Abstract
Background and Purpose
Scaphoid waist fractures are often stabilised with compression screws, Kirschner wires (K-wires), or a combination of both. While clinical and bio-mechanical studies evaluating their utility are available, the ideal configuration of implant that would provide adequate stability to permit early use of the hand is debatable. We examined configurations of a single screw, one screw along with a K-wire, and two K-wires used for a transverse scaphoid waist fracture fixation aiming to assess the stability provided by each in the immediate postoperative period.
Methods
Computer-aided design (CAD) models of the scaphoid, K-wire, and headless compression screw were created. A transverse fracture was created at the scaphoid waist, and the CAD models of the screw and K-wire were used to fix the fracture in different configurations in a distal to proximal direction. Finite Element Analysis (FEA) was used to examine the strength of configurations when they were subjected to compression and distraction forces. The total maximum deformation (TDef) and factor of safety (FoS) for each configuration were calculated and used as indirect indicators of postoperative stability.
Results
When a single screw was used, the configurations with the screw directed posteriorly from either centre or anterior had the best combined TDef and FoS values. For one screw and one K-wire, the configuration with screw and K-wire parallel to each other with the screw located along the long axis in the AP projection and anterior to the K-wire in the lateral projection had the best combined TDef and FoS values. When using two K-wires, configurations with the two wires diverging proximally on the lateral projection had the best combined TDef and FoS values.
Conclusions
When fixing a transverse scaphoid waist fracture with a single screw, the screw directed posteriorly from either the centre or anterior aspect of the distal pole has the best stability, a parallel configuration has the best stability when fixing it using a screw and a K-wire, and divergent configuration has the best stability when fixing it with two K-wires only.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Scaphoid is subjected to significant stresses from the usual day-to-day activities [1]. The current practice of scaphoid fracture management depends on the location of the fracture and the degree of displacement [2,3,4]. Undisplaced waist and distal pole fractures are often treated non-operatively and tend to heal well in most patients. Surgical fixation is the preferred treatment for displaced waist and proximal pole fractures [4]. Many centres internally fix all scaphoid fractures, including the undisplaced ones. An early return of wrist movement, higher union rates, and avoidance of cast are the purported benefits of such an approach [4].
Implants used for fracture fixation behave like internal splints, protecting and stabilising the reduction. After Herbert and Fisher’s headless screw design, many other screws based on similar concepts have been described [1, 5]. Kirschner wires (K-wires) have been used for the fixation of scaphoid fractures either as primary or salvage implants when screw fixation alone is judged to be inadequate by the operating surgeon [6, 7]. Biomechanical studies on cadaveric scaphoids with mechanical loading of the fixation construct have attempted to identify the most suitable screw design for fixation [1, 8]. Finite Element Analysis (FEA) has been used to examine stress–strain patterns, implant design, fracture load prediction, mechanical property determination, ideal implant direction [9, 10], the influence of K-wire position on the initial stability [11], and also to study the mechanism of development of a scaphoid waist fracture [12].
Despite preoperative planning, the surgeon may fail to place the implant in the desired position during surgery. While earlier studies have contributed to the knowledge and have aided in improving the practice of scaphoid fixation, literature on the ideal implant configuration that would provide enough stability for permitting an early wrist motion and use of the hand for routine activities is unavailable. The present study attempts to identify the implant configurations that would have adequate stability to withstand the application of physiological loads soon after fixation of a transverse fracture through the scaphoid waist.
Materials and Methods
Anonymized computed tomography (CT) images of a 32-year-old male who had suffered fracture of the middle phalanx were utilized for the creation of the scaphoid model. The images were obtained with the wrist in the prone position. A Standard Tessellation Language (STL) model of the scaphoid was constructed on Mimics Medical software (Materialise NV) using Digital Imaging and Communications in Medicine (DICOM) files. The scaphoid STL model was then rectified and converted into a computer aided design (CAD) model using Autodesk Meshmixer (RRID:SCR_015736, © 2020 Autodesk, Inc.) and FreeCAD (version 0.19.2), respectively. CAD was used to define the material properties of scaphoid. CAD model of 1.5 mm K-wire and Herbert type Headless screw (28 mm long, 3 mm diameter) were designed in SOLIDWORKS with accurate measurements. Their material properties were obtained from the manufacturers. The Institutional Human Ethics Committee approval was obtained before conducting the study (ref. IHEC-LOP/2021/IM0360).
