Abstract
Purpose
To compare the effects of three modalities of pain management i.e. SSNB (suprascapular nerve block) with NIR (non invasive rehabilitation), IAI (intra articular injection) with NIR and, NIR alone in idiopathic frozen shoulder patients.
Methods
A double blinded randomized clinical trial was conducted. 60 cases of idiopathic frozen shoulder were selected and randomly divided into three treatment groups; group 1: NIR, group 2: NIR + SSNB, group 3: NIR +IAI. Range of motion, pain score and disability (SPADI: shoulder pain and disability index) score were evaluated pre-treatment and at 12 weeks follow up.
Results
All three groups were homogenous and comparable regarding their age, sex ratio, pretreatment pain score, disability score and range of motion. There was significant improvement (p < 0.05) post treatment in all three groups with respect to pain score, disability score and range of motion. SSNB with NIR group patients demonstrated better improvement in all parameters examined, which was statistically significant in pain score, disability score and internal rotation but was statistically equivalent for total range of motion and external rotation as compared to shoulder injection group.
Conclusion
SSNB in combination with non invasive rehabilitation is an effective and safe mode of treatment for idiopathic frozen shoulder. Present study also proves that SSNB with NIR is a more effective mode of treatment for idiopathic frozen shoulder as compared to NIR alone or in combination with IAI.
Level of evidence: Level 1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adhesive capsulitis (frozen shoulder) is characterized by painful, gradual loss of both active and passive glenohumeral motion due to capsular inflammation leading to fibrosis and contracture of the glenohumeral joint capsule [1]. Frozen shoulder can be either primary (idiopathic as in there is no detectable underlying cause) or secondary. Secondary frozen shoulder is defined as that associated with trauma, cardiovascular disease, hemiparesis, or diabetes. The prevalence of frozen shoulder is 2–5% and commonly affects women and patients with diabetes [2, 3]. The pathology in the frozen shoulder is thickening and fibrosis of the shoulder joint capsule and soft tissues around the rotator interval [4,5,6]. Many modalities of treatment have been studied in the literature, including physical rehabilitation alone or in combination with intraarticular steroids, suprascapular nerve block, surgery, etc. [7,8,9]. But there is relatively very little evidence to support or refute the better efficacy of one modality of treatment over the other.
Recently suprascapular nerve block (SSNB) and intraarticular injection (IAI) as treatment of painful conditions of the shoulder have been studied extensively [10, 11]. Both SSNB and IAI have been shown to be the safe and efficacious modality of pain management in the shoulder joint, but till now there is no higher level of evidence study done to show the superiority of one modality of treatment over the other in idiopathic frozen shoulder. Thus, a well-designed Randomized Control Trial (RCT) comparing the efficacy of Non-Invasive Rehabilitation (NIR) therapy following SSNB with NIR following IAI or NIR alone is the need of the hour.
The suprascapular nerve runs through the posterior triangle of the neck, deep into the trapezius and omohyoid muscles pass through the suprascapular notch inferior to the superior transverse scapular ligament (STSL) and enter the supraspinous fossa. Around 70 percent of the sensory supply of the shoulder joint is by the suprascapular nerve [12]. It also supplies acromioclavicular joint, subacromial bursa, coracohumeral ligament, and coracoacromial ligaments and gives motor branches to supraspinatus and infraspinatus [13]. Previous studies in the literature have shown that ultrasound-guided SSNB using 10 ml of 0.5% bupivacaine and 2 ml injection of methylprednisolone acetate (40 mg in 1 ml) is a safe and reproducible method of giving nerve block [14]. We can see only few studies on this topic comparing single injection of SSNB with intra articular injection. We can find only one study [15] in literature comparing 3 modalities,but the drawback of the study was that the patients were not homogenous. Also in this study steroid injection was repeated up to 3 doses.
