Abstract
Objectives
To describe traumatic head and neck injuries in elite Australian cricket players, for the purposes of understanding risk and the role of protective equipment and regulations.
Design
Retrospective cohort study.
Methods
This study reviewed twelve seasons of clinical data for elite male and female cricket players who sustained a traumatic head or neck injury (excluding isolated concussion) whilst participating in a cricket match or training.
Results
199 events of head and neck injuries were recorded over the 12 seasons, equating to an average incidence of 5.6 per 100 players per season. Since the introduction of helmet regulations in 2016, the average incidence was 7.3. Including concurrent injuries, 232 injuries revealed contusions were the most common type of injury (41%, 35–48%), and the face was the most common location (63%, 57–69%). Injuries resulted in the player being unavailable for cricket for one or more days in 15% (11–22%) of events. Since the introduction of cricket helmet regulations, the proportion of injuries sustained while batting decreased from 54% (43–65%) to 38% (30–47%) (p = 0.026), and the proportion of injuries sustained while wicket keeping decreased from 19% (11-29%) to 6% (3-11%) (p=0.004).
Conclusion
Traumatic head and neck injuries occur at an incidence of approximately 7.3 per 100 players per season in elite Australian male and female cricket players. Whilst most injuries cause a low burden with respect to days unavailable, the risk of potentially serious or catastrophic consequences warrants further risk reduction strategies including tightening of the existing industry standard for helmets and governing body regulations.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic injuries to the head and neck are known to occur during cricket participation, however, a lack of clarity and consistency of reporting in the literature precludes understanding the true risk and direction for risk reduction strategies [1]. The occurrence of more severe traumatic head and neck injuries, including fatal and professional cricket career-ending, have been selectively documented in the media and later synthesised in the literature, including one fatality in elite Australian cricket in 2014 [2, 3]. Hospital admission data in Victoria (a State in Australia) has been reviewed to reveal an incidence of head and neck injuries requiring hospitalisation in the order of 1.2 per 1000 participants per season across all cricket participation levels [4].
Epidemiological research which has reviewed injury records of elite cricket players (primarily male) from key cricketing nations (United Kingdom, South Africa, New Zealand, West Indies) has reported traumatic and non-traumatic head and neck injuries as accounting for 0.2–9.1% of all injuries [1]. Most recently, a review of seven seasons of data from elite Australian cricket players has reported an average incidence of 55.4 head and neck injuries (traumatic and non-traumatic), including time loss and non-time loss injuries, per 100 male players per season, and 45.6 per 100 female players per season [5]. Excluding concussion and brain injuries, the incidence was 43.7 and 37.2 per 100 male and female players, respectively [5].
Head and neck injuries tend to be reported collectively in epidemiological research, however, a few studies which have reported types of injuries have revealed fracture, concussion, contusion, and laceration as more common [1]. The most common mechanisms reported in these studies are being hit by the ball, and the head hitting the ground whilst fielding [1]. Whether players were wearing a helmet at the time of injury is typically not reported [1], however, one study has reported injuries resulting from the ball contacting the player’s face between the peak and faceguard of the helmet [6]. Further research is needed to understand the types and mechanisms of traumatic head and neck injuries, and the efficacy of the cricket helmet, to target specific risk reduction strategies.
An industry standard for a cricket helmet including the faceguard was implemented in 2013, with a revision in 2019 to include additional protection of the upper neck (mastoid) region [7]. The International Cricket Council regulations do not require players to wear a helmet, however, if a batter playing at an international level chooses to wear a helmet it must comply with the industry standard. Cricket organisations of different nations and participation levels set their own regulations. In Australia at the elite level, players are required to wear a helmet that meets the industry standard when batting against pace bowling, wicket keeping up to the stumps (close to the batter) and fielding close (within seven meters) to the bat. This regulation was implemented at the elite Australian cricket level in July 2016. The impact of this regulation on the incidence and severity of traumatic head and neck injuries may be evaluated by comparing injury data prior to and since the 2016/17 season.
