Abstract
Purpose
Multi-institutional, prospective trial aimed to assess the impact of one of the two targeted interventions on burnout in general surgery residents.
Methods
Residents at 7 general surgery programs were invited to complete an electronic survey including the 2-item Maslach Burnout Inventory (MBI) and other assessments with validity evidence. Based on program-aggregated survey responses, programs were assigned to either a gratitude practices or job crafting (JC) intervention. Paired surveys were also conducted post-intervention. Statistical analysis was conducted using Kruskal–Wallis, Wilcoxon–Mann Whitney, and Wilcoxon signed-ranks tests, as appropriate, with the primary outcome of summed MBI score (scale 0–12).
Results
Of the 90 residents with complete pre- and post-intervention data (50.3%), 3 programs participated in the gratitude intervention (35.6%) and 4 programs participated in the JC intervention (64.4%). Initial mean burnout scores in the gratitude and JC groups were 6.0 and 5.3, respectively (p = 0.33), with no significant differences based on age, gender, institution, or PGY year. Pre- and post-intervention burnout scores were not different overall (5.6 vs 5.8, p = 0.55); neither was change in burnout scores among interventions (gratitude 6.0–5.8 vs JC 5.3–5.8, p = 0.35). On subset analysis, residents with high pre-intervention burnout risk experienced a statistically significant decrease in burnout (8.7–7.7, p = 0.02); however, the opposite occurred in those with low burnout risk pre-intervention (3.7–4.6, p = 0.02).
Conclusions
Gratitude and job crafting practices served as therapeutic interventions for individuals with high risk of burnout, but did not prevent progression in those with low burnout risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Burnout is defined as an overwhelming or unmanageable level of stress related to one’s work, and its prevalence has been well documented in the medical field [1,2,3]. Burnout in medical training occurs as early as medical school and remains throughout residency with a reported prevalence ranging from 42 to 69% in general surgery residents [4,5,6,7,8]. The consequences of burnout directly affect the physician, but also negatively impact health care economics and patient care through decreases in patient care satisfaction as well as increased medical errors [2, 9,10,11]. Ultimately, decreased productivity and increased costs related to burnout negatively impact the health care system in its entirety [9]. Resident physicians plagued by burnout are more likely to suffer from mental illness including substance abuse and suicide compared to the general population [2, 7]. This cycle self-perpetuates with poor outcomes increasing physician distress and furthering burnout [7, 10].
Burnout is mediated by both intrinsic qualities and extrinsic circumstances which may be targeted through interventions [2, 9, 12]. Both intrinsic and extrinsic factors have been established to predict burnout with positive experiences being more impactful than negative experiences [13]. Intrinsic qualities which are protective against burnout include emotional intelligence, resilience, and mindfulness [2, 14,15,16]. One often-studied approach to enhancing individuals’ intrinsic abilities to mitigate burnout harnesses the power of positivity to focus on “three good things” [17]. The “three good things” intervention was initially shown to increase happiness and decrease depression in the general population but has been applied to the health care setting with encouraging outcomes in well-being [17, 18]. “Three good things” content analysis identified three primary themes in a health care setting: strong support system, overall positive workday, and autonomy of personal time [18]. It was concluded that “three good things” could also be utilized as an intervention in this population to increase awareness of positive occurrences in one’s day [18].
The extent of external resources and job demands also impact burnout [9, 12]. Institutional-wide efforts such as team building, communication seminars, and duty hour limitations removes the burden from health care workers to resolve burnout on their own [12, 19, 20]. Physician well-being is frequently represented as work engagement in the health care setting [21]. In a review article on physician well-being and patient care, it was shown that work engagement improves patient satisfaction and adherence and decreases medical errors [21]. Work engagement can be interpreted as the antithesis of burnout and targeted by job crafting interventions [21].
Collective efforts to improve well-being are needed, but there is a gap of knowledge as to how to effectively address the problem [19, 20]. The purpose of this multi-institutional, prospective trial aimed to assess the impact on burnout following a targeted intervention, gratitude practice or job crafting, in general surgery residents in the United States.