Here we designed a randomized trial to compare the outcomes of three modalities of treatment i.e. SSNB (suprascapular nerve block) with NIR (noninvasive rehabilitation), IAI (intraarticular injection) with NIR and, only NIR in idiopathic frozen shoulder patients. Our hypothesis was SSNB with NIR is more effective than IAI with NIR or NIR alone in treating idiopathic frozen shoulder.
Materials and Methods
This randomized control trial (RCT) was performed on patients presenting to the shoulder clinic of a tertiary care Centre. Institutional ethics committee clearance was obtained before enrolling cases. Patients between 45 and 70 years of age, either gender who were diagnosed with frozen shoulder, and those who were consenting to participate in the trial were included. These patients had no much symptomatic relief after an initial course of physiotherapy and analgesics (minimum 6 weeks). Inclusion criteria’s were (a) Gross limitation of passive shoulder external rotation, (b) had their pain interfering with activities of daily living, (c) painful restriction of both active and passive elevation to less than hundred-degrees, (d) normal radiological appearance, (e) no known secondary causes, (f) patients with two negative tests out of following three: Neer’s impingement test, Hawkins Kennedy test, Jobe’s isolation test.
Patients with degenerative pathology (rotator cuff tear, supraspinatus tendinitis) by clinical examination, history of any trauma/injury to the shoulder, cervical pathology, inflammatory arthritis, psychiatric disorders, contraindications for steroid injection (e.g. uncontrolled diabetes mellitus, advanced osteoporosis), known lignocaine/bupivacaine or methylprednisolone drug allergy, any deformity in the affected upper limb, and trauma history in previous 4 weeks were excluded from the study.
Our sample size was calculated based on assuming the power of the study to be 80% and type 1 (α) error of 0.05. After calculating this we required a minimum of 20 patients in each of 3 groups. Out of 96 patients assessed for eligibility, 60 patients met the inclusion criteria. Patients were divided into three groups using block randomization method. Since we had selected only idiopathic frozen shoulder patients, we did not further stratify the patients. Patients were randomly allocated into 3 blocks of 20 patients in each group using a random number generation technique by computer. Patients and the investigator was blinded regarding which group they belong to. The pre-treatment shoulder range of motion was measured using a goniometer. The patients were evaluated for pain and disability scores using shoulder pain and disability index (SPADI).
Written consent for participation and intervention procedure was obtained from all the participants. All patients in the study group were evaluated for any systemic or local infection at the injection site, any allergic reaction to drugs like bupivacaine or lidocaine, or methylprednisolone acetate injection. Coagulation profile and HbA1c levels were obtained before the procedure.
(a) Group 1: This group included 20 patients who underwent only rehabilitation therapy which included shoulder range of motion exercises, stretching and strengthening exercises, short wave diathermy, and occupational therapeutic interventions.
(b) Group 2: This group included 20 patients who received a single suprascapular nerve block under ultrasound guidance (by Dr. YKB) and rehabilitation therapy. With the patient in the sitting position the ultrasound probe is placed horizontal to the scapular spine and the supraspinous fossa is checked by moving the probe anteriorly. The suprascapular notch is found by slowly locating the probe laterally. The pulsating suprascapular artery is found on color doppler ultrasound and is a good indicator for the location of suprascapular nerve [8]. SSNB was given by 10 ml of 0.5% bupivacaine and 2 ml injection methylprednisolone acetate (40 mg in 1 ml).
(c) Group 3: This group included 20 patients who received a single injection of an intraarticular steroid injection using a standard posterior approach (by Dr. VGG) and rehabilitation therapy. The solution was prepared using 3 ml 1% lidocaine, 2 ml of methylprednisolone acetate (40 mg in 1 ml), and 7 ml of normal saline.
All patients who underwent the interventional procedure were discharged on the same day evening on mild analgesics (Tab.Paracetamol 500 mg thrice daily for 3 days) and were encouraged to do physiotherapy exercises from the next day onwards. Post-treatment evaluation was done at 12 weeks for ROM and SPADI. These measurements were conducted by another doctor (by Dr. UG) blinded to this study, and the treatment methods were not explained to avoid bias, the authors who did perform the injections were not allowed to follow up the patients. Post injection the patients were asked to guess the type of injection given, and the results (data not presented) showed that patients could not identify the type of injection given, confirming the blinding of the study.
