Abstract
Introduction
The association between body mass index (BMI) and functional outcomes is unknown in elderly individuals with distal radius fracture (DRF).
Objective
The aim of this study is to evaluate if there is association between BMI and functional outcomes in patients older than 60 years with DRF treated conservatively.
Materials and Methods
A prospective observational study was performed. A total of 228 patients with extra-articular DRF were prospectively recruited. All patients were categorized by their BMI as normal, overweight, or obese. Functional outcomes were assessed after cast removal and at 1-year follow-up. The Disabilities of the Arm, Shoulder and Hand Outcome Measure (DASH), and Patient-Rated Wrist Evaluation (PRWE) questionnaires were used to assess upper limb and wrist/hand function, respectively, while the Jamar Dynamometer was used to assess grip strength.
Results
Of the total number of patients, 184 were female (80.7%), 87 were overweight (38.2%), and 111 were obese (48.7%). After cast removal, the correlations between BMI and functional outcomes were DASH 0.06 (p = 0.578), PRWE 0.04 (p = 0.692), and grip strength − 0.02 (p = 0.763). At 1-year follow-up, the correlations were DASH 0.55 (p = 0.036), PRWE 0.32 (p = 0.041), and grip strength − 0.21 (p = 0.043).
Conclusion
This study suggests that at 1-year follow-up, there was a low-to-moderate association between BMI and poor functional outcomes in elderly patients with extra-articular DRF treated conservatively.
Level of Evidence
Level IV, observational prospective study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal radius fracture (DRF) is one of the most common musculoskeletal injuries, representing 15–20% of all fractures treated by the emergency services [1]. DRFs have a bimodal distribution; the first peak is observed in pediatric patients, and the second peak is seen in patients aged 60 years and older [2]. In the latter age group, it is the second most common type of fracture, after hip fractures[3], and these fractures frequently result from low-energy trauma [4].
To select optimal therapeutic and preventive interventions, orthopaedic surgeons and physiotherapists should know the risk factors and prognostic factors of functional outcomes in patients with DRF. Older age, female gender, poor bone healing or an associated fracture of the ulnar styloid, a compensated workplace injury, lower socioeconomic status and level of education all contribute to poor clinical outcomes [2].
However, few studies have investigated the relationship between obesity and DRF severity following low-energy trauma [5, 6], even though obese patients have a 48% increased risk of trauma (including minor injuries and fractures). Obesity is associated with an increase in injuries to the upper limbs resulting from falls [7]. Additionally, up to 28% of women under 75 years of age with fractures resulting from a low energy mechanism are obese [8], and obesity is associated with an increase in the rate of falls from 24 to 92% [9].
The American Academy of Orthopedic Surgeons has provided some recommendations but they do not identify body composition or obesity in their algorithm for the treatment of DRFs [10]. Despite addressing many issues surrounding the treatment of DRF, the guidelines make no mention of the role that obesity might play in the initial evaluation of functional outcomes. To our knowledge, there are no studies that have evaluated functional outcomes in relation to BMI in elderly patients with DRF treated conservatively. We hypothesized that there is an association between BMI and functional outcomes in elderly patients with DRF treated conservatively.
Therefore, the aim of this study is to evaluate if there is an association between BMI and functional outcomes in patients older than 60 years with DRF treated conservatively.
Materials and Methods
Study Design
This research is a prospective observational study based on a quantitative approach and was approved by the IRB of the authors’ affiliated institutions. The Ethics Committee of the Central Metropolitan Health Service of Chile approved the study protocol on 10 January 2011, with registration number 0187. All patients’ respondents received an anonymous written informed consent included and this report does not contain any personal information that could lead to their identification.
Setting
Between January 2012 and March 2019, 228 patients over 60 years of age with an extra-articular DRF were recruited prospectively at the Clinical Hospital San Borja Arriaran. An orthopaedic surgeon, based on the clinical presentation and radiologic studies performed the diagnosis.
