Abstract
Introduction
Multi-ligament knee injuries (MLKIs) are rare and complex knee lesions and are potentially associated with intra-articular injuries, especially meniscal tears. Understanding the meniscal tear patterns involved in MLKI can help the orthopedic surgeon treat these complex injuries.
Objective
The purpose of this study was to describe the incidence, classification, and treatment of meniscal injuries in a cohort of patients with MLKIs and carry out an updated review of the evidence available.
Materials and methods
Descriptive retrospective study. Patients with a history of reconstructive surgery for MLKI performed between 2013 and 2023 were included. Informed consent was obtained from all patients included in the study. Patient demographics, magnetic resonance imaging (MRI) study, and operative reports were reviewed. Groups were then formed based on ligament injury patterns. Meniscal tears were identified by MRI and through diagnostic arthroscopy for each patient. The association between meniscal lesions and injury patterns was calculated through Fisher’s exact test. Agreement between the presence of meniscal tear on MRI and in diagnostic arthroscopy was measured using the kappa test. The sensitivity and specificity of MRI were calculated. We inferred the presence of a meniscal tear by injury pattern using the Agresti-Coull confidence interval. For the statistical analysis, a significance of 5% and a confidence interval of 95% were considered.
Results
Seventy patients with MLKIs were included, with a mean age of 30.69 years (SD 10.65). Forty-seven patients had meniscal lesions (67.1%). Of them, 6 had only medial meniscus tears, 31 had only lateral meniscus tears, and 10 had lesions of both menisci, comprising 57 meniscal lesions in total. An anterior cruciate ligament (ACL) + medial collateral ligament/posteromedial corner (MCL/PMC) was the most common injury pattern (52.86% of all patients). Of these 37 patients, 78.38% had meniscal injuries, and most of them (68.97%) were only lateral meniscus injuries. The odds ratio (OR) of having a meniscal tear when having an ACL + medial-side injury was 4.83 (95% CI; 0.89–26.17). Patients with ACL + lateral-side injury pattern had meniscal tears in 42.86%. The lateral meniscus was involved in 100% of these patients. 62.5% of medial meniscus injuries were treated by meniscal repair, and 37.5% by partial meniscectomy. 58.54% of lateral meniscus injuries were treated by meniscal repair, and 39.02% by partial meniscectomy. Agreement calculated using the kappa test between MRI and diagnostic arthroscopy for medial meniscal lesions was 78.57%, and for lateral meniscal lesions was 84.29%.
Conclusion
The ligament injury pattern and the side of the injured collateral ligament influenced the incidence and laterality of meniscal damage. ACL + medial-side injuries were shown to have significantly greater meniscal damage compared to other injury patterns. It is crucial to have a high index of suspicion, obtain a high-quality MRI, and arthroscopically evaluate any possible meniscal lesions in MLKIs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multi-ligament knee injuries (MLKIs) are uncommon lesions, reported to be around 0.02% to 0.20% of all orthopedic injuries [1]. These lesions may be underestimated because of the complexity and often challenging diagnosis. Still, the true incidence is likely to be underestimated due to spontaneous reduction or missed injuries in polytrauma patients [2].
These complex knee injuries are often the result of high-energy mechanisms producing extensive soft tissue damage to the knee, and potentially concomitant intra-articular injuries, including the articular cartilage and menisci [3].
Studies on MLKIs have placed their primary foci on the degree of ligament injury, treatment strategy, involvement of other soft tissues, and neurovascular injury. However, the incidence rates of concomitant intra-articular findings, including meniscal and cartilage injuries, remain largely unreported. The small sample sizes and wide diversity of these injuries, make it difficult to analyze these intra-articular damages, inducing very heterogeneous publications with low levels of evidence and a high risk of bias involving this patient population [4, 5].
According to registry studies, 23% to 31% of MLKIs involved meniscal injuries [6, 7]. A recent systematic review of 2021 regarding the rates of concomitant meniscal tears in MLKIs reported a high incidence ranging from 27 to 30% [5].
Concomitant injuries are considered important for achieving favorable clinical outcomes [8, 9]. Meniscal injuries may predispose patients to diminished outcomes, and increased failure rates and are associated with the development of early arthrosis [10].
Understanding meniscal tear patterns involved in MLKI can help the orthopedic surgeon treat these complex injuries.
The purpose of this study was to describe the incidence, classification, and treatment of meniscal injuries in a cohort of patients with MLKIs and carry out an updated review of the evidence available.
Materials and Methods
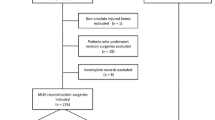
Patients were identified for this retrospective study using a prospectively gathered database at our institution.