Methods
Participation
This prospective intervention trial was conducted in 2019, wherein general surgery residents at the University of Alabama at Birmingham, University of Cincinnati, Emory University, University of Michigan, Pennsylvania State University. University of South Alabama, and Wake Forest University were invited to participate in one of the two interventions targeted to reduce burnout, with electronic surveys before and after. The phases of the study occurred within the same academic year, with the pre-intervention survey occurring in September to October, the intervention in January–February, and the post-intervention survey in late April to June. Class sizes at these 7 university and university affiliated institutions ranged from 5 to 9 categorical residents. Residents in all levels of training and participating in both clinical and research activities were included. Ten-dollar gift certificates were awarded to those who participated in both pre- and post-surveys. Additionally, location-specific resident- and faculty member-champions were selected to encourage participation. Informed consent was completed by participants at the initiation of the electronic survey. Institutional review board approval was obtained at the primary study site for use among all programs.
Survey tool
Electronic surveys were distributed to residents before and after participation in an intervention. The surveys gathered information on internal and external measures of wellness including the Brief Emotional Intelligence Scale (BEIS), Cognitive Affective Mindfulness Scale (CAMS), Connor–Davidson Resilience Scale (CD-RISC2), Utretch Work Engagement Scale (UWES-9), Job Resources Scale (JDRS), and 2-item Maslach Burnout Inventory (MBI) [22,23,24,25,26,27,28]. The BEIS is a 10-item measure of emotional intelligence measuring both appraisal and regulation of one’s own and others’ emotions [22]. Mindfulness was measured using the CAMS-R based on the four constructs of attention, focus, awareness, and acceptance [23]. The CD-RISC2 utilizes a 2-item questionnaire to measure resilience [24]. Vigor, absorption, and dedication are the foundation for work engagement measured by UWES-9 [25]. The JDRS is a measure of resources available at the workplace [26]. The primary outcome of interest, burnout, was measured with the 2-item MBI [27,28,29]. Results of the initial survey have been previously published [15].
The 2-item MBI encompasses two primary domains of burnout, emotional exhaustion and depersonalization. The two MBI questions represent each domain: “How often have you felt burned out?” and “Have you worried that your work is hardening you emotionally?”. Responses were recorded on a 0–6 frequency scale of never to daily. The 2-item MBI represented as a summed score has been shown to correlate closely with the full MBI in a health care setting [28]. Additionally, single-item questions representing emotional exhaustion and depersonalization predict the outcomes of health professionals in a similar manner to the full MBI-health service survey [29].
Study protocol
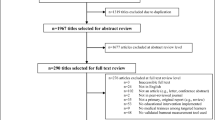
One of the two interventions, gratitude practice or job crafting, were assigned at a program level based on whether the mean of initial burnout scores among participants at the program were correlated with internal versus external factors (Fig. 1). Internal factors consisted of measures of emotional intelligence, mindfulness, and resilience, whereas external factors included work engagement and job resources. Programs where most residents’ initial survey results were low in internal factors were assigned the gratitude intervention. On the other hand, programs where most residents’ initial survey results were low in external factors were assigned the job crafting intervention. Duration of interventions was determined based on how they have historically been implemented [18, 30]. Instructions were distributed electronically via email, and participants engaged in their interventions virtually. Both groups received reminders in an effort to enhance participation.
The goal of the gratitude intervention was to address internal factors impacting burnout by focusing on positivity. Inspired by “Three Good Things,” participants in the gratitude intervention were instructed to document three positive occurrences in their day, every day, for 14 days [17]. Participants were encouraged to reflect on positivity and its causal relationship rather than fixate on negativity they may have experienced [17]. The job crafting intervention focused on finding the balance between job demands and resources [30]. In alignment with the job crafting technique, participants were encouraged to seek autonomy, feedback, and professional development [30]. Emails were distributed weekly over six weeks providing step-by-step instructions to develop job crafting skills. Each week worked toward different goals ultimately leading to a balance between job and personal demands to promote growth and satisfaction in the workplace.