The purpose of this study is to retrospectively review clinical data of traumatic head and neck injuries sustained during cricket participation for elite Australian male and female cricket players between July 2010 and June 2022 (12 seasons) to improve understanding of (a) types of injuries sustained, specific injury incidence and severity (time loss); (b) playing positions most at risk, (c) mechanisms of injury, and; (d) the efficacy of the helmet regulation introduced in 2016 on injury incidence and severity. This information is intended to provide clearer direction for risk reduction strategies. Concussion has been excluded from this study due to the evolution of diagnostic sensitivity over time, the subjectivity of diagnosis, and in-depth analyses in similar cohorts reported previously [6, 8, 9].
Materials and Methods
Ethics approval was gained from an Institutional Ethics Committee (La Trobe University HEC20058) which waived the need for individual informed consent. This manuscript was prepared according to the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology-Sport Injury and Illness Surveillance (STROBE-SIIS) [10].
The study population included male and female cricket players participating in Australian State and National programs between 1 July 2010 and 30 June 2022 (12 seasons, 1 July–30 June aligns with player contract periods). The average number of players per season was 294 (173 male, 121 female).
Data was extracted from Cricket Australia’s Athlete Management System (AMS) (Fair Play AMS Pty Ltd). Data were recorded at the time by medical staff (doctor and/or physiotherapist) working with state/territory and national cricket teams. Head and neck injuries were identified as coded according to the Orchard Sports Injury and Illness Classification System (OSIICS) [11]. Injuries were included if they were a traumatic injury to the head or neck which occurred during a cricket match or training. Injuries that occurred to players during strength or conditioning training or outside of cricket were excluded. Injuries were excluded if the diagnosis was concussion only.
Data extracted included demographic information, diagnosis, activity at the time of injury, mechanism of injury, and other clinical notes to ascertain details such as helmet use, specialist consultation (e.g., maxillofacial surgeon, plastic surgeon, dentist, ophthalmologist), and sutures. Injury locations were coded as occurring to the skull (forehead/frontal bone, crown, parietal and temporal bones as would be protected by the shell of a helmet), face (ear, eye, orbit, nose, maxilla, mouth, mandible as would be protected by the faceguard of a helmet), or neck (anterior and lateral neck, and cervical spine). Time loss was the number of days a player was deemed unavailable, as recorded by the treating medical staff in accordance with the definition of being unavailable to participate in a match (even if a match was not scheduled to be played on that day). Time-loss data were excluded from analysis if the athlete experienced a concomitant illness or injury (including concussion) which may have affected availability. As mentioned in the introduction, our dataset included one case fatality which was unable to be graded in terms of time-loss from cricket and, therefore, excluded from the time-loss analysis.
Data were tabulated and analysed using Excel (Microsoft, 2016 MSO) and SPSS (version 25, IBM, Armonk, NY, USA), with significance set a-priori at p < 0.05. Descriptive statistics were used to characterise the players included in the sample and the presentation and circumstances of injuries. Injury incidence was calculated as the number of injuries per 100 players per season. Average injury incidence was calculated as the average of each incidence per season, and compared using a two-sample t-test. Proportions were calculated with a Wilson 95% confidence interval (CI) and compared using a two-sample z test. Days unavailable were not normally distributed, hence descriptive statistics are reported as the median and interquartile range (IQR).
Injury events were used to calculate overall head and neck injury incidence. Some injury events included concurrent injuries (e.g., player sustained a fracture and laceration from the same traumatic event), which were counted separately for the incidence of specific injury types. If a player with concurrent injuries required one or more days unavailable, the days unavailable were attributed to the more severe injury (as described in the clinical notes) and left blank for the concurrent less severe injury or injuries. If the player with concurrent injuries had no days unavailable, zero days were included in analyses for all concurrent injuries. If a player had a concurrent injury from the same traumatic event which is not included in this study (e.g., concussion), days unavailable were left blank for the injury or injuries included in this study. For sub-analyses, “time-loss and more serious injuries” were defined as those which met one or more of the following criteria: (a) one or more days unavailable, (b) hospital stay, (c) surgery or invasive procedure including sutures, or (d) fracture.
Results
199 traumatic injury events to the head and neck were recorded over the 12 seasons (male n = 126, mean age 24.7 ± 5.4 years; female n = 73, mean age 23.2 ± 5.2 years). This included 32 concurrent head and neck injury events, resulting in a total of 232 injuries (31 had 2 concurrent injuries, one had 3) and 205 injury locations (6 had 2 concurrent locations) for analysis by injury type.