We included patients with a history of reconstructive surgery for multi-ligament knee injury performed between 2013 and 2023 by the same surgical team using standardized surgical techniques. Informed consent was obtained from all individual participants included in the study.
Patient demographics, magnetic resonance imaging (MRI) study, and operative reports were reviewed and recorded following approval from our institutional ethics committee.
The definition of a multi-ligament knee injury is commonly recognized as a tear of at least two of the four major knee ligament structures: the anterior cruciate ligament (ACL), the posterior cruciate ligament (PCL), the medial collateral ligament/posteromedial corner (MCL/PMC) and the lateral collateral ligament/posterolateral corner (LCL/PLC).
Patients were excluded for non-operative treatment only, prior ligament reconstructive surgery on the affected knee, and skeletally immature patients.
Groups were then formed based on ligament injury patterns. Injury patterns were further grouped using the Schenck classification [11], and side of injury (medial/lateral). Meniscal injuries were identified by magnetic resonance imaging and at the time of diagnostic arthroscopy for each group and then classified using Cooper classification (Fig. 1) [12].
Cooper classification of meniscal tears. Radial zones are divided into areas A, B, and C for the medial meniscus (posterior to anterior) and areas D, E, and F for the lateral meniscus (anterior to posterior). The 4 circumferential zones are 0 for the meniscocapsular junction, 1 for the outer third, 2 for the middle third, and 3 for the inner third
The association between meniscal lesions and injury patterns was calculated through Fisher's exact independence test, which is the gold standard for this testing [13]. When the independence test was significant, a logistic regression analysis was performed.
The agreement between the presence of meniscal tear on MRI and the presence of meniscal injury in arthroscopy was measured using the kappa test [14]. Sensitivity and specificity were calculated.
Given that the prevalence of certain injuries is very low, we calculated the confidence interval for the presence of meniscal injury by injury pattern using the Agresti-Coull correction [15, 16].
For the statistical analysis, a significance of 5% and a confidence interval of 95% were considered.
All data were processed in Stata 18.0.
Results
Demography and Injury Pattern
Seventy patients with multi-ligament knee injuries were included.
Patients had a mean age of 30.69 years (SD 10.65). Most patients were males (71.43%).
The injury pattern is presented in Table 1.
Forty-seven patients had meniscal lesions (67.1%). Of them, 6 had only a medial meniscus tear (12.8%), 31 had only a lateral meniscus tear (65.9%), and 10 had lesions of both menisci (21.3%), comprising 57 meniscal lesions in total.
ACL + MCL/PMC injury was the most common (N = 37; 52.86% of all patients). Of these 37 patients, 29 (78.38%) had meniscal injuries, and most of them were only lateral meniscus injuries (20/29 meniscal lesions, 68.97%). 7 patients with ACL + medial-side injury had Stener-like lesions. Of these, 6 had lateral meniscus tears, and none had medial meniscus tears.
The second most common injuries were ACL + LCL/PLC (7 patients, 10%) and KD IV injuries (ACL + PCL + MCL/PMC + LCL/PLC, 7 patients, 10%) (Fig. 2).
Patient with KD IV multi ligamentous injury and lateral meniscus tear of the left knee. A, B Coronal and sagittal PD-Fat sat MRI showing medial and lateral side injury, bicruciate ligament injury, and lateral meniscus tear. C Arthroscopic image of a posterior horn lateral meniscus tear with a meniscal flap. D Arthroscopic image of a lateral meniscal repair with an all-inside suture technique. E, F Post-operative control images after reconstruction of both cruciate and medial side injury
Patients with ACL + lateral-side injuries had meniscal injuries in 42.86% (3/7 patients). The lateral meniscus was involved in 100% of these patients. One patient had lateral meniscus injury only and two had injury of both menisci.
ACL + medial-side injuries were shown to have significantly greater meniscal damage compared to ACL + lateral-side injuries (29/37 patients vs. 3/7 patients; p = 0.003), and specifically greater likelihood of a lateral meniscus injury (p = 0.024).
The odds ratio of having a meniscal injury, when having an ACL + medial-side injury, is 4.83 (95% CI; 0.89–26.17), and specifically of having a lateral meniscus injury, it’s 3.15 (95% CI; 0.60–16.49).
In this study, the probability of presenting a meniscal injury in the case of a KD IV type injury and a KD IIIL is 100%, and the probability of a meniscal injury in a KD II type injury and PCL + lateral-side injury is 0% (p = 0.003).