A transverse fracture was created at the waist of the scaphoid model (Fig. 1). We chose the transverse pattern for studying fracture fixation as it is the most common pattern for scaphoid fractures [3, 13]. The CAD models of K-wire and screw were then inserted in a distal to proximal direction into the scaphoid model to simulate fixation of the fracture (Fig. 2). Although scaphoid waist fractures can be fixed either from ‘proximal to distal’ or ‘distal to proximal’ directions, we chose the ‘distal to proximal’ direction as this approach does not compromise the scaphoid vascularity which is predominantly from the dorsal surface; secondly, waist fractures are best approached from the anterior side affording good exposure [4].
The headless compression screw model was inserted into the scaphoid model using Boolean subtraction techniques. The leading end of the screw was in the proximal fragment. For simulating the creation of a track by a drill bit during surgery, part of the bone inside the cannulated screw was subtracted. For simulating the effect of compression produced by the screw, a pre-load of 20 Nm was applied. Six different CAD configurations of screw positions were designed with changes in the angle of insertion in two orthogonal radiographic projections, simulating a surgeon’s view (Fig. 3). The aim of varying the angle of the screw was to simulate the variations that a surgeon might have during surgery. However, pre-defined angles were not used as accurate measurement of angles are not usually feasible during an actual surgical procedure.
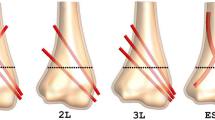
Six different one screw and one wire configurations were created such that in three of them the screw was placed anterior to the wire and in the other three it was posterior (Fig. 4). In none of the configurations, the wire and screw intersected each other. Like the one screw and one K-wire model, six different configurations of two K-wires were also created (Fig. 5). The CAD models of transverse scaphoid waist fractures were converted to Initial Graphics Exchange Specification (IGES) files for FEA in ANSYS 2022 R1 Student version (Ansys© Academic Research Mechanical). FEA requires the definition of the material properties of the scaphoid bone, the screw, and the K-wire [9,10,11]. Table 1 summarizes the values used in the study. AS performed the FEA under the guidance of RKD. JAS and PB provided the analysing team with the details of the possible variations in the direction of implant placement.
A fixed contact condition was applied at the contact of the scaphoid with radius. Static friction (µ = 0.4) between the two fractured parts of the scaphoid was introduced as described by Luria et al. [10] to simulate real-life condition. Bonded contact was defined between fractured bone and implants. Distally, the contact force was applied along the scaphotrapeziotrapezoid (STT) joint. We subjected each construct to compression and tensile forces of magnitude 300 and 100 N, respectively. These are the forces that would act on a patient’s operated scaphoid when s/he tries to get up from a chair by putting pressure on the wrist or tries to lift a light object, respectively. We assumed these were the routine activities a patient would want to perform as early as possible after surgery.
On the FEA, we looked at two parameters—total maximum deformation (TDef) of bone that is indicative of displacement between the two fragments at the fracture site after application of force, and factor of safety (FoS) of the construct that indicates the strength of construct under different loading conditions. The TDef is used in ANSYS© and is the square root of summation of the square of deformation in three axes (x, y, and z) and indicates the displacement occurring in a construct after it is subjected to loads; the FoS provides information as to how much stronger a construct is than it needs to be for an intended load [14]. Ideally, the TDef must be low and FoS must be high for any construct to be stable. A value of 1.0 was considered as the cutoff for FoS as per the acceptable international convention. We chose the implant placement across the fracture, assessing the two views—AP and lateral together to simulate the surgical condition faced by a surgeon. The implant placement was done by ‘eyeballing’ used for learned estimation of the implant configuration during most surgeries. These results were plotted graphically using Matlab (R2022a).
