led to calculation of statistical differences using one-way ANOVA (mod. LSD, p < 0.05). Fracture modes were analysed with Mann-Whitney U test (p < 0.05).
Results
The boxplot diagram of microtensile bond strengths is displayed in Fig. 4. Independent of the distance to the applied cement, all liner groups exhibited inferior μ-TBS to dentine of primary teeth compared to the control group without protective liner (p < 0.05). In test groups, values were not significantly different in different distances from the blob (p > 0.05) (Fig. 5). The results are presented in Table 3.
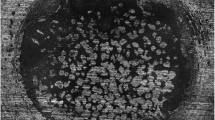
Qualitative SEM analysis of fractures specimens exhibited typically mixed fractures (Fig. 6) in the majority of cases. Fluorescence images helped to distinguish between dentine, polyacid-modified resin composite, and lining materials after microtensile bond strength testing.
Discussion
In this study, various protective liners were applied to primary molar dentine, followed by restoration with a compomer. It is evident that the reduction in bond strength for all liners compared to control is due to the reduced available for bonding dentine, irrespective of which material is used as a protective liner. Also compared to other studies dealing with self-etch adhesives in primary teeth, the test groups exhibit considerably lower results (Sardella et al. 2005; Krämer et al. 2014). It may be assumed that adjacent to the applied liner, bonding to the dentine may be compromised, but only there.
It was, therefore, assumed that a kind of gradient towards the periphery would occur, leading to an overall still acceptable bonding behaviour. In this context, microtensile bond strength evaluation is ideal, because it is possible to backtrack regional differences in dentine bonding behaviour over a complete "cavity" surface from its center to its periphery (Santschi et al. 2015).
Surprisingly, this described gradient from center to margin did not occur. Any application of a protective liner or a base material obviously interacted with the whole surface, resulting in significantly reduced dentine bonding all over the cavity (Fig. 5, Fig. 6). It may be concluded from the SEMs at first sight that there was a limited interaction, represented by the halo in Fig. 2. Reflected by focus on microtensile bond strength results, this was not the case. Beside pure microtensile bond strength results, also fractography is able to give hints on what exactly happened in the bonded interface (Fig. 3, Fig. 6).
A significant portion of cohesive failures in dentine or at least mixed failures can support those data, especially when experimental questions are involved like in the present investigation. However, neither light microscopic fracture analysis with fluorescence nor a closer look to failed interfaces under the SEM allowed a more detailed observation of results because the predominant number of bond failures was adhesive.
Conclusion
The results of this in vitro study evaluating the effect of different liners on the bond strength of a compomer to primary dentine reveal the following:
-
Protective liners reduce bonding to dentine of primary teeth.
-
The reduced bond strength seems to affect all the dentine, not only the lining area.
-
These materials should be used only when there are clear clinical indications.
Literatur
-
1.
Al-Zayer MA, Straffon LH, Feigal RJ, Welch KB. Indirect pulp treatment of posterior teeth: a retrospective study. Pediatr Dent. 2003;25(1):29-36.
-
2.
Boutsioukis C, Weber H, Lücker S, Frankenberger R, Krämer N. Comparative microtensile bond strength of universal adhesives in primary teeth. Oralprophylaxe Kinderzahnheilkd. 2017;39(3):110-5.
-
3.
Buyukgural B, Cehreli ZC. Effect of different adhesive protocols vs calcium hydroxide on primary tooth pulp with different remaining dentine thicknesses:24-month results. Clin Oral Investig. 2008;12(1):91-6.
-
4.
Casagrande L, Bento LW, Rerin SO, Lucas Ede R, Dalpian DM, de Araujo FB. In vivo outcomes of indirect pulp treatment using a self-etching primer versus calcium hydroxide over the demineralized dentine in primary molars. J Clin Pediatr Dent. 2008;33(2):131-5.
-
5.
Casagrande L, Bento LW, Dalpian DM, Garcia-Godoy F, de Araujo FB. Indirect pulp treatment in primary teeth: 4-year results. Am J Dent. 2010;23(1):34-8.
-
6.
dos Santos MP, Passos M, Luiz RR, Maia LC. A randomized trial of resin-based restorations in class I and class II beveled preparations in primary molars: 24-month results. J Am Dent Assoc. 2009;140(2):156-66.
-
7.
Duque C, Negrini Tde C, Hebling J, Spolidorio DM. Inhibitory activity of glass-ionomer cements on cariogenic bacteria. Oper Dent. 2005;30(5):636-40.
-
8.
Duque C, Negrini Tde C, Sacono NT, Spolidorio DM, de Souza Costa CA, Hebling J. Clinical and microbiological performance of resin-modified glass-ionomer liners after incomplete dentine caries removal. Clin Oral Investig. 2009;13(4):465-71.
-
9.