The ACL + medial side injury and the KD IV injury are significantly associated with presenting a meniscal injury, with a 95% confidence interval of Agresti-Coull of 0.63–0.89, and 0.59–1.00, respectively.
Cooper’s Classification
According to Cooper's classification, most lateral injuries involved zone F (posterior horn). Thirty-four injuries involved at least the posterior horn, 6 the anterior horn, and 12 the body of the meniscus.
Only 18 lateral meniscus lesions could be well described by zone (0–1-2–3). The majority of the adequately described lesions (11 out of 18) were in zone 2 (red-white), 4 in zone 0 (meniscocapsular junction), 4 in zone 1 (red), and 2 in zone 3 (white).
Most of the medial injuries (13 lesions) also involved the posterior horn (zone A), 7 involved zone B (body), and there were no lesions in zone C (anterior horn). Only 8 lesions could be well described by zone. Out of them, 1 was in zone 1 (red), 3 were in zone 3 (white), 3 were in zone 0 (meniscocapsular junction), and 1 was in zone 2 (red-white).
Treatment
Of the 16 medial meniscus tears, 10 (62.5%) were treated by meniscal repair, and 6 (37.5%) were treated by partial meniscectomy.
Of the 41 lateral meniscus tears, 24 (58.54%) were treated by meniscal repair, 16 (39.02%) were treated by partial meniscectomy and 1 (2.44%) partial stable tear was not treated.
Treatment of meniscus tear by injury pattern is described in Table 2.
MRI and Diagnostic Arthroscopy Agreement
The sensibility and specificity of MRI for detecting medial meniscus tears were 93.75% and 74.07%, respectively (Table 3).
The sensibility and specificity of MRI for detecting lateral meniscus tears were 82.93% and 86.21%, respectively (Table 4).
Agreement calculated using the kappa test between MRI and diagnostic arthroscopy for medial meniscal lesions was 78.57%, and for lateral meniscal lesions was 84.29% (Table 5).
Discussion
Our study showed a 67.1% of MLKI patients with meniscus lesions (47 patients). 8.5% of all patients with MLKI had only medial meniscus tears (6 patients), 44.3% had only lateral meniscus tears (31 patients) and 14.3% had a lesion of both menisci (10 patients).
Out of all the meniscal tears, most of them (71.9%) were lateral meniscus injuries, and only 28.1% affected the medial meniscus. Most lateral meniscus tears occurred without involving the medial meniscus (75.6%), unlike the medial meniscus, whose injuries mostly occurred in conjunction with injury to the lateral meniscus (62.5% of medial meniscus lesions).
A recent systematic review published by Kim et al. reported a pooled rate of 30.4% of medial meniscal tears and 27.5% of lateral meniscal tears in patients with MLKIs [5].
The incidence of lateral meniscal tears in MLKIs varied across studies, ranging from 1.8 to 56.4% [9, 17], so the incidence of medial meniscal tears was between 8.8 and 64% [18, 19].
A retrospective study from 2023 described meniscal injuries in 235 patients undergoing surgical treatment for MLKI. 29.4% of patients had a meniscal lesion; 15.3% had an isolated medial meniscus tear, 17.9% with an isolated lateral meniscus tear, and 3.8% had both menisci torn. They also reported significantly less meniscal damage in lateral-sided injuries than in medial-sided injuries (17.7% vs. 41%; p < 0.001) [8].
This was also demonstrated long before by Kaeding et al. [20] in 2005, and even longer ago by Shelbourne et al. [21] who reported that lateral meniscal damage was significantly higher in the ACL/MCL group, and medial meniscal damage was significantly lower in this group. They concluded that ACL + MCL + medial meniscus tear was, in fact, an unusual clinical entity among athletes with knee injuries.
This is consistent with our study, in which ACL + medial-side injuries were shown to have significantly greater meniscal damage compared to ACL + lateral-side injuries.
Our study describes a higher rate of meniscal injuries than the articles cited previously, nevertheless, King et al. [22] in 2015 reported a meniscal injury in 56% of patients (isolated medial 22%; isolated lateral 22%; combined, 12%), and Krych et al. [23] in the same year reported 55% of MLKIs with meniscal tears (38.8% isolated medial, 40.3% isolated lateral, and 20.9% combined medial/lateral), which is more consistent with the current study.
Meniscal injuries in MLKIs may predispose patients to diminished outcomes. Assessment and treatment of these injuries may help improve surgical results and functional scores in these patients, with good outcomes demonstrated for meniscal repair. A study conducted by Chahla et al. [24] showed that the failure rate for inside-out meniscal repair with concomitant multi-ligament reconstruction was low, regardless of meniscus laterality and tear characteristics. They suggest that the biological augmentation resulting from intra-articular ligament reconstruction tunnel reaming may partially contribute to the overall improved outcomes and the low failure rate of meniscal repair.
