Abstract
Background
Average bone healing times of common fractures in adults ranges from 3 to 12 weeks and is location dependent. Platelet Rich Plasma (PRP) stimulates natural healing process through growth factors contained in platelets and has been employed for the same in delayed unions.
Methods
All patients > 18 years and documented delayed union were included in the study. Patients were followed up monthly after each Leucocyte-rich PRP (LR-PRP) injection and a decision for repeat PRP injection was taken on basis of visible impression in radiograph after previous injection.
Results
Total 36 patients were studied in which 5 patients were lost to follow-up. Union was achieved in 28/31 (90.3%). 20 (71.4%) patients required only single PRP injections. 4 (14.3%) patients required 2 PRP injections, 3 (10.7%) patients required 3 PRP injections and 1 (3.6%) patient required 4 PRP injection. There was no significant correlation of number of PRPs to time from 1st PRP-union or time from last PPR- union.
Conclusion
Single/multiple dose percutaneously administered LR-PRP can be used as a fruitful alternative to catalyze union in patients having delayed union irrespective of site of injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A bone heals by direct and indirect method and is often affected by biology and stability at fracture site [1]. It is a complex physiological process involving coordinated interaction of hematopoetic and immune cells within bone marrow, in conjuction with vascular and skeletal cell precursors which are dependent on a gamut of cytokines and growth factors [2].
Average healing times of common fractures have been suggested in literature as follows: Phalanges (3 weeks), metacarpals (4–6 weeks), distal radius (4-6 weeks), lower arm (8–10 weeks), humerus (8–10 weeks), tibial shaft (10 weeks), femoral neck (12 weeks) and femoral shaft (12 weeks)[1, 3, 4]. Delayed union, by definition, is present when an adequate period of time has elapsed since the initial injury without achieving bone union.
Platelet Rich Plasma (PRP) stimulates natural healing process through growth factors contained in platelets. When PRP is injected at the fracture site, not only the process of physiological healing is accelerated but also tends to provide an anti-bacterial effect [3, 5]. Various studies have reported a beneficial effect of PRP in both nonunions and delayed unions [6,7,8,9,10,11].
Material and Methods
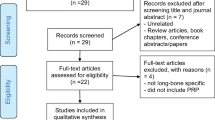
The study was conducted on patients presenting to orthopedics OPD at our tertiary care center either operated at our center or elsewhere. The inclusion criteria included: (i) age > 18 years, (ii) documented delayed union at follow-up. Exclusion criteria was (i) no signs of union in follow-up, (ii) pathological fracture, (iii) lost to follow-up.
All patients meeting the inclusion criteria, giving a informed consent were included in the study. Union was evaluated on orthogonal radiographs and was defined as union of at least 3 cortices and no pain at fracture site [12,13,14]. Delayed union was defined as inadequate but some consolidation (< 3 cortices on orthogonal views) on follow-up radiographs taken at least 2 months after from date of surgical fixation and no pain at fracture [8, 15, 16] Patients were followed up monthly after eachLeucocyte rich PRP (LR-PRP) injection and a decision for repeat LR-PRP injection was taken on basis of visible impression in radiograph after previous injection. Time to union from surgery, from 1stLR-PRP and last LR-PRP injection was noted along with number of LR-PRP injections required to do so. The endpoint was radiographic union.
Preparation of LR-PRP: 10 ml of autologous blood was withdrawn in ACD tubes and PRP was prepared using double spin method protocol standardized by the institute. Autologous blood was first centrifuged in centrifuge (Remi R8 C fixed angle microcentrifuge) at 1500 rpm for 15 min from which plasma was separated then it was again centrifuged at 2500 rpm for 10 min. Prepared PRP was later kept in platelet agitator (Terumo Penol platelet incubator and agitator PI400) for 30 min for activation.
Method of LR-PRP injection: LR-PRP injection was given under aseptic conditions. The needle was directed under radiographic guidance towards the fracture site. The final injection was given at the center of fracture.
Results
Total 36 patients were studied in which 5 patients were lost to follow-up (total sample n = 36; excluded n = 5; total patients included n = 31). Mean age of patients were 42.68 ± 17.44 years (range 18–74 years). There were 24 (85.7%) male patients and 4 (14.3%) female patients. 5 (17.9%) patients had open injury while 23 (82.1%) patients had closed injury. 17 (60.7%) patient had affected side as left, 10 (35.7%) had right side affection and 1 patient had bilateral affection.
3/31 (9.7%) patients showed no signs of union despite PRP (total patients evaluated for outcome n = 28). 1 patient had equivocal signs union of proximal tibia with only 2 cortices were united, but is walking pain-free. Two patients had nonunion but did not opt for any further intervention. Union was achieved in 28/31 (90.3%) and were used for statistical analysis.