Data were collected in a pre-designed format and analyzed using Statistical Package for Social Sciences (SPSS Inc Chicago, IL, Version 17.0 for Windows). The normality of measurable data was tested using the Kolmogorov–Smirnov test. The normally distributed measurable data were analyzed to find out a significant difference between the groups using ANOVA whereas the skewed data were analyzed using Kruskal–Wallis test. The effect of therapy within the group was tested using student t test or Wilcoxon signed-rank test as per their normality/skewness respectively. The association of the categorical data with the groups was calculated using the Chi square test. A p value of less than 0.05 is considered statistically significant.
Results
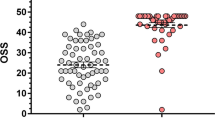
60 patients who met the inclusion criteria were randomly allocated into one of the three treatment groups. Each group consisted of 20 patients. All patients were aged between 45 and 70 years and each group were comparable regarding the mean age of the patient. Table 1 lists the demographic details of the patients. In our study, there were 35 females and 25 males and all 3 groups were comparable in their sex ratio. 70 percent of the study group had left-sided shoulder involvement. Interestingly non-dominant shoulder involvement was more common accounting for 91.66% (55 out of 60 patients) which was comparable in all three groups. We evaluated the patients before any treatment using shoulder pain and disability score and range of motion calculation. All three groups were comparable in their range of motion and pain and disability scores. Post-treatment evaluation was done at 12 weeks. 6 parameters were evaluated including pain score, disability score, mean abduction (MA), mean external rotation (MER), mean internal rotation (MIR), and a total range of motion (TROM) (Tables 2,3,4,5,6,7). All three groups of patients showed significant improvement in their pain score, disability score, and range of motion. A statistically significant improvement was seen in all parameters when compared between pre-intervention and post-intervention values, as the p values for all comparisons among the three groups were < 0.05. Amongst the three groups, the maximum improvement in all parameters was seen in SSNB + NIR group followed by SI + NIR group (Table 8, Fig. 1).
Discussion
This is a double-blinded randomized control study, comparing three modalities of treatment for idiopathic frozen shoulder. The key features of this study were (a) the study population was homogenous in terms of age, sex, pathology, comorbidities, (b) we used a valid and reproducible method for measurement of disability and pain, (c) we excluded shoulder pathology other than frozen shoulder with radiological changes and clinically which would have adversely affected the study results, (d) in our study suprascapular nerve block was given under ultrasound guidance after positively identifying the nerve unlike few of the other studies where it was given by blind technique [15] which reduced the chances of a unsuccessful block. Idiopathic frozen shoulder is a common problem presenting as pain that may be mild to severe and as a progressive loss of movement resulting in loss of function [16]. Pathoanatomically the common denominator is an inflammatory vascular proliferation followed by thickening, scarring, and contractures of the joint capsule and the rotator interval. Though it follows a self-limiting course, the pain and functional disability produced has a detrimental effect on the socioeconomic status of the society.