Outcome measures and statistical analysis
Low risk for burnout was defined as a summative score less than 7 and high risk for burnout greater than 6. This cut-off has been established to have a sensitivity of 60.1 and specificity of 99.7 [28]. High burnout within the individual domains was defined as a score greater than 3 as established in previous studies to be associated with high risk of burnout [31]. Change in burnout was defined as post-intervention score minus pre-intervention score with an increase indicated by a positive change and a decrease signified by a negative change. Demographic information was also collected including age, post-graduate year (PGY), gender, and status as a clinical or research resident. Notably race and ethnicity were not included in our survey. Statistical analysis was conducted using StataSE version 17 (StataCorp, College Station, TX). Categorical variables were analyzed with chi-square tests and ordinal variables with the Wilcoxon signed-ranks, Wilcoxon–Mann Whitney, or Kruskal–Wallis tests, as appropriate.
Results
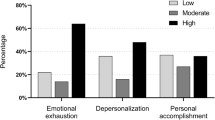
One hundred and seventy-five residents completed > 80% of the initial survey, and 90 residents completed > 80% of both the pre- and post-intervention survey resulting in a response rate of 51.4% Participants were nearly equally distributed between female (53%) and male (47%) with the majority of participants (57%) between the ages of 26 and 30 years old. There was representation throughout all years of residency, and 73% of participants were clinically active residents. Mean summed burnout score across the entire study population before intervention was 5.57, with 62% of residents being at low risk for burnout. High burnout risk for emotional exhaustion and depersonalization was experienced by 29% and 34% of respondents, respectively. No significant differences in initial burnout scores based on gender, age, institution, PGY, or clinical versus research status were identified among the population overall nor within the high-risk group (Table 1).
Based on the correlation of internal versus external factors and initial burnout, 3 programs were assigned to the gratitude intervention, while 4 programs participated in the job crafting intervention. There were also no significant differences when comparing pre- and post-intervention burnout scores among the population overall (p = 0.55) (Table 2); nor was there a difference in change in burnout on bivariate analysis examining gender, age, institution, or clinical status (p > 0.05 for all). However, within the depersonalization domain, there was a significant difference in PGY (p = 0.003). PGY-1 and PGY-5 residents experienced an increase in depersonalization scores, whereas PGY-2 through PGY-4 residents’ depersonalization scores decreased. There were no differences in change in burnout scores comparing the different intervention groups (p = 0.35).
Subset analysis revealed that individuals with high burnout risk experienced a significant decrease in burnout from pre-intervention to post-intervention (8.71–7.71, p = 0.02). However, participants with low burnout risk had a significant increase in burnout from pre-intervention to post-intervention (3.66–4.64, p = 0.02) (Table 3). These results are redemonstrated by significant difference in change scores when comparing participants with initially low versus high risk for burnout (p = 0.046) and for depersonalization. (p < 0.001) (Fig. 2). Participants with initially low risk experienced an increase in burnout and depersonalization. Whereas participants with initially high risk experienced a decrease in burnout and depersonalization following the intervention (Fig. 2). This pattern was not statistically significant in the emotional exhaustion domain (p = 0.12).
Discussion
The consequences of physician burnout in medicine are far-reaching, affecting not only the individual but also patient care. With the goal of mitigating these consequences, our prospective, multi-institutional study implemented two separate interventions, aimed to modulate external factors through job crafting or internal factors through gratitude practice. We found these interventions successful at decreasing burnout in participants who had an initial high risk of burnout, specifically in the domain of depersonalization. In early descriptions of burnout, depersonalization was identified as the most tightly associated with those in the human services profession, and therefore, it is not surprising our population experienced the largest mean change in burnout within this domain [27]. Although these interventions may be therapeutic to those who are high risk for burnout, the same was not observed in participants with initially low burnout risk, whose risk of burnout increased over the study period.
Although our study did not find a difference between job crafting and gratitude interventions, overall “positive psychology interventions” appear to have the greatest promise when targeting the individual [19]. Ultimately, integration of both individually and institutionally focused interventions is most likely to be successful in reducing burnout, along with those that include multiple goals of treatment [12, 20]. However, these gains in burnout reduction are often small, with one meta-analysis demonstrating the absolute reduction of burnout to be 10% [8, 12, 20]. However, even these small changes can have significant impacts on outcomes including medical errors, suicidal ideation, and professional effort [12, 32,33,34]. While the change in burnout score in our study was only one point before and after the intervention, this is still an encouraging step in the right direction to set the trajectory for improved patient outcomes and physician well-being.