Participants
All patients were treated with closed reduction and plaster cast immobilization for 6–7 weeks, and a three-point index was used to assess the displacement of the DRF [11]. After cast removal, all patients were prescribed acetaminophen (500 mg, every 8 h, for 7 days). Conversely, patients were excluded if they (1) presented immediate complications after cast removal, such as complex regional pain syndrome type I, or carpal tunnel syndrome; (2) treated with surgical interventions such as reduction with percutaneous Kirschner wires fixation, or open reduction and internal fixation with volar or dorsal plates; or (3) uncontrolled nutritional and metabolic diseases.
Interventions
All patients were treated with a supervised physiotherapy program, consisting of hydrotherapy, manual therapy and an exercise program based on motor skill training. The program consisted of 12 sessions, 2–3 times per week and approximately 1-h long session [12].
Variables
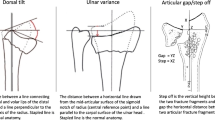
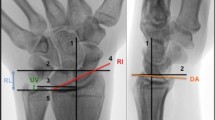
After cast removal, each patient underwent a radiological evaluation to assess the results of the orthopedic reduction. According to Kreder’s standardized technique [13], the orthopedic surgeon measured the following radiological parameters: radial inclination (normal: 21–25°), radial height (normal: 10–13 mm), volar tilt (normal: 7–15°), and ulnar variance (normal: 0.7–1.5 mm).
Body composition: weight was measured with the patient barefoot and in light clothing, while height was measured using a wall stadiometer, with the patient barefoot and upright and with the sagittal midline touching the backboard. BMI was calculated as weight in kg divided by the square of the height in meters (kg/m2). BMI was stratified into normal weight (18.5 ≤ BMI 24.9), overweight (25 ≤ BMI ≤ 29.9), and obesity (BMI ≥ 30) [14].
Functional assessments were performed after cast removal and at the 1-year follow-up. The primary outcome measured was the Disabilities of the Arm, Shoulder and Hand Outcome (DASH), this questionnaire was used to assess the upper limb function, scores range from 0 to 100 points, with higher scores indicating a worse condition [15]. The secondary outcome measures were the Patient-Rated Wrist Evaluation (PRWE), this questionnaire was used to assess the wrist/hand function, scores range from 0 to 100 points, with higher scores indicating a worse condition [16]. A Jamar Dynamometer was used to assess the grip strength. The participants were evaluated while seated, with their arm placed to the side of the body; they had their shoulders in neutral position, the elbow flexed to 90º, and the forearm in neutral rotation. Then patients were verbally instructed to make tight fists with all their strength to hold that position for 4 s with their hands and then rest for 30 s on each set. First, the unaffected side was evaluated and after that, the affected side was evaluated. In both cases, the highest value obtained from three attempts was recorded. An adjustment of 6% between the force of the dominant and nondominant sides was made. The final result was expressed as a percentage relative to the unaffected side [17]. These patients reported outcome measures have shown good validity, reliability, and responsiveness in the assessment of patients with DRF [18]. Physiotherapists not associated with the research team to blind the results performed the assessments.
Statistical Analysis
The sample size was calculated with the correlation point bi-serial model and “a priori” method was used with an effect size of 0.2 with a value of α = 0.05, and a statistical power of 90%, a minimum of 207 patients is needed. This minimal sample size estimate was increased by 10%, taking into consideration the potential dropouts, giving a total of 227 patients. The sample size was determined using the G-Power software, version 3.1.
Statistical analysis was performed using Stata 13.0 software. Continuous variables are presented as mean and standard deviation, and the categorical variables as number and percentage. The Spearman’s coefficient was used to determine the correlation between BMI and functional outcomes evaluated using the DASH and PRWE questionnaires, and grip strength with a Jamar dynamometer. Finally, the level of correlation was considered as follows: negligible (0–0.2), low (0.2–0.5), moderate (0.5–0.7), high (0.7–0.9), and very high (0.9–1) [19].