Since the pain plays an integral part in frozen shoulder pathology, breaking this vicious cycle between pain and non-compliance to therapeutic exercises is a must to achieve satisfactory results [17]. That is why many of the treatment modalities like oral NSAIDs, physical therapy [18], manipulation under anesthesia, intraarticular steroids, ultrasonography-guided hydro dissection, arthroscopic capsular release, and suprascapular nerve block to name a few have been advocated to reduce the disabilities imposed by the disease. NSAIDs or short course corticosteroids used in the early stage of the disease are not to relieve pain completely but instead used so that the patient can do physical therapy effectively. But till now there is no uniform protocol with added advantages over the others has been identified. Injection therapies like suprascapular nerve block (SSNB) or intraarticular injection should be considered before proceeding to surgical interventions like arthroscopic capsular release or manipulation under anesthesia (MUA) and this will relieve pain so that the patient can do physical or rehabilitation therapy much better and helps in shorten natural history of adhesive capsulitis. Moreover, complications like fractures, glenoid and labral injuries, rotator cuff pathology, and neuropraxia are associated with MUA [18]. SSNB has been studied extensively as the modality of pain management recently in many pathologies [3,4,5]. But most of the studies have failed to definitively show the superiority of one modality of treatment over the other. Klç et al. did an RCT comparing SSNB plus physical therapy to physical therapy alone for the treatment of adhesive capsulitis [19]. They conclude that the addition of SSNB to physical therapy improves pain and functional status of patients with adhesive capsulitis. In our study in addition to two groups as demonstrated by Klç Z et al. we had another comparable group of IAI plus NIR which added strength to our study.
Our study showed a statistically significant improvement in SPADI pain sub score, SPADI disability sub score, and range of motion in all three modalities of treatment. Although all the modalities were effective in reducing pain, patients in group II had maximum pain relief post therapy with mean pre-intervention pain score of 59% and post-intervention pain score of 32.85%. Patients in groups I and III also had statistically significant pain relief (p value 0.000) with mean pain score in group I and group III before treatment were 58.50% and 59.60% respectively and post-treatment scores were 46.50% and 38.45% respectively. So intra-articular steroids in combination with physiotherapy were more effective than physiotherapy alone in reducing pain at the end of three months. This finding is consistent with Abdelshafi et al. [15]. Though Taskaynatan et al. [20] had concluded that none among SSNB and SI was superior to each other in relieving pain in non-specific shoulder pain. In contrary, Green et al. [21] had concluded that physiotherapy alone was probably not effective at all in relieving pain in adhesive capsulitis.
The decrease in disability in all the three groups were also assessed using SPADI disability scale and the maximum decrease in disability was seen in patients in group II with mean pre-treatment disability index of 60.05% as compared to 35.48% of post-treatment disability index at the end of three months. The other two groups also had statistically significant (p value 0.000) decrease in disability, though group III had more improvement in disability in the post-treatment period as compared to group I. This is in accordance with the literature as Jones et al. [22] and Buchbinder et al. [23] both have demonstrated the efficacy of SSNB and SI in improving shoulder function. In contrast, Abdelshafi et al. [19] did not show any significant improvement in SPADI disability index after twelve weeks follow-up in any of the three groups in patients with frozen shoulder, though significant improvement in SPADI pain score was there. Dahan et al. [10] also found no significant improvement in shoulder function after SSNB, though improvement in pain was there at the end of 1 month. Total SPADI score was also significantly improved in all the three groups and improvement in group II was more marked as compared to group I and III. Between groups I and III, the latter showed more significant improvement at the end of 3 months. This is in accordance with Abdelshafi et al. [15], which also showed significant improvement in total SPADI score at the end of 12 weeks in patients treated with ultrasound-guided SSNB plus physiotherapy as compared to physiotherapy alone or in combination with SI.
The exact mechanism of pain relief in SSNB is yet to be identified, though many hypotheses have been proposed which include ‘wind down’ phenomenon causing a decrease in central sensitization of dorsal horn nociceptive neurons (because of a reduction of peripheral nociceptive input), decrease in pain-producing substance in the synovium, and infiltration into the supraspinatus muscle during the block. The superiority of SSNB over intraarticular injection has been proven from our study. This might be attributed to [1] wide area of sensory supply by the suprascapular nerve to about 70% of the shoulder joint, including the superior and posterosuperior regions of the shoulder joint and capsule, and the acromioclavicular joint, also it supplies motor branches to the supraspinatus and infraspinatus muscles. [2] Possibility of successful infiltration into the surrounding tissues in an attempted intraarticular injection. Previous studies have shown a low success rate of intraarticular injection when injected by a blind method as compared to the ultrasound-guided method [9]. In our study, we used the anatomical landmark method [24] for intraarticular injection of shoulder since that is the most commonly used method worldwide. Few of the reported complications of SSNB like pneumothorax [25] was not seen in our study which can be attributed to the use of ultrasound guidance for the procedure. Unlike intraarticular corticosteroid injection, there is no risk of iatrogenic septic arthritis, atrophy of cartilage in the long run in SSNB.