The average incidence of head and neck injury events over the 12 seasons was 16.6 injury events per season (5.6 per 100 players per season: male 6.1, female 5.0). The incidence of injury events increased over the earlier half of the study period, and plateaued over the latter half of the study period (Fig. 1). The incidence of time loss and more serious injuries decreased over the latter half of the study period (Fig. 2). The average incidence of injury events prior to the introduction of helmet regulations was 3.9 (male 5.0, female 2.5) and from July 2016 onwards was 7.3 (male 7.0, female 7.8) (all p = 0.028, male p = 0.252, female 0.004). The average incidence of time-loss and more serious injury events prior to the introduction of helmet regulations was 1.9 (male 2.8, female 0.8) and from July 2016 onwards was 2.2 (male 2.2, female 2.2) (all p = 0.614, male p = 0.514, female 0.143).
Injuries were sustained during a match (59%, 95% CI 52–66%), match warm-up (6%, 4–11%), or training (34%, 28–41%). Ball collision was the primary mechanism (77%, 71–82%), followed by diving or falling (impact with ground and/or whiplash) (11%, 7–16%), and player collision (7%, 4–11%).
Contusions were the most common injury type (41% of all injuries, 35–48%), followed by lacerations (29%, 24–35%), fractures (11%, 8–16%), sprains (11%, 8–16%), and abrasions (7%, 4–11%). The face was most commonly injured (63%, 57–69%), followed by the neck (22%, 18–28%), and skull (15%, 11–20%). Further detail on specific injury locations and types are detailed in Table 1 and illustrated in Fig. 3. A concurrent concussion was diagnosed in 15% (11–21%) of injury events.
Injuries typically did not require the player to be unavailable for cricket (Table 1). The median days unavailable for time-loss and more serious injuries was 0 (IQR 0–6 days). Fifteen percent (11–22%) of the 168 injury events with data available (excluding cases with a concurrent concussion or other injury) required one or more days off. Mandible fractures were the only injury (with sufficient cases) that consistently required time off cricket (median 8 days, IQR 7–35 days). Seven percent (4–11%) of the 199 injury events required surgery, for which the median days unavailable was 25 (11–30).
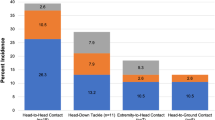
Injuries were most commonly sustained while batting (44%, 37–51%), followed by fielding (41%, 34–48%), wicketkeeping (10%, 7–15%), and bowling (5%, 3–9%) over the 12 seasons. Dividing the study period into pre- and post- the introduction of helmet regulations, the proportion of injuries sustained while batting decreased from 54% (43–65%) pre to 38% (30–47%) post (p = 0.026), and the proportion of injuries sustained while wicket keeping decreased from 19% (11–29%) pre to 6% (3–11%) post (p = 0.004) (Table 2, Fig. 4). The proportion of injuries sustained while fielding increased from 23% (15–34%) pre- to 51% (43–60%) post- the introduction of helmet regulations (p < 0.001). The proportion of time-loss and more serious injuries sustained while batting and wicketkeeping were similar pre- and post- the introduction of helmet regulations (Table 2). Since the introduction of helmet regulations, batters most commonly sustained injuries to the neck 43% (30–58%) and face 41% (28–56%). Injuries to the face were most commonly to the mandible (74%, 51–88%).
Injuries that occurred during training and warm-up accounted for 41% (34–48%) of injury events. Of these, the batting ‘nets’ environment was specified in the notes of 37% (27–48%) of events; 73% (56–86%) occurred to the batter and 27% (14–44%) to the bowler. Injuries sustained while bowling in the ‘nets’ environment was to the skull (50%, 22–78%) and face (50%, 22–78%), and 50% (22–78%) were time-loss or more serious injuries. Injuries that occurred whilst fielding in training or warm-ups were most commonly the result of ball impact (93%, 77–98%), of which misfielding was specified in the notes of 77% (58–89%) events.