Results
The baseline information characteristics of the study group are shown in Table 1. A total of 228 patients were included, of which 184 were female (80.7%), with a mean age of 68.8 years and standard deviation (SD) of 5.2. The mean height of the included patients was 1.5 m (SD = 0.8), and the mean weight was 68.6 kg (SD = 5.3), corresponding to a BMI of 30.1 kg/m2 (SD = 5.4). When stratified by BMI, 30 patients (13.1%) were classified as normal weight, 87 (38.2%) were overweight, and 111 (48.7%) were obese.
The results of the functional evaluations are shown in Table 2. Immediately after cast removal, we did not observe a direct correlation between BMI and the functional outcome measures (p > 0.05). At the 1-year follow-up, BMI was positively correlated with DASH 0.55 and PRWE 0.32. Furthermore, higher BMI was correlated with lower grip strength − 0.21; these Spearman’s correlation coefficient values indicate low-to-moderate correlation between BMI and functional outcomes, and the p values were below 0.05, indicating that the relationships were statistically significant.
Discussion
Main Findings of the Present Study
The present observational prospective study evaluates if there is an association between BMI and functional outcomes in patients older than 60 years with DRF treated conservatively with closed reduction and cast immobilization. In the present study, a bivariate analysis of patients stratified into normal weight, overweight, and obese demonstrated that there was a low-to-moderate association between obesity and poor functional outcomes in these patients at 1-year follow-up.
Comparison with Other Studies
Obesity is increasing worldwide, with various subsequent health problems, but it is not only reflected by metabolic diseases, but also by orthopedic problems such as fractures [6, 20]. Despite this, the relationship between overweight and risk of fracture is unclear. Some studies showed that an increase in body weight and bone mass reduces the risk of fracture [21, 22]. Conversely, other studies showed that obesity may increase the rate of musculoskeletal injuries and long-bone fractures, particularly among postmenopausal women [23, 24]. Additionally, the evidence is also unclear on whether obesity is associated with the severity of DRFs [5, 6, 25].
Regarding the association between BMI and functional outcomes after DRF, the following retrospective studies have provided findings in patients with DRF that are treated surgically. One study showed that both obese and non-obese patients have excellent functional outcomes after surgical treatment with volar plate fixation, without differences between groups at the 3-month and 1-year follow-up [26]. Another study showed that overweight patients may experience less function and disability after DRF, but this difference is not statistically significant [25]. The last study showed that normal and obese patients with DRF treated with volar plate fixation have no significant differences in functional outcomes at 7 years of follow-up [27]. However, there is no evidence of prospective studies that have assessed the relationship between BMI and functional outcomes in elderly patients with DRF treated conservatively.
Implication and Explanation of Findings
Regarding our findings, we hypothesized that the positive association between BMI and DASH questionnaire could be explained; as obese women use their upper extremities more extensively to facilitate standing from a seated position, we think that upper limb function could be more affected than in women with normal weight. Another explanation may be attributable to differences in baseline activity that may influence the perception of disability. Some studies in arthroplasty patients showed that obese do not reach the same functional outcomes as their non-obese [28, 29]. These patients may have a greater fall risk due to their decreased mobility and muscle strength [11]. Studies in geriatric patients further support these findings, showing that obese patients report worse functional outcomes and greater disability [30, 31]. Overall, obese patients may have a lower functional baseline that could bias their self-reported disability and could explain the observed differences in the correlation coefficient value of the DASH questionnaire at the 1-year follow-up. These findings reinforce the need for physicians and physiotherapists to identify subjects with high BMI and promote behaviors to minimize the adverse health consequences, just as they could be the functional limitations related to DRF. Regarding the relationship between BMI and handgrip strength, according to our findings, some studies [32,33,34] have reported a negative association between increased BMI and decrease handgrip strength. This could be explained based that the BMI is an indicator or index and it is unable to differentiate between the weight changes which are due to an increase or decrease in the muscularity and the body fat percentage.