Limitations
The limitations of our study were that we didn’t add any placebo injection in group I to compare the effect of any injection with other groups. We didn’t do MRI of shoulders to rule out rotator cuff injuries as it may add to additional cost for the patient, and we ruled out rotator cuff injury with history and clinical examination. Cervical spine/disc pathology was ruled out by history, clinical, and radiological examination only. MRI of the cervical spine was not done because of cost issues.
Conclusion
In summary, the present study shows that SSNB in combination with non-invasive rehabilitation is a safe and effective mode of treatment of the frozen shoulder. The study also conclusively shows that SSNB has a better effect in reducing pain and disability in the frozen shoulder than compared to non-invasive rehabilitation alone or in combination with shoulder intraarticular steroid injection. Future research should focus on identifying the optimal frequency of repetition of SSNB, long term effects of SSNB.
References
Fields, B. K. K., Skalski, M. R., Patel, D. B., White, E. A., Tomasian, A., Gross, J. S., et al. (2019). Adhesive capsulitis: Review of imaging findings, pathophysiology, clinical presentation, and treatment options. Skeletal Radiology, 48(8), 1171–1184.
Shah, N., & Lewis, M. (2007). Shoulder adhesive capsulitis: Systematic review of randomised trials using multiple corticosteroid injections. British Journal of General Practice, 57(541), 662–667.
Lee, S. Y., Lee, K. J., Kim, W., & Chung, S. G. (2015). Relationships between capsular stiffness and clinical features in adhesive capsulitis of the shoulder. PM R, 7, 1226–1234.
Cho, C.-H., Lee, Y.-H., Kim, D.-H., Lim, Y.-J., Baek, C.-S., & Kim, D.-H. (2020). Definition, diagnosis, treatment, and prognosis of frozen shoulder: A consensus survey of shoulder specialists. Clinics in Orthopedic Surgery., 12(1), 60–67.
Mezian, K., & Chang, K.-V. (2019). Contrast-enhanced ultrasonography for the diagnosis of frozen shoulder. Journal of Medical Ultrasound, 27(3), 146–147.
Cheng, X., Zhang, Z., Xuanyan, G., Li, T., Li, J., Yin, L., et al. (2017). Adhesive capsulitis of the shoulder: Evaluation With US-arthrography using a sonographic contrast agent. Scientific Reports, 7(1), 5551.
Mansfield, J. T., & Desai, M. J. (2020). Axillary peripheral nerve stimulation for chronic shoulder pain: A retrospective case series. Neuromodulation. https://doi.org/10.1111/ner.13096.
Cho, C.-H., Bae, K.-C., & Kim, D.-H. (2019). Treatment strategy for frozen shoulder. Clinics in Orthopedic Surgery., 11(3), 249–257.
Akhtar, M., Nadeem, R. D. A., Shah Gillani, S. F. H., Cheema, O. I., & Nadeem, M. R. (2019). Comparison of intra articular NSAID (ketorolac) injection versus hyaluronic acid injection for the mean decrease of pain score (according to UCLA shoulder rating scale) in the management of adhesive capsulitis. Pakistan Journal of Pharmaceutical Sciences, 32(3), 953–956.
Dahan, T. H., Fortin, L., Pelletier, M., Petit, M., Vadeboncoeur, R., & Suissa, S. (2000). Double blind randomized clinical trial examining the efficacy of bupivacaine suprascapular nerve blocks in frozen shoulder. Journal of Rheumatology, 27(6), 1464–1469.