It has been reported that specific demographic factors can contribute to burnout [3, 9]. Burnout has been shown to fluctuate during residency, in response to the specific demands and stressors experienced by PGY [32]. We observed a difference in change in depersonalization scores among PGY, but not burnout overall or emotional exhaustion. Residents during the middle of their training had a decrease in depersonalization following their respective intervention, whereas PGY-1 and PGY-5 experienced an increase. Longitudinal variability in burnout throughout general surgery residency training has been previously documented with depersonalization and emotional exhaustion peaking early in training [35]. The interpretation of our results is limited to change scores rather than a longitudinal trend. More research is needed to fully describe the relationship between PGY and burnout.
Our study attempted to describe residents who were at high risk of burnout in hopes of taking preventative measures specific for these populations. Our survey did not obtain the race/ethnicity of participants, so this remains an unexplored factor in this study. Previous studies have concluded that being female increases likelihood of burnout, although this has not been consistent across all studies [15, 36, 37]. Female physicians face unique challenges in the medical field related to gender bias, sexual harassment, wage gaps, and family planning [38]. Previous studies which support differences in burnout based on gender were overrepresented by male gender [36] or underrepresented in general surgeons [37]. In our analysis of participants with high risk for burnout pre-intervention, there were no significant differences within demographics including gender. However, awareness of the potentially increased risk for burnout among marginalized groups at an institutional level may help overcome the distinction of female and under-represented physicians as high-risk populations for burnout [38].
By stratifying our study population into high and low risk individuals, we illuminated a dichotomy of responses. Those with high risk of burnout benefited from a wellness intervention while those with low risk suffered, regardless of the type of intervention in which they were assigned. It is proposed by some in the medical community that wellness interventions do not address the underlying problem, and instead contribute to physician work-load [39, 40]. Our study supports that wellness interventions should not be implemented broadly or blindly. Rather they should address the needs of the program and target individuals at high risk of burnout. This approach proved to be beneficial for those at high risk of burnout, and it would also spare those at low risk of burnout.
Our study aimed to answer the need for targeted intervention trials aimed at reducing physician burnout and included a sample of trainees from geographically distributed areas. We revealed a unique risk stratification for burnout which further elucidated the interventions’ effects on specific sub-populations. However, it is also important to recognize the limitations of our study. All surveys and interventions were distributed electronically and assigned at the program level rather than the individual level for logistical feasibility. Hence, some individuals received interventions that did not target their individual contributions to burnout. This could be a consideration for more individually targeted studies. The retrospective, self-administered surveys can be limited by both recall and selection bias. In particular, our study population was > 50% female, while general surgery residents in 2019 nationally were only 43.1% female [41]. Furthermore, participation in the interventions and progress in the electronic surveys were self-monitored by participants and not collected to assess their completion. There also may be other unmeasured factors contributing to burnout in this population. Regarding our design, we did not include a control group which limits our analysis. Due to the high prevalence of burnout in our study population, it was deemed unethical to withhold a potentially efficacious intervention. This is an opportunity for future studies to consider implementing a crossover trial. Finally, we only received assessment of burnout over a short period of time.
In conclusion, our study utilized interventions targeted at either internal or external factors that can mitigate burnout, determining that these interventions were therapeutic for those with high burnout risk but not preventative of burnout for those with initially low risk. Moving forward, training programs could work to identify residents at high risk of burnout and target their participation in therapeutic initiatives. Future interventions should consider incorporating both structural and individual interventions over a longer period to assess longevity of intervention outcomes.
Data, materials and/or code availability
Available upon request.
References
Burn-out an “occupational phenomenon”: International Classification of Diseases. World Health Organization. 2019. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases. Accessed 27 April 2022.
Lebares CC, Guvva EV, Ascher NL, O’Sullivan PS, Harris HW, Epel ES. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018. https://doi.org/10.1016/j.jamcollsurg.2017.10.010.
Kumar S. Burnout and doctors: prevalence, prevention, and intervention. Healthc. 2016. https://doi.org/10.3390/healthcare4030037.
dos Santos Boni RA, Paiva CE, de Oliveira MA, Lucchetti G, Fregnani JHTG, Paiva BSR. Burnout among medical students during the first years of undergraduate school: Prevalence and associated factors. PLoS ONE. 2018. https://doi.org/10.1371/journal.pone.0191746.