Strengths and Limitations
One strength of our study to our knowledge is that this is the only prospective study that evaluates the association between BMI and functional outcomes in patient with extra-articular DRF treated conservatively. Second, in our study, we performed a sample size calculation to be able to make a higher statistical inference to improve the applicability of the results. Finally, it is the only study that evaluates the association with a 1-year follow-up prospectively.
One of the main limitations of our study was the use of simple correlation. We only addressed the influence of BMI status on functional outcomes and did not consider other variables or comorbidities that could act as confounding factors for the outcomes obtained. Another limitation is a lack of information on changes to BMI during the follow-up period, as the BMI was measured only once. Finally, using BMI as a measure of weight does not provide a direct measure of body fat amount and distribution, which may affect the risk of comorbidities independent of BMI; thus, our results should be taken with caution.
Conclusion, Recommendations, and Future Directions
At 1-year follow-up, there was a low-to-moderate association between BMI and poor functional outcomes in patients older than 60 years with extra-articular DRF that was treated conservatively. Future studies are needed with higher quality that consider controlling lifestyle factors that could influence functional limitations in patients with DRF.
References
Singer, B. R., McLauchlan, G. J., Robinson, C. M., & Christie, J. (1998). Epidemiology of fractures in 15 000 adults: The influence of age and gender. Journal of Bone and Joint Surgery, 80(2), 243–248. https://doi.org/10.1302/0301-620x.80b2.7762.
MacIntyre, N. J., & Dewan, N. (2016). Epidemiology of distal radius fractures and factors predicting risk and prognosis. Journal of Hand Therapy, 29(2), 136–145. https://doi.org/10.1016/j.jht.2016.03.003.
Ray, N. F., Chan, J. K., Thamer, M., & Melton, L. J. (1997). Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: Report from the National Osteoporosis Foundation. Journal of Bone and Mineral Research, 12(1), 24–35. https://doi.org/10.1359/jbmr.1997.12.1.24.
Diaz-Garcia, R. J., Oda, T., Shauver, M. J., & Chung, K. C. (2011). A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. Journal of Hand Surgery America, 36(5), 824-835.e2. https://doi.org/10.1016/j.jhsa.2011.02.005.
Ebinger, T., Koehler, D. M., Dolan, L. A., Mcdonald, K., & Shah, A. S. (2016). Obesity increases complexity of distal radius fracture in fall from standing height. Journal of Orthopaedic Trauma, 30(8), 450–455. https://doi.org/10.1097/BOT.0000000000000546.
Acosta-Olivo, C., Gonzalez-Saldivar, J. C., Villarreal-Villarreal, G., Torres-Botello, A., Gomez-Garcia, E., Tamez-Mata, Y., & Peña-Martinez, V. (2017). Correlation between obesity and severity of distal radius fractures. Orthopaedic & Traumatology: Surgery & Research, 103(2), 199–202. https://doi.org/10.1016/j.otsr.2016.12.007.
Jones, C. B. (2011). Management of upper extremity injuries in obese patients. Orthopaedic Clinics of North America, 42(1), 11–19. https://doi.org/10.1016/j.ocl.2010.08.002.
Premaor, M. O., Pilbrow, L., Tonkin, C., Parker, R. A., & Compston, J. (2010). Obesity and fractures in postmenopausal women. Journal of Bone and Mineral Research, 25(2), 292–297. https://doi.org/10.1359/jbmr.091004.
Hooker, E. R., Shrestha, S., Lee, C. G., Cawthon, P. M., Abrahamson, M., Ensrud, K., et al. (2017). Obesity and falls in a prospective study of older men: The osteoporotic fractures in men study. Journal of Aging and Health, 29(7), 1235–1250. https://doi.org/10.1177/0898264316660412.
Lichtman, D. M., Bindra, R. R., Boyer, M. I., Putnam, M. D., Ring, D., Slutsky, D. J., et al. (2010). Treatment of distal radius fractures. Journal of American Academy of Orthopaedic Surgeons, 18(3), 180–189. https://doi.org/10.5435/00124635-201003000-00007.