Ozkan, K., Ozcekic, A. N., Sarar, S., Cift, H., Ozkan, F. U., & Unay, K. (2012). Suprascapular nerve block for the treatment of frozen shoulder. Saudi Journal of Anaesthesia, 6(1), 52–55.
Ritchie, E. D., Tong, D., Chung, F., Norris, A. M., Miniaci, A., & Vairavanathan, S. D. (1997). Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: A new modality? Anesthesia and Analgesia, 84(6), 1306–1312.
Gray H. Anatomy: descriptive and applied. In: 30th ed. London: Longmans, Green and Co, 1949:1123–4.
Shanahan, E. M., Ahern, M., Smith, M., Wetherall, M., Bresnihan, B., & FitzGerald, O. (2003). Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Annals of the Rheumatic Diseases, 62, 400–406.
Abdelshafi, M. E., Yosry, M., Elmulla, A. F., Al-Shahawy, E. A.-D., AdouAly, M., & Eliewa, E. A.-K. (2011). Relief of chronic shoulder pain: A comparative study of three approaches. Middle East Journal Anaesthesiology, 21(1), 83–92.
Page, M. J., Green, S., Kramer, S., Johnston, R. V., McBain, B., Chau, M., et al. (2014). Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Systematic Review, 8, 011275.
Hanchard, N. C. A., Goodchild, L., Brealey, S. D., Lamb, S. E., & Rangan, A. (2019). Physiotherapy for primary frozen shoulder in secondary care: Developing and implementing stand-alone and post operative protocols for UK FROST and inferences for wider practice. Physiotherapy., 19(107), 150–160.
Redler, L. H., & Dennis, E. R. (2019). Treatment of Adhesive Capsulitis of the Shoulder. Journal of American Academy of Orthopaedic Surgeons, 27(12), e544–e554. https://doi.org/10.5435/JAAOS-D-17-00606.
Klç, Z., Filiz, M. B., Çakr, T., & Toraman, N. F. (2015). Addition of suprascapular nerve block to a physical therapy program produces an extra benefit to adhesive capsulitis: A randomized controlled trial. American Journal of Physical Medicine and Rehabilitation, 94(10 Suppl 1), 912–920. https://doi.org/10.1097/PHM.0000000000000336.
Taskaynatan, M. A., Yilmaz, B., Ozgul, A., Yazicioglu, K., & Kalyon, T. A. (2005). Suprascapular nerve block versus steroid injection for non-specific shoulder pain. Tohoku Journal of Experimental Medicine, 205(1), 19–25.
Green, S., Buchbinder, R., & Hetrick, S. (2003). Physiotherapy interventions for shoulder pain. Cochrane Database Systematic Review, 2, 004258.
Jones, D. S., & Chattopadhyay, C. (1999). Suprascapular nerve block for the treatment of frozen shoulder in primary care: A randomized trial. Br J Gen Pract J R Coll Gen Pract., 49(438), 39–41.
Buchbinder, R., Green, S., Youd, J. M., Johnston, R. V., & Cumpston, M. (2008). Arthrographic distension for adhesive capsulitis (frozen shoulder). Cochrane Database Systematic Review, 1, CD007005.
Moore TS, Paffett CL, Sibbitt WL, Hayward WA, Gibb JI, Kettwich SD, et al. Glenohumeral injection using anatomic landmark versus sonographic needle guidance. bioRxiv. 2018;395293.
Dominic Harmon and Conor Hearty. “Ultrasound-guided Suprascapular nerve block technique.” Pain Physician 2007; 10:743-746 • ISSN 1533–3159.
Funding
No funding sources for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
We took ethical committee approval from our institute, PGIMER Chandigarh.
Informed consent
Informed consent was taken from all the involved subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parashar, A., Goni, V., Neradi, D. et al. Comparing Three Modalities of Treatment for Frozen Shoulder: A Prospective, Double-Blinded, Randomized Control Trial. JOIO 55, 449–456 (2021). https://doi.org/10.1007/s43465-020-00201-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00201-8