Results
The values of TDef and FoS obtained during FEA are presented in Table 2. Figure 6 shows the FoS and TDef of different configurations of placement of a single screw construct. Under tensile load, the minimum and maximum TDef were seen in configurations 3 and 4, respectively, and the minimum and maximum FoS were seen in configurations 1 and 5. When TDef and FoS were considered together, configurations 1 and 4 had the poorest values. Under compressive loads, the TDef of all configurations was <0.01 mm and there was no gross variation in the values. The FoS for all the six configurations was more than three, the highest being for configuration 4.
Figure 6 also presents the FoS and TDef of one screw and one wire configurations. In the first three, the screw was placed anterior to the K-wire, and in the remaining, K-wire was placed anterior to the screw. Under both tensile and compressive loads, TDef values for all the configurations were <0.02 mm. FoS under tensile and compressive loads was poorest for configuration 5, where the implants were converging towards each other in both the views—from the front (antero-posterior) and side (lateral). FoS was more than four for configurations 1 and 2, wherein wire and screw were located on either side of the midline on the lateral view and the K-wire was located medial to the midline and the screw was located along the long axis of the scaphoid on frontal view.
Finally, Fig. 6 presents the FoS and TDef of the two K-wire configurations. TDef of more than 0.1 mm was noted in configuration 1, in which one of the K-wires was placed near the medial cortex in the AP projection and near the anterior cortex in the lateral position, while the second wire was placed along the mid-axis of the scaphoid in both the projections. This configuration had the least FoS too. Rest all configurations had TDef <0.02 mm in the two loading conditions. Configurations 2 and 3 had the highest FoS under tensile and compressive loading conditions, respectively. Configuration 5, with the wires convergent to each other on both the frontal and lateral projections, has a low FoS.
Discussion
The usual treatment for an undisplaced scaphoid fracture is immobilization in a cast for 8–12 weeks, and it is successful in achieving union in around 90% of patients [3, 4]. This prolonged immobilization in cast carries the risk of stiffness, decreased grip strength, and delayed return to work. For displaced fractures, the usual treatment is closed/open reduction and surgical fixation, which avoids the disadvantages of prolonged need for a cast [15, 16].
Screws with distinct structural properties have been used for transverse scaphoid waist fracture fixation with good results [1, 4, 5, 17]. A single screw placed along the central one-third of the scaphoid, i.e., in the centre–centre position, is the preferred orientation for the implant in biomechanical and finite element studies [10, 16, 18]. However, screw placement can be technically difficult and requires a high level of skill [3]. Swanstrom et al. studied the screw orientation, i.e., central versus perpendicular, for scaphoid waist fracture fixation in ten computer models; they reported that increasing the screw perpendicularity at the fracture site resulted in higher compression with maximum compression being achieved when the screw placement was perpendicular to the fracture [19]. However, in unstable fracture patterns, a single screw may not provide the required rotational stability during wrist extension-flexion and radioulnar deviation [20]. Mandelson et al. performed a biomechanical study of scaphoid waist fracture non-union where they compared three different fixation models—single compression screw, double screws and scaphoid plate. They found that double-screw fixation resulted in greater stiffness and load to failure than single screw fixation and was comparable to plate fixation [21]. Even with the availability of multiple designs of compression screws for scaphoid fixation, K-wires are still popular in practice as they are easier to insert with minimal dissection and as salvage implants after previously failed fixation [22].
Despite preoperative planning, scaphoid fracture fixation may not proceed as planned. In such a situation, the foreknowledge of the configuration of implants that may be safely accepted and the configurations that are better avoided would help the surgeon in intraoperative decision-making. In the present study, we have utilised two parameters, viz., TDef and FoS, that are frequently used in the field of mechanical engineering to evaluate the strength of any construct in a computer model before its actual execution in the real world. Based on our results, the following inferences can be drawn—
-
For single compression screw fixation, one would have the best combination of TDef and FoS in configurations 5 and 6; configurations 2 and 3 are also ‘acceptable’. The configurations 1 and 4 are ‘not acceptable’ (Fig. 5a)
-
For one screw and one wire fixation, configuration 5 in which the implants are converging proximally, is ‘not acceptable’; configuration 1 would be ideal, and configurations 4 and 6 could be considered as ‘acceptable’ (Fig. 5b).