Discussion
This study provides a comprehensive review of traumatic head and neck injuries (excluding concussion) in elite Australian cricket players over 12 seasons. In recent seasons, the incidence of traumatic head and neck injuries was 7.3 per 100 players per season. The incidence of these injuries increased in the latter half of the study period, particularly for female players which aligns with increased professionalism in the female part of the game in Australia. It is, therefore, possible that the increased number of these injuries may be related to more training and match exposure and increased resourcing of medical and sports science staff to detect and record injuries. The period in the latter half of the study period (circa 2015) also coincided with the introduction of a concussion policy across elite Australian cricket that required all head and neck impacts to be assessed and documented no matter how trivial the impact may be. This policy change undoubtedly would have increased the number of head and neck injuries recorded, especially those on the less severe end of the injury spectrum (non-time loss injuries). Other studies in cricket [12] and other sports [13, 14] have also reported large increases in reported concussions from the mid-2010s onwards, as this was an era when rigour around head impact recording increased in the vast majority of professional sports.
The burden of head and neck injuries with respect to days off cricket was low (median 0 days; only 15% of injuries required one or more days off), however, the severity (or potential severity) of head and neck injuries can not be dismissed. The data set included a fatality and some severe injuries requiring hospitalisation and surgery, and dental fractures which are permanent.
Batters have historically sustained the highest number of head and neck injuries compared to other player roles, however, the introduction of helmet regulations in July 2016 appears to have been an effective risk-reduction strategy. The data in this study was able to reveal that the proportion of all head and neck injuries that were sustained by batters has been reduced, particularly to the face. The proportion of time-loss and more serious head and neck injuries sustained by batters has trended towards a reduction, although not statistically significant.
The combination of an industry standard for cricket helmets and helmet regulations in elite Australian cricket are an effective risk-reduction strategy with respect to some injuries and are insufficient with respect to others. The industry standard, revised in 2013, stipulates that the helmet and faceguard must not allow the face to be contacted by the ball or faceguard [7]. Prior to the 2013 revision, traumatic facial injuries occurred when the ball could penetrate the gap between the helmet peak and faceguard, or the faceguard impacted the face. Since the introduction of helmet regulations, no injuries were recorded where the ball penetrated the gap between the helmet peak and faceguard, however, injuries continued to result from the faceguard impacting the face. The faceguard of helmets that meet the industry standard may impact the face if the helmet is not properly fitted and secured with the retention system and chin strap. Currently, manufacturers provide helmet-specific instructions regarding correct fit, including the use of the restraint system. However, we recommend the industry standard be revised to specify the requirements of the fit and restraint system. Player education regarding the importance of correct fit and use of the retention system may offer an additional risk reduction strategy.
Since the introduction of helmet regulations, batters primarily sustained injuries to the mandible and neck. The mandible is exposed to a ball coming from below the faceguard, highlighting an insufficiency of the faceguard. A revision of the industry standard may address this insufficiency by extending the ‘no contact’ zone of the face to include the mandible and adding a testing angle where the ball comes from below the faceguard.
Despite the introduction of neck protectors to protect the upper neck (mastoid) region, the neck remains largely unprotected for practical reasons. Impact on the neck away from the mastoid region is unlikely to cause a catastrophic injury such as vertebral artery dissection [15], so the risk may be weighed against the ability to perform when playing cricket. Neck protectors do not impede cricket performance and therefore should be part of helmet regulations going forward.
The industry standard for helmets does not currently prescribe requirements for the size or impact attenuation of the helmet peak. Clinical notes described multiple instances where a contusion resulted from impact to the peak of the helmet, raising the question of whether the peak focussed on the area of impact. Laboratory testing is needed to determine whether the peak creates an increased injury risk and if so, whether further regulation is required. Although outside of the scope of this study, we also note the occurrence of concussion resulting from impact to the helmet and reiterate the recommendation that the industry standard be revised to require increased impact attenuation of the helmet [9].
Fielders sustain approximately half of all head and neck injuries. One contributing factor to this finding may be a higher exposure for fielders. Another possible factor is that their role involves fielding a ball on the run, opening up the possibility of misfielding or colliding with another player, the ground, or a fixture. This risk may have increased with the increased intensity and athleticism of the newer and faster formats of cricket. Misfielding may be related to catching technical deficits or visibility issues as the ball colour (red, white, or pink) may be temporarily lost in the background (e.g., crowd, stadium, sky) by fielders. There may be an opportunity for risk reduction, for example more practice in these changing environments. Cervical sprain (whiplash) injuries often resulted from diving with or without head impact with the ground. Diving technique may be considered as a risk reduction strategy, along with fielding techniques more generally.