Falster CA, Araujo FB, Straffon LH, Nor JE. Indirect pulp treatment: in vivo outcomes of an adhesive resin system vs calcium hydroxide for protection of the dentine-pulp complex. Pediatr Dent. 2002;24(3):241-8.
-
10.
Foley J, Evans D, Blackwell A. Partial caries removal and cariostatic materials in carious primary molar teeth: a randomised controlled clinical trial. Br Dent J. 2004;197(11):697-701.
-
11.
Frankenberger R, Perdigao J, Rosa BT, Lopes M. "No-bottle" vs "multi-bottle" dentin adhesives-a microtensile bond strength and morphological study . Dent Mater. 2001;17(5):373-80.
-
12.
Franzon R, Casagrande L, Pinto AS, Garcia-Godoy F, Maltz M, de Araujo FB. Clinical and radiographic evaluation of indirect pulp treatment in primary molars: 36 months follow-up. Am J Dent. 2007;20(3):189-92.
-
13.
Fuks AB. Vital pulp therapy with new materials for primary teeth: new directions and treatment perspectives. Pediatr Dent. 2008;30(3):211-9.
-
14.
Itota T, Nakabo S, Torii Y, Narukami T, Doi J, Yoshiyama M. Effect of fluoride-releasing liner on demineralized dentine. Quintessence Int. 2006;37(4):297-303.
-
15.
Kramer N, Frankenberger R. Compomers in restorative therapy of children: a literature review. Int J Paediatr Dent. 2007;17(1):2-9.
-
16.
Krämer N, Tilch D, Lucker S, Frankenberger R. Status of ten self-etch adhesives for bonding to dentine of primary teeth. Int J Paediatr Dent. 2014;24(3):192-9.
-
17.
Lewis BA, Burgess JO, Gray SE. Mechanical properties of dental base materials. Am J Dent. 1992;5(2):69-72.
-
18.
Marchi JJ, de Araujo FB, Froner AM, Straffon LH, Nor JE. Indirect pulp capping in the primary dentition: a 4 year follow-up study. J Clin Pediatr Dent. 2006;31(2):68-71.
-
19.
Pashley DH, Carvalho RM, Sano H, Nakajima M, Yoshiyama M, Shono Y, Fernandes CA, Tay F. The microtensile bond test: a review. J Adhes Dent. 1999;1(4):299-309.
-
20.
Pinto AS, de Araujo FB, Franzon R, Figueiredo MC, Henz S, Garcia-Godoy F, et al. Clinical and microbiological effect of calcium hydroxide protection in indirect pulp capping in primary teeth. Am J Dent. 2006;19(6):382-6.
-
21.
Santschi K, Peutzfeldt A, Lussi A, Flury S. Effect of salivary contamination and decontamination on bond strength of two one-step self-etching adhesives to dentine of primary and permanent teeth. J Adhes Dent. 2015;17(1):51-7.
-
22.
Sardella TN, de Castro FL, Sanabe ME, Hebling J. Shortening of primary dentine etching time and its implication on bond strength. J Dent. 2005;33(5):355-62.
-
23.
Schmalz G, Hiller KA, Nunez LJ, Stoll J, Weis K. Permeability characteristics of bovine and human dentine under different pretreatment conditions. J Endod. 2001;27(1):23-30.
-
24.
Vij R, Coll JA, Shelton P, Farooq NS. Caries control and other variables associated with success of primary molar vital pulp therapy. Pediatr Dent. 2004;26(3):214-20.
Oralprophylaxe Kinderzahnheilkd 2021 · 43: 42-49 · https://doi.org/10.1007/s44190-021-0016-0 Erstveröffentlicht in European Archives of Paediatric Dentistry. Die Erstveröffentlichung ist erhältlich bei Springer über https://doi.org/10.1007/s40368-020-00601-2 Eingereicht: 05.08.2020 / Angenommen: 18.12.2020 / Online Publiziert: 03.02.2021 · © European Academy of Paediatric Dentistry 2021
Acknowledgments
The authors would like to thank Ms. Ingrid Heidmann for the fluorescence microscope and SEM imaging and Mr. Johannes Herrmann for the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
RF has received research Grants from following companies: Dentsply, 3M, Ivoclar, GC, Kulzer. NK has received research grants from 3M, Pulpdent, GC, Dentsply. RF has received a speaker honorarium from Dentsply, Ivoclar, 3M, Kulzer, and ADS. NK has received speaker honorarium from Dentsply, Kulzer, GC, 3M, and ADS. SN and SL do not have any conflict of interest.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved with AZ 190/14 by the Ethics committee of the Justus-Liebig-University Giessen, Germany.
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Frankenberger, R., Nassiri, S., Lücker, S. et al. The effect of different liners on the bond strength of a compomer to primary teeth dentine: in vitro study. Oralprophylaxe Kinderzahnheilkd 43, 42–49 (2021). https://doi.org/10.1007/s44190-021-0016-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44190-021-0016-0