-
For the two K-wires fixation, configurations 1 and 5 with least FoS and highest TDef are ‘not acceptable’; configurations 2, 3, 4, and 6 having divergence of the wires in the lateral views are all ‘acceptable’ (Fig. 5c).
The highest FoS was noted for single compression screw configuration 5 for tensile loading and configuration 4 for compression loading. The maximum absolute values for single compression screw configurations were more than that for two K-wire constructs. One plausible explanation could be the lower stiffness and strength of the K-wire compared to the compression screw. This aspect needs to be further evaluated in future studies as the results run contrary to those obtained for two screw constructs in previous studies [20].
Our study has a few notable limitations. Being a software-based study, our findings do not consider the influence that soft tissues and surrounding bones may have on the trajectory of implant placement. Although by using the ‘free-hand technique’ we have tried to address this issue, it is not possible to address for all the variables. We assumed uniform density across all the scaphoids, and hence, the effect of cortical shell and cancellous centre of scaphoid on construct stability was not evaluated. A direct comparison between the available computational studies could not be made as the study design, and the parameters studied were different. Additionally, in a few cases, a surgeon might need multiple attempts to place a provisional K-wire and then guidewire before screw placement. This might alter the internal structure of the scaphoid and affect the strength. This study has not taken these scenarios into consideration.
Notwithstanding the limitations, the findings of this FEA would provide the surgeon with the necessary confidence in determining the acceptable implant configuration intraoperatively. A single well-placed compression screw should be enough if it is in an ‘acceptable’ configuration; however, in case the screw placement is not acceptable, then a second implant, either another screw or a K-wire may be added. In double implant fixation, divergent screws or K-wires in the lateral view are ‘acceptable’.
Data Availability
Not applicable for this work.
References
Toby, E. B., Butler, T. E., McCormack, T. J., & Jayaraman, G. (1997). A comparison of fixation screws for the scaphoid during application of cyclical bending loads. Journal of Bone and Joint Surgery. American Volume, 79(8), 1190–1197.
Dias, J. J., Brenkel, I. J., & Finlay, D. B. (1989). Patterns of union in fractures of the waist of the scaphoid. Journal of Bone and Joint Surgery. British Volume, 71(2), 307–310.
Dias, J. J., Wildin, C. J., Bhowal, B., & Thompson, J. R. (2005). Should acute scaphoid fractures be fixed? A randomized controlled trial. Journal of Bone and Joint Surgery. American Volume, 87(10), 2160–2168.
Rhemrev, S. J., Ootes, D., Beeres, F. J., Meylaerts, S. A., & Schipper, I. B. (2011). Current methods of diagnosis and treatment of scaphoid fractures. International Journal of Emergency Medicine, 4, 4.
Herbert, T. J., & Fisher, W. E. (1984). Management of the fractured scaphoid using a new bone screw. Journal of Bone and Joint Surgery. British Volume, 66(1), 114–123.
Christodoulou, L. S., Kitsis, C. K., & Chamberlain, S. T. (2001). Internal fixation of scaphoid non-union: A comparative study of three methods. Injury, 32(8), 625–630.
Leow, M. Q. H., Chung, S., & Tay, S. (2020). The effect of intra-carpal Kirschner wire augmentation in screw fixation of scaphoid—A retrospective cohort study. Malaysian Orthopaedic Journal, 14(3), 104–109.
Shaw, J. A. (1991). Biomechanical comparison of cannulated small bone screws: A brief follow-up study. The Journal of Hand Surgery, 16(6), 998–1001.