Injuries during training and warm-up accounted for approximately 40% of all injuries. Unlike match scenarios where attention is on one ball in play, some training and warm-up activities involve multiple balls in play at any given time. Groups of players may also be doing different drills beside one another, opening up the risk of a ball being unsighted or player collision. These settings offer more scope for risk reduction strategies to be implemented as they are much more controllable environments than match-play.
A strength of this study is the consistent recording of clinical notes for a large cohort of cricket players over the twelve seasons. As discussed, a limitation is that the evolution of the game, helmet technology and regulations, and recording requirements likely impacted the number and type of injuries over the study period. A further limitation is that helmet use was not required to be noted, precluding specific analyses of the efficacy of helmets. Instead, the efficacy of helmet regulations was assessed which required assumptions with respect to playing position and use in training. Similarly, fielding position was not required to be noted, precluding analyses of the specific risk of fielding close to the batter and the potential effect of the helmet regulation.
Head and neck impacts that resulted in concussion with no concurrent injury were excluded from this study. These exclusion criteria were chosen to focus attention on all other traumatic head and neck injuries, as concussion in elite Australian cricket players has been reported previously [8, 9, 16, 17]. The exclusion of both concussive injuries and head and neck impacts that do not result in concussion or injury precludes calculating the full incidence of traumatic head and neck events, and the risk of traumatic head and neck injuries as a proportion of all traumatic head and neck events.
Conclusion
Traumatic head and neck injuries occur at an incidence of approximately 7.3 per 100 players per season in elite Australian male and female cricket players. Whilst most injuries cause a low burden with respect to days unavailable, the risk of potentially serious or catastrophic consequences warrants further risk reduction strategies. The introduction of helmet regulations appears to have been an effective risk reduction strategy for batters and wicketkeepers, however, additional risk reduction may be offered by tightening these regulations. For instance, refining the industry standard and extending regulations at the governing body level. Ongoing player education and skill refinement also have a role.
Data availability statement
The data that support the findings of this study are not openly available due to reasons of sensitivity. Non-identifiable data may be made available by the corresponding author upon reasonable request and with approval from Cricket Australia.
References
Kodikara, D., Twomey, D. M., & Plumb, M. S. (2022). A systematic review of head, neck and-facial injuries in cricket. International Journal of Sports Medicine, 43(06), 496–504. https://doi.org/10.1055/a-1684-9033. Epub 2021/11/02.
Tripathi, M., Shukla, D. P., Bhat, D. I., Bhagavatula, I. D., & Mishra, T. (2016). Craniofacial injuries in professional cricket: No more a red herring. Journal of Neurosurgery, 40(4), E11. https://doi.org/10.3171/2016.2.Focus15341
Brukner, P., Gara, T. J., & Fortington, L. V. (2018). Traumatic cricket-related fatalities in Australia: A historical review of media reports. Medical Journal of Australia, 208(6), 261–264.
Kodikara, D., Plumb, M. S., & Twomey, D. M. (2020). A decade of head, neck and facial cricket injury hospitalisations in Victoria, Australia: From 2007/08 to 2016/17. Journal of Science and Medicine in Sport, 23(12), 1161–1165. https://doi.org/10.1016/j.jsams.2020.06.010
Orchard, J. W., Inge, P., Sims, K., Kountouris, A., Saw, A. E., Saw, R., et al. (2023). Comparison of injury profiles between elite Australian male and female cricket players. Journal of Science and Medicine in Sport, 26(1), 19–24. https://doi.org/10.1016/j.jsams.2022.12.002
Ranson, C., Peirce, N., & Young, M. (2013). Batting head injury in professional cricket: a systematic video analysis of helmet safety characteristics. British Journal of Sports Medicine, 47(10), 644–648.
British Standards Institute (BSI). (2019). Specification for head protectors for cricketers. BS 7928:2013+A1:2019. London: BSI Standards Ltd.