20 (71.4%) patients required only single LR-PRP injections. 4 (14.3%) patients required 2 LR-PRP injections, 3 (10.7%) patients required 3 LR-PRP injections and 1 (3.6%) patient required 4 LR-PRP injection. There was no significant correlation of number of LR-PRPs to time from 1st PRP-union or time from last PRP- union. Independent samples test showed no significant difference for distribution of values across various fracture sites for time from surgery to union (p = 0.51), time from 1st PRP to union (p = 0.70), time from last LR-PRP to union (p = 0.63) and no. of LR-PRPs administered to achieve union (p = 0.75). Table 1 shows in detail the parameters studied. Figures 1 and 2 are showing radiographic effect of LR-PRP on healing following delayed union.
Figure showing immediate postoperative radiograph A of 42 year old male with distal tibia spiral fracture treated with open reduction and internal fixation with medial distal tibial plate. Figure B shows 3 months postoperative radiograph demonstrating delayed union following which PRP was given and figure C shows 1 month postinjection radiograph demonstrating union
Figure showing immediate postoperative radiograph A of 34 year old female with distal tibia shaft fracture treated with closed reduction and internal fixation with intramedullary interlocking nail and distal shaft fibula treated with open reduction and internal fixation with 6 hole DCP. Figure B shows 5 months postoperative radiograph demonstrating delayed union following which PRP was given and figure C shows 2 month postinjection radiograph demonstrating union
Discussion
Delayed union and nonunion are two phases of bone healing disorders [9]. Impaired healing can occur in 10–15% of fracture patients leading to delayed union or non-union [17]. Impaired healing can show various characteristics such as persistent pain at fracture site and poor callus formation seen as a persistent radiolucent line on radiograph [6, 18].
Many modalities have been reported to deal with delayed union. Often a bone graft or bone graft substitute is used to act as a biologic stimulus. Various substitutes in recent times have been developed vastly. Bioactive factor such as BMP-2 has been confirmed to promote healing of bone and has also been approved by US FDA for the same. PRP is being widely used as a new safe and cheaper experimental tool to achieve union in such cases. PRP has been used a sole modality of intervention or along with other modalities such as biomaterial scaffolds, bone grafting and mesenchymal stem cells [10, 19, 20]. Both PRP (LR-PRP) and Platelet concentrates or LP-PRP has been used in for delayed unions and non-unions worldwide, although the data is inadequate for a proper comparison due to difference in method of preparation and inadequate data on platelet concentration in PRP used [3, 8, 9, 15, 21].
Healing occurs in three phases: inflammation, proliferation and remodeling. Oryanet al in a review on effect of PRP on bone healing showed that various growth factors play an important role such as platelet derived growth factor, vascular endothelial growth factor, transforming growth factor –beta, fibroblast growth factor, insulin-like growth factor, epidermal growth factor and platelet factor-4 [22]. Platelets release growth factors and cytokines when activated, which regulates the inflammatory phase of bone healing and modulates soft and hard callus development and bone remodelling [23]. Growth factors can effectively influence bone healing due to their major regulatory function on cell migration, proliferation, differentiation, and maturation, as well as matrix synthesis and remodelling [22, 24].
Healing rate and time taken to unite are two common determinants that has been used in literature to determine the efficacy of PRP in delayed union [8, 9, 16]. Samuel et al. studied 40 delayed unions and showed a union rate of 78% with PRP compared to 59% in control group. The mean time to fracture union following a PRP injection was 15.33 ± 9.91 weeks (approximately 3.5 ± 2.25 months) [8]. Though the control group in study by Samuel et al. showed a lesser union rate, it also showed a non-significant tendency of earlier union without PRP [8]. This may be an incidental statistical finding.Bielecki et al showed a mean union time of 9.3 weeks (5–12 weeks) following PRP injection in delayed union with all delayed unions achieving union (100% healing rate) [16]. This is comparable to our study which showed union following 1st PRP injection at mean duration of 4.82 ± 3.49 months. A higher duration in our study may be due to COVID19 related delays in getting follow-up radiographs of these patients. Ghaffarpasand et al reported 81.1% union rate for nonunion of long bone fractures in PRP group as compared to 55.3% with placebo of 5 ml normal saline in a RCT of 75 patients. We had 90.3% union rate with PRP (See Table 2 for comparison with literature). A shorter healing duration (8.1 ± 1.2 months) was reported in PRP group as compared to placebo group (8.5 ± 0.7 months). The mean duration for union in our study was comparable with 8.1 ± 3.9 months. The mean duration for union was 7.9 ± 0.6 months for upper extremity fractures and 8.4 ± 1.3 months for lower extremity fractures in PRP group [7].