Alemdaroǧlu, K. B., Iltar, S., Aydoǧan, N. H., Say, F., Kilinç, C. Y., & Tiftikçi, U. (2010). Three-point index in predicting redisplacement of extra-articular distal radial fractures in adults. Injury, 41(2), 197–203. https://doi.org/10.1016/j.injury.2009.08.021.
Gutiérrez-Espinoza, H., Arriagada-Núñez, V., Araya-Quintanilla, F., Zavala-González, J., Rubio-Oyarzún, D., Sfeir-Castro, R., & Gana-Hervias, G. (2018). Physical therapy in patients over 60 years of age with a massive and irreparable rotator cuff tear: A case series. Journal of Physical Therapy Science, 30(8), 1126–1130. https://doi.org/10.1589/jpts.30.1126.
Kreder, H. J., Hanel, D. P., McKee, M., Jupiter, J., McGillivary, G., & Swiontkowski, M. F. (1996). X-ray film measurements for healed distal radius fractures. Journal of Hand Surgery America, 21(1), 31–39. https://doi.org/10.1016/S0363-5023(96)80151-1.
WHO. (2015). Preventing and managing the global epidemic of obesity. WHO. World Health Organization.
Hudak, P. L., Amadio, P. C., & Bombardier, C. (1996). Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder, and head). American Journal of Industrial Medicine, 29(6), 602–608. https://doi.org/10.1002/(SICI)1097-0274(199606)29:6%3c602::AID-AJIM4%3e3.0.CO;2-L.
MacDermid, J. C. (1996). Development of a scale for patient rating of wrist pain and disability. Journal of Hand Therapy, 9(2), 178–183. https://doi.org/10.1016/S0894-1130(96)80076-7.
Trampisch, U. S., Franke, J., Jedamzik, N., Hinrichs, T., & Platen, P. (2012). Optimal jamar dynamometer handle position to assess maximal isometric hand grip strength in epidemiological studies. Journal of Hand Surgery America, 37(11), 2368–2373. https://doi.org/10.1016/j.jhsa.2012.08.014.
Kleinlugtenbelt, Y. V., Krol, R. G., Bhandari, M., Goslings, J. C., Poolman, R. W., & Scholtes, V. A. B. (2018). Are the patient-rated wrist evaluation (PRWE) and the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire used in distal radial fractures truly valid and reliable? Bone & Joint Research, 7(1), 36–45. https://doi.org/10.1302/2046-3758.71.BJR-2017-0081.R1.
Mukaka, M. M. (2012). Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Medical Journal, 24(3), 69–71.
Compston, J. (2013). Obesity and fractures. Joint Bone Spine, 80(1), 8–10. https://doi.org/10.1016/j.jbspin.2012.07.016.
De Laet, C., Kanis, J. A., Odén, A., Johanson, H., Johnell, O., Delmas, P., et al. (2005). Body mass index as a predictor of fracture risk: A meta-analysis. Osteoporosis International, 16(11), 1330–1338. https://doi.org/10.1007/s00198-005-1863-y.
Xiang, B. Y., Huang, W., Zhou, G. Q., Hu, N., Chen, H., & Chen, C. (2017). Body mass index and the risk of low bone mass-related fractures in women compared with men: A PRISMA-compliant meta-analysis of prospective cohort studies. Medicine (United States). https://doi.org/10.1097/MD.0000000000005290.
Johansson, H., Kanis, J. A., Odén, A., McCloskey, E., Chapurlat, R. D., Christiansen, C., et al. (2014). A meta-analysis of the association of fracture risk and body mass index in women. Journal of Bone and Mineral Research, 29(1), 223–233. https://doi.org/10.1002/jbmr.2017.
Kim, S. H., Yi, S. W., Yi, J. J., Kim, Y. M., & Won, Y. J. (2018). Association between body mass index and the risk of hip fracture by sex and age: A prospective cohort study. Journal of Bone and Mineral Research, 33(9), 1603–1611. https://doi.org/10.1002/jbmr.3464.