Hill, T., Orchard, J., & Kountouris, A. (2019). Incidence of concussion and head impacts in Australian elite-level male and female cricketers after head impact protocol modifications. Sports Health., 11(2), 180–185. https://doi.org/10.1177/1941738118811315
Saw, A. E., Howard, D. J., Kountouris, A., McIntosh, A. S., Orchard, J. W., Saw, R., et al. (2020). Situational factors associated with concussion in cricket identified from video analysis. Journal of Concussion, 4, 2059700220947197.
Bahr, R., Clarsen, B., Derman, W., Dvorak, J., Emery, C. A., Finch, C. F., et al. (2020). International Olympic Committee consensus statement: Methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). British Journal of Sports Medicine, 54(7), 372. https://doi.org/10.1136/bjsports-2019-101969
Orchard, J. W., Meeuwisse, W., Derman, W., Hägglund, M., Soligard, T., Schwellnus, M., et al. (2020). Sport Medicine Diagnostic Coding System (SMDCS) and the Orchard Sports Injury and Illness Classification System (OSIICS): Revised 2020 consensus versions. British Journal of Sports Medicine, 54(7), 397–401. https://doi.org/10.1136/bjsports-2019-101921
Orchard, J. W., Kountouris, A., & Sims, K. (2016). Incidence and prevalence of elite male cricket injuries using updated consensus definitions. Open access Journal of Sports Medicine, 7, 187–194. https://doi.org/10.2147/OAJSM.S117497
West, S. W., Cross, M., Trewartha, G., Taylor, A., Brooks, J., Kemp, S., et al. (2021). Trends in match concussion incidence and return-to-play time in male professional Rugby Union: A 16-season prospective cohort study. Brain Injury., 35(10), 1235–1244. https://doi.org/10.1080/02699052.2021.1972142. Epub 2021/09/09.
Adams, R., Lau, G. K., Dai, J. B., Li, A. Y., Cheung, K. P., Haider, S., et al. (2018). Evaluation of concussion incidence and modulating factors in the 2013–2017 Australian Football League. Cureus., 10(10), e3465. https://doi.org/10.7759/cureus.3465. Epub 2018/12/27.
Saw, A. E., McIntosh, A. S., & Kountouris, A. (2019). Vertebral artery dissection in sport: Expert opinion of mechanisms and risk-reduction strategies. Journal of Clinical Neuroscience, 68, 28–32. https://doi.org/10.1016/j.jocn.2019.07.016
Lallenec, L. M., Saw, A. E., Kountouris, A., Saw, R., & Orchard, J. (2021). Concussion in cricket: Clinical findings using Sport Concussion Assessment Tool and recovery timeframes. Journal of Concussion, 5, 2059700221993322.
James, K., Saw, A. E., Saw, R., Kountouris, A., & Orchard, J. W. (2021). Evaluation of CogSport for acute concussion diagnosis in cricket. BMJ Open Sport and Exercise Medicine., 7(2), e001061.
Acknowledgements
The authors would like to acknowledge the medical professionals who collected the data over the 12 year study period.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
TE, AS, AK and JO conceptualised and designed the study; TE and AS extracted and reviewed the data; TE and AS wrote the first draft of the manuscript, and all authors critically reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Anna Saw is a sport science and sport medicine research specialist at Cricket Australia. Alex Kountouris is the head of medical and sport science at Cricket Australia. John Orchard is the chief medical officer of Cricket Australia. Tane Eunson declares he has no conflicts of interest.
Ethics approval
Ethics approval was gained from an Institutional Ethics Committee (La Trobe University HEC20058).
Competing interests
Anna Saw, Alex Kountouris and John Orchard are all employed by Cricket Australia but are not funded specifically for this study. Tane Eunson has no competing interests within the last 3 years that are directly or indirectly related to this publication.
Informed consent
Informed consent specifically for this study was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eunson, T.H., Saw, A.E., Kountouris, A. et al. Traumatic Head and Neck Injuries in Elite Australian Cricket Players: Retrospective Analysis from 12 Seasons. JOIO 57, 1584–1591 (2023). https://doi.org/10.1007/s43465-023-00916-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-023-00916-4