The retrospective design of the present study confers some inherent limitations. First, potential selection biases may occur, given the retrospective recruitment of patients, for example, non-operative MLKIs were not included because arthroscopic diagnosis was used to assess the meniscal status. Another example is that few patients did not sign the consent to be included in future studies, limiting the number of patients.
Second, we didn’t assess the impact of timing on the presence and treatment of the meniscal tears. Song et al. [25] confirmed that early surgery increased the prevalence of meniscus repair, especially when the tear is located in the posterior horn of the lateral meniscus.
Third, mainly in chronic cases, some initial ligament and meniscal damage may have healed when the patient was cared for. This would explain some of the discrepancies between MRI and diagnostic arthroscopy.
Fourth, these results are from a cohort of a single institution and may not reflect the global incidence. The number of patients is limited, especially in some injury patterns, with none or only 1 patient included, which could taint the results and lead to wrong conclusions based on the number of patients.
On the other hand, this current study has several clinical implications. First, these findings encourage evaluating concomitant intra-articular injuries in all MLKIs, and expect surgical care according specific lesions associated. Second, the difference in associated meniscal damage in different MLKI injury patterns reflects that these are different lesions, with different injury mechanisms, and treatment decision parameters should not be the same for all. Furthermore, increasing meniscal assesment in acute multi ligamentous reconstruction could help decide the ideal timing for surgical care of this intra-articular injuries.
Conclusion
Meniscal injuries are commonly associated with MLKIs.
The ligament injury pattern and the side of the injured collateral ligament influenced the incidence and laterality of meniscal damage. ACL + medial-side injuries were shown to have significantly greater meniscal damage compared to other injury patterns.
It is crucial to have a high index of suspicion, obtain a high-quality MRI, and arthroscopically evaluate any possible meniscal lesions and other concomitant injuries in MLKIs to decide the ideal timing and appropriate treatment of these complex injuries.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Howells, N. R., Brunton, L. R., Robinson, J., Porteus, A. J., Eldridge, J. D., & Murray, J. R. (2011). Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee. Injury, 42, 1198–1204. https://doi.org/10.1016/j.injury.2010.11.018
Fanelli, G. C., Orcutt, D. R., & Edson, C. J. (2005). The multiple-ligament injured knee: Evaluation, treatment, and results. Arthrosc J Arthrosc Relat Surg, 21, 471–486. https://doi.org/10.1016/j.arthro.2005.01.001
Hassebrock, J. D., Gulbrandsen, M. T., Asprey, W. L., Makovicka, J. L., & Chhabra, A. (2020). Knee ligament anatomy and biomechanics. Sports Med Arthrosc, 28, 80–86. https://doi.org/10.1097/JSA.0000000000000279
Hankins, D. A., Fletcher, I. E., Prieto, F., Ockuly, A. C., Myers, O. B., Treme, G. P., et al. (2019). critical evaluation of the methodologic quality of the Top 50 cited articles relating to knee dislocation and multiligamentous knee injury. Orthopaedic Journal of Sports Medicine, 7, 232596711988050. https://doi.org/10.1177/2325967119880505
Kim, S. H., Park, Y.-B., Kim, B.-S., Lee, D.-H., & Pujol, N. (2021). Incidence of associated lesions of multiligament knee injuries: A systematic review and meta-analysis. Orthopaedic Journal of Sports Medicine, 9, 232596712110104. https://doi.org/10.1177/23259671211010409
Lind, M., Menhert, F., & Pedersen, A. B. (2009). The first results from the Danish ACL reconstruction registry: Epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surgery, Sports Traumatology, Arthroscopy, 17, 117–124. https://doi.org/10.1007/s00167-008-0654-3
Lind, M., Nielsen, T. G., & Behrndtz, K. (2017). Both isolated and multi-ligament posterior cruciate ligament reconstruction results in improved subjective outcome: results from the Danish Knee Ligament Reconstruction Registry. Knee Surgery, Sports Traumatology, Arthroscopy. https://doi.org/10.1007/s00167-017-4577-8
Labarre, C., Kim, S. H., & Pujol, N. (2023). Incidence and type of meniscal tears in multilligament injured knees. Knee Surgery, Sports Traumatology, Arthroscopy, 31, 465–474. https://doi.org/10.1007/s00167-022-07064-6
Alentorn-Geli, E., Lazarides, A. L., Utturkar, G. M., Myers, H. S., Samuelsson, K., Choi, J. H. J., et al. (2019). Factors predictive of poorer outcomes in the surgical repair of multiligament knee injuries. Knee Surgery, Sports Traumatology, Arthroscopy, 27, 445–459. https://doi.org/10.1007/s00167-018-5053-9
Rao, A. J., Erickson, B. J., Cvetanovich, G. L., Yanke, A. B., Bach, B. R., & Cole, B. J. (2015). The meniscus-deficient knee. Orthopaedic Journal of Sports Medicine, 3, 232596711561138. https://doi.org/10.1177/2325967115611386
Schenck, R. C. (1994). The dislocated knee. Instructional Course Lectures, 43, 127–136.