Acar, B., Kose, O., Kati, Y. A., Egerci, O. F., Turan, A., & Yuksel, H. Y. (2018). Comparison of volar versus dorsal screw fixation for scaphoid waist fractures: A finite element analysis. Orthopaedics and Traumatology: Surgery and Research OTSR, 104(7), 1107–1113.
Luria, S., Hoch, S., Liebergall, M., Mosheiff, R., & Peleg, E. (2010). Optimal fixation of acute scaphoid fractures: Finite element analysis. The Journal of Hand Surgery, 35(8), 1246–1250.
Ezquerro, F., Jiménez, S., Pérez, A., Prado, M., de Diego, G., & Simón, A. (2007). The influence of wire positioning upon the initial stability of scaphoid fractures fixed using Kirschner wires A finite element study. Medical Engineering & Physics, 29(6), 652–660.
Santoshi, J. A., Behera, P., Dwivedi, R. K., & Srivastav, A. (2023). Mechanism of scaphoid waist fracture: Finite element analysis. Journal of Hand Surgery (European Volume), 48(5), 426–434.
Ten Berg, P., Drijkoningen, T., Strackee, S., & Buijze, G. (2016). Classifications of acute scaphoid fractures: A systematic literature review. Journal of Wrist Surgery, 5(2), 152–159.
Ching, J. (2009). Equivalence between reliability and factor of safety. Probabilistic Engineering Mechanics, 24(2), 159–171.
Fowler, J. R., & Ilyas, A. M. (2010). Headless compression screw fixation of scaphoid fractures. Hand Clinics, 26(3), 351–361.
Kawamura, K., & Chung, K. C. (2008). Treatment of scaphoid fractures and nonunions. The Journal of Hand Surgery, 33(6), 988–997.
Wolfe, S. W., Pederson, W. C., Hotchkiss, R. N., Kozin, S. H., & Cohen, M. S. (2016). Green’s operative hand surgery (7th ed., pp. 588–624). Philadelphia: Elsevier Health Sciences.
McCallister, W. V., Knight, J., Kaliappan, R., & Trumble, T. E. (2003). Central placement of the screw in simulated fractures of the scaphoid waist: A biomechanical study. Journal of Bone and Joint Surgery. American Volume, 85(1), 72–77.
Swanstrom, M. M., Morse, K. W., Lipman, J. D., Hearns, K. A., & Carlson, M. G. (2017). Effect of screw perpendicularity on compression in scaphoid waist fractures. Journal of Wrist Surgery, 6(3), 178–182.
Surke, C., Huntington, L. S., Zhang, X., Ek, E. T. H., Ackland, D., & Tham, S. K. (2022). Double-screw osteosynthesis in an unstable scaphoid fracture model: A biomechanical comparison of two screw configurations. The Journal of Hand Surgery. American Volume, 47(11), 1118.e1-1118.e8.
Mandaleson, A., Tham, S. K., Lewis, C., Ackland, D. C., & Ek, E. T. (2018). Scaphoid fracture fixation in a nonunion model: A biomechanical study comparing 3 types of fixation. The Journal of Hand Surgery, 43(3), 221–228.
Gokce, V., Oflaz, H., Dulgeroglu, A., Bora, A., & Gunal, I. (2011). Kirschner wire fixation for scaphoid fractures: An experimental study in synthetic bones. Journal of Hand Surgery (European Volume), 36(4), 325–328.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
AS performed the finite element study and approved the draft of the manuscript. PB analysed the data and prepared the manuscript for submission. RD performed the finite element study and analysed the data. JAS conceptualized and designed the study and approved the manuscript for submission. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical Standard
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
The study was approved by the Institutional Review Board (ref. IHEC-LOP/2021/IM0360). A waiver of consent was obtained from the IHEC as the CT images of one patient was used in an anonymous manner.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Srivastav, A., Behera, P., Dwivedi, R.K. et al. Finite Element Analysis of Postoperative Stability of Transverse Scaphoid Waist Fracture. JOIO 58, 785–793 (2024). https://doi.org/10.1007/s43465-024-01156-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01156-w