Montague, M. D., Lewis, J. T., Moushmoush, O., & Ryu, J. (2019). Distal radius fractures: Does obesity affect fracture pattern, treatment, and functional outcomes? Hand, 14(3), 398–401. https://doi.org/10.1177/1558944717750915.
Hall, M. J., Ostergaard, P. J., Dowlatshahi, A. S., Harper, C. M., Earp, B. E., & Rozental, T. D. (2019). The impact of obesity and smoking on outcomes after volar plate fixation of distal radius fractures. Journal of Hand Surgery America, 44(12), 1037–1049. https://doi.org/10.1016/j.jhsa.2019.08.017.
Ruckenstuhl, P., Bernhardt, G. A., Wolf, M., Sadoghi, P., Cip, J., Leithner, A., & Gruber, G. (2019). Influence of body mass index on health-related quality of life after surgical treatment of intra-articular distal radius fractures. A retrospective 7-year follow-up study. Hand Surgery & Rehabilitation, 38(6), 364–368. https://doi.org/10.1016/j.hansur.2019.09.004.
Gross, C. E., Lampley, A., Green, C. L., DeOrio, J. K., Easley, M., Adams, S., & Nunley, J. A. (2016). The effect of obesity on functional outcomes and complications in total ankle arthroplasty. Foot and Ankle International, 37(2), 137–141. https://doi.org/10.1177/1071100715606477.
Vincent, H. K., Horodyski, M. B., Gearen, P., Vlasak, R., Seay, A. N., Conrad, B. P., & Vincent, K. R. (2012). Obesity and long term functional outcomes following elective total hip replacement. Journal of Orthopaedic Surgery and Research, 7(1), 16. https://doi.org/10.1186/1749-799X-7-16.
Friedmann, J. M., Elasy, T., & Jensen, G. L. (2001). The relationship between body mass index and self-reported functional limitation among older adults: A gender difference. Journal of the American Geriatrics Society, 49(4), 398–403. https://doi.org/10.1046/j.1532-5415.2001.49082.x.
An, R., & Shi, Y. (2015). Body weight status and onset of functional limitations in U.S. middle-aged and older adults. Disability and Health Journal, 8(3), 336–344. https://doi.org/10.1016/j.dhjo.2015.02.003.
Lad, U. P., Satyanarayana, P., Shisode-Lad, S., Siri, C. C., & Ratna, K. N. (2013). A study on the correlation between the Body Mass Index (BMI), the body fat percentage, the handgrip strength and the handgrip endurance in underweight, normal weight and overweight adolescents. Journal of Clinical and Diagnostic Research, 7(1), 51–54. https://doi.org/10.7860/JCDR/2012/5026.2668.
Sánchez Torralvo, F. J., Porras, N., Abuín Fernández, J., García Torres, F., Tapia, M. J., Lima, F., et al. (2018). Valores de normalidad de dinamometría de mano en España Relación con la masa magra. Nutricion Hospitalaria, 35(1), 98–103. https://doi.org/10.20960/nh.1052.
Araujo, A. B., Chiu, G. R., Kupelian, V., Hall, S. A., Williams, R. E., Clark, R. V., & McKinlay, J. B. (2010). Lean mass, muscle strength, and physical function in a diverse population of men: A population-based cross-sectional study. BMC Public Health., 10(1), 508. https://doi.org/10.1186/1471-2458-10-508.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article (Universidad de las Américas 4811).
Author information
Authors and Affiliations
Contributions
HG-E, FA-Q, CO-H: study design. FA-Q, IC-V, MR-R: data collection and analysis. HG-E, FA-Q, CO-H, IC-V, MR-R, JV-F: manuscript preparation. HG-E, FA-Q, CO-H, IC-V, MR-R, JV-F: final approval.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gutiérrez-Espinoza, H., Olguín-Huerta, C., Cuyul-Vásquez, I. et al. Association Between Body Mass Index and Functional Outcomes in Elderly Patients with Extra-articular Distal Radius Fracture: A Prospective Observational Study. JOIO 55, 1009–1014 (2021). https://doi.org/10.1007/s43465-021-00358-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00358-w