Cooper, D. E., Arnoczky, S. P., & Warren, R. F. (1991). Meniscal repair. Clinics in Sports Medicine, 10, 529–548.
Fisher, R. A. (1922). On the interpretation of χ2 from contingency tables, and the calculation of P. Journal of the Royal Statistical Society, 85, 87. https://doi.org/10.2307/2340521
Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20, 37–46. https://doi.org/10.1177/001316446002000104
Agresti, A., & Coull, B. A. (1998). Approximate is better than “exact” for interval estimation of binomial proportions. American Statistician, 52, 119–126. https://doi.org/10.1080/00031305.1998.10480550
Brown, L. D., Cai, T. T., & DasGupta, A. (2001). Interval estimation for a binomial proportion. Statistical Science. https://doi.org/10.1214/ss/1009213286
Wajsfisz, A., Bajard, X., Plaweski, S., Djian, P., Demey, G., Limozin, R., et al. (2014). Surgical management of combined anterior or posterior cruciate ligament and posterolateral corner tears: For what functional results? Orthopaedics & Traumatology, Surgery & Research, 100, S379–S383. https://doi.org/10.1016/j.otsr.2014.10.003
Yeh, W.-L., Tu, Y.-K., Su, J.-Y., & Hsu, R.W.-W. (1999). Knee dislocation. The Journal of Trauma: Injury, Infection, and Critical Care, 46, 693–701. https://doi.org/10.1097/00005373-199904000-00023
Kosy, J. D., Matteliano, L., Rastogi, A., Pearce, D., & Whelan, D. B. (2018). Meniscal root tears occur frequently in multi-ligament knee injury and can be predicted by associated MRI injury patterns. Knee Surgery, Sport Traumatol Arthrosc, 26, 3731–3737. https://doi.org/10.1007/s00167-018-5009-0
Kaeding, C. C., Pedroza, A. D., Parker, R. D., Spindler, K. P., McCarty, E. C., & Andrish, J. T. (2005). Intra-articular findings in the reconstructed multiligament-injured knee. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 21, 424–430. https://doi.org/10.1016/j.arthro.2004.12.012
Shelbourne, K. D., & Nitz, P. A. (1991). The O’Donoghue triad revisited. American Journal of Sports Medicine, 19, 474–477. https://doi.org/10.1177/036354659101900509
King, A. H., Krych, A. J., Prince, M. R., Sousa, P. L., Stuart, M. J., & Levy, B. A. (2015). Are meniscal tears and articular cartilage injury predictive of inferior patient outcome after surgical reconstruction for the dislocated knee? Knee Surgery, Sports Traumatology, Arthroscopy, 23, 3008–3011. https://doi.org/10.1007/s00167-015-3671-z
Krych, A. J., Sousa, P. L., King, A. H., Engasser, W. M., Stuart, M. J., & Levy, B. A. (2015). Meniscal tears and articular cartilage damage in the dislocated knee. Knee Surgery, Sports Traumatology, Arthroscopy, 23, 3019–3025. https://doi.org/10.1007/s00167-015-3540-9
Chahla, J., Dean, C. S., Matheny, L. M., Mitchell, J. J., Cinque, M. E., & LaPrade, R. F. (2017). Outcomes of inside-out meniscal repair in the setting of multiligament reconstruction in the knee. American Journal of Sports Medicine, 45, 2098–2104. https://doi.org/10.1177/0363546517698944
Song, X., Chen, D., Qi, X., Jiang, Q., & Xia, C. (2021). Which factors are associated with the prevalence of meniscal repair? BMC Musculoskeletal Disorders, 22, 295. https://doi.org/10.1186/s12891-021-04107-w
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
Informed consent was obtained from all patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Figueroa, D., Figueroa, M.L., Cañas, M. et al. Meniscal Lesions in Multi-Ligament Knee Injuries. JOIO 58, 1224–1231 (2024). https://doi.org/10.1007/s43465-024-01217-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01217-0