Carlos et al. showed an earlier bone consolidation with PRP exhibiting union at mean of 19.9 weeks in contrast to 25.4 weeks without PRP. However, they did bone grafting at the site for delayed union in all cases and thus results may be confounded [10]. Duramaz in a study on 29 patients showed that long bone nonunions had a nearly significant tendency (p = 0.053) to heal faster with PRP (16.71 ± 2.4 weeks) than exchange nailing (19.07 ± 3.67 weeks). Also, healing with PRP showed a 92.8% success with PRP as compared to 80% with exchange nailing. The healing rate with PRP is comparable to our study [11].
Li et al. in their systematic review showed that healing rates with PRP differed from as low as 30% to upto 100% [9]. This 30% union rate was found by Say et al. in their study on 8 delayed union and 12 nonunions [25].When commenting on only delayed unions, the healing rate boosted to 75% [25]. Kaushik et al reported a union rate of 65% with PRP for delayed union with mean union time of 3 months [5]. Taking this fact into account, the union rate was 65%- 100% in delayed union cases [5, 9, 25]. Li et al. also showed that odds of healing increased by 3.07 (1.37–6.87) when PRP was used in non-union as compared to control groups. Though they used only 3 studies for this calculation, i.e., by Ghaffarpasand et al., Carlos et al. and Samuel et al. [7,8,9,10]. A comparison of LR-PRP and LP-PRP was not made in our study due to limited data on quality of PRP used in different studies in terms of platelet concentration.
Various complications have been reported with PRP such as local infection, subcutaneous hematoma, transient subcutaneous swelling and postinjectionpain. We did not find any such complication in our study [9]. A lower sample size and strict aseptic precautions may be the reason for same.
Based on our findings and literature review, we recommend that LR-PRP should be used in all suspected cases of delayed union, if not responding, multiple serial injections can be tried. With a union rate of > 75% in most studies, it can be used to avoid unnecessary re-surgeries and complications related to bone grafting.
The sample size is either comparable to or greater when compared for most of the studies reported in literature. Limitations of the study include delays in getting proper follow-up radiographs due to COVID19 pandemic and absence of a control group to compare the effect of LR-PRP in delayed union in given population.
Conclusion
Single dose percutaneously injected LR-PRP can be used as a fruitful alternative to catalyze union in patients having delayed union irrespective of site of injury, although sometimes multiple injections at regular intervals may be needed. Multicentric RCTs, although, are recommended to determine the usefulness of this particular intervention as compared to no intervention, other invasive interventions such as bone grafting or non-invasive intervention such as ultrasonography and difference between effectiveness of LR-PRP and LP-PRP.
References
Ruedi, T., Buckley, R., & Moran, C. (2007). AO principles of fracture management, books and DVD. Thieme.
Tsiridis, E., Upadhyay, N., & Giannoudis, P. (2007). Molecular aspects of fracture healing: Which are the important molecules? Injury, 38, S11–S25.
Ravish, V. (2019). The role of platelet rich plasma in delayed union of long bones. International Journal of Orthopaedics, 5, 14–17.
Islam, O., Soboleski, D., Symons, S., Davidson, L., Ashworth, M., & Babyn, P. (2000). Development and duration of radiographic signs of bone healing in children. American Journal of Roentgenology, 175, 75–78.
Kaushik, S. K., Khan, A., Mathur, M., Jaiswal, M., & Jadon, D. (2020). Role of PRP injection in delayed union and non union of long bone fractures. Indian Journal of Orthopaedics, 6, 35–40.
Andersen, C., Wragg, N. M., Shariatzadeh, M., & Wilson, S. L. (2021). The use of platelet-rich plasma (PRP) for the management of non-union fractures. Current osteoporosis reports, 19, 1–14.
Ghaffarpasand, F., Shahrezaei, M., & Dehghankhalili, M. (2016). Effects of platelet rich plasma on healing rate of long bone non-union fractures: A randomized double-blind placebo controlled clinical trial. Bulletin of Emergency & Trauma, 4, 134.
Samuel, G., Menon, J., Thimmaiah, S., & Behera, G. (2018). Role of isolated percutaneous autologous platelet concentrate in delayed union of long bones. European Journal of Orthopaedic Surgery & Traumatology, 28, 985–990.