Dyrbye LN, Power DV, Massie FS, et al. Factors associated with resilience to and recovery from burnout: a prospective, multi-institutional study of US medical students. Med Educ 2010; https://doi-org.ezproxy3.lhl.uab.edu/https://doi.org/10.1111/j.1365-2923.2010.03754.x
Elmore LC, Jeffe DB, Jin L, Awad MM, Turnbull IR. National survey of burnout among US general sur- gery residents. J Am Coll Surg. 2016. https://doi.org/10.1016/j.jamcollsurg.2016.05.014.
Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, Souza T, Gonçalves AK. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS ONE. 2018. https://doi.org/10.1371/journal.pone.0206840.
Regehr C, Dylan G, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians. J Nerv Ment Disord. 2014. https://doi.org/10.1097/NMD.0000000000000130.
West CP, Dyrebye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018; https://doi-org.ezproxy3.lhl.uab.edu/https://doi.org/10.1111/joim.12752.
Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, Collicott P, Novotny PJ, Sloan J, Freischlag J. Burnout and medical errors among American surgeons. Ann Surg. 2010. https://doi.org/10.1097/SLA.0b013e3181bfdab3.
Scheepers RA, Boerebach BC, Arah OA, Heineman MJ, Lombarts KMJMH. A systematic re- view of the impact of physicians’ occupational well-being on the quality of patient care. Int J Behav Med. 2015; https://doi.org/10.1007/s12529-015-9473-3.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016. https://doi.org/10.1016/S0140-6736(16)31279-X.
Lindeman B, Petrusa E, McKinley S, et al. Association of burnout with emotional intelligence & personality in surgical residents: can we predict who is most at risk? J Surg Educ. 2017;74(6):e22–30.
Lindeman B, Petrusa E, McKinley S, Hashimoto DA, Gee D, Smink DS, Mullen JT, Phitayakorn R. Association of burnout with emotional intelligence and personality in surgical residents: can we predict who is most at risk? J Surg Educ. 2017. https://doi.org/10.1016/j.jsurg.2017.11.001.
Mullins CH, Gleason F, Wood T, Baker SJ, Cortez AR, Lovasik B, Sandhu G, Cooper A, Hildreth AN, Simmons JD, Delman KA, Lindeman B. Do internal or external characteristics more reliably predict burnout in resident physicians: a multi-institutional study. J Surg Educ. 2020. https://doi.org/10.1016/j.jsurg.2020.09.024.
Gleason F, Malone E, Wood L, Baker SJ, Hollis RH, Richman JS, Chu DI, Lindeman B. The job demands-resources model as a framework to identify factors associated with burnout in surgical residents. Surg Res. 2020. https://doi.org/10.1016/j.jss.2019.10.034.
Seligman MEP, Steen TA, Park N, Peterson C. Positive psychology progress empirical validation of interventions. Am Psychol. 2005. https://doi.org/10.1037/0003-066X.60.5.410.
Rippstein-Leuenberger K, Mauthner O, Sexton JB, Schwendimann R. A Qualitative analysis of three good things intervention in healthcare workers. BMJ Open. 2017. https://doi.org/10.1136/bmjopen-2017-015826.
Murray M, Murrah L, Donnelly M. Systematic review of interventions to improve the psychological well-being of general practitioners. BMC Fam Pract. 2016. https://doi.org/10.1186/s12875-016-0431-1.
Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, Dawson S, van Marwijk H, Geraghty K, Esmail A. Controlled interventions to reduce burnout in physicians a systematic review and meta-analysis. JAMA Intern Med. 2017. https://doi.org/10.1001/jamainternmed.2016.7674.
Scheepers RA. Physicians’ professional performance: an occupational health perspective. Perspect Med Educ. 2017. https://doi.org/10.1007/s40037-017-0382-9.
Davies KA, Lane AM, Devonport TJ, Scott JA. Validity and reliability of a Brief Emotional Intelligence Scale (BEIS-10). J Individ Differ. 2010. https://doi.org/10.1027/1614-0001/a000028.