Li, S., Xing, F., Luo, R., & Liu, M. (2021). Clinical effectiveness of platelet-rich plasma for long-bone delayed union and nonunion: a systematic review and meta-analysis. Frontiers in Medicine. https://doi.org/10.3389/fmed.2021.771252
Acosta-Olivo, C., Garza-Borjon, A., Simental-Mendia, M., Vilchez-Cavazos, F., Tamez-Mata, Y., & Peña-Martinez, V. (2017). Delayed union of humeral shaft fractures: Comparison of autograft with and without platelet-rich plasma treatment: A randomized, single blinded clinical trial. Archives of Orthopaedic and Trauma Surgery, 137, 1247–1252.
Duramaz, A., Ursavaş, H. T., Bilgili, M. G., Bayrak, A., Bayram, B., & Avkan, M. C. (2018). Platelet-rich plasma versus exchange intramedullary nailing in treatment of long bone oligotrophic nonunions. European Journal of Orthopaedic Surgery & Traumatology, 28, 131–137.
Park, J., & Yang, K. H. (2013). Indications and outcomes of augmentation plating with decortication and autogenous bone grafting for femoral shaft nonunions. Injury, 44, 1820–1825.
De Giacomo, A. F., & Tornetta, P., III. (2016). Alignment after intramedullary nailing of distal tibia fractures without fibula fixation. Journal of orthopaedic trauma, 30, 561–567.
Konda, S. R., Goch, A. M., Haglin, J., & Egol, K. A. (2018). Ultralow-dose CT (REDUCTION protocol) for extremity fracture evaluation is as safe and effective as conventional CT: An evaluation of quality outcomes. Journal of orthopaedic trauma, 32, 216–222.
Gołos, J., Waliński, T., Piekarczyk, P., & Kwiatkowski, K. (2014). Results of the use of platelet rich plasma in the treatment of delayed union of long bones. Ortopedia, traumatologia, rehabilitacja, 16, 397–406.
Bielecki, T., Gazdzik, T., & Szczepanski, T. (2008). Benefit of percutaneous injection of autologous platelet-leukocyte-rich gel in patients with delayed union and nonunion. European Surgical Research, 40, 289–296.
Panagiotis, M. (2005). Classification of non-union. Injury, 36, S30–S37.
Zeckey, C., Mommsen, P., Andruszkow, H., Macke, C., Frink, M., Stübig, T., Hüfner, T., Krettek, C., & Hildebrand, F. (2011). The aseptic femoral and tibial shaft non-union in healthy patients–an analysis of the health-related quality of life and the socioeconomic outcome. The open orthopaedics journal, 5, 193.
Yamada, Y., Ueda, M., Naiki, T., Takahashi, M., Hata, K.-I., & Nagasaka, T. (2004). Autogenous injectable bone for regeneration with mesenchymal stem cells and platelet-rich plasma: Tissue-engineered bone regeneration. Tissue engineering, 10, 955–964.
Sarkar, M. R., Augat, P., Shefelbine, S. J., Schorlemmer, S., Huber-Lang, M., Claes, L., Kinzl, L., & Ignatius, A. (2006). Bone formation in a long bone defect model using a platelet-rich plasma-loaded collagen scaffold. Biomaterials, 27, 1817–1823.
Chaudhary D, Rohit K, Kalla R Fucntional outcome and results of platelet rich plasma (PRP) in treatment of delayed union, 2016, 5 (1)
Oryan, A., Alidadi, S., & Moshiri, A. (2016). Platelet-rich plasma for bone healing and regeneration. Expert opinion on biological therapy, 16, 213–232.
Alsousou, J., Thompson, M., Hulley, P., Noble, A., & Willett, K. (2009). The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: A review of the literature. The Journal of bone and joint surgery British, 91, 987–996.
Moshiri, A., Oryan, A., Meimandi-Parizi, A., & Koohi-Hosseinabadi, O. (2014). Effectiveness of xenogenous-based bovine-derived platelet gel embedded within a three-dimensional collagen implant on the healing and regeneration of the Achilles tendon defect in rabbits. Expert opinion on biological therapy, 14, 1065–1089.
Say, F., Türkeli, E., & Bülbül, M. (2014). Is platelet-rich plasma injection an effective choice in cases of non-union? Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca, 81(5), 340–345.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Kishor Kunal, Nitesh Gahlot, Neeraj Choudhary and Abhay Elhence declare that they have no conflict of interest.
Ethical approval
AIIMS/IEC/2020/3107.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kunal, K., Gahlot, N., Choudhary, N. et al. Single/ Multiple Dose Percutaneously Injected LR-PRP Enhances Union Rate in Fracture Delayed Unions: A Prospective Case Series. JOIO (2024). https://doi.org/10.1007/s43465-024-01265-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43465-024-01265-6