Feldman G, Hayes A, Kumar S, Greeson J, Laurenceau JP. Mindfulness and emotional regulation: the development and initial validation of the cognitive and affective mindfulness scale-revised (CAMS-R). J Psychopathol Behav Assess. 2007. https://doi.org/10.1007/s10862-006-9035-8.
Vaishnavi S, Connor K, Davidson JRT. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: Psychometric properties and applications in psychopharmacologic trials. Psych Res. 2007. https://doi.org/10.1016/j.psychres.2007.01.006.
Schaufeli WB, Bakker AB, Salanova M. The measurement of work engagement with a short questionnaire: a cross-national study. Educ Psychol Meas. 2006. https://doi.org/10.1177/0013164405282471.
Crawford ER, LePine JA, Rich BL. Linking job demands and resources to employee management and burnout: A theoretical extension and meta-analytic test. J Appl Psychol. 2010. https://doi.org/10.1037/a0019364.
Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
Li-Sauerwine S, Rebillot K, Melamed M, Addo N, Lin M. A 2-question summative score correlates with the maslach burnout inventory. West J Emerg Med. 2020. https://doi.org/10.5811/westjem.2020.2.45139.
West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012. https://doi.org/10.1007/s11606-012-2015-7.
van Wingerden J, Bakker AB, Derks D. The longitudinal impact of a job crafting intervention. Eur J Work Organ Psychol. 2017. https://doi.org/10.1080/1359432X.2016.1224233.
West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318–21. https://doi.org/10.1007/s11606-009-1129-z.
Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, Collicott P, Novotny PJ, Sloan J, Freishlag J. Burnout and medical errors among American surgeons. Ann Surg; 2010. doi: https://doi.org/10.1097/SLA.0b013e3181bfdab3.
Shanafelt TD, Balch CM, Dyrbye L, Bechamps G, Russell T, Satele D, Rummans T, Swartz K, Novotny PJ, Sloan J, Oreskovich MR. Suicidal ideation among american surgeons. Arch Surg. 2011. https://doi.org/10.1001/archsurg.2010.292.
Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, Sloan JA, Swensen SJ, Buskirk SJ. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016. https://doi.org/10.1016/j.mayocp.2016.02.001.
Cortez AR, Winer LK, Kassam A, Hanseman DJ, Kuethe JW, Sussman JJ, Quillin III C. Exploring the relationship between burnout and grit during general surgery residency: A longitudinal, single-institution analysis. Am J Surg; 2020. https://doi.org/10.1016/j.amjsurg.2019.09.041.
Shanafelt TD, Oreskovich MR, Dyrbye LN, Satele DV, Hanks JB, Sloan JA, Balch CM. Avoiding burnout: the personal health habits and wellness practices of US surgeons. Ann Surg. 2012. https://doi.org/10.1097/SLA.0b013e31824b2fa0.
Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Satele DV, Carlasare LE, Dyrbye LN. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019; https://doi.org/10.1016/j.mayocp.2018.10.023.
Stonnington CM, Files JA. Burnout in women physicians: prevention, treatment, and management. Springer International Publishing AG; 2020.
Dr.Glaucomflecken. How to Fix Burnout. Jan 28, 2022. https://www.youtube.com/watch?v=MUVzRs3E5g4.
Dr. Glaucomflecken. The Cure for Burnout. April 12, 2022. https://www.youtube.com/watch?v=Oi8fnQjo90E.
ACGME Residents and fellows by sex and specialty, 2019. In: physician specialty data report. Association of American Medical Colleges. 2019 https://www.aamc.org/data-reports/interactive-data/acgme-residents-and-fellows-sex-and-specialty-2019. Accessed October 6, 2022.
Funding
This study was funded by the ASE MERG- Multi-institutional Education Research Grant.
Author information
Authors and Affiliations
Contributions
All authors contributed either to the study conception and design or material preparation, data collection and analysis. The first draft of the manuscript was written by Garrett Barnes. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
We have no competing interests to declare that are relevant to the content of this article.
Ethical approval
Approval was obtained from the ethics committee of the primary study site. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barnes, G.A., Baker, S.J., Cortez, A.R. et al. A therapeutic intervention for burnout in general surgery residents. Global Surg Educ 2, 25 (2023). https://doi.org/10.1007/s44186-023-00100-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44186-023-00100-0